Abstract
Objective:
This study aimed to assess the relationship between religiosity and quality of life (QoL) in patients with breast cancer in a Muslim population.
Methods:
This descriptive-correlational study was conducted in 84 Muslim patients with breast cancer who were admitted to Ahvaz Shafa Hospital, Iran, during 2015. QoL and religiosity were measured with the Short Form-36 questionnaire and Muslim Religiosity questionnaire based on the Glock and Stark model, respectively. Data were analyzed using a software program for descriptive statistics, the Chi-square test, Pearson's correlation, and an independent sample t-test.
Results:
Most patients had high religiosity (69%) and moderate QoL (46.5%) scores. Total scores and all subscales scores for QoL were significantly higher in patients with high religiosity than patients with moderate religiosity (P < 0.0001). Moreover, a direct correlation was found between religiosity (total and all subscales) and QoL (total and all subscales) (P < 0.0001).
Conclusions:
A significant relationship was found between religiosity and QoL in patients with breast cancer. Accordingly, care team members, especially midwifery and nursing staff, should pay more attention to religious beliefs among these patients to improve their QoL.
Keywords: Breast neoplasms, Iran, Islam, palliative care, quality of life, religion

Introduction
Breast cancer is the leading cause of oncological death in women.[1] The incidence rate of breast cancer is increasing, both in developed and developing countries.[2] In the Islamic Republic of Iran, a developing country, breast cancer has been the most prevalent cancer among women in the past few decades, with a rising incidence and mortality rate.[3,4] Based on the last national cancer registry report in Iran, the incidence of breast cancer increased from 16.0 to 28.3/100,000 from 1995 to 2010, and the general mortality rate increased during 2003–2009 from 0.96 to 4.33/100,000.[3] Moreover, the projected incidence of breast cancer in Iranian women in 2020 is 63.0/100,000.[4] In Khuzestan province, in the southwest of Iran, a high incidence rate of breast cancer has been reported in recent years.[5,6]
In spite of considerable progress in diagnosis, treatment, care, and outcomes in the last decade, breast cancer negatively influences women's quality of life (QoL), due to psychosocial issues and physical symptoms, and particularly the adverse effects of systemic adjuvant therapy (chemotherapy).[7,8] Recent studies showed poor to moderate QoL in patients with breast cancer, not only after initial treatment (1–2 years) but also long after treatment (>5 years).[9,10] Therefore, there is an urgent need to improve the QoL in patients with breast cancer.[11]
Palliative care, defined as an approach that improves the QoL of patients and families facing life-threatening disease through prevention or early identification and treatment, is a key intervention for women living with breast cancer.[12] Religiosity is an essential component of palliative care that has attracted increasing interest in recent years among cancer patients, especially those with breast cancer.[13,14] Religiosity is an expression of spirituality and is defined as a set of beliefs and practices associated with a particular religious tradition or denomination.[15] Associations between religiosity and QoL in patients with breast cancer have been discussed in different cultures, with conflicting results. Some studies have indicated that religiosity has a heightened role in improvement of women's QoL.[16,17,18] However, others reported no association between religiosity and QoL,[19,20] or only found an association in some dimensions of QoL.[21,22,23]
In Iranian patients with breast cancer, recent investigations related to religiosity and QoL have focused on religious coping strategies or qualitative design,[18,24,25] and the relationship between religiosity and QoL has not been well-investigated among this population to date in a prospective manner, using specific measures. Therefore, considering that religiosity is different across various cultures and due to the contradictory results of previous research regarding the relationship between religiosity and QoL in patients with breast cancer, we decided to assess the relationship between these variables in a population of Iranian Muslims with breast cancer.
Methods
This descriptive–correlational study was conducted in Muslims patients with breast cancer who were admitted to Ahvaz Shafa Hospital, Iran, from May to December 2015. Inclusion criteria were as follows: (1) cancer diagnosis for at least 1 year; (2) cognitive understanding about cancer prognosis; (3) mental and physical ability to complete the questionnaires; and (4) under treatment with surgery, radiotherapy, or chemotherapy. Patients who had chronic diseases (i.e. diabetes, renal failure, and other types of cancer) were excluded from the study.
