Abstract
Objective:
The purpose of the study is to determine the prevalence of TMDs among the 12-18 years and 19-30 years patient age group requiring orthodontic treatment by using the Fonseca's questionnaire.
Material and Methods:
A total of 390 patients who visited the orthodontic department for treatment were asked to fill Fonseca's questionnaire. The results were analyzed for both the age groups and the percentage values were compared between males and females, different types of malocclusion and presence of TMDs.
Results:
In the 12-18 years age group, around 18.75% of the males and 12.28% of the females were having some degree of TMJ dysfunction. In the 19-30 years age group, around 30.32% of the females were found to have some severity of TMJ dysfunction as opposed to 19.23% of males. In the 12-18 years age group, around 11% of Class I, 16% of Class II and 50% of class III patients were having some degree of temporomandibular dysfunction. In the 19-30 years age group, the results showed that around 24% of Class I and class II patients and 50% of Class III patients presented with some degree of TMD. In the 12-18 years age group around 15% and in the 19-30 years age group, around 25% of the patients presented with some degree of TMD ranging from mild, moderate to severe.
Conclusion:
The study concludes that significantly more number of females presented with TMDs as compared to males in the 19-30 years age group. As the age increases the presence of TMDs also increases because of the significant presence of TMDs in the 19-30 years age group as compared to 12-18 years age group.
Keywords: Malocclusion, orthodontics, research, temporomandibular disorders, temporomandibular joint
Introduction
Temporomandibular disorders (TMDs) are a collective term that defines a subgroup of painful orofacial disorders, involving complaints of pain in the temporomandibular joint (TMJ) region, fatigue of the cranio-cervico-facial muscles (especially masticatory muscles), limitation of mandible movement, and the presence of articular clicking.[1] The etiology of TMDs can be multifactorial which can include traumatic injury, immunological disorders, neoplasm, stress, and local factors such as interferences in occlusion, malocclusion, postural changes, abnormal functioning of the masticatory musculature, changes in the TMJ structure, clenching or bruxing, or a combination of such factors.[2] Loading, altered jaw position, and mechanical stress in response to the treatments induce morphological changes in the TMJ, due to its inherent adaptive capacity.[3]
The interrelationship between the causation of TMD because of the presence of malocclusion and vice versa is highly debatable. A recent systematic review concludes that there are insufficient research data on the relationship between active orthodontic intervention and TMD on which to base our clinical practice.[4] However, it is important to know the existing level of TMDs before starting with an orthodontic treatment. This can help us plan the treatment better and evaluate the factors which can accentuate or relive the symptoms.
The prevalence of TMDs ranges from 20% to 50%.[5,6,7] The variability in prevalence may be attributed to differences in the race of the population, in the sampling design and criteria. Screening for TMDs in a population is a challenge for researchers and clinicians, and several TMD assessment tools have been proposed in the literature. However, no universal diagnostic criteria have yet been established. In response to this need for a universally accepted TMD assessment tool, research diagnostic criteria for TMDs (RDC/TMDs)[8] were proposed, which have since been used in several clinical and epidemiological studies. A new comprehensive version of the RDC/TMDs, known as the diagnostic criteria for TMDs (DC/TMDs), has been proposed by Schiffman et al. in 2014.[9] According to them, the DC/TMD includes a valid and reliable screening questionnaire and diagnostic algorithms for the most common pain-related TMDs. With all the advantages, the RDC/TMD and DC/TMD are still cumbersome tools for assessment as they require the presence of the person to reach a TMD diagnosis and also they are difficult to use on large samples.
The Fonseca's anamnestic index (FAI) is a self-administered, low-cost, easily applied questionnaire that can be used for TMD assessment in the nonpatient population. The use of FAI for detecting TMD signs and symptoms offers the advantage of being easily used by either general practitioners or epidemiologists. Thus, the FAI would serve as a preliminary TMD screening tool. After identifying the affected population, a complete clinical examination and further use of diagnostic instruments is required to confirm the diagnosis. Campos et al. in 2009[10] have recommended the use of FAI as it is simple, takes less time to fill, and cost effectiveness. The questionnaire also provides a severity index with less influence from the examiner and less variability in the measures.
Fonseca's questionnaire follows the characteristics of a multidimensional evaluation. It is composed of 10 questions that screen for the presence of pain in the TMJ, head, and back; pain while chewing; parafunctional habits; movement limitations; joint clicking; perception of malocclusion; and sensation of emotional stress.
The purpose of the study is to determine the prevalence of TMDs among the patients requiring orthodontic treatment and to understand the association of malocclusion with the TMDs.
