Abstract
Background:
Fixed orthodontic retainers must be well retained on the tooth surfaces, allow physiologic movement of teeth and exert minimal forces on the teeth to be retained. Previous studies analyzed the bond strength and amount of deflection caused due to the debonding force but not the magnitude of force needed for unit deformation.
Aims:
This study aims to evaluate and compare the bond strength and load deflection rate (LDR) of three different fixed retainer wires.
Materials and Methods:
The wires were divided into three Groups: A – three-stranded twisted ligature wire, B – Bond-A-Braid (Reliance Orthodontics), and C – three-stranded twisted lingual retainer wire (3M Unitek). Twenty models were prepared for each group with a passive 15 mm long lingual retainer wire bonded to two lower incisors. An occlusogingival force was applied to the wire until it debonded. For LDR, three-point bending test was done at 0.5 mm deflection. These forces were measured using a Universal Instron Testing Machine.
Statistical Analysis:
Mean bond strength/LDR and pairwise comparisons were analyzed with one-way ANOVA and Tukey's honest significant difference post hoc test, respectively.
Results:
Group C exhibited the highest mean bond strength and LDR of 101.17N and 1.84N, respectively. The intergroup comparisons were all statistically significant.
Conclusion:
Compared to the other two wire types, Group C might be better retained on the teeth due to its higher bond strength. With its relatively higher LDR value, it may resist deformation from occlusal forces, thereby reducing inadvertent tooth movement and yet remain flexible enough to allow physiologic tooth movements.
Keywords: Bond strength, fixed retainer, load deflection rate
Introduction
Perfecting facial esthetics and improving dental health are the main objectives in orthodontic treatment that can be achieved by correctly aligning the teeth. However, if it is not retained on the long run, it can be an unsuccessful and expensive ordeal. Apart from achieving good alignment and retention, patient perception and satisfaction are very important in clinical success. Most patients are unaware of posterior occlusion, but they recognize anterior crowding. Larger part of patients returning for orthodontic retreatment does so because of the crowding that relapsed during retention phase.[1]
Moyers defined orthodontic retention as “the holding of teeth following orthodontic treatment in the treated position for the period necessary for the maintenance of the result.”[2] Posttreatment retention of teeth often require much skill than aligning them and yet considered lightly. Aligned teeth may show no relapse for years but retain its tendency for relapse. Hence, retention has to be a lifelong plan, especially with regard to rotations, midline diastemas, open bites, etc., or at least till growth completion in other cases. Therefore, many orthodontists opt for permanent retention in most of their patients.[3]
Retaining teeth in its aligned position ensures reorganization of periodontal tissues, minimizes changes due to growth, allows neuromuscular adaptation to the new position of the teeth and holds teeth in stable positions with good contact points.[1] Success of these fixed retainers depends on various factors mainly the diameter of the wire and its flexibility, the number of strands of wire and the bond strength with composite. Flexible wires reduce the stress concentration within the bonding composite, thereby minimizing bond failures. However, elastic deformation incorporated into the wire during its manipulation and mechanical deformation from masticatory forces can lead to unwanted tooth movements.[4] Modulus of elasticity or its clinical analog, i.e. load deflection rate (LDR) is a characteristic of the alloy that is used for making the wires and determines its flexibility.[5] LDR is the amount of external loading needed for unit deformation. Wires with very high LDR applies excessive forces on teeth, and their strength decreases quickly with tooth movement.[6]
Hence, a good choice of wire for fixed retention must be flexible enough to allow physiologic tooth movement while exerting minimal forces on the teeth. It should also maintain the teeth in their intended position and be well retained on the teeth without the loss of dimensional stability. However, with the wide arrays of choices, clinicians must be prudent in selecting the appropriate retainer. Although the previous studies have analyzed various fixed retainer wires, the three-stranded twisted retainer wire (3M Unitek) has not been studied so far. These studies also evaluated the amount of deflection brought about by the debonding force but not the magnitude of force needed for unit deformation.[7,8,9] Therefore, the present study was designed to evaluate and compare the bond strength of three commonly used fixed retainer wire-composite system including the three-stranded twisted retainer wire (3M Unitek) as well as the LDR for 0.5 mm deformation in these lingual retainer wires.
