Abstract
Objectives
To determine whether historical neighborhood poverty measures are associated with mothers’ reports of their children’s sleep duration and to compare results from historical neighborhood poverty measures to contemporaneous measures of neighborhood poverty.
Design
The Geographic Research on Wellbeing (GROW) study is a follow-up survey of mothers who gave birth between 2003-2007. GROW mothers assessed their own and their children’s health and health behaviors 5-10 years later (2012-2013).
Setting
Urban Californian counties.
Participants
GROW respondents.
Measurements
We categorized children’s sleep as adequate or inadequate using clinical age-specific guidelines and based on mothers’ reports of their child’s sleep duration. We conducted a latent class analysis to identify historical poverty classes for all California census tracts using data from 1970 to 2005-2009, and we categorized current neighborhood poverty based on data from 2005-2009 only. We then assigned children to different neighborhood exposure classes based on their neighborhood of residence at birth and follow-up.
Results
Logistic models indicated that net of controls for demographics, child behavior and health characteristics, mother characteristics, and household socioeconomic status, children who grew up in historically low (OR: 0.64, 95% CI = 0.45-0.92) or historically moderate poverty classes (OR: 0.68, 95% CI = 0.48-0.98) had lower odds of inadequate sleep duration compared with children who grew up in historically high poverty. We show that the historical specification of neighborhood poverty remained significant despite controls while contemporaneous measures of neighborhood poverty did not.
Conclusions
Our findings indicate strong associations between historical neighborhood poverty and child sleep duration.
Keywords: Neighborhoods, Sleep, Children, Poverty, California
Introduction
Mounting evidence stresses the critical importance of quality sleep for children and adolescents1. Indeed, empirical research has found that lower quality or shorter duration sleep is associated with worse physical2,3, behavioral4–6, emotional7, and academic8 outcomes for children. The influence of sleep on developmental outcomes is not surprising given that other research stresses the importance of sleep for neurological connectivity and physical development9. As lower quality sleep is disproportionately concentrated among economically and socially disadvantaged children10 and leads to numerous detrimental outcomes, lower quality sleep among disadvantaged children could be an important mechanism whereby lifelong social inequality is reproduced.
Like the consequences of sleep, the individual determinants of sleep for children are relatively well documented and include factors such as age, socioeconomic status, race/ethnicity, BMI, daily routine, stress, physical activity, and screen time10,11–14. However, comparably less attention has been given to how neighborhoods may influence sleep for children. This omission is important because of the broad influences, both direct and indirect, that can occur through the characteristics of the surrounding neighborhood15. That is, neighborhoods can influence sleep through direct factors such as noise and indirect factors such as the ability to be physically active. Indeed, neighborhood factors can dampen or condition other individual or household determinants of sleep. This is especially relevant for neighborhood disadvantage as many threats to sleep are concentrated in disadvantaged neighborhoods. For example, low-income neighborhoods can be stressful environments with high rates of crime16, population density17, noise/air pollution18, and a climate that prompts vigilance to threats and discourages comforting night-time routines, including reading, bathing, and other activities shown to promote healthy sleep19,20.
Critically, the neighborhood factors that may inhibit healthy sleep for children are likely amplified in neighborhoods that have been impoverished for prolonged periods of time. For example, crime and the accompanying stress have become largely confined to specific impoverished neighborhoods over the past few decades21. As the socioeconomic profile of the neighborhood changes, the availability of healthy and unhealthy food changes as well, leaving impoverished neighborhoods with higher concentrations of corner stores and fast food restaurants and lower numbers of grocery stores17. When parks or outdoor areas are available they are slowly degraded22. Therefore, despite having the exact same current level of poverty as measured by a census, a neighborhood that recently became economically impoverished may in fact have lower rates of crime, better access to healthy food, and safer outdoor play areas compared to a neighborhood that has been impoverished for decades. Thus, it may be important to measure a neighborhood’s history of poverty longitudinally, rather than simply measuring a neighborhood’s current level of poverty. Implicitly, capturing neighborhoods’ poverty histories or measuring neighborhood poverty longitudinally acknowledges that neighborhoods, like people, transform dynamically and this facilitates quantifying meaningful dynamic neighborhood processes such as the concentration of poverty23.
In this analysis, we therefore examine how historical or longitudinal latent trajectories of neighborhood poverty spanning four decades are associated with child sleep and compare our results to current measures (or cross-sectional specifications) of neighborhood poverty. We also build on previous research showing that children who grow up in disadvantaged neighborhoods have lower quality sleep15,24 by utilizing multi-wave data, which encapsulates greater levels of exposure to neighborhood conditions than cross-sectional studies allow. We additionally use objective measures rather than subjective reports of neighborhood conditions, as while subjective reports of neighborhood conditions can be predictive of concurrent perceptions of health, conclusions about causal effects are vulnerable to alternative explanations, especially mental health or other dispositional factors25. We finally compare the historical classification of neighborhood poverty to traditionally-employed current measures of neighborhood poverty.
Participants and Methods
Participants
The participants for this investigation came from the Geographic Research on Wellbeing (hereafter GROW) study. GROW was a population-based study conducted in 2012-2013 as a follow up to those surveyed in the California Maternal and Infant Health Assessment (henceforth MIHA) from 2003-2007. MIHA is a statewide annual survey of about 3,500 Californian women who have recently given birth. MIHA focuses on questions about the pregnancy and birth outcomes of a specific child. GROW, conducted 5-10 years after, examines responses to health-related questions regarding the mother and the index child along with questions concerning their experience with certain social factors and their neighborhood. Detailed information regarding the sampling techniques and frame, response rates, methodology and other factors relating to GROW have been published elsewhere26. The survey responses, and georeferenced addresses of the mother from MIHA and GROW constitute the individual measures of our analysis; however, the only variable that uses information from MIHA is the residential location. Originally, GROW sampled 3,016 mothers, but 229 mothers were dropped due to issues with the reported address, such as inaccurate geocodes or moves from California; 49 mothers were dropped due to death of their child, the child living with someone else, or completing the survey regarding a different child, and 18 were dropped due to non-response on questions about their child’s sleep. These criteria led to the analytic sample of 2,720 (90.2% of the original sample) mothers and their children.
