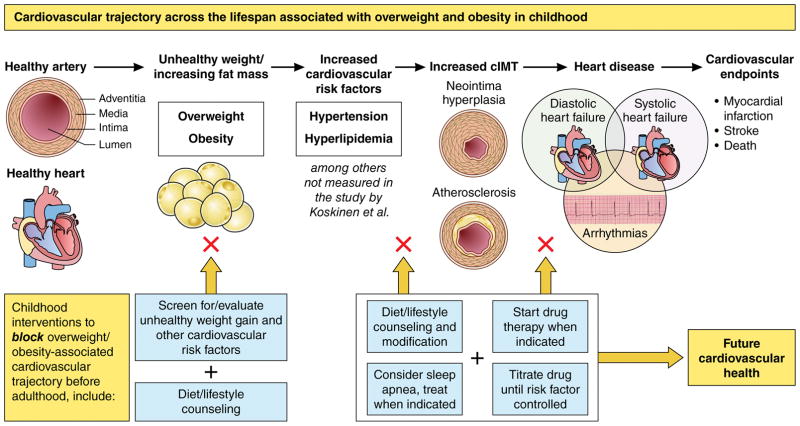
Carotid intima media thickness (cIMT) measured via ultrasound correlates with risk of future cardiovascular events, including myocardial infarction and death1. Thus, researchers use cIMT as an intermediate outcome to denote atherosclerosis in younger populations who would not have time to develop clinical cardiovascular endpoints. In this issue of Circulation2, Koskinen and colleagues use data from the International Childhood Cardiovascular Cohort (i3C) Consortium to identify antecedents in childhood of high cIMT (>90th study-specific percentile) in adulthood. This rich dataset includes 23.4 years of longitudinal follow-up on 2,893 12–18-year-old participants from four studies (Cardiovascular Risk in Young Finns, Childhood Determinants of Adult Health, Bogalusa Heart, and Insulin Studies) across three continents. The combined i3C data show childhood obesity, hypertension, and dyslipidemia in adolescence predict presence of high cIMT in adulthood.
In the analysis, obesity is the risk factor most strongly associated with high cIMT, increasing risk 3.7 (2.0–7.0) fold. This makes sense because adolescent obesity is highly prevalent, very challenging to treat, and strongly associated with obesity and premature mortality in adulthood3. Prevalence of childhood overweight and obesity has nearly tripled in the US since 1988, and rates worldwide have increased 10-fold.4 Short-term weight stabilization or loss is achievable with intensive family-based behavioral approaches, but disturbingly few adolescents with obesity (2%) achieve clinically meaningful treatment responses at three years5. Of even greater concern is the co-occurrence of obesity-related comorbidities: over 60% of adolescents with obesity have additional risk factors such as hypertension or dyslipidemia. These risk factors improve with lifestyle changes and pharmacological treatments. For this reason, pediatric guidelines for weight management, hypertension, and hyperlipidemia recommend treating obesity-related comorbidities with intensive lifestyle counseling coupled with effective pharmacological therapies, when indicated6,7.
Hypertension is strongly linked to obesity, with significant consequences for the heart and vasculature6. Although prevalence of hypertension in US children overall is 3–5%, prevalence among children with obesity is much higher (up to 25%)6. As fat mass increases, so does total blood volume via central (e.g., renin-angiotensin and sympathetic systems) and peripheral mechanisms (e.g., baroreceptors and autonomic dysregulation)8. The resultant increase in stroke volume, cardiac output, systemic vascular resistance, and afterload leads to elevated blood pressure, hypertension, increased left ventricular mass, and left ventricular concentric hypertrophy8. Total blood volume and hypertension increase further in the presence of sleep apnea (present in 55% of adolescents undergoing bariatric surgery6). Repetitive obstructive apneas/hypopneas cause dramatic fluctuations in intrathoracic pressure and blood pressure, increased left ventricular preload, left atrial dilatation, arrhythmias (particularly atrial fibrillation), and left ventricular eccentric hypertrophy8. Together, these changes mechanically stress arterial walls and provoke vascular smooth muscle cells to both proliferate (causing smooth-muscle hypertrophy) and migrate (leading to neointimal hyperplasia), contributing to increased cIMT. In i3C, hypertension was associated with 1.9 (1.3–2.9) fold increased risk of high cIMT. Interestingly, a separate study of children with high cIMT documented that 90% also had left ventricular hypertrophy9. Hypertension and sleep apnea both are treatable with weight loss and disease-specific therapies.
