Abstract
Background:
Fixed orthodontic treatment is time-consuming procedure. Pain is usually associated with orthodontic treatment. The aim of the present study was to evaluate the role of low-level laser therapy (LLLT) on orthodontic tooth movement (OTM) duration and pain perception.
Materials and Methods:
This randomized double-blind splint-mouth controlled clinical study includes 20 (8 males and 12 females) orthodontic patients requiring bilateral canine retraction. Time taken for canine retraction with LLLT (Group A) over control (Group B) quadrant on the same patient was assessed along with pain experience using facial pain scale. The data were tabulated and statistically evaluated using SPSS 20 for windows (Microsoft, Chicago, IL, USA) and t-test with P < 0.05. The difference in pain was evaluated with Wilcoxon signed-rank test.
Results:
There was no difference in values for age and sex of patient for tooth movement and pain (P > 0.05). There was statistically significant decrease in rate of canine retraction in Group A compared to Group B. There was statistically significant difference for maxillary and mandibular arches in Group A whereas it was not significant in Group B. Pain experience was statistically significant till 2nd day, and after 3rd day, it was not significant between the groups.
Conclusion:
LLLT can reduce the fixed OTM timing and pain experience.
Keywords: Laser therapy, orthodontic, pain, tooth movement
Introduction
Orthodontic tooth movement (OTM) is the result from remodeling of bone and periodontal tissue in response to mechanical forces.[1,2] Light mechanical forces are advised to prevent root resorption and necrosis of bone. This results into increased duration of orthodontic treatment, higher chances of root resorption, and dental caries.[1,3] Various methods have been advocated to reduce the treatment duration by nonsurgical (ultrasound waves and electric current), surgical (alveolar decortications, corticotomy, distraction), and pharmacological methods (parathyroid hormones, osteocalcin, and prostaglandin injection). Pharmacological methods are not much promising and can cause pain at the site of injection, while surgical methods are invasive with certain limitation.[1,2,3]
Low-level laser therapy (LLLT) is easy to use, localized, nonsurgical, noninvasive method with no adverse effect hence gaining importance in OTM by many researchers. Various studies have shown that LLLT enhances the vascularization, collagen fiber organization, and osteoblastic activity. There is controversy among the researchers on OTM by LLLT.[1,2] There are very few reported studies on the role of LLLT on OTM. Hence, the present study was undertaken to evaluate the role of LLLT on OTM and on pain experience among the patients.
Materials and Methods
In this randomized double-blind splint-mouth controlled clinical study, 20 patients under fixed orthodontic treatment with simple Class I bimaxillary protrusion cases were included. Sample size of 20 was selected from 200 orthodontic patients at confidence level of 95% with confidence interval of 20.84. In 20 participants, 12 were females and 8 were male patients in the age range of 17–24 years. The study was performed between April 2013 and July 2016. In these patients, each quadrant in maxillary and mandibular arch was divided by third evaluator as study (Group A, LLLT) and control (Group B, no laser therapy) group. Neither the participant nor the first evaluator knows the grouping. Ethical approval was obtained from the institutional ethical committee. Informed consent was obtained from all participating individuals.
The inclusion criteria include extracted first premolars in maxillary and mandibular on both sides at least 3 months before starting to move canines distally after complete aligning and leveling, canines, second premolars, and first molars present in the maxillary and mandibular arches. The exclusion criteria include history of organ transplant, pregnancy, allergy and medications, poor periodontal health, and systemic condition which interferes with OTM.
The initial orthodontic treatment includes sectional alignment and leveling of canines, second premolars, and the first molars. MBT bracket system was used for this study with 0.022” slot. Canines were retracted using sectional closing loops (fabricated from 16 × 22 steel wire 5 and 7 mm leg length in the mandible and maxilla, respectively) placed in the middle of the extraction site and a force of 150 g was applied. The amount of force was measured using a Correx (Haag-Streit Ber) force gauge. The loops were reactivated on both sides every month for 2 mm. The amount of tooth movement was determined by measuring the distance between the canine cusp tip and mesiobuccal cusp tip of the first molar on dental casts after the application of force using a digital caliper (Mitutoyo, Japan).