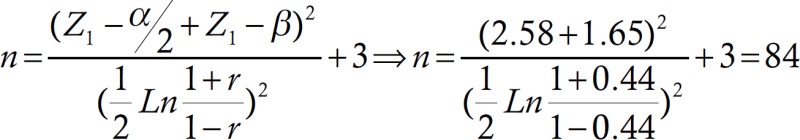
To estimate the sample size, with a confidence level of 99%, β = 0.1, and r = 0.44,[26] the number of needed samples was calculated as 84 patients based on the following formula. A sequential sampling method was used to identify the patients.
A sociodemographic and clinical characteristics checklist, developed at the Department of Midwifery of Jundishapur University of Medical Sciences, Ahvaz, Iran, was administered to record demographic and clinical variables, including the age, marital status, education, religion, occupation, income, age at cancer onset, total duration of cancer, and details of treatment.
Religiosity was measured with Serajzadeh's Muslim Religiosity questiossnnaire, based on the Glock and Stark model. This scale is comprised of 26 questions with 4 subscales as follows: (1) believing; (2) emotional; (3) consequential; and (4) ritualistic. The scale is scored based on a 5-point Likert method (4 = totally agree, 3 = agree, 2 = somewhat agree, 1 = disagree, and 0 = totally disagree). Total scores range from zero to 104, with a higher score indicating higher religiosity. Depending on the mean and standard deviation (SD), the religiosity status is categorized as: low (<26), moderate (26–78), or high (more than 78). This scale is one of the most reliable tools for assessment of Muslim religiosity, and its reliability and validity were previously confirmed in Iran.[27,28] In the present study, the face and content validity of the scale were confirmed using inter-rater agreement for 10 patients and faculty members of the Midwifery Department of Jundishapur University of Medical Sciences, Ahvaz, Iran. For internal consistency, the reliability of the total score was 0.867; subscale scores ranged from 0.309–0.726, showing good reliability.
The 36-item Short Form Survey (SF-36) was used to measure QoL. The SF-36 is a generic, 36-item questionnaire that was developed in the USA to survey health status in the medical outcomes study.[29] The survey is divided into 8 subscales as follows: (1) physical functioning; (2) role limitations due to physical health problems; (3) bodily pain; (4) general health; (5) vitality; (6) social functioning; (7) role limitations due to emotional problems; and (8) mental health. Subscale scores range from 0 to 100. Total scores range from 0 to 800, with higher scores reflecting better QoL. To compare QoL scores, we categorized total QoL status into 3 distinct level as: low (<400), moderate (400–600), or high (600 or more). All 8 subscales have been shown to be reliable and to have adequate construct validity in Iran and among patients with breast cancer.[30,31]
First, clinical and sociodemographic details were obtained by interviewing the patients and their families, and by reviewing treatment records. Then, eligible patients were asked to go to the counseling room. All items of the religiosity and SF-36 questionnaires were read to the patients by an interviewer to make sure that they understood the questions because some patients were illiterate and had limited education. To avoid distraction by the interviewer, another researcher filled out the questionnaires.
This study was approved by the Research Ethics Board of Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran (code No. ajums. REC.1393.419). After obtaining an introduction letter from this committee and representing it to a Hospital Manager, the researcher was referred to the recruitment center and selected patients who met the inclusion criteria. At first, each patient was assessed by a physician in the recruitment center to verify her current status. Once a patient met the study inclusion criteria, written informed consent was obtained after a brief verbal description of the study was presented. All patients were assured that the personal information would be anonymous and confidential, and all were informed that they had the right to refuse to participate in the study.
For statistical analysis, SPSS software version 20 (SPSS, Inc., Chicago, IL, USA) was applied. Descriptive statistical tests (mean, SD, numbers, and percent) were used for demographic and clinical characteristics. The Kolmogorov–Smirnov test was used for normal distribution testing. Student's t-test was used to assess differences in QoL between the groups according to the degree of religiosity. Pearson's test was used to assess correlations of religiosity with QoL and of demographic and clinical characteristics with religiosity and QoL.
Results
A total of 84 patients participated in the study. The mean ± SD of patient age was 54.71 ± 10.46 years. All patients were married and living with their spouses, and mean ± SD of marriage age was 22.67 ± 3.06 years. All patients belonged to the Shia religion and most (95.2%) were housewives. Most patients (84.5%) were illiterate and few (2.4%) achieved graduate level or higher. Regarding income status, 47 patients (56%) had moderate income (5000,000–10,000,000 RLs) and 37 (44%) had low income (<5000,000 RLs). The mean ± SD of the total duration of cancer and age of cancer onset were 4.61 ± 1.41 years and 49.22 ± 11.22 years, respectively.