Dyslipidemia in youth—specifically elevated triglycerides and low HDL—is also strongly linked to obesity. Nearly 17% of US adolescents with obesity have abnormal non-HDL cholesterol and severity of obesity correlates with prevalence of high total cholesterol (10% with overweight to 19% with class III obesity), low HDL cholesterol (up to 19% with class III obesity), and high triglycerides (29% with class III obesity)10. In contrast to obesity-related dyslipidemia, the relationship between obesity and LDL cholesterol is less strong. This may partially explain why, in the study by Koskinen et al., adding lipid levels to a model containing obesity, hypertension, and sex minimally improved discrimination of high cIMT risk (AUC increased from 0.698 to 0.717)10. Despite this, LDL cholesterol is a well-established risk factor for atherosclerosis. In lipid disorders where high LDL predominates (e.g., familial hypercholesterolemia [FH]), early detection is critical for initiating pharmacological therapy to reduce the substantial risk for early myocardial infarction7. Numerous studies document that cIMT is both markedly higher in children with FH and reduced by statin therapy7. Thus, the finding that lipids do not greatly improve discrimination of high cIMT risk should not be interpreted as an indication against childhood lipid screening. Lipid screening in children detects both genetic lipid abnormalities (e.g., including FH that affects 1 in 250 individuals) and dyslipidemia that responds favorably to lifestyle modification. For children with obesity, identifying abnormal lipids invigorates dietary counseling, by heightening the immediate importance of dietary changes for cardiovascular health.
Despite recognition that hypertension and dyslipidemia are associated with childhood obesity, these major risk factors are infrequently diagnosed or treated in childhood with potentially dire cardiovascular consequences by young adulthood11, 12. At the time of hypertension diagnosis, 20–40% of children have left ventricular hypertrophy, which correlates with high cIMT in childhood, and is a known antecedent to heart failure6. Children with dyslipidemia also have high cIMT in childhood7. Koskinen and colleagues’ findings build on data from the individual i3C cohorts to demonstrate that hypertension and dyslipidemia in childhood correlate with high cIMT in adulthood. Disturbingly, childhood obesity has been associated with a documented 50% rise in heart-failure incidence among 18–34-year-olds (from 1987–2006), increasing frequency of stroke in young adults, and an 8-fold increased risk of kidney failure13–15. Although it is unclear whether childhood hypertension or hyperlipidemia increase these clinical events, these data caution us to the critical need for improved childhood diagnosis and treatment of overweight/obesity, hypertension, and dyslipidemia.
Unfortunately, despite an estimated 24.5 million US children with obesity and additional cardiovascular risk factors, major barriers exist in identifying and treating obesity, hypertension, and dyslipidemia in childhood5–7,11, 12. Obesity is the easiest of these risk factors to identify, yet the most challenging to durably improve. Healthcare providers report discomfort and inadequate training in communicating about unhealthy weight with patients and families16. Shame and judgement surround obesity at home, in provider offices, and in the community16. This weight stigmatization insidiously undermines the ability of patients and healthcare providers to unite in positive and meaningful dialogue about how to achieve healthy lifestyles and reduce overweight/obesity. Childhood hypertension and dyslipidemia are even more under-recognized due to lack of familiarity with current guideline recommendations, plus complex thresholds for diagnosis, evaluation, and treatment. For example, to determine pediatric hypertension thresholds in <13-year-olds, providers must reference age-, sex-, and height-specific normative tables manually or compute them using websites or electronic health records11,12. Moreover, diagnosis of pediatric hypertension requires that providers identify elevated blood pressures at three separate encounters. This is very difficult for children <13-years old, because each blood pressure needs to be referenced to the percentile-based threshold for the child’s height and age at the time of the blood-pressure measurement. Many of these barriers may be reduced using alerts, decision support, and additional technological advances that maximize the value of electronic health records in healthcare delivery.
Findings from i3C reported by Koskinen et al underscore that obesity, hypertension, and dyslipidemia are three key modifiable risk factors in childhood of high cIMT in adulthood. All can be effectively treated by lifestyle modification and pharmacotherapy. Obesity is the common denominator and driving force behind blood volume, blood pressure, and blood lipid changes that impact vascular health. Thus, lifestyle modification to improve obesity is first-line. If obesity proves unalterable, or blood pressure or cholesterol do not improve using lifestyle modification alone, hypertension and dyslipidemia must be treated using effective guideline-recommended pharmacological approaches. If we can improve our comfort engaging patients and families in health-focused communication about unhealthy weight, increase our rates of screening, diagnosis, and treatment of hypertension and dyslipidemia, and expand our knowledge of guideline-based lifestyle and pharmacological therapies, we can better partner with patients and families to improve their weight, blood pressure, dyslipidemia and future cardiovascular health.
Supplementary Material
Figure 1.