The four quadrants were randomly divided into laser and control groups. Laser group was irradiated with low-level Ga-Al-As laser (810 nm, 5 J/cm2). A gallium-aluminum-arsenide semiconductor diode laser emitting infrared radiation was used at continuous mode with a power output of 0.2 W and a frequency of 2 Hz. The laser was applied to the buccal and palatal aspect of the tooth for 80 s weekly for 21 days. The laser was applied in accordance with the protocol of the Photon Lase Plus unit (DMC, São Carlos, São Paulo, Brazil). During laser application, the tip was applied in close contact to apical, middle, and cervical third of root on buccal and lingual side for 5 s. Tooth movement was measured on progress models.
Amount of canine retraction was evaluated on 4 pairs of casts for each patient at onset of retraction (C1), 2 months after canine retraction (C2), and 3 months after retraction (C3), on completion (C4). The rate of canine retraction was assessed with T1 at 2 months, T2 at 4 months (C3-C1), and T3 on completion (C4-C1). The data were further verified by 2nd investigator.
Patients were asked to record the level of pain experienced on days 1 to 7 following laser application on Wong-Baker Faces Rating Scale which consists of number of faces ranging from happy to crying.
The data were tabulated and statistically evaluated using SPSS 20 for windows (Microsoft, Chicago, IL, USA) and t-test with P < 0.05. The difference in pain was evaluated with Wilcoxon signed-rank test.
Results
In our study, the mean age range was 19.75 ± 1.65 years. There was no difference in values for age and sex of patient for tooth movement and pain (P > 0.05). There was statistically significant decrease in rate of canine retraction in LLLT over control group [Table 1]. In Group A, LLLT for maxillary arch rate of canine retraction was 1.17 ± 0.15 after 2nd month, 1.78 ± 0.28 after 4th month, and 1.97 ± 0.21 after completion of treatment. In mandibular arch for Group A, it was 0.78 ± 0.013, 0.87 ± 0.014, and 0.97 ± 0.011 after 2nd month, 4th month, and after treatment completion, respectively. For Group B in maxillary arch, it was 1.01 ± 0.25, 1.38 ± 0.24, and 1.57 ± 31, respectively, after 2nd month, 4th month, and after completion. For mandibular arch, it was 0.68 ± 0.26, 0.85 ± 011, and 0.88 ± 0.15, respectively, after 2nd month, 4th month, and after treatment completion [Table 1]. There was 1.17–1.9-fold increase in the rate of canine tooth movement in Group A. The results were statistically significant.
Table 1.
Canine retraction rate between Group A and Group B
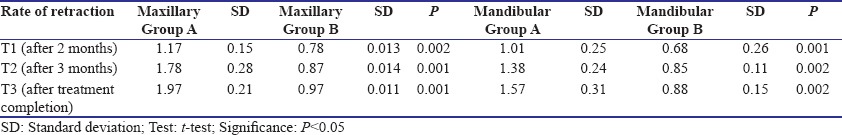
Table 2 shows the comparison of maxillary and mandibular arches in Group A which is statistically significant. Table 3 shows comparison between maxillary and mandibular arches in Group B, which was statistically not significant.
Table 2.
Comparison of canine retraction rate between maxillary and mandibular Group A
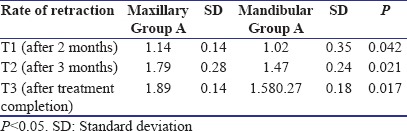
Table 3.
Comparison of canine retraction rate between maxillary and mandibular Group B

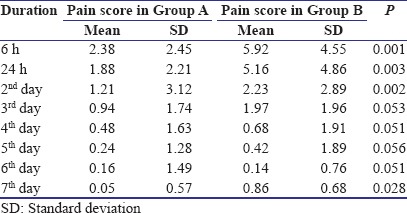
Table 4 shows pain experience in Group A over Group B from 6 h time to 7th day postoperatively. There was a gradual decrease in pain perception in both the groups. It was statistically significant till 2nd day, and after 3rd day, it was not significant between the groups.
Table 4.
Pain score comparison between Group A and Group B with facial pain scale
Discussion
Main drawback of orthodontic procedure is pain and longer duration of treatment following application of forces. Various methods such as laser therapy have been tried to reduce the pain and the treatment duration.[2] However, it is not studied thoroughly, and the available studies are quite controversial; hence, the present study was done to evaluate the role of LLLT on treatment duration and pain.
Photobiomodulation is referred to as LLLT, which is gaining importance nowadays. LLLT is also called as low-power laser, biostimulation laser, therapeutic laser, soft-tissue laser, cold laser, and laser accupunctation.[4] Biomodulation effect of laser is based on Arndt–Schulz law. This law states that small dose of any substance or drug has a stimulating effect, whereas higher dose has inhibitory effect.