Materials and Methods
Evaluation of bond strength
Bond strength was tested using an in vitro model designed such that a vertical force could be simulated at the interdental wire between two mandibular incisors.[9] Caries-free human mandibular incisor teeth with intact lingual enamel were obtained from patients undergoing extractions due to periodontal, prosthetic or orthodontic reasons. The model was prepared by placing two incisors adjacent to each other so as to simulate a contact point between their crowns and the roots embedded in self-cure acrylic till the cervical margin.
The enamel surface of each tooth was cleaned with oil-free pumice, washed with distilled water and dried with air. Lingual enamel surfaces were etched with 37% orthophosphoric acid gel (Transbond™ XT etching gel system; 3M Unitek, Monrovia, California, USA) for 30 s, followed by thorough washing and drying. A 15 mm length of lingual retainer wire gently curved for a passive fit to the lingual surfaces of the teeth was used for each specimen. Following the application of primer (Transbond™ XT system; 3M Unitek), the wire was bonded with light cure adhesive (Transbond™ XT adhesive; 3M Unitek) between the two incisors such that the midpoint of the wire would coincide with the interdental area. A dome-shaped mould wire bonder (Mini-Mold™, Ortho-Care Ltd., Bradford, West Yorkshire, UK) was used to standardize the composite diameter and maximum depth of 4 mm and 1.5 mm respectively; resulting in an area of 12.6 mm2 for each bond and a total bond area of 25.2 mm2 for each specimen. It was light-cured using LEDition Ivoclar Vivadent light cure unit once the excess composite was removed.
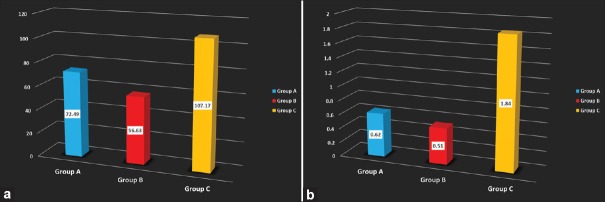
Sixty such models were prepared and divided into three groups (Group A, B, and C) of 20 each. Three different types of wires [Figure 1] were tested; Group A – custom-made three-stranded twisted ligature wires 0.010 inch each (three-stranded-0.030 inch), Group B – 0.016 × 0.022 inch (Bond-A-Braid®, Reliance Orthodontic Products, Itasica, Illinois, USA.) and Group C – three-stranded twisted lingual retainer wire 0.036 inch (3M Unitek). The specimens were stored in distilled water for 24 h before the testing.
Figure 1.
Three types of fixed retainer wires used-Group A (custom-made three-stranded twisted ligature wires), Group B (Bond-A-Braid®, Reliance Orthodontic Products, Itasica, Illinois, USA.), and Group C (three-stranded twisted lingual retainer wire, 3M Unitek)
Shear bond strength was tested with a universal testing machine (Instron, Canton, MA, USA). The model with the embedded teeth was placed in the fixed lower jaw of the machine and the chisel edge attached to the movable upper jaw delivered the vertical force on to the marked midpoint of the interdental wire segment producing a shear force at the wire-tooth interface with a crosshead speed of 2 mm/min. The bond strength measured as the maximum force in Newton (N) to cause debonding/wire removal from the composite pad on at least one of the incisor pairs in each specimen. The reading displayed on the electronic console attached to the Instron unit was recorded.