Of 84 patients, 58 (69%) and 26 (31%) had high and moderate religiosity, respectively. Mean and SD of total score and subscale scores of patient religiosity are presented in Table 1. Among sociodemographic and clinical characteristics, the results of Pearson's test indicated a strongly negative correlation between religiosity and total duration of cancer (r = −0.3, P = 0.003).
Table 1.
Mean and SD of patents’ religiosity using Glock and Stark's scale
| Variables | Status Mean±SD | ||
|---|---|---|---|
| Moderate (n=26) | High (n=58) | Total (n=84) | |
| Believing subscale | 20.1±1.96 | 26.63±1.7 | 24.6±3.5 |
| Emotional subscale | 19.1±2.4 | 22.6±1.6 | 21.59±2.5 |
| Consequential subscale | 18.2±2.27 | 21.08±1.96 | 20.2±2.43 |
| Ritualistic subscale | 12.5±2.4 | 15.9±2.7 | 14.9±3.08 |
| Total | 70.03±5.4 | 86.63±4.7 | 81.5±9.1 |
Regarding QoL, 8 (9.5%), 39 (46.5%), and 37 (44%) patients had low, moderate, and high status, respectively. Mean and SD of total and subscale scores of patient QoL are shown in Table 2. The results of Pearson's test indicated a moderate negative correlation between QoL and age (r = −0.51, P < 0.0001), as well as total duration of cancer (r = −0.49, P < 0.0001). In addition, a weak, direct but significant relationship existed between QoL and income (r = 0.27, P < 0.0001) and education (r = 0.28, P < 0.0001).
Table 2.
Mean and SD of patients’ QoL using SF-36 questionnaire
| Variables | Status Mean±SD | |||
|---|---|---|---|---|
| Low (n=8) | Moderate (n=39) | High (n=37) | Total (n=84) | |
| General health subscale | 55.62±13.21 | 70.2±4.2 | 77.43±7.1 | 73.02±9.2 |
| Physical functioning subscale | 60±6.5 | 73.4±9.7 | 82.7±9.6 | 76.25±11.6 |
| Role limitations due to physical health problems subscale | 55±7.07 | 76.2±7.4 | 87.5±9.8 | 79.2±12.7 |
| Role limitations due to emotional problems subscale | 61.8±9.9 | 75.7±8.6 | 91.4±7.8 | 81.3±12.8 |
| Social functioning subscale | 60±9.2 | 74.2±8.8 | 86.8±8.7 | 78.4±12.1 |
| Bodily pain subscale | 57.8±8.2 | 83.3±10.5 | 95.6±6.1 | 86.3±13.9 |
| Vitality subscale | 59.3±8.2 | 69.1±5.1 | 81.8±7.3 | 73.8±10.04 |
| Mental health subscale | 63.2±8.3 | 73.2±5.1 | 83.2±5.2 | 76.7±8.5 |
| Total | 473.4±38.1 | 597.5±36.2 | 687.3±31.5 | 625.2±73.9 |
A comparison of QoL in patients with high and moderate religiosity is shown in Table 3. Based on Student's t-test, QoL (total and all subscales) was significantly higher in patients with high religiosity status compared to patients with moderate religiosity status (P < 0.0001). Pearson's test showed a direct correlation between QoL (total and all subscales) and religiosity (total and all subscales) (P < 0.0001) [Table 4].
Table 3.
Comparison of patients’ QoL in groups with high and moderate religiosity status
| QoL variables | Religiosity status Mean±SD | P † | |
|---|---|---|---|
| Moderate (n=58) | High (n=26) | ||
| General health subscale | 62.42±9.6 | 75.43±6.7 | <0.0001 |
| Physical functioning subscale | 67.69±9.9 | 80.08±10.28 | <0.0001 |
| Role limitations due to physical health problems subscale | 68.84±12.02 | 83.87±10.1 | <0.0001 |
| Role limitations due to emotional problems subscale | 69.89±9.6 | 86.5±10.6 | <0.0001 |
| Social functioning subscale | 67.4±9.9 | 83.4±9.5 | <0.0001 |
| Bodily pain subscale | 75.76±15.1 | 91.03±10.4 | <0.0001 |
| Vitality subscale | 65.96±7.07 | 77.32±9.1 | <0.0001 |
| Mental health subscale | 69.6±8.01 | 79.89±6.7 | <0.0001 |
| Total | 549.6±60.8 | 659.2±50.4 | <0.0001 |
†Obtained from independent samples t-test
Table 4.