It has been observed from previous studies that LLLT reduces duration of tooth movement by improving alveolar bone remodeling by increasing number of osteoclasts, pdl cellular proliferation, and mineralized bone formation.[5]
In the present study, 810 nm, 5 J/cm2 of laser irradiation was applied at 8 spots for 10 s. We have observed that 65% lesser time was required for canine retraction in laser group over control one. Similar results were found in Kochar et al.[1] LLLT has shown decrease in treatment timing; these results are in agreement with results of studies by Sousa et al. and Cruz et al.[6,7] We found 1.6-fold increase in canine retraction rate which is in agreement with results of Kocher et al., Sousa et al., and Youssef et al.[1,6,8] We found 1.17–1.97 retraction rates in maxilla and 0.78–0.97 in mandible for canine retraction with LLLT, but it was only 1.01–1.57 in maxilla and 0.66–0.88 in Group B from T1 to T3. These results are similar to that of Kocher et al. and Moaffak et al.[1,9] In contrast to our results, Dalaie et al., Heravi et al., and Alten et al. found no difference in retraction time between irradiated and nonirradiated site.[2,10,11]
Different researchers used different wavelength of laser therapy for the procedure ranging from 600 nm to 1000 nm with an energy density of 0.04–60 J/cm2 with diode laser, Ga-Al-As diode laser, or He-Ne laser. Different researchers used different wavelength radiation of laser and obtained acceptable result for orthodontic tooth movement and pain reduction. Dalaie et al. used 880 nm, Gama et al. used 790 nm wavelengths, Yoshida et al. and Fujita et al. used 810 nm, Al Sayed Hasan et al. used 830 nm, similarly by Sobuti et al., Amid et al. and we have used 810 nm wavelength for similar results.[2,12,13,14,15,16,17] Meta-analysis has shown weaker response rate at 780 nm 5 J/cm2 with output power of 20 mW. Dalaei et al. observed greater effect with laser irradiation in maxilla over mandible similar to our results.[2] Yassaei et al. and Amid et al. form systematic review and concluded that LLLT can help in increasing the OTM.[3]
Root resorption is major adverse effect in OTM. Seifi et al. suggested that laser beam irradiation in combination with alloplastic materials used for socket preservation could reduce the degree of root resorption significantly.[18] Ng et al. found lesser root resorption with LLLT compared to placebo laser.[19]
Pain is the major complaint among the patients undergoing fixed orthodontic treatment. It has been reported that 28% orthodontic patients discontinue treatment due to pain. Although pain is subjective and may vary among individuals, studies have shown that all patients, regardless of age, have reported some degree of pain during treatment.[20] Analgesics are commonly prescribed to reduce pain. Several researchers have believed that use of these analgesics to reduce pain can decrease OTM by disrupting the osteoclast activity and inhibiting prostaglandin action.[16] We have found that there was reduction in pain experience initially for 2 days with LLLT compared to control group with facial pain scale [Table 4]. Later on, the pain experience became similar in both the groups. Our results are consistent with results of Sobouti et al. who observed lower pain perception with laser compared to control side. They used single-dose He-Ne laser therapy (632.8 nm, 10 mw, 6 J/cm2 density) and observed 4.06 ± 2.85 and 2.35 ± 1.77 average pain score on control and laser-treated side, respectively.[16] In contrast to our results, Furquim et al. observed no significant reduction in pain sensation with LLLT.[20] Similar to our study, Farias et al., Eslamian et al., and Youssef et al. found reduction in orthodontic pain using 810 wavelength laser for 15 seconds per point.[21,22,23] Deana et al. conducted a search in the MEDLINE, EMBASE, Scopus, Cochrane Library, Web of Science, and EBSCO host databases and included 20 articles from 467 identified articles. They observed reduction of spontaneous and chewing pain with LLLT 780–940 nm in orthodontic treatment. Researchers observed that 810 nm laser was found to be most effective.[24] Bayani et al. from randomized controlled trial study concluded that single irradiation form LLLT to be best strategy for orthodontic pain control.[25]
Verschueren et al. concluded that LLLT generates a photobioactive reaction to stimulate cellular proliferation and differentiation which leads to increased local blood circulation that removes the pain-inducing inflammatory mediators and enhances the cellular activities.[26] LLLT is found to combat pain by accelerating the removal of pain-inducing substances such as substance P, histamine, dopamine, and prostaglandins and decrease pain through the reduction of prostaglandin-E2 levels and the inhibition of cyclooxygenase-2, interleukin-1 beta, tumor necrosis factor-alpha, and edema.[4,27] Eshghpour et al. found reduction in pain after 3rd molar surgery using 810 nm LLT.[28]
We have observed from the present study that LLLT has shown promising results in decreasing the duration of fixed orthodontic treatment procedure and pain experience during the course compared to control group (without use of LLLT). Increased tooth movement in LLLT may be due to increased revascularization, bone remodeling, and college synthesis.