Neighborhood-level information came from a latent trajectory analysis conducted on the reported percentage of residents who lived in poverty for every Californian census tract from 1970-2009. More detailed information regarding this analysis has been published elsewhere27 and can be found in Appendix Figure 1 and Appendix Tables 1 and 2. As an overview, the data came from the decennial censuses from 1970-2000, obtained from the neighborhood change database (Geolytics, Inc.), which harmonized census tract boundaries over time. We also used data from the 2005-2009 American Community Survey (ACS). Unfortunately, income/poverty was not collected in the 2010 census. Therefore we chose the 2005-2009 estimates from the ACS to be a midpoint between the two waves and that represents an “average” level of historical poverty in the midpoint of the child’s life, to be consistent with previous research27. Including this measure was important as it allowed us to extend our longitudinal classification of neighborhood poverty histories but before the dependent variable was measured. To examine how current specifications of neighborhood poverty compare to the longitudinal latent class specification, we also used data from the 2005-2009 ACS to analyze the association between current or cross-sectional specifications of poverty (i.e., the percentage of residents in the tract who live in poverty) and child sleep.
Measures
Our dependent variable for this analysis was a dichotomous measure of the mother’s report of their child’s sleep per night on weeknights. Specifically, we used clinically-based consensus recommendations for children’s sleep duration by age28. Children aged 4-5 years were coded as having adequate sleep if they slept 10-13 hours and inadequate sleep if they slept less than 10 or more than 13 hours. Children aged 6-10 were coded as having adequate sleep if they slept 9-12 hours and inadequate sleep if they slept less than 9 or more than 12 hours. For each age group, we coded inadequate sleep as “1” and adequate sleep as “0.” While sleeping for long durations can indicate health problems or lower-quality sleep28, we also performed analyses using alternative specifications, such as defining inadequate sleep as eight or fewer hours for all children, which yielded substantively similar results. Albeit not objective measures of sleep, mothers’ reports of children’s sleep have been shown to have moderately strong concordance with objective measures of sleep duration29,30.
Our key independent variable was designed to measure exposure to the long-term neighborhood poverty trajectories at both time points. We operationalized neighborhoods as census tracts out of convenience and to be consistent with previous research31. We then conducted a latent trajectory analysis that identified three unique historical poverty trajectory classes (see Appendix Figure 1). We linked the geo-referenced addresses of the respondents in these latent class tracts as the focal independent variable in the analysis. As mentioned, this is the only variable that uses information from MIHA: specifically their residential location. Given that the three-class model fit best17,27, we classified tracts into “High- Historical Poverty,” “Moderate-Historical Poverty,” and “Low-Historical Poverty.” Since we had two measures of residential location (baseline (i.e., childbirth), MIHA; follow-up (5-10 years later), GROW), we coded respondents into one of five categories: 1) those that lived in high historical poverty tracts at both time points, i.e., “High-High” (reference), 2) those that lived in moderate historical poverty tracts at both time points, i.e., “Moderate-Moderate”, 3) those that lived in low historical poverty at both time points, i.e., “Low-Low”, 4) those that moved from a high historical or long-term moderate poverty neighborhood to a neighborhood that had less historical poverty, i.e., “Upwardly mobile”, and 5) those that moved from historically low or historically moderate poverty neighborhood to a neighborhood that had greater long-term poverty, i.e., “Downwardly mobile”. While this coding scheme may miss moves between infancy (MIHA) and childhood (GROW), it does account for inter-class mobility between these two time points. The full inter-class mobility distribution is presented in Appendix Table 3. Exposure to these neighborhood circumstances is based on information from MIHA and GROW.
In terms of covariates we included demographic characteristics of the child, all of which are from GROW. Specifically, we included: age measured in years, the child’s gender (girls = reference) and race/ethnicity categorized as: non-Latino white (reference), Latino, Asian/Pacific Islander, Black, and other/multiple. We also included measures of child activity and health. Since previous research has suggested that physical activity is positively associated with sleep13, we included a measure of weekly physical activity based on how many days per week the child was reported to engage in physical activity. Because weight is associated with sleep among children33, we included a variable indicating if the child was above the 85th percentile for his/her age and sex. We also included a measure that indicated if the child was diagnosed with Attention Deficit Disorder.
Moreover, scholars have argued that the determinants of child sleep should be conceptualized at the “family level”34; thus, we added characteristics of the mother and her household. Specifically, we included mother’s age at time of survey, a continuous measure of the number of stressful events experienced by the mother in the past year, and the number of stressful events experienced by the mother during her childhood. We used the sum of the stressful measures as previous research suggests this is the most optimal specification35. We additionally included self-reported measures of the mothers’ sleep measured categorically in hours per night on a weeknight (with five or less as the reference category). We also included categorical measures of household socioeconomic status, which has been tied to child sleep10, specifically: educational attainment coded as less than high school (reference), high school, some college, or college or more. We specified total annual family income from all sources as a categorical variable relative to the federal poverty level: 0-100% (reference), 101-200%, 201-300%, 301-400%, and 400%+. We included marital status as: married (reference), separated/widowed/divorced, and never married. Finally, we measured the type of home lived in as a categorical variable: house (reference), duplex/townhome, apartment complex <10 units, apartment complex 10+ units, and other housing type.
Statistical Analysis
To analyze the association between historical neighborhood poverty trajectories and mothers’ reports of their child’s sleep, we implemented the following protocol. First, we descriptively documented the characteristics of the sample. Next, we fit progressively adjusted logistic regression models predicting inadequate sleep as reported by the mother to test if the association between historical or longitudinal poverty trajectories and sleep was explained by specific sets of controls. Our progressive adjustment strategy was as follows: we began with the bivariate association. In sequential models, we then added 1) child’s demographics, 2) controls for the child’s activity and health, 3) mother’s demographics, stress, and own sleep, and 4) socioeconomic status indicators of the mother and household.