Aims and objective
The aims of the study are as follows:
To assess the epidemiological prevalence of TMD in males and females in the 12–18 years and 19–30 years age group through a cross-sectional descriptive study based on Fonseca's questionnaire among the outpatients visiting Government Dental College, Indore
To assess the presence of TMD with the type malocclusion (Angle's molar relationship) present in the 12–18 years and 19–30 years age group.
Materials and Methods
Study design
This descriptive cross-sectional research project was performed in the Government College of Dentistry, Indore, Madhya Pradesh, India. Considering 5% margin of error, 95% confidence level, 20,000 population size, and 50% response distribution, a sample size of 377 was recommended for the study. Random sampling method was used to select the sample subjects. In total, 390 patients of malocclusion were evaluated between the period of June 2015 and May 2016. All the participants were informed about the study aims, and a brief information about TMD was given to volunteers. There was no time limit for the participants to complete the questionnaire.
Inclusion criteria for the study group included age group of 12–30 years and no previous history of orthodontic treatment. Exclusion criteria for the study group included patients having history of neurological or musculoskeletal disorders, history of TMJ trauma or treatment, and immunocompromised patients.
Data collection
The questionnaire conceived by Fonseca (1992) was used to evaluate the degree of TMD in sample subjects of this study, as it demonstrates a high efficiency in obtaining epidemiological data. This questionnaire contains an anamnestic index, and the sample subjects were rated accordingly as non-TMD (0–15), light TMD (20–40), moderate TMD (45–65), and severe TMD (70–100). The questionnaire consists of 10 questions, and the possible answers are “SOMETIMES,” “YES,” or “NO,” with a single answer to be marked for each question. The results were analyzed using the frequency distribution of the questionnaire answers according to the anamnestic index proposed by Fonseca (1992). The positive answers (“yes” and “sometimes”) were summed. The percentage values were compared between males and females, different types of malocclusion, and presence of TMDs.
Results
The data were formulated, computed, and analyzed. Chi-square analysis was used as a test of statistical significance. P < 0.05 was considered statistically significant. Table 1 represents the presence of TMDs based on FAI in male and female population of 12–18 years group. Around 18.75% of the males and 12.28% of the females had some degree of TMJ dysfunction. The difference was found to be statistically insignificant. Table 2 represents the presence of TMDs based on FAI in male and female population of 19–30 years group. Around 30.32% of the females were found to have some severity of TMJ dysfunction as opposed to 19.23% of males. The data were found to be statistically significant (P < 0.05). Table 3 represents the presence of TMDs based on Angle's molar relationship in male and female population of 12–18 years group. Around 11% of Class I, 16% of Class II, and 50% of Class III patients had some degree of temporomandibular dysfunction. The difference was found to be statistically insignificant. Table 4 represents the presence of TMDs in different malocclusion based on Angle's molar relationship in male and female population of 19–30 years group. The results showed that around 24% of Class I and Class II patients and 50% of Class III patients presented with some degree of TMD. These results were found to be statistically insignificant (P < 0.05). Table 5 represents the presence of TMDs in different malocclusion based on the age group of 12–18 years and 19–30 years. Around 15% of the younger age group and 25% of the older age group presented with some degree of TMD ranging from mild, moderate to severe. These results were found to be statistically significant (P < 0.05).
Table 1.
Presence of temporomandibular disorders based on Fonseca's anamnestic index in male and female population of 12-18 years group
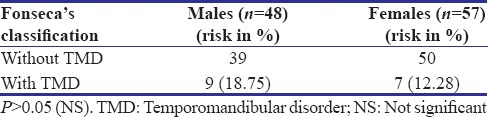
Table 2.
Presence of temporomandibular disorders based on Fonseca's anamnestic index in male and female population of 19-30 years group
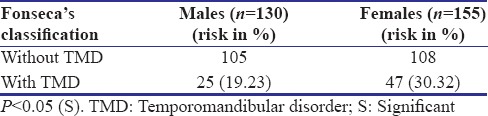
Table 3.
Presence of temporomandibular disorders based on Angle's molar relationship in population of 12-18 years group
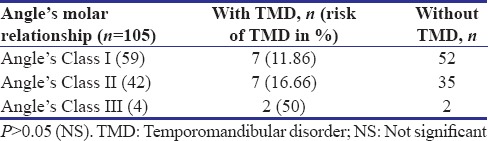
Table 4.
