Abstract
Aim:
This exploratory qualitative research is an attempt to assess the health care ethical challenges in dental practice in an Indian scenario.
Methodology:
Qualitative indepth interview was conducted on 20 dental professionals to assess the ethical challenges prevailing in dental practice in Indian scenario. After obtaining the responses the verbatims were categorized into categories and finally 36 themes emerged. Later from two group of 6 panellists each after conducting focus group discussion the themes of ethical issues occurring in dental practice were ranked based on order of significance impact on the practice, patient and society using Delphi method.
Result:
The top ten ethical challenges listed by the panellists are inadequate sterilization and waste management in dental clinics, poor knowledge and attitude towards ethics among our dental practitioners, in competence among dental professional, increase in cost of oral health service, poor informed consent process, requirement of consensus about the treatment procedures among dentists, Conflict in Advertising, clustering of dental clinics in urban areas, disagreement with treatment modalities among dentist and patient, poor medical record maintenance among our dental practitioners.
Conclusion:
The study attempts to bring the prevailing ethical challenges in oral health care practice in Indian scenario.
Keywords: Dental ethics, dentists, informed consent, medical record, qualitative research
Introduction
The ultimate motto or supreme goal of any profession is to provide quality and standard services to people; these professions are governed by the set of rules and ethical principles to achieve these goals. Ethics is a belief that determines the people behavior and resides in the realm of human values, moral, individual culture interpersonal belief, and faith.[1]
Ethical practice in health care is defined as consisting of informed consent, respect for integrity and patient autonomy.[2] In the past few decades, the balance of decision-making in determining what is the “best” treatment has shifted from professional paternalism toward respecting the informed and autonomous decision of the patient.[3]
Since 1960, dentistry has reached great heights in improving diagnosis and treatment of oral health.[4] Advancement in technology has changed the way the dental professionals’ practice.[5] Like any other profession, the focus on ethical aspects of dentistry is increasing than ever before, and oral health practitioner is facing ethical issues or dilemmas in everyday practice.
In the past two decades, India has witnessed significant raise in the number of dentists, dental practices, and dental negligence cases on the other hand, there is an increased demand for quality care by the patient, and also the advancement of dental technology in terms of diagnosis and treatment has created the new areas of ethical ambiguity and uncertainty, thus placing the dental practitioners in a challenging situation in patient care.
Given this situation, dentist should be knowledgeable and be able to analyze and attempt to resolve any issues arising in patient care.
Studies have reported limited formal training in health-care ethics for dentists and they rely only on the experience and the outline of ethical principles studied during undergraduation and constantly struggling between right and wrong which has a significant impact on the patient and society at large. The evidences related to dental ethics are of Western origin, and the perspectives cannot be generalized to our situation. However, the studies regarding dental ethics in Indian scenario focus on research ethics’ and clinical settings, patient autonomy, and informed consent.
To our knowledge, there is no work done either at micro or macrolevel with respect to dental ethical challenges faced by the dentist in the Indian scenario. Hence, the present study was conducted to assess the ethical challenges in dental practice and to rank the top ten challenges faced by the Indian dentists.
Methodology
Type of research
Qualitative research was used to assess the ethical issues in dental practice.[6] As the data available related to ethical challenges in Indian Scenario were very meager, qualitative research was chosen as it provides the deeper understanding and the expert's perceptive on ethical issues in dental practice. It also uses interpretative and naturalist approaches to the research question. Since the qualitative method uses the inductive method of data analysis, qualitative research can be used in the absence of any theory.[7]
Theoretical frameworks
The study aimed to focus on individual, group, and societal framework related to ethical issues in dental practice. At individual level, it helps to assess expert's opinion, perception, learning, and personality about the ethical challenges present in dental practice. At group level, the study will be helpful to assess expert's opinion on ethical issues in work team, interpersonal network, and interaction of expert's experience. At social level, the study helps to assess dental professional ethical issues related to professional organization relation, rules, globalization, advertisements, and interaction with professional bodies.
Method
Open-in-depth interview and focus group discussion were done to assess the ethical issues in dental practice among a group of subject experts and general dental practitioners. Open-in-depth interview encouraged the participant to talk in depth about their perspective on ethical challenges in dental practice in Indian Scenario. Focus group discussion motivated the participants to understand the other perspectives and exchange ideas. This led to the better understanding when some doubt and confusion aroused among the study participants.
