Abstract
Background
Identifying patients at risk of harm in general practice is challenging for busy clinicians. In UK primary care, trigger tools and case note reviews are mainly used to identify rates of harm in sample populations.
Aim
This study explores how adaptions to existing trigger tool methodology can identify patient safety events and engage clinicians in ongoing reflective work around safety.
Design and setting
Mixed-method quantitative and narrative evaluation using thematic analysis in a single East London training practice.
Method
The project team developed and tested five trigger searches, supported by Excel worksheets to guide the case review process. Project evaluation included summary statistics of completed worksheets and a qualitative review focused on ease of use, barriers to implementation, and perception of value to clinicians.
Results
Trigger searches identified 204 patients for GP review. Overall, 117 (57%) of cases were reviewed and 62 (53%) of these cases had patient safety events identified. These were usually incidents of omission, including failure to monitor or review. Key themes from interviews with practice members included the fact that GPs’ work is generally reactive and GPs welcomed an approach that identified patients who were ‘under the radar’ of safety. All GPs expressed concern that the tool might identify too many patients at risk of harm, placing further demands on their time.
Conclusion
Electronic trigger tools can identify patients for review in domains of clinical risk for primary care. The high yield of safety events engaged clinicians and provided validation of the need for routine safety checks.
Keywords: case notes, medical errors, medical records, organisation and administration, patient safety, prevention and control, primary care, trigger tools
INTRODUCTION
The nature of generalist work is high volume, complex, and time pressured. The general practice environment sets clinicians up to make mistakes that can potentially result in harm to patients. Despite the large number of consultations every day in primary care, reliable data about patient harm are hard to obtain. Studies based on case record reviews suggest a median of around two to three incidents per 100 consultations per patient records reviewed. The most common reported errors relate to diagnostics, medication, and communication.1,2
For many clinicians the main reflective work undertaken around safety involves significant event analysis.3 This tends to focus on major incidents such as a delayed diagnosis or a patient complaint and, although clinically important, significant events are generally of low frequency. Such events tend to hold the focus of clinical teams, which may be to the detriment of common areas of risk. Audit and peer feedback are widely used as quality improvement tools. Although research suggests that peer feedback can be valuable for improving quality, there are few studies that examine the impact on patient outcomes. Those available have found limited safety improvements.4 Both significant event analysis and audit focus on retrospective snapshots of activity. The challenge for busy GPs is knowing where to look, and what tools are needed, to understand more about how safe their practice is on a day-to-day basis.
Case note reviews are considered the ‘gold standard’ in identifying patient safety incidents, but they are labour intensive and there are challenges in selecting the most useful patient notes to review.5 Trigger tools were developed as an attempt to streamline the case note review process by flagging up triggers: elements of patient care that identify patients at higher risk of harm.
What is a trigger?
Triggers are defined as easily identifiable flags, occurrences, or prompts in patient records that alert reviewers to potential adverse events that may be undetected.6 These flags could include a safety-critical diagnosis, high-risk medications, results handling, or care delivered in more than one setting.1 The IHI Global Trigger Tool for Measuring Adverse Events was developed in 2003.7 Since that time trigger tool methodology has emerged as the leading approach for adverse event detection across a range of healthcare settings.8,9
Existing primary care trigger tool approach
Trigger tools have been in use in the UK primary care setting for around 9 years. The main work in the UK has been undertaken in Scotland,6,10 and in England by the NHS Institute for Innovation and Improvement.7 Most recently, the trigger tool has been included in the Royal College of General Practitioners’ Patient Safety Toolkit for General Practice.11 The focus of such work has been to provide the GP team with opportunities to identify patient safety-related incidents and for improvement activity.6
How this fits in
Trigger tool case note reviews have been used to identify patient safety events in UK primary care since 2009. They are mainly used to estimate the rate of adverse events and the types of processes most commonly associated with harm. This evaluation shows that the use of electronic triggers to identify areas of known risk can be incorporated into the regular work of general practice. Concerns about high volumes of patient safety events were not justified. GPs were reassured by tools that seek out errors before they become critical incidents.
The existing process for review using the trigger tool is to randomly select 25 patient records from an agreed cohort, for example, patients aged ≥75 years. These records are manually screened for the previous 4 months to identify triggers and any patient safety incidents. From this, an adverse event rate can be derived. This process is usually undertaken once, but can then be repeated at a future date to identify improvement.
UK and Australian primary care studies found an adverse event rate of around 9% from case note reviews using trigger tools.6,12 Harm rates were higher in older people and most harms were related to medication.10 Trigger tool studies undertaken in acute settings have found considerable variation in adverse event reporting between sites. This is most likely due to methodological differences in the interpretation of what constitutes severity and preventability of patient safety events.13,14
The existing trigger tool approach has drawbacks that limit the uptake in primary care. The time required for training and running the manual screening and review process requires a considerable investment for the practice, which will come at an opportunity cost to other activities.10 The case note reviews generate a lot of ‘noise’ and not much ‘signal’ when it comes to flagging up patient safety events. The yield of patient safety events obtained, around 9% in the published literature,10,12 may be insufficient to justify the additional time. As a result, they have not become established as part of everyday reflective practice around clinical safety in primary care.