Presence of temporomandibular disorders based on Angle's molar relationship in population of 19-30 years group
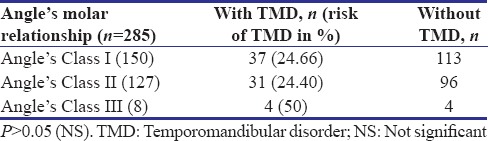
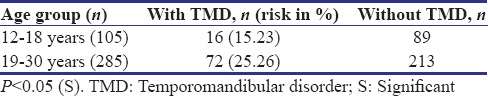
Table 5.
Presence of temporomandibular disorders based on the age group of 12-18 years and 19-30 years
Discussions
The present study provides information about the prevalence of TMDs, based on the FAI, in the orthodontic patients visiting Government College of Dentistry, Indore, Madhya Pradesh, India. In this study, around 18.75% of males and 12.28% females in the 12–18 years age group presented with some degree of TMDs. Around 30.32% of the females in the 19–30 age group showed the presence of TMDs as compared to 19.23% males in the same age group [Tables 1 and 2]. This finding reveals that as the age increases, the presence of TMD also increases. Furthermore, these data are statistically significant and support the finding of the other studies performed by de Oliveira et al. and Nomura et al. that females have a greater predisposition toward the risk of developing TMDs as compared to males studies.[11,12] Females sex hormone estrogen can be responsible for this sex-related difference in the prevalence of TMDs.[13] Stress and anxiety play important roles in TMDs by acting as predisposing or aggravating factors. A high incidence of these symptoms has been reported in TMD patients. In our study, around 52% of the total females from both the age groups have responded “sometimes/yes” to the last question of the Fonseca's questionnaire which is, “Do you consider yourself a tense (nervous) person”? as compared to 22% males. However, it is difficult to measure a variable such as stress or anxiety. Psychological factors are known to play a role in the etiology and persistence of TMDs.
As the patients presented themselves for orthodontic treatment, the findings of malocclusion in the anteroposterior plane (Angle's molar relationship) were also recorded. Around 11.86% of the patients with Class I, 16.66% with Class II, and 50% with Class III in the 12–18 years age group presented with some form of TMDs [Table 3]. In the 19–30 years age group, around 24.66% patients with Class I, 24.40% with Class II, and 50% with Class III presented with some degree of TMDs [Table 4]. No statistically significant difference has been found in the different types of malocclusion and the age groups. A study conducted by Thilander et al.[14] in the 5–17 years age group reported that the prevalence of TMDs in Class I, II, and III malocclusion was 25.3%, 28.9%, and 32.1%, respectively. In our study, similar results have been found except in Class III where more prevalence of TMD has been seen. In this study, posterior crossbite, unilateral crossbite, extreme maxillary overjet, and frequent clenching have also been found to be associated with severe form of TMD.
When both the studied age groups were compared for the presence or absence of TMDs, it was shown that around 15.23% of participants in the age group of 12–18 years and 25.26% participants in the age group of 19–30 years were classified by the FAI as having TMDs [Table 5]. This prevalence is less than the range of FAI-based TMD prevalence rates (42%–68%) reported by other investigators.[6,11,12,15,16] The variation in TMD prevalence among these studies may be attributed to ethnic background, race, different age groups, and gender distribution.
When the data of the participants with severe form of TMD was analyzed in this study, it was revealed that in the 12–18 years age group, around 4% of the males and 3.5% of the females presented with severe form of TMD. In the same age group, when malocclusion and severe TMD were compared, it was shown that 1.6% of Class I, 4.7% of Class II, and 25% Class III had severe TMD. In the 19–30 years age group, around 5% of the males and 9% of the females had severe TMD. In addition, 4% of Class I, 6% of Class II, and 25% of Class III had severe form of TMD.
In the present study, only the anteroposterior relationship has been taken into consideration. Also, the sample size for Class III is less. Hence, there is a need for studies with large sample size of this issue in the local population. Although our study provided some information regarding the prevalence and severity of TMDs in the population, long-term clinical studies should be conducted in this region.