Further research is required to evaluate the role of LLLT on fixed orthodontic treatment in larger sample size on patients with different geographic background.
Conclusion
LLLT can increase the fixed OTM timing and reduce the pain experience during orthodontic procedure.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Kochar GD, Londhe SM, Varghese B, Jayan B, Kohli S, Kohli VS. Effect of low level laser therapy on orthodontic tooth movement. J Indian Orthod Soc. 2017;51:81–6. [Google Scholar]
- 2.Dalaie K, Hamedi R, Kharazifard MJ, Mahdian M, Bayat M. Effect of low-level laser therapy on orthodontic tooth movement: A Clinical investigation. J Dent (Tehran) 2015;12:249–56. [PMC free article] [PubMed] [Google Scholar]
- 3.Yassaei S, Fekrazad R, Shahraki N. Effect of low level laser therapy on orthodontic tooth movement: A review article. J Dent (Tehran) 2013;10:264–72. [PMC free article] [PubMed] [Google Scholar]
- 4.Kohale B, Agarwal AA, Sope AB, Paradeshi KV, Raut CP. Low level laser therapy: A literature review. Int J Laser Dent. 2015;5:1–5. [Google Scholar]
- 5.Ekizer A, Türker G, Uysal T, Güray E, Taşdemir Z. Light emitting diode mediated photobiomodulation therapy improves orthodontic tooth movement and miniscrew stability: A randomized controlled clinical trial. Lasers Surg Med. 2016;48:936–43. doi: 10.1002/lsm.22516. [DOI] [PubMed] [Google Scholar]
- 6.Sousa MV, Scanavini MA, Sannomiya EK, Velasco LG, Angelieri F. Influence of low-level laser on the speed of orthodontic movement. Photomed Laser Surg. 2011;29:191–6. doi: 10.1089/pho.2009.2652. [DOI] [PubMed] [Google Scholar]
- 7.Cruz DR, Kohara EK, Ribeiro MS, Wetter NU. Effects of low-intensity laser therapy on the orthodontic movement velocity of human teeth: A preliminary study. Lasers Surg Med. 2004;35:117–20. doi: 10.1002/lsm.20076. [DOI] [PubMed] [Google Scholar]
- 8.Youssef M, Ashkar S, Hamade E, Gutknecht N, Lampert F, Mir M, et al. The effect of low-level laser therapy during orthodontic movement: A preliminary study. Lasers Med Sci. 2008;23:27–33. doi: 10.1007/s10103-007-0449-7. [DOI] [PubMed] [Google Scholar]
- 9.Moaffak MA, Hasan A, Sultan K, Hamadah O. Low-level laser therapy effectiveness in accelerating orthodontic tooth movement: A randomized controlled linical trial. Angle Orthod. 2017;87:499–504. doi: 10.2319/062716-503.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Heravi F, Moradi A, Ahrari F. The effect of low level laser therapy on the rate of tooth movement and pain perception during canine retraction. Oral Health Dent Manag. 2014;13:183–8. [PubMed] [Google Scholar]
- 11.Altan BA, Sokucu O, Toker H, Sumer Z. The effects of low-level laser therapy on orthodontic tooth movement: Metrical and immunological investigation. JSM Dent. 2014;2:1040. [Google Scholar]
- 12.Gama SK, Habib FA, Monteiro JS, Paraguassú GM, Araújo TM, Cangussú MC, et al. Tooth movement after infrared laser phototherapy: Clinical study in rodents. Photomed Laser Surg. 2010;28(Suppl 2):S79–83. doi: 10.1089/pho.2009.2618. [DOI] [PubMed] [Google Scholar]
- 13.Yoshida T, Yamaguchi M, Utsunomiya T, Kato M, Arai Y, Kaneda T, et al. Low-energy laser irradiation accelerates the velocity of tooth movement via stimulation of the alveolar bone remodeling. Orthod Craniofac Res. 2009;12:289–98. doi: 10.1111/j.1601-6343.2009.01464.x. [DOI] [PubMed] [Google Scholar]
- 14.Fujita S, Yamaguchi M, Utsunomiya T, Yamamoto H, Kasai K. Low-energy laser stimulates tooth movement velocity via expression of RANK and RANKL. Orthod Craniofac Res. 2008;11:143–55. doi: 10.1111/j.1601-6343.2008.00423.x. [DOI] [PubMed] [Google Scholar]