Evaluation of load deflection rate
The LDR was measured using the three-point bending test with the Instron Machine (Universal Testing Machine, Model 2710-103; Instron, Canton, MA, USA). The same grouping as for bond strength test (Group A, B, and C) was followed with each group having 20 straight pieces of the corresponding wire cut to a length of 30 mm each. The striker or brass rod was attached to the upper movable head of the Instron three-point bending machine, and a vertical force was applied toward the middle of the wire specimen at a crosshead speed of 1 mm/min for loading. The mid-portion of the wire was loaded until it deflected by 0.5 mm. All specimens were prepared and various measurements carried out under identical testing conditions by the same researcher for the purpose of standardization.
Statistical analysis
Descriptive statistics including the mean bond strength and LDR along with the standard deviation was calculated for each group. One-way ANOVA was used to compare the mean bond strength and LDR among the three groups, and Tukey's honest significant difference (HSD) post hoc test was used for pairwise comparisons. Statistical analysis was performed with SPSS version 17.0 (SPSS Inc. Released 2008. SPSS Statistics for Windows, Version 17.0. Chicago: SPSS Inc.) with P threshold set at 0.05.
Results
Bond strength
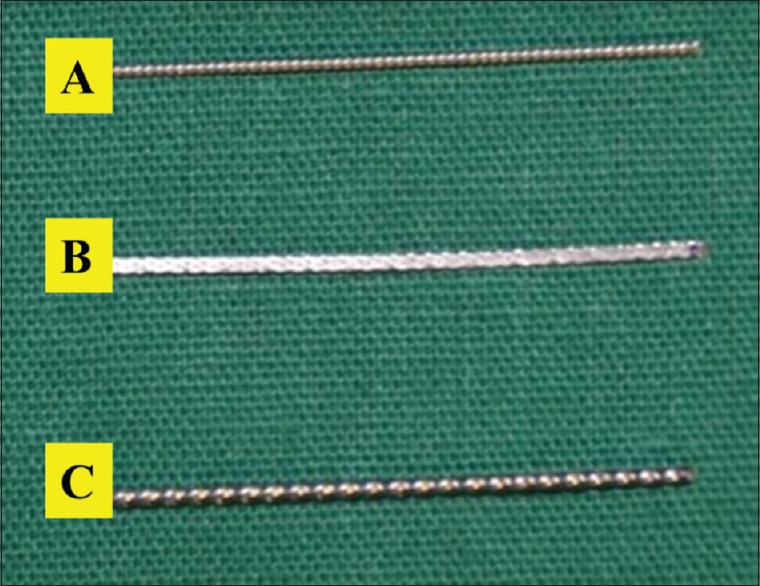
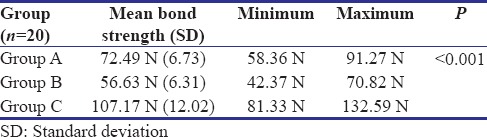
Group C showed the maximum mean bond strength (107.17 N) followed by the Group A and Group B wire with 72.49 N and 56.62 N, respectively [Table 1]. The minimum and maximum bond strength for Group A was 58.36 N and 91.27 N, Group B was 42.37 and 70.82 N, and Group C showed 81.33 N and 132.59 N, respectively. The difference between the mean bond strength of the three groups was analyzed further using Tukey's HSD post hoc test for multiple pairwise comparisons. Mean bond strength of Group A was more than Group B by 15.858 N but less than Group C by 34.684 N. The mean bond strength of Group B was less than Group C by a notable 50.543 N. These comparisons were all statistically significant (P < 0.001).
Table 1.
Mean bond strength of the three retainer wires
Load deflection rate
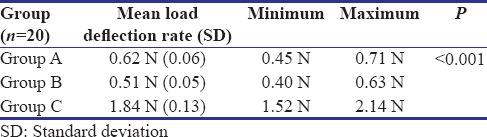
With regard to the LDR, Group C showed the highest mean LDR of 1.84 N followed by Group A and Group B with 0.615 N and 0.511 N, respectively [Table 2]. The minimum and maximum LDR for Group A was 0.445 N and 0.715 N while that of Group B was 0.404 N and 0.632 N, respectively. LDR of Group C showed minimum and maximum values of 1.523 N and 2.144 N, respectively. The difference in the mean LDR between the three groups was analyzed using Tukey's HSD post hoc test to make multiple pairwise comparisons. Mean LDR of Group A was more than Group B by 0.1053 and lesser than Group C by 1.2271 N. LDR of Group B was less than Group C by 1.3324 N. All these findings were statistically significant.