Sampling and sampling design
The purposive and judgmental sampling method was used to collect data from subject experts and general dental practitioners. Purposive sampling was done because due to their experience in research interest, academics, and clinical practice these people were believed as experts in the field of ethics and law in dental practice. Due to the interest in research, the selected participants they were also hoped to provide a rich source of data related to ethical challenges in dental practice.[8]
Source of data
Dental subject experts
Twenty-five persons who qualified the eligibility criteria were selected for the study. Due to their interest and experience in research, academics, and clinical practice, these professionals were believed as experts in the field of the study.
Eligibility criteria
Among subject experts in the first stage for in-depth interview, dental professionals involved in academics for 10 years, recognized PG teacher, who had research interest in ethics, and also having clinical practice experience were included in the study. In second stage for focus group discussion, dental professionals who had at least 6 years of academics, who had a research interest in ethics and law and also involved in clinical practice were selected.
General dental practitioners
General dental practitioners who are in active and full-time clinical dental practice were considered.
After explaining the purpose of the study, totally 32 persons gave consent and participated in the study. In first stage of the study, five subject experts and 15 practicing dentists participated in in-depth interview, and in the second stage, 12 dental professionals participated.
Interview guide for the study
In the first stage, five experts were interviewed using unstructured interview guides. Open-ended question was used since it gave the degree of freedom to the experts in expressing their opinion. Dental subject experts were requested to site some ethical and legal challenges faced in dental practice in India. Second, they were questioned if they can you describe an incident or two in your or colleague's practice which has made you morally uncomfortable, which has implications on patient or practice. How was that incident resolved? Finally, they were questioned if the dental curriculum has enough scope for learning clinical ethics for incorporating into dental practice. And also what steps that can be taken to enhance ethical practice among our dental professionals.
Methodology
The subject expert's and dental practitioners were interviewed in a convenient place both for the study participants and investigator with the in-depth, open-ended question using unstructured interview guide. A standardized general interview guide approach and grounded theory were used to gather information to ensure that the same general areas of information are collected from each interviewee. Interviews ranged from 15 to 25 min. All the interviews were audiotaped. Notes were also taken down by the investigator during the interview and elaborate memo writing was done after each interview. Interviews were transcribed by the two investigators (V. K and K. G) separately so as to avoid interviewer bias with related to understanding of the investigator and later compared for coding. Attempt was made to include as many themes were possible so that it included different perspectives of all the experts. Interview brought the significant information related to ethical challenges in dental practice.
Grounded theory helps focus on social processes or actions. Grounded theory approach uses inductive method of data analysis moving from particular to general. It develops new theories or hypotheses from many observations. Common coding technique and constant comparative method of qualitative data analysis were used for coding statements given by subject experts and general practitioners. According to constant comparative technique as new transcripts were reviewed and new codes emerged, new quotes were compared with previous codes in an iterative process. Attempts were made to look into the theoretical insight of the statements. The aim of the analysis was to generate the conceptual category and its relative subcategory.[8,9]
After interview with subject experts and practicing dentist to achieve triangulation, i.e. a procedure to reach redundancy of all the ethical challenges’ different sources of information such as review of literature was done. Attempt was made to include as many themes were possible so that it included different perspectives of all the experts. Finally, based on the interview and review of literature, totally 36 themes were generated. Then, remaining subject experts were invited for focus group discussion to discuss the themes and rank them in the order of significance. Two rounds of focus group discussion each consisting of six person panellist were done. At the end of the discussion, the panellist was asked to rank these themes, and finally, all the 12 experts separately ranked the themes. The criteria for ranking included how often or frequently these ethical challenges occur or likely to occur in day-to-day practice. After obtaining the ranking from the experts, the ranks for the individual themes were summed up separately, and the themes with maxing response were given the higher ranking (1st rank), and similarly, subsequent ranks were given. The highest ranked theme was assigned the 10 marks and next highest 9 marks; similarly, the subsequent ranks were assigned. The maximum score that could be achieved by a single item was 120, which would result only if the same item was ranked as the top challenge by all 12-panel members.
This method of analyzing the data is called Delphi Method. Here, the data collected are analyzed by consensus building and inductive analysis is used. This has an advantage of reflective analysis of each panellists and thus avoiding personality conflicts between each panellists.[8,9] Ethical clearance-Human Ethical Clearance was obtained from MR Ambedkar Dental College Ethical Review Committee, Bengaluru.
Results
This exploratory study attempted to analyze the subject's experts and general practitioners’ opinion on perceived ethical challenges in dental practice among Indian dentists. The results were based on 19 subject experts and 15 dental practitioners’ perceptions.