Correlation of patients’ QoL and religiosity in patients with breast cancer
| Religiosity variables QoL variables | Believing subscale | Emotional subscale | Consequential subscale | Ritualistic subscale | Total |
|---|---|---|---|---|---|
| General health subscale |
r=0.53 P<0.0001 |
r=0.48 P<0.0001 |
r=0.42 P<0.0001 |
r=0.37 P<0.0001 |
r=0.57 P<0.0001 |
| Physical functioning subscale |
r=0.49 P<0.0001 |
r=0.46 P<0.0001 |
r=0.40 P<0.0001 |
r=0.17 P<0.0001 |
r=0.49 P<0.0001 |
| Role limitations due to physical health problems subscale |
r=0.52 P<0.0001 |
r=0.48 P<0.0001 |
r=0.39 P<0.0001 |
r=0.33 P<0.0001 |
r=0.55 P<0.0001 |
| Role limitations due to emotional problems subscale |
r=0.63 P<0.0001 |
r=0.58 P<0.0001 |
r=0.41 P<0.0001 |
r=0.35 P<0.0001 |
r=0.63 P<0.0001 |
| Social functioning subscale |
r=0.63 P<0.0001 |
r=0.54 P<0.0001 |
r=0.43 P<0.0001 |
r=0.40 P<0.0001 |
r=0.63 P<0.0001 |
| Bodily pain subscale |
r=0.51 P<0.0001 |
r=0.41 P<0.0001 |
r=0.35 P<0.0001 |
r=0.29 P<0.0001 |
r=0.52 P<0.0001 |
| Vitality subscale |
r=0.53 P<0.0001 |
r=0.54 P<0.0001 |
r=0.33 P<0.0001 |
r=0.37 P<0.0001 |
r=0.59 P<0.0001 |
| Mental health subscale |
r=0.51 P<0.0001 |
r=0.56 P<0.0001 |
r=0.41 P<0.0001 |
r=0.32 P<0.0001 |
r=0/59 P<0.0001 |
| Total |
r=0.69 P<0.0001 |
r=0.64 P<0.0001 |
r=0.46 P<0.0001 |
r=0.39 P<0.0001 |
r=0.71 P<0.0001 |
All P value obtained by Pearson correlation test
Discussion
This study examined the relationship between religiosity and QoL in patients with breast cancer in an Iranian Muslim community. The study results showed a direct correlation between total score and subscale scores on the Muslim Religiosity questionnaire and total score on the SF-36 questionnaire and scores on all subscales. QoL (total and all subscales) was significantly higher in patients with high religiosity status compared to patients with moderate religiosity status.
A growing body of literature has evaluated the role of religiosity in QoL of patients with breast cancer in different cultures using different methodologies, with conflicting results. The present findings support previous studies that indicated a direct or positive relationship between religiosity and QoL in patients with breast cancer.[16,17,18] In accordance with our findings, a similar study by Zamanian et al. in Iranian Muslims with breast cancer, using the Brief Religious Coping and Functional Assessment of Cancer Therapy-Breast (FACT-B) instruments, showed that positive religious coping was associated with improved QoL, whereas negative religious coping was significantly associated with worse QoL.[18] A prospective longitudinal study among Korean women with breast cancer by Jang et al. indicated that the duke religious index scores of Protestant respondents were significantly and positively correlated with scores of the European Organization for Research and Treatment of Cancer QoL (EORTC QLQ-C30) questionnaire at 1 year after surgery.[16] In another study by Aukst-Margetić et el., in Zagreb, Croatia, moderate or poor religiosity based on the Santa Clara Strength of Religious Faith questionnaire was associated with perception of worse physical health, as measured by the International Breast Cancer Study Group QoL questionnaire.[17] Despite the differences in methodology and cultures, all studies are in accordance with our findings.