Conclusion
Based on the FAI, the prevalence of TMD appears to be evident in the population. The FAI is a useful TMD screening tool that has important implications for the early diagnosis of TMD. Longitudinal studies in this population are warranted to follow the prevalence of TMD and the health-care needs of TMD patients. The followings are the conclusions from this study:
Significantly more number of females presented with TMDs as compared to males in the 19–30 years age group
In the 19–30 years age group, the presence of TMDs was more as compared to 12–18 years age group.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Habib SR, Al Rifaiy MQ, Awan KH, Alsaif A, Alshalan A, Altokais Y, et al. Prevalence and severity of temporomandibular disorders among university students in Riyadh. Saudi Dent J. 2015;27:125–30. doi: 10.1016/j.sdentj.2014.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.de Santis TO, Motta LJ, Biasotto-Gonzalez DA, Mesquita-Ferrari RA, Fernandes KP, de Godoy CH, et al. Accuracy study of the main screening tools for temporomandibular disorder in children and adolescents. J Bodyw Mov Ther. 2014;18:87–91. doi: 10.1016/j.jbmt.2013.05.018. [DOI] [PubMed] [Google Scholar]
- 3.Arnett GW, Milam SB, Gottesman L. Progressive mandibular retrusion – idiopathic condylar resorption. Part I. Am J Orthod Dentofacial Orthop. 1996;110:8–15. doi: 10.1016/s0889-5406(96)70081-1. [DOI] [PubMed] [Google Scholar]
- 4.Michelotti A, Iodice G. The role of orthodontics in temporomandibular disorders. J Oral Rehabil. 2010;37:411–29. doi: 10.1111/j.1365-2842.2010.02087.x. [DOI] [PubMed] [Google Scholar]
- 5.Lee JY, Kim YK, Kim SG, Yun PY. Evaluation of Korean teenagers with temporomandibular joint disorders. J Korean Assoc Oral Maxillofac Surg. 2013;39:231–7. doi: 10.5125/jkaoms.2013.39.5.231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Modi P, Shaikh SS, Munde A. A cross sectional study of prevalence of temporomandibular disorders in university students. Int J Sci Res Publ. 2012;2:1–3. [Google Scholar]
- 7.Vojdani M, Bahrani F, Ghadiri P. The study of relationship between reported temporomandibular symptoms and clinical dysfunction index among university students in Shiraz. Dent Res J (Isfahan) 2012;9:221–5. doi: 10.4103/1735-3327.95240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dworkin SF, LeResche L. Research diagnostic criteria for temporomandibular disorders: Review, criteria, examinations and specifications, critique. J Craniomandib Disord. 1992;6:301–55. [PubMed] [Google Scholar]
- 9.Schiffman E, Ohrbach R, Truelove E, Look J, Anderson G, Goulet JP, et al. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for clinical and research applications: Recommendations of the international RDC/TMD Consortium Network and Orofacial Pain Special Interest Group. J Oral Facial Pain Headache. 2014;28:6–27. doi: 10.11607/jop.1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Campos JA, Goncalves DA, Camparis CM, Speciali JG. Reliability of a questionnaire for diagnosing the severity of temporomandibular disorder. Rev Bras Fisioter. 2009;13:38–43. [Google Scholar]
- 11.de Oliveira AS, Dias EM, Contato RG, Berzin F. Prevalence study of signs and symptoms of temporomandibular disorder in Brazilian college students. Braz Oral Res. 2006;20:3–7. doi: 10.1590/s1806-83242006000100002. [DOI] [PubMed] [Google Scholar]
- 12.Nomura K, Vitti M, Oliveira AS, Chaves TC, Semprini M, Siéssere S, et al. Use of the Fonseca's questionnaire to assess the prevalence and severity of temporomandibular disorders in Brazilian dental undergraduates. Braz Dent J. 2007;18:163–7. doi: 10.1590/s0103-64402007000200015. [DOI] [PubMed] [Google Scholar]
- 13.Cairns BE. Pathophysiology of TMD pain – Basic mechanisms and their implications for pharmacotherapy. J Oral Rehabil. 2010;37:391–410. doi: 10.1111/j.1365-2842.2010.02074.x. [DOI] [PubMed] [Google Scholar]
- 14.Thilander B, Rubio G, Pena L, de Mayorga C. Prevalence of temporomandibular dysfunction and its association with malocclusion in children and adolescents: An epidemiologic study related to specified stages of dental development. Angle Orthod. 2002;72:146–54. doi: 10.1043/0003-3219(2002)072<0146:POTDAI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 15.Conti PC, Ferreira PM, Pegoraro LF, Conti JV, Salvador MC. A cross-sectional study of prevalence and etiology of signs and symptoms of temporomandibular disorders in high school and university students. J Orofac Pain. 1996;10:254–62. [PubMed] [Google Scholar]
- 16.Shiau YY, Chang C. An epidemiological study of temporomandibular disorders in university students of Taiwan. Community Dent Oral Epidemiol. 1992;20:43–7. doi: 10.1111/j.1600-0528.1992.tb00672.x. [DOI] [PubMed] [Google Scholar]