Study aims
The aims of this study were to explore how adaptions to the existing trigger tool concept11 can use the electronic health record to identify patients at risk of harm and engage clinicians in reflective work around safety; and to evaluate the impact of the electronic trigger tool, including acceptability to clinicians, ease of use, and rates of finding patient safety events.
METHOD
This study was undertaken in an East London training practice with a population of 11 280 patients using the EMIS Web clinical record system. The project team included GPs, practice administrators (PAs), and staff based at the Clinical Effectiveness Group at Queen Mary University of London.
Development and implementation of trigger tools
The project team reviewed findings from the literature on the use of trigger tools in primary care. They chose to focus on three areas of clinical activity that are known to pose higher risk: results handling, prescribing, and uncoded diagnoses.10
The team developed working criteria to shortlist possible effective clinical triggers. It was agreed that triggers should:
be clinically important;
occur frequently enough to be measurable within a 1-year period;
be Read coded and hence searchable in the electronic record; and
be actionable in primary care should a patient safety event be identified.
Having agreed the first set of triggers, the team used an iterative approach to test and refine five EMIS Web searches to identify relevant patients. These searches are summarised in Box 1.
Box 1. Summary of five trigger tools searches.
| Clinical activity | Trigger | Which patients to search | Importance of trigger |
|---|---|---|---|
| Prescribing | ‘Triple threat’ | People >65 years co-prescribed NSAIDs, ACEIs/ARBs, and diuretics | This combination of medications is responsible for significant numbers of medication-related hospital admissions as it can put patients at increased risk of acute kidney injury |
| Heart failure and NSAIDs | People with coded heart failure prescribed NSAIDs as repeat medication | NSAIDs and risk of worsening heart failure | |
| Results handling | >75 years with low haemoglobin or ferritin | People >75 years old with haemoglobin <100 g/L or ferritin <15 ng/ml | To identify patients with occult blood loss |
| Falling eGFR | People with a drop of ≥10 ml/minute in eGFR compared with previous result | To identify patients at risk of progressive CKD | |
| Uncoded diagnoses | Uncoded CKD | People with eGFR <60 ml/minute but not coded as CKD | Uncoded CKD is associated with suboptimal primary care management and increased prescribing risk |
ACEI/ARB = angiotensin-converting enzyme inhibitor/angiotensin receptor blockers. CKD = chronic kidney disease. eGFR = estimated glomerular filtration rate. NSAID = non-steroidal anti-inflammatory drug.
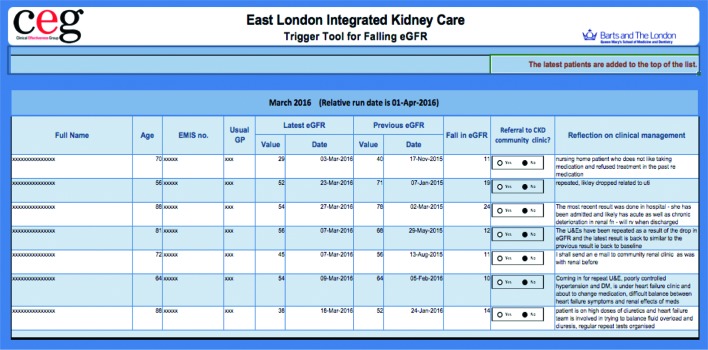
To make the process of case note review straightforward, a macro-enabled Excel worksheet was developed for each of the five trigger searches to guide the case note review. The PA ran the searches on the dates specified in the trigger tool manual and exported the results to the relevant worksheet (Figure 1). This was automatically populated with relevant clinical information for each identified patient, highlighting areas on which to focus the review, and providing space for a narrative reflection.
Figure 1.
Example of a trigger tool worksheet.
As an incentive to complete the trigger tool review, the worksheet functionality includes the option for GPs to export the anonymised data to their appraisal toolkit as evidence of reflective practice. However, there was no external financial or other incentive to complete reviews.
During implementation a four-step trigger tool process was developed by the project team (Box 2).
Box 2. Four-step trigger tool process.
| 1. Search: | EMIS searches run by practice administrator to identify patients with triggers. Patients identified were exported to worksheets for review by GPs |
| 2. Review: | GPs were alerted to undertake a case note review of patient notes using trigger tool worksheets. GPs focused on the preceding 3 months of care to establish a management narrative and identify any areas where patient safety events may have occurred, or may be at risk of occurring |
| 3. Action: | To remedy any identified patient safety event, for example, medication monitoring, informing patients about diagnoses, repeating blood tests, and making referrals to other services |
| 4. Reflect: | Record free-text reflections on clinical care delivered and any patient safety problems identified. This reflection and the anonymised contents of the worksheet could be exported to use for clinical appraisal |
Evaluation methods
A mixed-method evaluation was carried out. The quantitative aspect included summary statistics from the worksheets completed between April 2015 and March 2016, including the numbers of patients identified and reviewed, and the rate of identification of patient safety events from each trigger tool worksheet.