In contrast with our results, some studies reported no association between religiosity and QoL.[19,20] Manning–Walsh studied patients with breast cancer in the USA, and reported that religiosity measured with the Religious Support Scale was not directly related to QoL measured with the Functional Assessment of Chronic Illness Therapy-Spiritual Well-being 12 (FACIT-SP12) scale.[19] In addition, Purnell et al., in New York State, found that religious practice, assessed with the Social Network Index, was not significantly associated with QoL measured with the SF-36 among survivors of breast cancer.[20] In contrast to our findings, most previous studies have not indicated a positive association between religiosity and QoL in all dimensions.[21,22,23] In a recent study in Ibadan, Nigeria, Elumelu et al. found a significant difference between patients who used religious coping (assessed with the B-COPE questionnaire) and those who did not, in the overall QoL (assessed with the FACIT-SP12); however, no difference was found in physical-well-being dimensions.[22] Among Korean-American and Korean breast cancer survivors, Lim and Yi reported that religiosity, assessed with a 6-item scale adapted from the spiritual well-being subscale of the QoL-Cancer Survivor (QOL-CS) scale, was only significantly related to the general health perception domain of QoL evaluated with the SF-36 questionnaire.[23] Wildes et al. studied breast cancer survivors in the USA, and found no significant correlations between emotional well-being and physical well-being subscales of the Functional Assessment of Cancer Therapy-General (FACT-G) and religiosity, measured with the Systems of Belief Inventory-15 Revised.[21] The discrepancy in the findings may be attributed to using different measures of religiosity and QoL and reliance on cross-sectional designs, given the various definitions used for religiosity, the time of assessment during the course of the disease, and failing to incorporate cultural diversity in measures and designs.
However in recent decades, a variety of evidence has shown a relationship between religiosity and QoL, but the mechanism underlying this relationship is unclear. One review suggested that religiosity was associated with behavioral, physiological, psychological, and social support mechanisms that can mitigate the severity of cancer symptoms.[15] Results of recent studies have shown that patients with breast cancer adjust to life-threatening illnesses by holding onto hope, compensating for losses, and actively maintaining their personal lives through a process of experiential learning. This learning process allowed patients to create or discover opportunities that might lead to maintaining or gaining some enjoyment of life, even as suffering continued during their cancer and recovery.[24,32]
Based on our results and the importance of QoL in palliative treatment, and due to its beneficial effects on health outcomes in patients with breast cancer, it is imperative to gain insight into religious care as a substantial component of holistic care. Therefore, health-care professionals, especially nurses and midwives, should pay more attention to patients with breast cancer and assess the role of religiosity in developing personalized plans of care as they accompany these patients throughout the cancer journey. These professionals should also nurture and support their own religiosity, to be available as a religious resource for their clients and to better recognize, understand, and attend to their clients’ religious needs and concerns.
The study had some limitations that should be considered. First, the cross-sectional design made it impossible to establish causality between religiosity and QoL. Second, this study was conducted in a Muslim population, whose religion may differ considerably from that in other countries. Therefore, to fully understand the role of religiosity in QoL of patients with breast cancer, future studies are needed. In addition, use of longitudinal and randomized controlled trial designs and specific questionnaires are suggested.
Conclusion
A significant relationship was found between religiosity and QoL in patients with breast cancer. Thus, religiosity should be considered in palliative care of breast cancer patients, especially by midwifery and nursing staff.
Financial support and sponsorship
This study was adopted from MSc thesis that was supported by Ahvaz Jundishapur University of Medical Sciences, Iran (Grant No. N.M000149).
Conflicts of interest
There are no conflicts of interest.