Table 2.
Mean load deflection rate of the three retainer wires
Discussion
Achieving stability is an important aspect of active orthodontic treatment that continues even into the retentive phase. Active orthodontic treatment achieves stability by moving teeth to establish proper occlusion within the limits of normal muscle balance with due consideration of apical base/bases and the relationship of the bases to one another.[10] During retention phase, stability is achieved by reorganization of the gingival and periodontal fibers to the new position of the teeth. Both these mechanisms help to prevent relapse.[11] Lack of stability can lead to loss of either the function or esthetics or both that was achieved during the active phase of treatment. Apart from gingival and periodontal reorganization, the type of treatment along with growth changes that happen after treatment can additionally contribute to relapse. For these reasons, any existing orthodontic control over tooth position and occlusal relationships must be slowly withdrawn to reduce the chances of relapse.[1,2,12] Hence, long-term preservation of anterior teeth in its aligned position with fixed retainers is essential and the type of retention must be included in the initial treatment plan.
The changes in the periodontal ligament that happens during active orthodontic treatment does not revert back to its normal architecture as long as teeth are rigidly splinted to one another. Therefore, as soon as teeth movement is completed, each tooth must be allowed to respond on its own to masticatory forces. Such reorganization may take about 3–4 months and would also allow for any mobility of teeth that was present during appliance removal to wane off. The gingival fibers and supracrestal fibers reorganize at an extremely slow pace and hence produce enough forces to cause relapse. These forces may remain active even beyond 1 year of removal of orthodontic appliance and warrants the role of prolonged retention. Hence, fixed palatal or lingual retainers are advisable. Such retainers remain effective as long as they remain bonded to the tooth surface and are able to withstand occlusal forces without breakage, deformation, or causing inadvertent forces onto the teeth.[1]
The present study was undertaken to examine the bond strength and LDR of three commonly used fixed retainer wires. Although the previous studies evaluated different lingual retainer wires, adhesive systems or their combinations, the three-stranded-twisted lingual retainer wire (3M Unitek) has not been tested before.[7,8,9] Most of these studies evaluated the amount of deflection that occurs during debonding but not the force required to bring about unit deflection (LDR).[7,8,9]
Multistranded wires were chosen for the present study since they can allow for physiological movement of the teeth and their braided surface enhances the retention. A strict protocol was followed to minimize bond failures due to moisture contamination, movement of lingual retainer during curing of the composite or due to inadequate bulk of composite used for bonding. Adequate moisture control was maintained throughout the procedure. To avoid movement of the wire during curing, a passive fit to the lingual surface of the teeth was ensured by incorporating gentle curve into the wire. The amount of composite used for each bond was standardized using the mould wire bonder. It also ensured that the wire would be centered within the composite bond by means of the groove present on the mould. The choice of etchant, primer, and adhesive, length of retainer wire and the steps in bonding were all the same in the three groups so as to the minimize chances of errors. The same operator performed all these procedures, and hence standardization was achieved in this regard.
When the bond strength for the three different retainer wires was studied, it was seen that Group C exhibited the highest bond strength of 107.17 N followed by Group A (72.49 N) and Group C (56.63 N) [Figure 2a]. The value range of bond strength for Group B (Bond-A-Braid) was in accordance with the values obtained for the same in the study done by Baysal et al.[9] Another study done by Radlanski and Zain also showed similar values (64.3N) for bond strength.[13] However, the investigation protocol was different where the force was applied to the adhesive pad of a wire/bond interface. An additional finding in the present study was that wire fractures were encountered with the Group B (Bond-A-Braid). The previous studies on orthodontic brackets showed that a bond strength of 6–8 MPa were sufficient to withstand orthodontic forces while the normal oral loading was between 3 and 18 N. Although it can be assumed that the fixed retainer wires will not be subject to oral loading to the same extent, very little information is available on the minimum clinically acceptable bond strength in relation to bonded retainer wires.[14,15]
Figure 2.