Next, we compared the results from the longitudinal, historical specification of neighborhood poverty to current specifications of neighborhood poverty, using data from the 2005-2009 American Community Survey. In this model, we used four additional specifications including one specification used in previous research27, a specification used by the census to classify poverty status of neighborhoods36, and the tertile/quartile specification of the Californian distribution of tract poverty. We then compared the results from the model that included all the controls, noting the significance of the neighborhood characteristics. As a further sensitivity check we carried out an additional longitudinal classification of tracts from a Hierarchical Ordered Partitioning and Collapsing Hybrid (HOPACH) or cluster model. We utilized this classification technique because it was more flexible in terms of functional form of the trajectories and thus it was more sensitive to shorter-term changes in neighborhood poverty. Extensive details regarding this model and results have been published elsewhere26.
Results
In Table 1 we show the descriptive statistics for the sample of 2,720 children and their households. Almost one quarter of children were reported as getting inadequate sleep for their age (24.3%). In terms of neighborhood residence and mobility, 7.8% lived in High-High historical poverty tracts, 17.9% lived in Moderate-Moderate historical poverty tracts, 59.3% lived in Low-Low historical poverty tracts, 8.9% were upwardly mobile, and 6.1% were downwardly mobile. The children were on average 6.8 years old and a slight majority of the sampled children (51.7%) were boys.
Table 1.
Weighted Descriptive Statistics, Geographic Research on Wellbeing Study, 2012-2013, N=2,720
| Mean/Proportion | SE | |
|---|---|---|
|
|
||
| Mother Reported Child Sleep (Ref=sleeps inadequate amount for age) | ||
| Sleeps Recommended Amount for Age | 75.6% | |
| Does not Sleep Recommended Amount for Age | 24.3% | |
| Neighborhood poverty Historya | ||
| High-High Poverty (Ref) | 7.8% | |
| Moderate-Moderate Poverty | 17.9% | |
| Low-Low Poverty | 59.3% | |
| Upwardly Mobile | 8.9% | |
| Downwardly Mobile | 6.1% | |
| Child Demographics | ||
| Age | 6.8 | 0.0 |
| Gender (Girl = Ref) | ||
| Boy | 51.7% | |
| Child Race/Ethnicity | ||
| White (Ref) | 26.5% | |
| Latino(a) | 49.8% | |
| Asian/PI | 7.3% | |
| Black | 8.6% | |
| Other/Multiple | 7.8% | |
| How Often Child Gets Physical Activity | ||
| 0 days per week (Ref) | 3.7% | |
| 1–2 days per week | 22.3% | |
| 3–4 days per week | 29.3% | |
| 5–6 days per week | 17.1% | |
| Everyday | 27.5% | |
| Child Health Conditions | ||
| Weight above 85th Percentile for age (Ref = not) | 23.0% | |
| Has Attention Deficit Disorder (Ref= does not) | 3.0% | |
| Mother Characteristics | ||
| Age | 37.1 | 0.1 |
| Number of Stressors Past Year | 0.7 | 0.0 |
| Number of Stressors as a Child | 0.9 | 0.0 |
| Hours of Sleep per night (Weeknights) | ||
| Five or Less (Ref) | 9% | |
| Six | 23% | |
| Seven | 35% | |
| Eight | 28% | |
| Nine or more | 5% | |
| Educational Attainment | ||
| Less than High School Degree (Ref) | 17.0% | |
| High School Degree/GED | 18.1% | |
| Some College | 24.3% | |
| College or More | 40.5% | |
| Household Income as Percent of Federal Poverty Level | ||
| 0–100% FPL (Ref) | 26.7% | |
| 101–200% FPL | 18.8% | |
| 201–300% | 10.6% | |
| 301–400% | 9.1% | |
| >400% | 34.8% | |
| Marital Status | ||
| Married/Cohabitating (Ref) | 83.0% | |
| Separated/Divorced/Widowed | 7.2% | |
| Never Married | 9.8% | |
| Current Home Type | ||
| House (Ref) | 67.5% | |
| Duplex/Townhome | 1.9% | |
| Apartment Complex <10 units | 8.9% | |
| Apartment Complex 10+ Units | 8.7% | |
| Other | 13.1% | |
| N = 2,720 | ||
Sources: Geographic Research on Wellbeing Study (GROW), 2012-2013, Maternal and Infant Health Assessment, 2003-2007, 1970-2000 Decennial Censuses, and the 2005-2009 American Community Survey.
Italics indicate: Uses information from the Maternal and Infant Health Assessment.
Table 2 depicts progressively adjusted logistic regression models predicting mothers’ reports of their child’s sleep, specifically children not sleeping the recommended duration for their age, hereafter referred to as inadequate sleep. Model 1 simply documents the bivariate association, in this model, those who lived in Moderate-Moderate (OR: 0.61 95% CI = 0.44-0.85), Low-Low (OR: 0.34 95% CI = 0.25-0.45), or Upwardly Mobile historical poverty tracts (OR: 0.61 95% CI = 0.41-0.90) had significantly lower odds of inadequate sleep than those who lived in High-High historical poverty tracts. Model 2 included controls for the demographic characteristics of the child. Net of these characteristics, the children who lived in Low-Low or Moderate-Moderate historical poverty tracts had significantly lower odds of inadequate sleep (OR: 0.51, 95% CI = 0.37-0.70, OR: 0.65, 95% CI = 0.46-.91, respectively) than those who lived in High-High historical poverty tracts. The non-significant inter-class mobility results, when controls were added, were likely due to small cell sizes. Indeed, of those who were upwardly mobile, the majority (67%) moved from moderate historical poverty tracts to historical low tracts, meaning that only 33% moved out of the historical high poverty neighborhoods. Unfortunately, the small cell sizes of the specific moves preclude a finer analysis. For example, 14 respondents who lived in historical low poverty moved to historical High poverty (see Appendix Table 3). In Model 3, we added controls for children’s physical activity and health conditions. Even net of these controls, the neighborhood poverty trajectories remain significant. The children who lived in Moderate-Moderate historical poverty tracts had lower odds (OR: 0.64, 95% CI = 0.45-0.91) of inadequate sleep than those who lived in High-High tracts and, likewise, the children who lived in Low-Low historical poverty tracts (OR: 0.52, 95% CI = 0.38-0.73).