References
- 1.Liu FC, Lin HT, Kuo CF, See LC, Chiou MJ, Yu HP, et al. Epidemiology and survival outcome of breast cancer in a nationwide study. Oncotarget. 2017;8:16939–50. doi: 10.18632/oncotarget.15207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.da Costa Vieira RA, Biller G, Uemura G, Ruiz CA, Curado MP. Breast cancer screening in developing countries. Clinics (Sao Paulo) 2017;72:244–53. doi: 10.6061/clinics/2017(04)09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sharifian A, Pourhoseingholi MA, Emadedin M, Rostami Nejad M, Ashtari S, Hajizadeh N, et al. Burden of breast cancer in Iranian women is increasing. Asian Pac J Cancer Prev. 2015;16:5049–52. doi: 10.7314/apjcp.2015.16.12.5049. [DOI] [PubMed] [Google Scholar]
- 4.Zahmatkesh B, Keramat A, Alavi N, Khosravi A, Kousha A, Motlagh AG, et al. Breast cancer trend in Iran from 2000 to 2009 and prediction till 2020 using a trend analysis method. Asian Pac J Cancer Prev. 2016;17:1493–8. doi: 10.7314/apjcp.2016.17.3.1493. [DOI] [PubMed] [Google Scholar]
- 5.Amoori N, Mirzaei M, Cheraghi M. Incidence of cancers in Kuzestan province of Iran: Trend from 2004 to 2008. Asian Pac J Cancer Prev. 2014;15:8345–9. doi: 10.7314/apjcp.2014.15.19.8345. [DOI] [PubMed] [Google Scholar]
- 6.Karami K, Cheraghi M, Amori N, Pedram M, Sobhani A. Common cancers in Khuzestan province, South West of Iran, during 2005-2011. Asian Pac J Cancer Prev. 2014;15:9475–8. doi: 10.7314/apjcp.2014.15.21.9475. [DOI] [PubMed] [Google Scholar]
- 7.Li J, Humphreys K, Eriksson M, Dar H, Brandberg Y, Hall P, et al. Worse quality of life in young and recently diagnosed breast cancer survivors compared with female survivors of other cancers: A cross-sectional study. Int J Cancer. 2016;139:2415–25. doi: 10.1002/ijc.30370. [DOI] [PubMed] [Google Scholar]
- 8.Schoormans D, Czene K, Hall P, Brandberg Y. The impact of co-morbidity on health-related quality of life in breast cancer survivors and controls. Acta Oncol. 2015;54:727–34. doi: 10.3109/0284186X.2014.998277. [DOI] [PubMed] [Google Scholar]
- 9.Ng CG, Mohamed S, See MH, Harun F, Dahlui M, Sulaiman AH, et al. Anxiety, depression, perceived social support and quality of life in Malaysian breast cancer patients: A 1-year prospective study. Health Qual Life Outcomes. 2015;13:205. doi: 10.1186/s12955-015-0401-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kamińska M, Ciszewski T, Kukiełka-Budny B, Kubiatowski T, Baczewska B, Makara-Studzińska M, et al. Life quality of women with breast cancer after mastectomy or breast conserving therapy treated with adjuvant chemotherapy. Ann Agric Environ Med. 2015;22:724–30. doi: 10.5604/12321966.1185784. [DOI] [PubMed] [Google Scholar]
- 11.Zdenkowski N, Tesson S, Lombard J, Lovell M, Hayes S, Francis PA, et al. Supportive care of women with breast cancer: Key concerns and practical solutions. Med J Aust. 2016;205:471–5. doi: 10.5694/mja16.00947. [DOI] [PubMed] [Google Scholar]
- 12.Eng LG, Dawood S, Dent R. Palliative systemic therapy for young women with metastatic breast cancer. Curr Opin Support Palliat Care. 2015;9:301–7. doi: 10.1097/SPC.0000000000000163. [DOI] [PubMed] [Google Scholar]
- 13.Abou Kassm S, Hlais S, Khater C, Chehade I, Haddad R, Chahine J, et al. Depression and religiosity and their correlates in Lebanese breast cancer patients. Psychooncology. 2017 Jan 26; doi: 10.1002/pon.4386. doi: 10.1002/pon. 4386. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 14.Gall TL, Bilodeau C. “Why me?” – Women's use of spiritual causal attributions in making sense of breast cancer. Psychol Health. 2017;32:709–27. doi: 10.1080/08870446.2017.1293270. [DOI] [PubMed] [Google Scholar]
- 15.Ahmadi Z, Darabzadeh F, Nasiri N, Askari M. The effects of spirituality and religiosity on well-being of people with cancer: A literature review on current evidences. Jundishapur J Chronic Dis Care. 2015;4:e28386. [Google Scholar]
- 16.Jang JE, Kim SW, Kim SY, Kim JM, Park MH, Yoon JH, et al. Religiosity, depression, and quality of life in Korean patients with breast cancer: A 1-year prospective longitudinal study. Psychooncology. 2013;22:922–9. doi: 10.1002/pon.3083. [DOI] [PubMed] [Google Scholar]