Comparison among the three retainer wires. (a) Mean bond strength. (b) Mean load deflection rate
Similarly, when the mean LDR for the three groups were compared, it was seen that the highest LDR was exhibited by Group C (1.84 N) followed by Group A (0.62 N) and Group B (0.51 N) [Figure 2b]. The higher LDR of Group C (three-stranded-twisted lingual retainer wire) helps it to better resist deformation and hence prevent inadvertent tooth movement. On the contrary, Group A and B exhibited lower LDR (0.5 mm deflection). The previous studies done until date has only assessed the amount of deflection brought about by the debonding force but not the force required to bring about unit deflection.[7,8] Hence, comparison with other studies could not be made with regard to this finding.
According to Lie Sam Foek et al., the results of such in vitro studies can relate to in vivo conditions. However, more clinical studies may be needed to assess the effect of saliva, physiologic movement of teeth, functional forces of tongue, and mastication as well as the presence of plaque and calculus. This inability to mimic in vivo conditions can be considered as a drawback of the present study. Although only human mandibular incisor teeth were used, the wide age group of the teeth donors, varied morphology of lingual surface, tooth size, etc., could have also influenced the results by altering the forces created at the wire-composite-tooth interface. However, this was unavoidable due to difficulties in obtaining teeth based on numerous criteria.[16]
Complex forces could also have arisen when a vertical force was applied to the interdental segment of the wire that was bonded on both ends to the uneven lingual surfaces of lower incisors. Hence, the force value could be expressed only in newton and not as megapascals.[17] The manner in which debonding was done in the investigative the protocol of the study might not be the true representation of the same in the oral cavity. In vivo situations also utilize longer retainer wire lengths extending from canine to canine. The properties of periodontal tissues including its viscoelasticity, width of periodontal ligament space, supporting alveolar bone characteristics, length, shape, and number of roots could not be incorporated into the design of the models, and hence, its influence on the success or failure of the retainers was not evaluated. Another drawback was that the investigative protocols differed among studies and hence, comparison of the results with other studies was difficult. For example in the present study, the debonding force was applied at the interdental segment of the wire. However, some authors preferred to apply force directly at the bonding site.
Conclusion
Ideally, the bond strength of the fixed retainer wires must be high so that they are well retained on the tooth surfaces, and the LDR should be high enough to withstand occlusal forces without deformation but still render the wire flexible enough to allow physiologic tooth movement. If the LDR is low, the wire can deform easily causing inadvertent tooth movement or result in cracks within the composite. Forces of mastication or cleaning the retainer using floss can cause repetitive deformation and ultimately lead to breakage. Lower LDR that results in easy deformation of wires can be an unnoticed cause of relapse. Such an active component may result from improper manipulation of the wire by the clinician or a mechanical deformation by masticatory forces due to lower LDR of the wire.