Table 2.
Odds Ratios from Logistic Regression Models Predicting Not Sleeping Recommended Amount for Age among Children, Geographic Research on Wellbeing Study, 2012-2013, N=2,720.
| Model 1
|
Model 2
|
Model 3
|
Model 4
|
Model 5
|
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| O.R. | (95% CI) | O.R. | (95% CI) | O.R. | (95% CI) | O.R. | (95% CI) | O.R. | (95% CI) | |
| Neighborhood poverty Historya | ||||||||||
| High-High Poverty (Ref) | ||||||||||
| Moderate-Moderate Poverty | 0.61 | (0.44–0.85) | 0.65 | (0.46–0.91) | 0.64 | (0.45–0.91) | 0.65 | (0.45–0.93) | 0.68 | (0.48–0.98) |
| Low-Low Poverty | 0.34 | (0.25–0.45) | 0.51 | (0.37–0.70) | 0.52 | (0.38–0.73) | 0.52 | (0.37–0.73) | 0.64 | (0.45–0.92) |
| Upwardly Mobile | 0.61 | (0.41–0.90) | 0.77 | (0.51–1.15) | 0.77 | (0.51–1.17) | 0.77 | (0.51–1.16) | 0.83 | (0.54–1.27) |
| Downwardly Mobile | 0.75 | (0.49–1.15) | 0.82 | (0.53–1.27) | 0.81 | (0.52–1.26) | 0.76 | (0.48–1.18) | 0.78 | (0.48–1.23) |
| Child Demographics | ||||||||||
| Age | 0.74 | (0.70–0.79) | 0.74 | (0.69–0.79) | 0.74 | (0.69–0.79) | 0.73 | (0.68–0.79) | ||
| Gender (Girl = Ref) | ||||||||||
| Boy | 0.88 | (0.73–1.05) | 0.84 | (0.70–1.01) | 0.84 | (0.70–1.02) | 0.85 | (0.71–1.04) | ||
| Child Race/Ethnicity | ||||||||||
| White (Ref) | ||||||||||
| Latino(a) | 3.02 | (2.27–4.02) | 2.92 | (2.19–3.90) | 2.73 | (2.03–3.67) | 1.97 | (1.42–2.73) | ||
| Asian/PI | 2.46 | (1.62–3.73) | 2.37 | (1.55–3.63) | 2.23 | (1.45–3.42) | 2.34 | (1.51–3.61) | ||
| Black | 4.47 | (3.07–6.50) | 4.25 | (2.90–6.22) | 3.49 | (2.35–5.17) | 2.90 | (1.91–4.39) | ||
| Other/Multiple | 1.35 | (0.86–2.14) | 1.32 | (0.83–2.09) | 1.20 | (0.75–1.91) | 1.12 | (0.70–1.81) | ||
| How Often Child Gets Physical Activity | ||||||||||
| 0 days per week (Ref) | ||||||||||
| 1–2 days per week | 0.50 | (0.31–0.80) | 0.52 | (0.32–0.84) | 0.56 | (0.34–0.91) | ||||
| 3–4 days per week | 0.40 | (0.25–0.64) | 0.41 | (0.26–0.66) | 0.43 | (0.27–0.69) | ||||
| 5–6 days per week | 0.35 | (0.21–0.57) | 0.37 | (0.22–0.61) | 0.41 | (0.24–0.68) | ||||
| Everyday | 0.52 | (0.32–0.83) | 0.52 | (0.32–0.83) | 0.52 | (0.32–0.84) | ||||
| Child Health Conditions | ||||||||||
| Above 85th Percentile for age (Ref = not) | 1.32 | (1.06–1.65) | 1.32 | (1.05–1.66) | 1.31 | (1.04–1.65) | ||||
| Has Attention Deficit Disorder | 1.90 | (1.11–3.25) | 1.75 | (1.00–3.05) | 1.69 | (0.96–2.97) | ||||
| Mother Characteristics | ||||||||||
| Age | 0.99 | (0.97–1.00) | 1.00 | (0.99–1.01) | ||||||
| Number of Stressors Past Year | 1.09 | (1.00–1.18) | 1.04 | (0.96–1.14) | ||||||
| Number of Stressors as a Child | 0.95 | (0.88–1.03) | 0.94 | (0.87–1.01) | ||||||
| Hours of Sleep per night (Weeknights) | ||||||||||
| Five or Less (Ref) | ||||||||||
| Six | 0.89 | (0.64–1.25) | 1.00 | (0.71–1.41) | ||||||
| Seven | 0.60 | (0.43–0.83) | 0.66 | (0.47–0.93) | ||||||
| Eight | 0.52 | (0.37–0.73) | 0.56 | (0.40–0.80) | ||||||
| Nine or more | 0.24 | (0.13–0.44) | 0.25 | (0.14–0.46) | ||||||
| Educational Attainment | ||||||||||
| Less than High School Degree (Ref) | ||||||||||
| High School Degree | 1.19 | (0.89–1.59) | ||||||||
| Some College | 0.94 | (0.68–1.28) | ||||||||
| College or More | 0.52 | (0.36–0.76) | ||||||||
| Household Income as Percent of Federal Poverty Level | ||||||||||
| 0–100% FPL (Ref) | ||||||||||
| 101–200% FPL | 0.95 | (0.71–1.27) | ||||||||
| 201–300% | 0.90 | (0.61–1.31) | ||||||||
| 301–400% | 0.78 | (0.51–1.21) | ||||||||
| >400% | 0.80 | (0.54–1.19) | ||||||||
| Marital Status | ||||||||||
| Married/Cohabitating (Ref) | ||||||||||
| Separated/Divorced/Widowed | 1.37 | (0.95–1.97) | ||||||||
| Never Married | 1.14 | (0.83–1.56) | ||||||||
| Current Home Type | ||||||||||
| House (Ref) | ||||||||||
| Duplex/Townhome | 0.73 | (0.36–1.49) | ||||||||
| Apartment Complex <10 units | 0.85 | (0.60–1.20) | ||||||||
| Apartment Complex 10+ Units | 0.87 | (0.62–1.22) | ||||||||
| Other | 1.12 | (0.85–1.48) | ||||||||
| Constant | 0.69 | (0.52–0.91) | 1.70 | (.95– 3.04) | 3.70 | (1.78–7.70) | 9.59 | (3.79–24.27) | 9.26 | (3.46–24.77) |
| N = 2,720 | ||||||||||
Sources: Geographic Research on Wellbeing Study (GROW), 2012-2013, Maternal and Infant Health Assessment, 2003-2007, 1970-2000 Decennial Censuses, and the 2005-2009 American Community Survey.