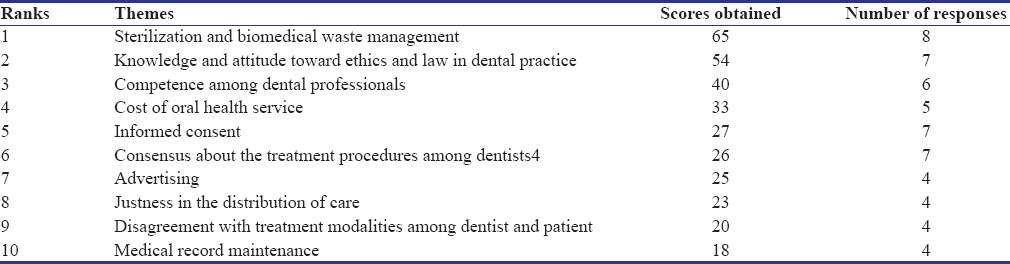
After first round of in-depth interview with the subject experts and general practitioners, the verbatims were made to categorize into categories and finally 36 themes were developed. Later, these themes were ranked top 10 by subject experts in order of severity and magnitude of ethical issues of occurring in the Indian context [Table 1].
Table 1.
Top10 ethical challenges in dental practice
The top one ethical challenge citied was the inadequate sterilization and waste management in dental clinics. Standard infection control includes a number of specific practices such as PPE, prevention of cross-contamination, proper waste disposal, and worker protection.[10] Subject experts were concerned that the general practitioners were not following universal precautions and said “Sterilization protocol not followed in most of the clinics and when patient's ask I feel uncomfortable to report to them,” “sterilization prevents the transfer of bacteria/infection from one patient to another.” General dental practitioners were concerned about health-care waste management and said “Improper waste disposal contaminate the environment,” “It is the duty of dentist that waste is disposed in a proper manner in the interest of safety.” Dentists are not getting attached to waste management company and disposing health-care waste along with regular waste. Dentists were also concerned with needle stick injuries in dental clinics and said “A used needle should be disposed in the correct manner to prevent needlestick injuries. It is the duty of dentist that waste is disposed in a proper manner in the interest of safety.”
The second ethical challenges presented by our panellists were poor knowledge and attitude toward ethics among our dental practitioners: considering ethics and giving importance only to the technical aspect. Subject expert felt that “Ethics is extremely important and it differs from doctor to doctor. What I feel ethical might not be ethical to others a uniform code is wherein patient interest has to be taken first, his need his finance and before the doctor economic consideration,” other subject expert citied that “Dentist who is unaware of ethical issues can land in trouble.” Subject expert citied that “Lack of knowledge about the subject as well as lack of commitment leads to under treatment.” Dentists should participate in continuing education activities that provide information, strengthen clinical competencies, and enhance professional judgment. While it is not possible for any dentist to be abreast of all advancements, dentists should make every effort to at least be familiar with clinical developments that may potentially affect their practices including the general scientific basis of such developments and related issues and problems. The general dental practitioners who participated in the study were not aware of any programs related to ethics and law. One of the general practitioners citied “I am not aware of an extra course. It would be helpful. We had a chapter on ethics I can't say whether it is sufficient.”
The third ethical challenge was competence among dental professional. The competent dentist is able to diagnose and treat the patient's oral health needs and to refer when it is in the patient's best interest. Maintaining competence requires continual self-assessment about the outcome of patient care and involves a commitment to lifelong learning. The general dental practitioners said about the incompetence of few dentists that “I thought I should not criticize the other dentist. Or tell the patient it's wrong,” “I don't know any law what has to be done in such a situation. Maybe I should seek a lawyer.” Incompetence can also lead to over and under treatment “Unhealthy competition is putting unnecessary burden on patient.” Dentist not practicing the policy of wait and watch, performing the restoration even in incipient caries lesion, etc., money mindedness. Subject expert regarding the ethical issue of overtreatment said that “it has become a marketing strategy to project to the patient that extreme make over's. In reality it is question as to whether we are doing justice to the patient by subjecting unnecessarily as to extreme treatment modalities.”
The fourth ethical challenge is the increase in cost of oral health service: rising cost of health care can limit patient access to health care, limited resources can lead to rationing and delaying, and denial of care to people in need. Escalating cost can lead to inverse care law. Regarding the cost factor, the subject expert's cited “The disparity in the economic status forces the budding doctors to opt for a sector where they are highly paid and thus not opting for rural service and thus making them suffer.” General dental practitioners defended that “Cost depends on the experience of the dentist too apart from laboratory work.” Regarding the high cost of dental care, general dental practitioners feel “Patient demand for a better looking clinic. We have to spend on exterior, so price shoots up. However, in reality, we need to provide quality work. Most of the medical clinics have just got the bench and chairs, and patient goes there but when it comes to dentistry patient expectation changes.”
