The state of medical care at the end of life in the United States was recently highlighted in the Institute of Medicine’s report titled, “Dying in America”.1 However, this report focused mostly on cancer and did not address specific challenges faced by patients with heart disease, which continues to be the most common cause of death in the United States. This significant omission is because most research in end of life care has been conducted on cancer patients and most care models, including hospice, have been designed to optimize care for that population. Therefore, unsurprisingly, cancer patients continue to be over-represented in hospice, while patients with heart disease are under-represented. (Figure)
Figure.
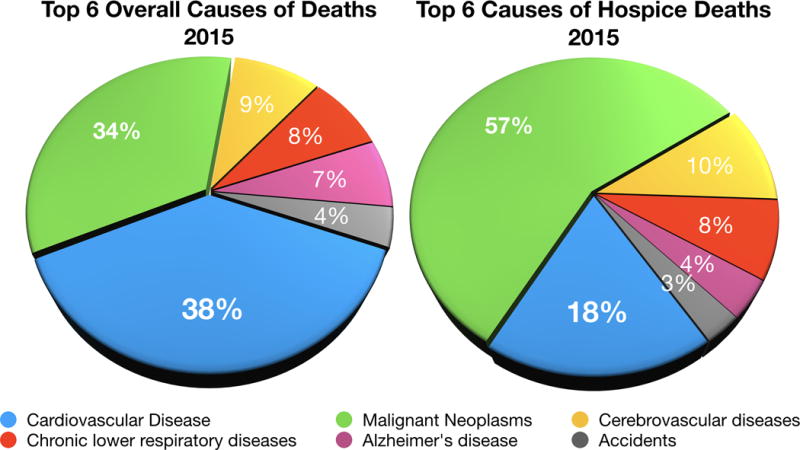
Authors’ analysis of Centers for Disease Control and Prevention (CDC) data shows the relative proportions of the top 6 causes of death in the United States, both overall and in hospice.
Advances in modern medicine have helped patients with cardiovascular disease live better and longer but many suffer disproportionately when the end is near. The inability to predict prognosis accurately is a primary reason patients with heart disease suffer disproportionately when close to death. Physicians are both less accurate and less comfortable in estimating prognosis in heart failure compared to cancer.2 The episodic nature of heart disease, punctuated by exacerbations and resolutions, contributes to this difficulty. Lack of accurate prognostication in cardiovascular patients not only affects patients’ ability to make important decisions but also affects their openness and subsequent referral to palliative care and hospice.
Clinical risk assessment is becoming increasingly difficult in heart disease patients with multiple comorbidities, competing risks and additional factors that interact with each other. The failure to accurately predict individual patients’ prognosis is a challenge that could potentially be addressed by the use of artificial intelligence.3 Preliminary analytic models have been developed using machine learning algorithms, natural language processing and recurrent neural networks for early detection of heart failure onset.3 These methodologies can collate the high-density of variables present for these patients. While these methodologies have considerable room to improve, it remains unknown if being presented with survival data will change the behavior of clinicians, patients or their caregivers.
Patients with heart failure suffer from a wide variety of symptoms at the end of life with the most common symptom being dyspnea. Three out of four heart failure patients in the United States experience difficult breathing in the last year before dying.4 Furthermore, the prevalence of other debilitating symptoms appears to be on the rise in patients with heart failure. From 1998 to 2008, no reduction was noted in the prevalence of dyspnea in heart failure patients, while the prevalence of pain and depression in patients with heart failure increased by 12% and 27% in 2008.4 The increasing burden of non-cardiac comorbidities could represent one reason for this trend. Over the same time period, more modest increases in pain and depression were noted amongst cancer patients (7.9% and 8.8% respectively).
The care of patients with advanced cardiovascular disease is challenging and quite different from patients with malignancies, who have traditionally been the focus of research conducted in this area. Terminally ill heart failure patients frequently require palliative interventions outside of the paradigm of routine hospice care such as inotropic support, drainage of pleural, pericardial and peritoneal effusions and outpatient/in-home intravenous diuretics. Expanding hospice services including testing models that incorporate more intensive palliative interventions and improving the training of nursing staff is critical.
Death is an inevitable outcome, which physicians can delay but never prevent. How patients die, though, is something that falls fully within the purview of physicians’ responsibilities. A critical step in improving end of life care in patients with heart disease is recognition from patients, families and physicians that there is a certain point in the natural history of cardiovascular disease beyond which more therapeutic interventions might be either futile or harmful. After such recognition is reached, it is necessary that pathways exist in which ‘doing less’ actually means doing more to cater to the specific needs of the patient. The provision of palliative care in patients with advanced heart failure was recently shown to improve quality of life in the PAL-HF trial.5 However, there is a burgeoning need for multicenter trials to explore the generalizability of specific palliative care interventions in heart disease patients.
Cardiologists have achieved great success in helping extend the lives of their patients. However, new challenges pertaining to the end of life have emerged that we need to address with similar intensity. We need to do more at an individual and system-wide level to ensure that every patient’s death is as comfortable and congruent with their wishes as possible.
Footnotes
Relevant disclosures: none
References
- 1.2014.IOM (Institute of Medicine) Dying in America: Improving quality and honoring individual preferences near the end of life. Washington, DC: The National Academies Press; [PubMed] [Google Scholar]
- 2.Warraich HJ, Allen LA, Mukamal KJ, Ship A, Kociol RD. Accuracy of physician prognosis in heart failure and lung cancer: Comparison between physician estimates and model predicted survival. Palliative medicine. 2016;30:684–9. doi: 10.1177/0269216315626048. [DOI] [PubMed] [Google Scholar]
- 3.Krittanawong C, Zhang H, Wang Z, Aydar M, Kitai T. Artificial Intelligence in Precision Cardiovascular Medicine. J Am Coll Cardiol. 2017;69:2657–2664. doi: 10.1016/j.jacc.2017.03.571. [DOI] [PubMed] [Google Scholar]
- 4.Singer AE, Meeker D, Teno JM, Lynn J, Lunney JR, Lorenz KA. Symptom trends in the last year of life from 1998 to 2010: a cohort study. Ann Intern Med. 2015;162:175–83. doi: 10.7326/M13-1609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rogers JG, Patel CB, Mentz RJ, Granger BB, Steinhauser KE, Fiuzat M, Adams PA, Speck A, Johnson KS, Krishnamoorthy A, Yang H, Anstron KJ, Dodson GC, Taylor DH, Jr, Kirchner JL, Mark DB, O’Connor CM, Tulsky JA. Palliative Care in Heart Failure: The PAL-HF Randomized, Controlled Clinical Trial. J Am Coll Cardiol. 2017;70:331–41. doi: 10.1016/j.jacc.2017.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]