Overall results showed that the bond strength as well as the LDR was better for Group C (three-stranded twisted ligature wire– 3M Unitek). Hence, as compared to the other two types of wires, Group C might be better retained on the teeth. Due to its relatively high LDR value, it resists deformation from occlusal forces, thereby reducing the chances of inadvertent tooth movement and yet remains flexible enough to allow physiologic tooth movements.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Proffit WR, Fields HW, Sarver DM. Retention. In: Contemporary Orthodontics. 4th ed. Dolan J, editor. St. Louis: Mosby Elsevier; 2007. pp. 617–31. [Google Scholar]
- 2.Moyers RE. Force systems and tissue responses to forces in orthodontics and facial orthopedics. In: Marshall DK, editor. Handbook of Orthodontics. 4th ed. Chicago: Year Book Medical Publishers; 1973. pp. 306–28. [Google Scholar]
- 3.Little RM, Riedel RA, Artun J. An evaluation of changes in mandibular anterior alignment from 10 to 20 years postretention. Am J Orthod Dentofacial Orthop. 1988;93:423–8. doi: 10.1016/0889-5406(88)90102-3. [DOI] [PubMed] [Google Scholar]
- 4.Zachrisson BU. Clinical experience with direct-bonded orthodontic retainers. Am J Orthod. 1977;71:440–8. doi: 10.1016/0002-9416(77)90247-0. [DOI] [PubMed] [Google Scholar]
- 5.Nanda R. Biologic Mechanisms in Orthodontic Tooth Movement. In: Rudolph P, editor. Biomechanics and Esthetic Strategies in Clinical Orthodontics. 1st ed. St. Louis: Elsevier Saunders; 2005. pp. 17–35. [Google Scholar]
- 6.Yang WS, Kim BH, Kim YH. A study of the regional load deflection rate of multiloop edgewise arch wire. Angle Orthod. 2001;71:103–9. doi: 10.1043/0003-3219(2001)071<0103:ASOTRL>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 7.Cooke ME, Sherriff M. Debonding force and deformation of two multi-stranded lingual retainer wires bonded to incisor enamel: An in vitro study. Eur J Orthod. 2010;32:741–6. doi: 10.1093/ejo/cjq017. [DOI] [PubMed] [Google Scholar]
- 8.Aldrees AM, Al-Mutairi TK, Hakami ZW, Al-Malki MM. Bonded orthodontic retainers: A comparison of initial bond strength of different wire-and-composite combinations. J Orofac Orthop. 2010;71:290–9. doi: 10.1007/s00056-010-9947-5. [DOI] [PubMed] [Google Scholar]
- 9.Baysal A, Uysal T, Gul N, Alan MB, Ramoglu SI. Comparison of three different orthodontic wires for bonded lingual retainer fabrication. Korean J Orthod. 2012;42:39–46. doi: 10.4041/kjod.2012.42.1.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lundström AF. Malocclusion of the teeth regarded as a problem in connection with the apical base. Int J Orthod Oral Surg Radiogr. 1925;11:591–602. [Google Scholar]
- 11.Salzmann JA. Factors in successful orthodontic therapy before and after using appliances. Am J Orthod. 1963;49:581–7. [Google Scholar]
- 12.Graber TM, Vanarsdall RL. Retention and relapse. Orthodontics Current Principles and Techniques. In: Schreiber J, editor. 3rd ed. St Louis: Mosby; 2000. pp. 985–1009. [Google Scholar]
- 13.Radlanski RJ, Zain ND. Stability of the bonded lingual wire retainer-a study of the initial bond strength. J Orofac Orthop. 2004;65:321–35. doi: 10.1007/s00056-004-0401-4. [DOI] [PubMed] [Google Scholar]
- 14.Reynolds IR. A Review of direct orthodontic bonding. Br J Orthod. 1975;2:171–8. [Google Scholar]
- 15.Waters NE. Some mechanical and physical properties of teeth. Symp Soc Exp Biol. 1980;34:99–135. [PubMed] [Google Scholar]
- 16.Lie Sam Foek DJ, Ozcan M, Verkerke GJ, Sandham A, Dijkstra PU. Survival of flexible, braided, bonded stainless steel lingual retainers: A historic cohort study. Eur J Orthod. 2008;30:199–204. doi: 10.1093/ejo/cjm117. [DOI] [PubMed] [Google Scholar]
- 17.Katona TR, Moore BK. The effects of load misalignment on tensile load testing of direct bonded orthodontic brackets – A finite element model. Am J Orthod Dentofacial Orthop. 1994;105:543–51. doi: 10.1016/s0889-5406(94)70138-5. [DOI] [PubMed] [Google Scholar]