Note: Missing data were handled by STATAs multiple imputation suite.
Uses information from the Maternal and Infant Health Assessment.
In Model 4 we included controls for characteristics of the mother: specifically, we included her age, number of recent stressors, number of stressors as a child and the number of average hours of sleep per night of the mother. After controlling for these factors, historical neighborhood poverty was still significantly associated with child sleep: the children who lived in Moderate-Moderate historical poverty tracts had lower odds (OR: 0.65, 95% CI = 0.45-0.93) of inadequate sleep than those who lived in High-High historical poverty tracts. Similarly, children who lived in Low-Low historical poverty tracts (OR: 0.52, 95% CI = 0.37-0.73) had significantly lower odds of inadequate sleep than children who lived in High-High historical poverty tracts.
The fully adjusted model (Model 5) included additional controls for socioeconomic factors, including mothers’ education, household income, marital status, and type of home (apartment, house, duplex, etc.). Even net of these controls, the association between neighborhood type and inadequate sleep remained significant. Indeed, compared to children who lived in High-High poverty neighborhoods, children who lived in Moderate-Moderate historical poverty tracts (OR: 0.68, 95% CI = 0.48-0.98) and children who lived in Low-Low historical poverty tracts (OR: 0.64, 95% CI = 0.45-0.92) had significantly lower odds of inadequate sleep.
Sensitivity Analysis: Current Specifications of Neighborhood Poverty
We next compared the significance of neighborhood coefficients and overall model fit with fully adjusted models predicting inadequate sleep based on different classifications of historical and current neighborhood poverty. The results of this analysis are presented in Appendix Table 4. As mentioned we tested the historical specification of neighborhoods against four different current specifications of neighborhood poverty and one additional longitudinal specification. However, consistent with the longitudinal specification, we allowed inter-class mobility, including upwards and downwards, mobility between MIHA and GROW and tracts for each of the current poverty specifications.
These results show that the only neighborhood measures significantly associated with reports of child sleep, after full adjustment, were the historical specifications. Indeed, the additional historical classification that uses tract classifications from a Hierarchical Ordered Partitioning and Collapsing Hybrid model, yields somewhat similar results as the latent class model. That is, there are significant differences in child sleep for those who lived in the most historically advantaged tracts relative to those who lived in the historically disadvantaged tracts. These results are consistent with the results presented above in that this other longitudinal perspective has significant differences between classes and inadequate child sleep (whereas none of the cross-sectional specifications were significant) but different in that all of the tract classes were not significant relative to the most disadvantaged class. Overall these results provide evidence that current specifications of neighborhood poverty may conceal how neighborhoods influence sleep among children and suggests that researchers use historical data to measure neighborhood disadvantage in relation to child sleep.
Discussion
Adequate sleep is critical for child development outcomes including: academic achievement, social adjustment, and physical well-being1. The relationship between neighborhood factors and sleep during childhood is not as well understood as individual or household determinants of sleep. In this analysis, we examined the association between historical or longitudinal neighborhood poverty trajectories and sleep among a sample of Californian children. We classified neighborhoods by their historical latent poverty trajectories due to the notion that current poverty specifications could be underestimating the influence of neighborhood disadvantage and child sleep, especially in neighborhoods that have been consistently impoverished. Indeed, the proximate and distal pathways through which neighborhoods may negatively influence sleep are likely markedly worse in neighborhoods which have been consistently or historically impoverished. We contributed to previous research that has analyzed the association between neighborhood poverty and sleep among children by taking this historical perspective of neighborhoods, controlling for important confounders, and by using measures of neighborhood at both birth and in childhood to capture neighborhood poverty exposure at two important points in the life course among the sampled children.
Our analysis finds that historical neighborhood poverty trajectories are significantly associated with the mothers’ reports of their child’s sleep. Specifically, children who grew up in neighborhoods with low or moderate historical poverty had significantly lower odds of inadequate sleep durations than those who lived in neighborhoods that experienced high historical poverty during MIHA and GROW. These results are notable given the important controls, including children’s activity levels and health conditions, household socioeconomic status, mothers’ sleep and home type. While the coefficient operated in the expected direction, there was no significant difference between children who were in the “High-High” poverty tracts compared to those who were “Upwardly Mobile,” which is likely due to small cell sizes (please see Appendix Table 3).
Our results also suggest that longitudinal measures of neighborhood poverty are significantly associated with reports of children’s sleep, while contemporaneous specifications of neighborhood poverty are not, at least when important controls are included in multivariate models. These results suggest that a neighborhood’s historical experience of poverty may be more strongly associated with child sleep than the current level of poverty in the neighborhood. The more proximate pathways through which neighborhoods influence sleep such as noise, stress, access to food, access to parks, and crime, are likely markedly worse in neighborhoods which have been consistently impoverished than in neighborhoods which have been consistently advantaged or neighborhoods which recently became impoverished. Thus, longitudinal measures of neighborhood disadvantage may be better equipped to identify the most disadvantaged neighborhoods, and thus the neighborhoods that are worst for sleep.