Cardiovascular trajectory across the lifespan associated with overweight and obesity in childhood
References
- 1.Den Ruijter HM, Peters SA, Anderson TJ, Britton AR, Dekker JM, Eijkemans MJ, Engstrom G, Evans GW, de Graaf J, Grobbee DE, Hedblad B, Hofman A, Holewijn S, Ikeda A, Kavousi M, Kitagawa K, Kitamura A, Koffijberg H, Lonn EM, Lorenz MW, Mathiesen EB, Nijpels G, Okazaki S, O’Leary DH, Polak JF, Price JF, Robertson C, Rembold CM, Rosvall M, Rundek T, Salonen JT, Sitzer M, Stehouwer CD, Witteman JC, Moons KG, Bots ML. Common carotid intima-media thickness measurements in cardiovascular risk prediction: a meta-analysis. JAMA. 2013;310:1739. doi: 10.1001/jama.2012.9630. [DOI] [PubMed] [Google Scholar]
- 2.Koskinen Juha, Juonala Markus, Dwyer Terence, Venn Alison, Thomson Russell, Bazzano Lydia, Berenson Gerald S, Sabin Matthew A, Burns Trudy L, Viikari Jorma SA, Woo Jessica G, Urbina Elaine M, Prineas Ronald, Hutri-Kähönen Nina, Sinaiko Alan, Jacobs David, Steinberger Julia, Daniels Stephen, Raitakari Olli T, Magnussen Costan G. Impact of Lipid Measurements in Youth in Addition to Conventional Clinic-Based Risk Factors on Predicting Preclinical Atherosclerosis in Adulthood: The International Childhood Cardiovascular Cohort (i3C) Consortium. Circulation. 2017 doi: 10.1161/CIRCULATIONAHA.117.029726. https://doi.org/10.1161/CIRCULATIONAHA.117.029726 [in press] [DOI] [PMC free article] [PubMed]
- 3.Franks PW, Hanson RL, Knowler WC, Sievers ML, Bennett PH, Looker HC. Childhood obesity, other cardiovascular risk factors, and premature death. N Engl J Med. 2010;362:485–493. doi: 10.1056/NEJMoa0904130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.NCD Risk Factor Collaboration (NCD-RisC) Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet. 2017;390:2627–2642. doi: 10.1016/S0140-6736(17)32129-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Danielsson P, Kowalski J, Ekblom O, Marcus C. Response of severely obese children and adolescents to behavioral treatment. Arch Pediatr Adolesc Med. 2012;166:1103–1108. doi: 10.1001/2013.jamapediatrics.319. [DOI] [PubMed] [Google Scholar]
- 6.Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, Daniels SR, de Ferranti SD, Dionne JM, Falkner B, Flinn SK, Gidding SS, Goodwin C, Leu MG, Powers ME, Rea C, Samuels J, Simasek M, Thaker VV, Urbina EM Subcommittee on screening and management of high blood pressure in children. Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents. Pediatrics. 2017;140:e20171904. doi: 10.1542/peds.2017-1904. [DOI] [PubMed] [Google Scholar]
- 7.Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents; National Heart, Lung, and Blood Institute. Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: summary report. Pediatrics. 2011;128(Suppl 5):S213–S256. doi: 10.1542/peds.2009-2107C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hall JE. Pathophysiology of obesity hypertension. Curr Hypertens Rep. 2000;2:139–147. doi: 10.1007/s11906-000-0073-4. [DOI] [PubMed] [Google Scholar]
- 9.Sorof JM, Alexandrov AV, Cardwell G, Portman RJ. Carotid artery intimal-medial thickness and left ventricular hypertrophy in children with elevated blood pressure. Pediatrics. 2003;111:61–66. doi: 10.1542/peds.111.1.61. [DOI] [PubMed] [Google Scholar]
- 10.Skinner AC, Perrin EM, Moss LA, Skelton JA. Cardiometabolic risks and severity of obesity in children and young adults. N Engl J Med. 2015;373:1307–1317. doi: 10.1056/NEJMoa1502821. [DOI] [PubMed] [Google Scholar]
- 11.Brady TM, Solomon BS, Neu AM, Siberry GK, Parekh RS. Patient-, provider-, and clinic-level predictors of unrecognized elevated blood pressure in children. Pediatrics. 2010;125:e1286–e1293. doi: 10.1542/peds.2009-0555. [DOI] [PubMed] [Google Scholar]
- 12.de Ferranti SD, Rodday AM, Parsons SK, Cull WL, O’Connor KG, Daniels SR, Leslie LK. Cholesterol Screening and Treatment Practices and Preferences: A Survey of United States Pediatricians. J Pediatr. 2017;185:99–105. e2. doi: 10.1016/j.jpeds.2016.12.078. [DOI] [PubMed] [Google Scholar]
- 13.Barasa A, Schaufelberger M, Lappas G, Swedberg K, Dellborg M, Rosengren A. Heart failure in young adults: 20-year trends in hospitalization, aetiology, and case fatality in Sweden. Eur Heart J. 2014;35:25–32. doi: 10.1093/eurheartj/eht278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sultan S, Elkind MS. The growing problem of stroke among young adults. Curr Cardiol Rep. 2013;15:421. doi: 10.1007/s11886-013-0421-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vivante A, Golan E, Tzur D, Leiba A, Tirosh A, Skorecki K, Calderon-Margalit R. Body mass index in 1.2 million adolescents and risk for end-stage renal disease. Arch Intern Med. 2012;172:1644–1650. doi: 10.1001/2013.jamainternmed.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pont SJ, Puhl R, Cook SR, Slusser W Section on Obesity, Obesity Society. Stigma Experienced by Children and Adolescents With Obesity. Pediatrics. 2017;140:e20173034. doi: 10.1542/peds.2017-3034. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.