The fifth ethical challenge was the poorly informed consent process. Ethical concerns regarding the process of informed consent and refusal extend beyond the level required for compliance with the law. The process of informed consent requires comprehensive knowledge on the part of the practitioner, uncompromising veracity, unbiased presentation of all reasonable alternatives, and consequences including costs and the probability of outcomes. It also requires the ability of practitioner to communicate clearly on a level assuring comprehension by the patient or appropriate authority. Subject experts advice the dentist to work in full accordance with informed consent. “It safeguards the dentist against misuse by patients. At the same time patients are also safe from anything done apart from the treatment committed at the beginning.”
The sixth ethical challenge is the requirement of consensus about the treatment procedures among dentists: advancement in biotechnology like to do or not to do treatment, choosing of treatment modalities when different approaches are present has led to disagreement in treatment procedures among dentists. Hence, the experts cited that “The practical experience of each and every dentist varies from one to another. It is always good to incorporate a collective experience and choose the best out of the lot.” One of the general dental practitioner was concerned about the faulty treatment of neighboring dentist and stated “Previous dentist had said that he is doing all ceramic crown and charged a very high amount when I examined I found it to be acrylic crown. I did not know what to do.” When such issue arises, they were in dilemmas and conflict of what they should do. One of the general practitioner also stated “I was in a middle of a see-saw; we don't know whether to go with patient what he wants or do ethical practice. I could not say that you had been doped.” Another general practitioner stated “I thought I should not criticize the other dentist. Or tell the patient it's wrong,” general dental practitioners are also in dilemma whom to contact “I don't know any law what has to be done in such a situation. Maybe I should seek a lawyer.”
Subject experts felt that when in conflict with the treatment procedure “Obtaining second opinion can make the patient mentally satisfied of receiving correct treatment. Also it gives the doctor boost of his correct decision.”
The seventh ethical challenge in dentistry is conflict in advertising: Law says advertising by a dentist must not misrepresent fact, mislead or deceive by partial disclosure of relative facts, and create false or unjustified expectations of favorable results. Today's dental practitioners feel that advertisement is needed and stated “I feel the policy of advertising is not for today's scenario, dentistry is practiced in multistoried building and keeping only the small Name board is not sufficient. Using attractive colours and increase font is required so that it is visible to people,” “Advertising can also be used as an education tool. It increases knowledge and awareness.” General dental practitioners stated “Advertising make people aware of a clinic or specialty,” “In present scenario patients are in confusion among to which hospital or doctors are best and advertisement can create awareness.” Even though they were not against advertisement, they were against wrong advertising “Claiming superspeciality is misguiding to the patients.” One of the subject experts gave corporate culture as a reason for change in advertisement “In present scenario patients are in confusion among to which hospital or doctors are best and advertisement can create awareness.”
The eighth ethical challenge is the clustering of dental clinics in urban areas: issues of fairness are pervasive in dental practice and range from elemental procedural issues such as whom shall receive treatment first, to complex questions of who shall receive treatment at all. Regarding the practice of location and accessibility of dental care to patients, the general dental practitioners said “The just dentist must be aware of these complexities when balancing the distribution of benefits and burdens in practice. It is the choice of the dentist to choose his/her area/locality of practice,” “Laws can be made by the government to ensure that all population has access to care and also providing employment to dentists.” Dentist population ratio is 80:20 where 80% of dentist practice in place where 20% of population live in urban areas and inversely only 20% of dentist live where 80% of population live. Regarding accessibility of oral health care, inverse care law is still existing even though there is rise in graduating dentist; there is shortage of dentist in few places because of inappropriate distribution of dentist. Subject experts were concerned that “Dental clinics in shopping malls,” “Dental clinics in high floored buildings,” “Poor accessibility for continuation of treatment.” Advanced dental care setup was in it can have potential financial burden for patients for basic oral health care.