Of course, this research has important limitations that the reader should consider. These results are only generalizable to urban Californian children. The influence of historical neighborhood poverty trajectories and sleep should be investigated in other settings, especially settings with rural children where the proximate causes of inadequate sleep may differ from those in urban areas. Another limitation is that we used mother-reported measures of child sleep. While these reports have relatively high concordance with objectively measured sleep30,37, objective measures, such as actigraphy would be preferable to reduce measurement error38. However, these examinations are more expensive and intrusive than mother reports, which would have likely limited the sample and thus the generalizability of the results. While having multiple time periods was important, by only having addresses at two-time periods we miss mobility and moves between waves. However, we do have two important periods in our sampled children’s life course. Additionally, while we aimed to explicitly focus on exposure, our specification of exposure to neighborhood tract disadvantage makes it difficult to understand if the disadvantaged neighborhoods are leading to poor sleep, or deciding to remain in those neighborhoods leads to poor sleep. Finally, as with any associational study, it is impossible to know if there are other unmeasurable factors driving the observed association.
Conclusion
In terms of scientific contributions, our analysis contributes to our understanding of 1) the determinants of sleep among children and 2) how the relationship between neighborhood poverty and health measures may differ depending on the time period in which poverty is measured. Specifically, we compared historical measures of neighborhood characteristics to multiple current specifications of neighborhood poverty and found that the historical measures of neighborhood poverty were more strongly associated with child sleep than the current measures. While we faced important limitations, it is also worth noting that two complications of neighborhood research: selection and exposure, are somewhat minimized when analyzing children. Young children have little agency in choosing their neighborhood, thus reducing attributions to selection factors in neighborhood-based associations. Adults can move frequently from home to home and neighborhood to neighborhood, sometimes spending little time in certain neighborhoods and thus gaining proportionally small lifetime exposure to the risks and resources of their immediate surroundings. Future research should analyze which factors within these neighborhoods directly or indirectly generate insufficient sleep of children, with the caveat that without ameliorating the overall poverty, the negative neighborhood impact on sleep will likely remain39. Future research should also analyze if different race/ethnic groups are disproportionately impacted by disadvantaged neighborhoods. Finally, future research should investigate and compare shorter-term neighborhood changes (5-10 years) in disadvantage to longer-term changes in relation to child sleep. To fully understand the importance of neighborhoods for sleep, we argue it is time for a longitudinal perspective with regard to neighborhoods.
Supplementary Material
Acknowledgments
We thank the University of Texas Population Research Center (Grant R24 HD42849) for administrative and computing support; the NICHD Ruth L. Kirschstein National Research Service Award (T32 HD007081-35) and the National Institute of Aging training grant (T32 AG000037) for training support; and the American Cancer Society (RSGT-11-010-01-CPPB) for a grant to C. Cubbin. The contents of this manuscript are solely the responsibility of the authors.
Appendices
Appendix Figure 1 depicts the results of the Latent trajectory analysis of the level of measured poverty in all Californian census tracts from 1970-2009. This Latent analysis identified three unique poverty trajectories: “historical high poverty,” “historical moderate poverty,” and “historical low poverty.” The full results are also presented in Appendix Table 1. It is important to note that in some of the tracts the poverty levels seem somewhat noisy as they vary dramatically from census to census. The latent class analysis can help to sort through the noise and identify latent poverty trajectories from the whole state. Using a multinomial logistic regression model, we found results consistent with the notion that my classification was measuring poverty as percentage renters, percentage with less than a high school education, percentage multi-unit housing, and percentage receiving public assistance all operated in the expected direction (see Appendix Table 2). We show the inter-class mobility of the children between MIHA and GROW (Appendix Table 3). Finally, we show the full results from contemporaneous neighborhood poverty as well as two historical classification schemes (Appendix Table 4).
Appendix Figure 1.
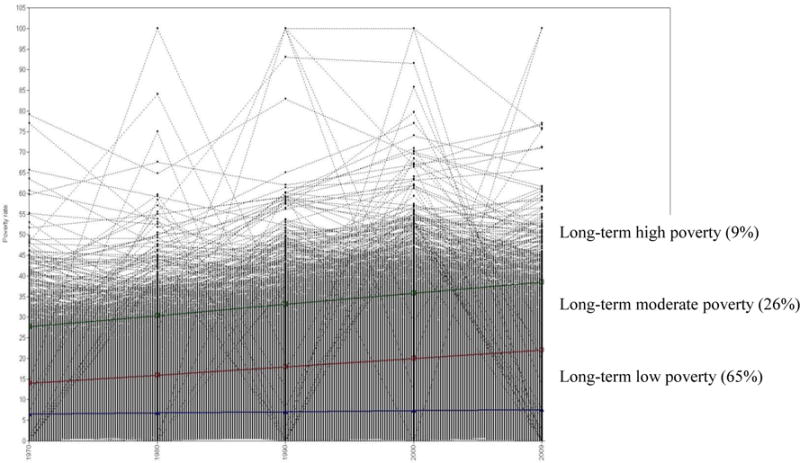
Latent Class Poverty Trajectories for All Californian Census Tracts (1970–2010)
Appendix Table 1.
Latent Class Growth Model Fit Statistics, Census Tract-Level Poverty Trajectories, Californian Census Tracts, 1970-2009.
| BIC | LMR-LRT p-Value | Entropy | |
|---|---|---|---|
|
|
|||
| 2 Class Model | 242,893 | <.001 | 0.947 |
| 3 Class Model | 236,684 | <.001 | 0.912 |
| 4 Class Model | 234,101 | 0.004 | 0.900 |
| 5 Class Model | 233,152 | 0.659 | 0.899 |
| N=7,049 | |||
Sources: 1970-2000 Decennial Censuses, 2005-2009 American Community Survey.
Appendix Table 2.