- 17.Aukst-Margetić B, Jakovljević M, Ivanec D, Margetić B, Ljubicić D, Samija M, et al. Religiosity and quality of life in breast cancer patients. Coll Antropol. 2009;33:1265–71. [PubMed] [Google Scholar]
- 18.Zamanian H, Eftekhar-Ardebili H, Eftekhar-Ardebili M, Shojaeizadeh D, Nedjat S, Taheri-Kharameh Z, et al. Religious coping and quality of life in women with breast cancer. Asian Pac J Cancer Prev. 2015;16:7721–5. doi: 10.7314/apjcp.2015.16.17.7721. [DOI] [PubMed] [Google Scholar]
- 19.Manning-Walsh J. Social support as a mediator between symptom distress and quality of life in women with breast cancer. J Obstet Gynecol Neonatal Nurs. 2005;34:482–93. doi: 10.1177/0884217505278310. [DOI] [PubMed] [Google Scholar]
- 20.Purnell JQ, Andersen BL, Wilmot JP. Religious practice and spirituality in the psychological adjustment of survivors of breast cancer. Couns Values. 2009;53:165. doi: 10.1002/j.2161-007x.2009.tb00123.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wildes KA, Miller AR, de Majors SS, Ramirez AG. The religiosity/spirituality of Latina breast cancer survivors and influence on health-related quality of life. Psychooncology. 2009;18:831–40. doi: 10.1002/pon.1475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Elumelu TN, Asuzu CC, Akin-Odanye EO. Impact of active coping, religion and acceptance on quality of life of patients with breast cancer in the department of radiotherapy, UCH, Ibadan. BMJ Support Palliat Care. 2015;5:175–80. doi: 10.1136/bmjspcare-2012-000409. [DOI] [PubMed] [Google Scholar]
- 23.Lim JW, Yi J. The effects of religiosity, spirituality, and social support on quality of life: A comparison between Korean American and Korean breast and gynecologic cancer survivors. Oncol Nurs Forum. 2009;36:699–708. doi: 10.1188/09.ONF.699-708. [DOI] [PubMed] [Google Scholar]
- 24.Sadati AK, Lankarani KB, Gharibi V, Fard ME, Ebrahimzadeh N, Tahmasebi S, et al. Religion as an empowerment context in the narrative of women with breast cancer. J Relig Health. 2015;54:1068–79. doi: 10.1007/s10943-014-9907-2. [DOI] [PubMed] [Google Scholar]
- 25.Rohani C, Abedi HA, Omranipour R, Langius-Eklöf A. Health-related quality of life and the predictive role of sense of coherence, spirituality and religious coping in a sample of Iranian women with breast cancer: A prospective study with comparative design. Health Qual Life Outcomes. 2015;13:40. doi: 10.1186/s12955-015-0229-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jafari N, Farajzadegan Z, Zamani A, Bahrami F, Emami H, Loghmani A, et al. Spiritual well-being and quality of life in Iranian women with breast cancer undergoing radiation therapy. Support Care Cancer. 2013;21:1219–25. doi: 10.1007/s00520-012-1650-1. [DOI] [PubMed] [Google Scholar]
- 27.Serajzadeh SH, Pouyafar MR. Empirical comparison of religiosity measures: Methodological implications of the application of three measures in the same population. Iran J Soc. 2008;8:37–71. [Google Scholar]
- 28.Dehghani-Firoozabadi ES, Mohtashami J, Atashzadeh-Shoorideh F, Nasiri M, Dolatian M, Sedghi S. Correlation between religious attitude and resiliency of women under domestic violence. Glob J Health Sci. 2017;9:199–208. [Google Scholar]
- 29.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–83. [PubMed] [Google Scholar]
- 30.Montazeri A, Goshtasebi A, Vahdaninia M, Gandek B. The short form health survey (SF-36): Translation and validation study of the Iranian version. Qual Life Res. 2005;14:875–82. doi: 10.1007/s11136-004-1014-5. [DOI] [PubMed] [Google Scholar]
- 31.Musarezaie A, Ghasemi TM, Esfahani HN. Investigation the quality of life and its relation with clinical and demographic characteristics in women with breast cancer under chemotherapy. Int J Prev Med. 2012;3:853–9. doi: 10.4103/2008-7802.104856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schreiber JA, Brockopp DY. Twenty-five years later – What do we know about religion/spirituality and psychological well-being among breast cancer survivors? A systematic review. J Cancer Surviv. 2012;6:82–94. doi: 10.1007/s11764-011-0193-7. [DOI] [PubMed] [Google Scholar]