The ninth ethical challenge is the disagreement with treatment modalities among dentist and patient: In the era of internet, it is not uncommon to come across patients who already surfed internet about the disease and its treatment options. Subject experts were of the opinion that it the age of internet “Patients these days surf internet for information they are presented with. Situations arise wherein patients challenge the treatment plan of dentists.” General dental practitioners were concerned that “Patients are unaware that each situation is different and dentists have learnt it from experience and in profession. Everything cannot be read in internet,” “If patient asks for some inappropriate treatment then we have to educate the patient it's not that we have to blindly follow patient will. Doctor should help the patient to make the informed choice,” “Some people had come with pre conceived idea about treatment and when we give the options they don't agree and say some other treatment we try to convince but if patient is not agreeing then we will explain and tell to think about it for some time and if still not convinced we go ahead with the treatment they want.” This is particularly true where the normative and felt need of the person varies. Examples to this include extraction versus root canal treatment and orthodontic versus no treatment. General dental practitioner were also concerned that “Children teeth are neglected, most of the parents don't agree with preventive treatment modalities like space maintainers, pulpectomy because of lack of finance or knowledge, so children are not benefited. Milk teeth are not considered important and convincing them is very difficult even among educated parents, it is changing but in very small percentage,” sometimes the dentist feel that “People attitude prevents one from practicing ethics and I don't agree establishing clinic's ethics consultation committees.” Some general dental practitioners felt that there is a high expectation from patients and stated that “When patient comes to clinic with sensitivity and we diagnose gingivitis I advise scaling and give medication. But the patient will be expecting immediate result which cannot be attained and its put me difficult position since I am not able to convince the patient”. Contradicting to this one of the general practitioners stated “I think the patient should demand, he need to ask for a certificate. He should ask for authentication of the work done. What is the material used. Some times when patient shifts from one place to another certification helps.” Subject experts also felt the high expectation because of which there is a high pressure on the practitioners “Doing fixed orthodontics in periodontally compromised patient, here the prognosis is poor but treatment has to be done because of pressure from patient, parent pressure.” Meeting patient expectation is a challenge. Patients who used to accept dentists’ advice unquestioningly now ask dentists to defend their recommendations.
The tenth ethical challenge was the poor medical record maintenance among our dental practitioners: as the consumer negligence cases are increasing, it is important to maintain medical records. Subject experts felt that “Medial Record is a legal document and reference for future cases. It safeguards the dentists against fraud/false statements by patients which are intended to harm/defame them.”
Discussion
This qualitative study was conducted to explore health-care ethical challenges in current dental practice in the perspective of subject experts and general dental practitioners’ opinion in Indian Scenario. Qualitative study provided some degrees of flexibility in data collection, statistical analysis and helped in generalizability of the study result since it uses the general inductive approach. The participants who participated in the present study were selected based on the assumption that they will be in a position to understand and provide a rich source of data compared to the representative group of dental professionals. Interview gave an in-depth understanding and individual opinion in personal matter and focus group discussion helped in understanding severity and intensity of the opinion.
The present study showed the first ethical challenge as sterilization and waste management in health care. The dentists felt that there is no uniform, standardized sterilization and waste management. The participants are of the opinion that sterilization protocol is not followed in dental clinics and it might lead to health hazards. Studies have shown that serious shortcoming in infection control in developing countries.[10] In a study done by Sudhakar and Chandrashekar on dental practitioners in Bangalore city, a large proportion of the dentists were not practicing proper methods of health-care waste disposal. Nearly 42.1% felt that there was a lack of waste management agency services and 16.9% felt that a lack of knowledge were the main hurdles. The authors felt that dentists need education regarding health-care waste disposal methods to improve their knowledge.[11] In a study done Sanjeev in Kothamangalam, 18.2% of dental professionals dispose the biomedical waste into general garbage and 19.3% of the dental professionals were not having any tie-up with any biomedical waste management company.[12] In a study done by Zohara Kayamali in Chennai City, 89.6% of the dental professionals disposed the waste in common bin and only 10.4% dispose their dental wastes to certified collectors.[13]
The present study showed that there was a concern among panellist that there is a lack of knowledge and attitude of health-care ethics among our dental professionals. Empirical studies have shown that the physicians, dentists, and nurses have appreciated the importance of knowledge of ethics, but the majority of studies have shown poor knowledge of ethics and health law which has resulted in a violation of ethical principles.[3,14,15,16,17,18,19] Contrastingly, some of the studies have reported good to fair knowledge among dental professionals.[18,20,21]