Multinomial Logistic Regression Models Predicting Latent Poverty Class Affiliation, Californian Census Tracts.
| Historical Low Poverty
|
Historical Moderate Poverty
|
Historical High Poverty (Base Category)
|
|
|---|---|---|---|
| Californian Census Tracts | b | b | |
| Percentage Renter | −0.12 *** | −0.06 *** | |
| Percentage Less than High School | −0.15 *** | −0.06 *** | |
| Percentage Black | −0.06 *** | −0.04 *** | |
| Percentage Multi-Unit | 0.02 *** | 0.00 | |
| Percentage Public Assistance | −0.30 *** | −0.12 *** | |
| Constant | 14.81 *** | 8.41 *** | |
| N | 7,049 | ||
Sources: 1970-2000 Decennial Censuses, 2005-2009 American Community Survey.
Notes: Based on 2000 Census tracts. Missing data handled with Stata’s Multiple Imputation Suite
p < 0.1
p <0.05
p <0.01
p < 0.001.
Appendix Table 3.
Distribution of Historical Poverty Class Inter-class Mobility between MIHA (2003-2007) and GROW (2012-2013).
| GROW | |||||
|---|---|---|---|---|---|
| High Historical Poverty | Moderate Historical Poverty | Low Historical Poverty | Total | ||
| High Historical Poverty | 211 | 46 | 36 | 293 | |
| MIHA | Moderate Historical Poverty | 37 | 487 | 159 | 683 |
| Low Historical Poverty | 14 | 116 | 1,614 | 1,744 | |
| Total | 262 | 649 | 1,809 | 2,720 |
Sources: Geographic Research on Wellbeing Study, 2012-2013, 1970-2000 Decennial Censuses, 2005-2009 American Community Survey.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Connor Sheehan, Department of Sociology and Population Research Center, University of Texas at Austin.
Daniel Powers, Department of Sociology and Population Research Center, University of Texas at Austin.
Claire Margerison-Zilko, Department of Epidemiology and Biostatistics, Michigan State University.
Teresa Mcdevitt, School of Psychological Sciences, University of Northern Colorado.
Catherine Cubbin, School of Social Work and Population Research Center, University of Texas at Austin.
References
- 1.Moran AM, Everhart DE. Adolescent sleep: review of characteristics, consequences, and intervention. Sleep Disord Treat Care. 2015;2012 [Google Scholar]
- 2.Liu J, Hay J, Joshi D, Faught BE, Wade T, Cairney J. Sleep difficulties and obesity among preadolescents. Can J Public Heal Can Santee Publique. 2011:139–143. doi: 10.1007/BF03404163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nielsen L, Danielsen K, Sørensen T. Short sleep duration as a possible cause of obesity: critical analysis of the epidemiological evidence. Obes Rev. 2011;12(2):78–92. doi: 10.1111/j.1467-789X.2010.00724.x. [DOI] [PubMed] [Google Scholar]
- 4.Hansen BH, Skirbekk B, Oerbeck B, Wentzel-Larsen T, Kristensen H. Associations between sleep problems and attentional and behavioral functioning in children with anxiety disorders and ADHD. Behav Sleep Med. 2014;12(1):53–68. doi: 10.1080/15402002.2013.764525. [DOI] [PubMed] [Google Scholar]
- 5.Kamphuis J, Meerlo P, Koolhaas JM, Lancel M. Poor sleep as a potential causal factor in aggression and violence. Sleep Med. 2012;13(4):327–334. doi: 10.1016/j.sleep.2011.12.006. [DOI] [PubMed] [Google Scholar]
- 6.Owens JA. Sleep disorders and attention-deficit/hyperactivity disorder. Curr Psychiatry Rep. 2008;10(5):439–444. doi: 10.1007/s11920-008-0070-x. [DOI] [PubMed] [Google Scholar]
- 7.Silva G, Goodwin J, Parthasarathy S, et al. longitudinal association between short sleep, body weight, and emotional and learning problems in Hispanic and Caucasian children. Sleep. 2011;34(9):1197–1205. doi: 10.5665/SLEEP.1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ravid S, Afek I, Suraiya S, Shahar E, Pillar G. Sleep disturbances are associated with reduced school achievements in first-grade pupils. Dev Neuropsychol. 2009;34(5):574–587. doi: 10.1080/87565640903133533. [DOI] [PubMed] [Google Scholar]
- 9.Kurth S, Achermann P, Rusterholz T, LeBourgeois MK. Development of brain EEG connectivity across early childhood: does sleep play a role? Brain Sci. 2013;3(4):1445–1460. doi: 10.3390/brainsci3041445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.El-Sheikh M, Bagley EJ, Keiley M, Elmore-Staton L, Chen E, Buckhalt JA. Economic adversity and children’s sleep problems: Multiple indicators and moderation of effects. Health Psychol. 2013;32(8):849. doi: 10.1037/a0030413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gau SS-F, Soong W-T, Merikangas KR. Correlates of sleep-wake patterns among children and young adolescents in Taiwan. Sleep J Sleep Sleep Disord Res. 2004 [PubMed] [Google Scholar]
- 12.Jenni OG, O’Connor BB. Children’s sleep: an interplay between culture and biology. Pediatrics. 2005;115(Supplement 1):204–216. doi: 10.1542/peds.2004-0815B. [DOI] [PubMed] [Google Scholar]
- 13.Duraccio KM, Jensen CD. Associations between physical and sedentary activity regularity and sleep in preschoolers and kindergartners. Sleep Health J Natl Sleep Found. 2017;3(4):263–268. doi: 10.1016/j.sleh.2017.04.001. [DOI] [PubMed] [Google Scholar]
- 14.Williams NJ, Grandne MA, Snipes A, et al. Racial/ethnic disparities in sleep health and health care: importance of the sociocultural context. Sleep Health. 2015;1(1):28. doi: 10.1016/j.sleh.2014.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Singh GK, Kenney MK. Rising prevalence and neighborhood, social, and behavioral determinants of sleep problems in US children and adolescents, 2003–2012. Sleep Disord. 2013;2013 doi: 10.1155/2013/394320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stretesky PB, Schuck AM, Hogan MJ. Space matters: An analysis of poverty, poverty clustering, and violent crime. Justice Q. 2004;21(4):817–841. [Google Scholar]