- 15.Hassan MM, Sultan K, Hamadah O. Low level laser therapy effectiveness in accelerating orthodontic tooth movement: A randomized controlled clinical trial. Angle Orthod. 2017;87:499–504. doi: 10.2319/062716-503.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sobout F, Khatami M, Chiniforush N, Rakhshan V, Shariati M. Effect of single-dose low-level helium-neon laser irradiation on orthodontic pain: A split-mouth single-blind placebo-controlled randomized clinical trial. Prog Orthod. 2015;16:2–7. doi: 10.1186/s40510-015-0102-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Amid R, Kadkhodazadeh M, Ahsaie MG, Hakakzadeh A. Effect of low level laser therapy on proliferation and differentiation of the cells contributing in bone regeneration. J Lasers Med Sci. 2014;5:163–70. [PMC free article] [PubMed] [Google Scholar]
- 18.Seifi M, Atri F, Yazdani MM. Effects of low-level laser therapy on orthodontic tooth movement and root resorption after artificial socket preservation. Dent Res J (Isfahan) 2014;11:61–6. [PMC free article] [PubMed] [Google Scholar]
- 19.Ng D, Chan AK, Papadopoulou AK, Dalci O, Petocz P, Darendeliler MA, et al. The effect of low-level laser therapy on orthodontically induced root resorption: A pilot double blind randomized controlled trial. Eur J Orthod. 2017 doi: 10.1093/ejo/cjx065. doi: 10.1093/ejo/cjx065 [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 20.Furquim RD, Pascotto RC, Neto JR, Cardoso JR, Ramos AL. Low-level laser therapy effects on pain perception related to the use of orthodontic elastomeric separators. Dent Press J Orthod. 2015;20:37–42. doi: 10.1590/2176-9451.20.3.037-042.oar. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Farias RD, Closs LQ, Miguens SA., Jr Evaluation of the use of low-level laser therapy in pain control in orthodontic patients: A randomized split-mouth clinical trial. Angle Orthod. 2016;86:193–8. doi: 10.2319/122214-933.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Eslamian L, Borzabadi-Farahani A, Hassanzadeh-Azhiri A, Mr B, Fekrazad R. The effect of 810-nm low-level laser therapy on pain caused by orthodontic elastomeric separators. Lasers Med Sci. 2014;29:559–64. doi: 10.1007/s10103-012-1258-1. [DOI] [PubMed] [Google Scholar]
- 23.Youssef M, Ashkar S, Hamade E, Gutknecht N, Lampert F, Mir M, et al. The effect of low-level laser therapy during orthodontic movement: A preliminary study. Lasers Med Sci. 2008;23:27–33. doi: 10.1007/s10103-007-0449-7. [DOI] [PubMed] [Google Scholar]
- 24.Deana NF, Zaror C, Sandoval P, Alves N. Pain Res Manag 2017. 2017. Effectiveness of low-level laser therapy in reducing orthodontic pain: A systematic review and meta-analysis. Article: 8560652, 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bayani S, Rostami S, Ahrari F, Saeedipouya I. A randomized clinical trial comparing the efficacy of bite wafer and low level laser therapy in reducing pain fallowing initial arch wire placement. Laser Ther. 2016;25:121–9. doi: 10.5978/islsm.16-OR-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Verschueren RC, Koudstaal J, Oldhoff J. The carbon dioxide laser; Some possibilities in surgery. Acta Chir Belg. 1975;74:197–204. [PubMed] [Google Scholar]
- 27.Pandit A, Singhvi J, Bhardwaj S, Singh A, Sharma S. Efficacy of soft tissue diode laser on pain reduction induced by elastomeric separators: A clinical investigation. Int J Oral Health Med Res. 2017;4:22–6. [Google Scholar]
- 28.Eshghpour M, Ahrari F, Takallu M. Is low-level laser therapy effective in the management of pain and swelling after mandibular third molar surgery? J Oral Maxillofac Surg. 2016;74:1322e1–8. doi: 10.1016/j.joms.2016.02.030. [DOI] [PubMed] [Google Scholar]