The third ethical challenges emphasized by our panellist were related to competence in professional health-care services. Incompetence can lead to unfavorable behavior among the dental professionals in their service. Professionalism expands on the basic principles of ethics to include the conduct, character, aims, and qualities that characterize a professional. It should accompany the use of superior knowledge, skill, and judgment to the benefit of patient and society, before any consideration of self-interest.[22,23,24] Dentists should keep up the basic levels of competency required for delivering effective oral health-care delivery. The lack of competence has serious consequences on the oral health and psychosocial well-being. Due to the rapid progress of the medical knowledge, dentists have to study continuously to maintain their competence at high standards.[15,25,26] Deviated dental professional behaviors such as defensive medicine, overtreatment, and treatment error could be due to lack of professional skill and knowledge. Even though dentistry is a noble profession, it has become more commercial. Nexus between doctors, the practice of cross reference as a routine, is also burdening patients psychologically and financially.[27] Kress et al. identify dentist issues such as poor-quality treatment delivered by another dentist, difficulty in maintaining OSHA regulations.[15] Parsapoor et al., and Breslin et al. have identified the treatment error because of incompetence and poor consensus among dental professionals.[17,28]
The fifth ethical challenge panellist identified it as increase in cost of dental health services. In the present study dental professionals perceived that cost escalation of the dental service could also be due to patient expectation of high tech dental clinics. In our other study, bioethicists were also concerned about the commercialization of dental practice.[29] Referral charges, billing, and cost are few of the top challenges as reported by Daniel. J. Schulte in Michigan Dental Association Annual Session 2009.[30] A national survey of practicing dentist in America and in the study done by Kress et al. have citied high operating costs such as infection control requirements, staff benefits, equipment, and supplies as a cause for increasing in the cost of dental care.[3,15,31]
In the present study, panellist felt the importance of informed consent and advised the dental professionals to take informed consent as it also helps them to safeguard themselves form litigations. In Jonathan's study, the panel of experts says that there is a huge gap in the process of informed consent in theory and practice. Sometimes, the patients cannot understand what is right and wrong related to their diagnosis and treatment procedures. Sometimes, informed consent is not taken for all the procedures in patient understanding, but the treatment would have been carried out taking granted that informed consent is obtained.[19,32,33] In the study done by SAT Porter on practicing dentist in Queensland, 98% of respondents believe that the patient should be provided with detail of all options and be involved in the choice of treatment.[3] Even though in majority of the studies, dental professionals obtain consent it is more general compared to consent obtained for individual treatments.[21,34]
Advertisements were another imported ethical challenge as reported by the panellists. In the Dentists (Code of Ethics) Regulations 1976, highlight advertising, “whether directly or indirectly, for the purpose of obtaining patients or promoting his own professional advantage,” or “acquiescing in the publication of notice commending or directing attention to the practitioner's skills, knowledge, service or qualifications, or of being associated with or employed by those who procure or sanction such advertising or publication through press reports” is defined as unethical. In spite of the ban on advertising by dentists, there are some who have resorted to some kinds of advertising to promote their services. The present study emphasized an attitude change emerging in the upcoming generation of dentists, as the majority of younger dentists approve of advertising, while their seniors reject it. Studies have shown that this may be a reflection of industry competition, a drop in ethical standards, or a greater familiarity with the world of advertising and media among younger age groups.[35]
Dable et al. found that, in her study, 32.62% felt that advertisement could be beneficial as it helps in communication. Only 26.9% felt that advertisement could be hazardous. Nearly 83.68% of the dentists strongly opposed advertisements such as “Get teeth in one day and painless dentistry” which were regarded as unscientific and misleading. In a retrospective study done by Pacheco on ethical proceedings against dentist in Espirito Santo for infringements to the code of dental ethics. It demonstrated that among 529 cases examined 39.7% were on illicit advertising. The code permits advertisement of the inauguration of a hospital, shifting of hospital, and facilities available at a hospital, but the advertisement has to have a prescribed format and size. Nobody observes this code these days. An escape route of advertisement issued by well-wishers is also found.[35,36]
Recommendations
Subject experts and general practitioners recommended requirement of updating the ethics curriculum to resolve issue by including the ethics teaching in clinical practice and to make it more case sensitive with giving examples. One of them citied that “Clinical ethics taught as part of PG curriculum not UG because of time constraints” “Practical orientation in clinics of UG should be emphasized or stressed A seed gives a better yield if sown on a fertile ground. As with any professional student, their mind is more receptive when they first encounter the subject. The legal and moral responsibility of a health care student can be best inculcated during this time which remains for a life time.” Dental practitioners also recommended to attend CDE programs “I feel the need for continuing dental education programs to enhance my knowledge related to clinical ethics.” Some advice to resolve ethical issues during their practice and citied “I resolved this type of patients by effectively communicating with the patient from the beginning of the clinical encounter. I involved the patient in decision making. I have found this useful.” Studies have emphasized that professional education should pay attention to character the formation of an every dentist as it is central to moral life. Role modeling by faculty members should be done to build a sustainable community of clinicians focused on the ethical concerns for patients and societies. Different clinical teaching methods such as role play, standardized patient, and internet-based cases’ scenarios should be used. Enhancing professional communication skill and teaching clinical ethics at the chair side with staff having both clinical and ethical skills should be done.[18,37]
Limitations
Generalizability of qualitative research is questionable since the results are applicable to the study particular group of population and also in that region. Since the coding is more a subjective nature, a varied interpretation could be possible but attempts were made by doing multiple coding to reduce the investigator bias. Due to lack of qualitative research, few quantitative researches were included for the comparison.