- 17.Sheehan CM, Cantu PA, Powers DA, Margerison-Zilko CE, Cubbin C. Long-term neighborhood poverty trajectories and obesity in a sample of california mothers. Health Place. 2017;46:49–57. doi: 10.1016/j.healthplace.2017.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Evans GW, Saegert S. Theoretical Perspectives in Environment-Behavior Research. Springer; 2000. Residential crowding in the context of inner city poverty; pp. 247–267. [Google Scholar]
- 19.Evans GW. The environment of childhood poverty. Am Psychol. 2004;59(2):77. doi: 10.1037/0003-066X.59.2.77. [DOI] [PubMed] [Google Scholar]
- 20.Buxton OM, Chang A-M, Spilsbury JC, Bos T, Emsellem H, Knutson KL. Sleep in the modern family: protective family routines for child and adolescent sleep. Sleep Health. 2015;1(1):15–27. doi: 10.1016/j.sleh.2014.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Massey DS. Getting away with murder: Segregation and violent crime in urban America. Univ Pa Law Rev. 1995:1203–1232. [Google Scholar]
- 22.Kelly CM, Schootman M, Baker EA, Barnidge EK, Lemes A. The association of sidewalk walkability and physical disorder with area-level race and poverty. J Epidemiol Community Health. 2007;61(11):978–983. doi: 10.1136/jech.2006.054775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kirk DS, Laub JH. Neighborhood change and crime in the modern metropolis. Crime Justice. 2010;39(1):441–502. [Google Scholar]
- 24.Spilsbury JC, Storfer-Isser A, Kirchner HL, et al. Neighborhood disadvantage as a risk factor for pediatric obstructive sleep apnea. J Pediatr. 2006;149(3):342–347. doi: 10.1016/j.jpeds.2006.04.061. [DOI] [PubMed] [Google Scholar]
- 25.Weden MM, Carpiano RM, Robert SA. Subjective and objective neighborhood characteristics and adult health. Soc Sci Med. 2008;66(6):1256–1270. doi: 10.1016/j.socscimed.2007.11.041. [DOI] [PubMed] [Google Scholar]
- 26.Cubbin C. Survey methodology of the geographic research on wellbeing (GROW) study. BMC Res Notes. 2015;8(1):1. doi: 10.1186/s13104-015-1379-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Margerison-Zilko C, Cubbin C, Jun J, Marchi K, Fingar K, Braveman P. Beyond the Cross-Sectional: Neighborhood Poverty Histories and Preterm Birth. Am J Public Health. 2015;105(6):1174–1180. doi: 10.2105/AJPH.2014.302441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Paruthi S, Brooks L, D’Ambrosio C, et al. Recommended Amount of Sleep for Pediatric Populations: A Statement of the American Academy of Sleep Medicine. J Clin Sleep Med JCSM Off Publ Am Acad Sleep Med. 2016 doi: 10.5664/jcsm.5866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kushnir J, Sadeh A. Correspondence between reported and actigraphic sleep measures in preschool children: the role of a clinical context. J Clin Sleep Med JCSM Off Publ Am Acad Sleep Med. 2013;9(11):1147. doi: 10.5664/jcsm.3154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Werner H, Molinari L, Guyer C, Jenni OG. Agreement rates between actigraphy, diary, and questionnaire for children’s sleep patterns. Arch Pediatr Adolesc Med. 2008;162(4):350–358. doi: 10.1001/archpedi.162.4.350. [DOI] [PubMed] [Google Scholar]
- 31.Iceland J, Steinmetz E. The effects of using census block groups instead of census tracts when examining residential housing patterns. US Census Bur Wash DC. 2003 [Google Scholar]
- 32.Lippert AM. Stuck in Unhealthy Places How Entering, Exiting, and Remaining in Poor and Nonpoor Neighborhoods Is Associated with Obesity during the Transition to Adulthood. J Health Soc Behav. 2016;57(1):1–21. doi: 10.1177/0022146515627682. [DOI] [PubMed] [Google Scholar]
- 33.Golley RK, Maher C, Matricciani L, Olds T. Sleep duration or bedtime? Exploring the association between sleep timing behaviour, diet and BMI in children and adolescents. Int J Obes. 2013;37(4):546–551. doi: 10.1038/ijo.2012.212. [DOI] [PubMed] [Google Scholar]
- 34.Meltzer LJ, Montgomery-Downs HE. Sleep in the family. Pediatr Clin North Am. 2011;58(3):765–774. doi: 10.1016/j.pcl.2011.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Friedman E, Montez J, Sheehan C, Guenewald T, Seeman T. Childhood Adversities and Adult Cardiometabolic Health: Does the Quantity, Timing, and Type of Adversity Matter? J Aging Health. 2015 doi: 10.1177/0898264315580122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bishaw A. Areas with Concentrated Poverty: 2006–2010. Vol. 9. US Department of Commerce, Economics and Statistics Administration, US Census Bureau; 2011. [Google Scholar]
- 37.Lockley SW, Skene DJ, Arendt J. Comparison between subjective and actigraphic measurement of sleep and sleep rhythms. J Sleep Res. 1999;8(3):175–183. doi: 10.1046/j.1365-2869.1999.00155.x. [DOI] [PubMed] [Google Scholar]
- 38.Lauderdale DS, Knutson KL, Yan LL, Liu K, Rathouz PJ. Sleep duration: how well do self-reports reflect objective measures? The CARDIA Sleep Study. Epidemiol Camb Mass. 2008;19(6):838. doi: 10.1097/EDE.0b013e318187a7b0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Link BG, Phelan J. Social conditions as fundamental causes of disease. J Health Soc Behav. 1995:80–94. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