Conclusion
We conclude that there were many ethical challenges faced by the dentist in their practice. The present study could rank them as top ten significant challenges from knowledge to advertisement. However, quantitative analysis is required to see the strength and severity and other factors associated with these challenges and also to resolve or adapt to these challenges by dentist in their day today practice.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Edge RS, Groves JR. 2nd ed. Blackwell's, UK: Delmar Publishers; 1998. Ethics of Health Care: A Guide for Clinical Practice. [Google Scholar]
- 2.Hansson MG, Kihlbom U, Tuvemo T, Olsen LA, Rodriguez A. Ethics takes time, but not that long. BMC Med Ethics. 2007;8:6. doi: 10.1186/1472-6939-8-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Porter SA, Grey WL. Ethical dilemmas confronting dentists in Queensland, Australia. Aust Dent J. 2002;47:241–8. doi: 10.1111/j.1834-7819.2002.tb00336.x. [DOI] [PubMed] [Google Scholar]
- 4.Lebuis A, Lai B, Emami E, Feine JS. New technologies in health care. Part 1: A moral and ethical predicament. J Can Dent Assoc. 2008;74:631–5. [PubMed] [Google Scholar]
- 5.Muriel JB. Promoting ethical development and professionalism: Insights from education research in the professions. Univ St Thomas Law J. 2008;5:366–403. [Google Scholar]
- 6.Golafshani N. Understanding reliability and validity in qualitative research. Qual Rep. 2003;8:597–607. [Google Scholar]
- 7.Tavallaei M, Mansor AT. A general perspective on role of theory in qualitative research. J Int Soc Res. 2010;3:571–7. [Google Scholar]
- 8.Marshall MN. Sampling for qualitative research. Fam Pract. 1996;13:522–5. doi: 10.1093/fampra/13.6.522. [DOI] [PubMed] [Google Scholar]
- 9.Sbaraini A, Carter SM, Evans RW, Blinkhorn A. How to do a grounded theory study: A worked example of a study of dental practices. BMC Med Res Methodol. 2011;11:128. doi: 10.1186/1471-2288-11-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Scarlett MI, Grant LE. Ethical oral health care and infection control. J Dent Educ. 2015;79:S45–7. [PubMed] [Google Scholar]
- 11.Sudhakar V, Chandrashekar J. Dental health care waste disposal among private dental practices in Bangalore City, India. Int Dent J. 2008;58:51–4. doi: 10.1111/j.1875-595x.2008.tb00176.x. [DOI] [PubMed] [Google Scholar]
- 12.Sanjeev R. Knowledge, attitude, and practices about biomedical waste management among dental healthcare personnel in dental colleges in Kothamangalam: A cross-sectional study. Health Sci. 2014;1:JS001I. [Google Scholar]
- 13.Charania ZK. Awarness and practices of dental care waste management among dental practitioners in Chennai City. J Contemp Dent. 2011;1:15–21. [Google Scholar]
- 14.Cederberg RA, Valenza JA. Ethics and the electronic health record in dental school clinics. J Dent Educ. 2012;76:584–9. [PubMed] [Google Scholar]
- 15.Kress GC, Hasegawa TK, Jr, Guo IY. A survey of ethical dilemmas and practical problems encountered by practicing dentists. J Am Dent Assoc. 1995;126:1554–62. doi: 10.14219/jada.archive.1995.0087. [DOI] [PubMed] [Google Scholar]
- 16.DuVal G, Sartorius L, Clarridge B, Gensler G, Danis M. What triggers requests for ethics consultations? J Med Ethics. 2001;27(Suppl 1):i24–9. doi: 10.1136/jme.27.suppl_1.i24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Breslin JM, MacRae SK, Bell J, Singer PA. University of Toronto Joint Centre for Bioethics Clinical Ethics Group. Top 10 health care ethics challenges facing the public: Views of Toronto bioethicists. BMC Med Ethics. 2005;6:E5. doi: 10.1186/1472-6939-6-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.John JS. A Study on the Awareness among the Doctors about Consumer Protection Act in a Selected Hospital. Dissertation Rajiv Gandhi University of Health Sciences. 2005 [Google Scholar]
- 19.Hariharan S, Jonnalagadda R, Walrond E, Moseley H. Knowledge, attitudes and practice of healthcare ethics and law among doctors and nurses in Barbados. BMC Med Ethics. 2006;7:E7. doi: 10.1186/1472-6939-7-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Milind TW. Awareness of medico-legal issues among medical and dental college health professionals of Vadodara, Gujarat. J Indian Assoc Public Health Dent. 2011;9:280–4. [Google Scholar]
- 21.Gupta VV, Bhat N, Asawa K, Tak M, Bapat S, Chaturvedi P, et al. Knowledge and attitude toward informed consent among private dental practitioners in Bathinda City, Punjab, India. Osong Public Health Res Perspect. 2015;6:73–8. doi: 10.1016/j.phrp.2014.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Brosky ME, Keefer OA, Hodges JS, Pesun IJ, Cook G. Patient perceptions of professionalism in dentistry. J Dent Educ. 2003;67:909–15. [PubMed] [Google Scholar]
- 23.Bruscino T. Basic Ethics in Dentistry. The Academy of Dental Learning & OSHA Training. 2012 [Google Scholar]
- 24.Seidemann M. Ethics and dentistry: A symbiosis and challenge. Int Coll Dent. 1997;7:59–68. [Google Scholar]
- 25.Rosenbaum JR, Bradley EH, Holmboe ES, Farrell MH, Krumholz HM. Sources of ethical conflict in medical housestaff training: A qualitative study. Am J Med. 2004;116:402–7. doi: 10.1016/j.amjmed.2003.09.044. [DOI] [PubMed] [Google Scholar]
- 26.Frâncu LL. Legal and ethical problems in dental medicine. Rom J Bioeth. 2009;7:157–62. [Google Scholar]
- 27.Thompson DF. Understanding financial conflicts of interest. N Engl J Med. 1993;329:573–6. doi: 10.1056/NEJM199308193290812. [DOI] [PubMed] [Google Scholar]
- 28.Parsapoor A, Mohammad K, Malek Afzali H, Ala'eddini F, Larijani B. Observance of patient's rights: A Survey on the views of patients, nurses, and physicians. J Med Ethics Hist Med. 2012;5:5. [PMC free article] [PubMed] [Google Scholar]
- 29.Kemparaj V, Panchmal GS. Qualitative assessment of ethical issues in dental practice: An expert opinion. J Educ Ethics Dent. 2016;6:20–6. [Google Scholar]
- 30.Daniel JS. Michigan Dental Association Annual Session. Conference. 2009 [Google Scholar]
- 31.Singer PA, Pellegrino ED, Siegler M. Clinical ethics revisited. BMC Med Ethics. 2001;2:E1. doi: 10.1186/1472-6939-2-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tai MC, Lin CS. Developing a culturally relevant bioethics for Asian people. J Med Ethics. 2001;27:51–4. doi: 10.1136/jme.27.1.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jafarey AM, Farooqui A. Informed consent in the Pakistani milieu: The physician's perspective. J Med Ethics. 2005;31:93–6. doi: 10.1136/jme.2002.002220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kotrashetti VS, Kale AD, Hebbal M, Hallikeremath SR. Informed consent: A survey of general dental practitioners in Belgaum city. Indian J Med Ethics. 2010;7:90–4. doi: 10.20529/IJME.2010.031. [DOI] [PubMed] [Google Scholar]
- 35.Dable RA, Prasanth M, Singh SB, Nazirkar GS. Is advertising ethical for dentists? An insight into the Indian scenario. Drug Healthc Patient Saf. 2011;3:93–8. doi: 10.2147/DHPS.S25708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Santos Pacheco KT, Silva Junior MF, Meireles NR. Ethical proceedings against dentists in espírito santo for infringements to the code of dental ethics. Braz Oral Res. 2014;28 pii: S1806-83242014000100219. [PubMed] [Google Scholar]
- 37.Şahinkesen G. Identification of daily bioethical dilemmas in Turkish dentists. Gulhane Medical Journal. 2009;51:141–4. [Google Scholar]