A narrative evaluation was undertaken by a qualitative consultancy (CSR International) using thematic analysis. Semi-structured, videorecorded, face-to-face, and telephone interviews with five GPs and one administrative member of the practice team were undertaken to explore barriers and benefits to implementation, ease of use, and value of the trigger tool in the context of a busy GP surgery. Each interview typically took 30 minutes and all participants gave written consent. The interview schedule was developed from the trigger tool literature13 and from project planning meetings. The full interview schedule is available from the authors on request.
RESULTS
Quantitative evaluation
During the 1-year study period the trigger searches identified 204 patients for GPs to review. Of these patients, 117 (57%) had a case note review by a GP (Table 1).
Table 1.
Summary results of trigger tool implementation in April 2015 to March 2016 (N = 11 280)
| Trigger | Time period for EMIS Web search | Patients identified, n | Case note review completed, n | Patient safety issues requiring action, n (%) |
|---|---|---|---|---|
| Falling eGFR | Monthly | 67 | 54 | 34 (63) |
| Heart failure and NSAIDs | Quarterly | 7 | 3 | 2 (67) |
| Uncoded CKD | Quarterly | 48 | 21 | 15 (71) |
| >75 years with low ferritin or haemoglobin | Quarterly | 48 | 35 | 9 (26) |
| Triple threat (ACEI/ARB, NSAID, and diuretic) | Quarterly | 34 | 4 | 2 (50) |
| Total | – | 204 | 117 | 62 (53) |
ACEI/ARB = angiotensin-converting enzyme inhibitor/angiotensin receptor blockers. CKD = chronic kidney disease. eGFR = estimated glomerular filtration rate. NSAID = non-steroidal anti-inflammatory drug.
Patient safety events were identified in 26–71% of the case note reviews depending on the trigger search, and in 53% of the case note reviews across all five trigger searches.
The trigger searches identified around four patients per GP per month to review. Completion rates for the case note reviews improved over the course of the study.
The types of patient safety issues identified were generally incidents of omission and would be classified as ‘no harm’ or ‘low harm’ based on UK National Patient Safety Agency definitions.14 The categories of patient safety events identified, and the actions required for mitigation, are summarised in Box 3.
Box 3. Categories of patient safety issues identified and actions required.
| Category of patient safety issue or action required on case note review | Example of action required |
|---|---|
| Incorrect coding |
|
| Action required but not taken |
|
| Routine monitoring not done |
|
| Investigations |
|
| Medication changes |
|
| Clinical contact |
|
Qualitative evaluation
The following themes emerged from the interviews with practice members.
Perceptions of safety
Clinical work for GPs is high volume and high pressure, and is generally reactive. GPs acknowledged that under pressure they cannot always do as good a job as they would like, and are aware that sometimes patient safety could be negatively affected as a result:
‘We’re generally reactive. If a patient has a haemoglobin of 8 we act on it, but we give responsibility to the patient for the follow-up. If they don’t do it there is no system in place to follow it up or highlight that it has not been done. So you might just come across them a year later and act on it.’
(GP 1)
‘Because of the way we work in general practice and the increase in pressures over the last 5–10 years, we don’t always do as good a job as we like … so there are potentially things going on that are unsafe that we don’t know about.’
(GP 2)
Finding the hidden risks
Many patients identified through the tools were already on GPs’ radar as regular attenders and GPs believed they were on top of their management. But the trigger tools identified other patients for whom GP awareness was lower and this enabled GPs to take action to avoid future problems. For example, some of the tools highlighted patients who had not taken action following previous GP advice and the tool prompted the GP to contact them again. In other cases the tool flagged up conditions that may have been overlooked by GPs or that were not coded correctly, the results of tests requiring repeat, and medications that needed review or stopping:
‘As a safety mechanism it is very valuable. I know at least one patient I picked up in the last 6 months whose kidney function had deteriorated and for some reason it wasn’t actioned, and this was a reminder to do something about it.’
(GP 3)
‘Its value lies in finding hidden risks and identifying errors before they happen — it’s telling us if something could go wrong more than us being reactive, we’re anticipating it.’
(GP 1)
Given their working environment, a tool that helps to identify potential risk and aids reflective practice appealed to GPs in the study because they could see the potential benefits. It allowed for a degree of ‘back-checking’ that GPs did not have time to undertake and systemised reflective practice. This in turn encouraged a corporate approach to managing known risks and sensitised the GP team to the identification of other areas of risk.
Will it add to my workload?
Regardless of the potential value, at the start of this project it was uncertain how much additional work use of the trigger tool would generate. The GPs all expressed concern that the tool might identify too many patients at risk of harm, place further demands on GP time, and require additional resources to manage properly. These concerns illustrate the current uncertainty in practice about the potential volume of hidden risks to patient care:
‘Heart said “good idea”. Head said “hope it doesn’t significantly increase my workload”!’
(GP 2)
‘If it was producing 50 patients each time then you would wonder how you were going to find the time to action that.’
(GP 4)
The PA played a critical role in running the searches, exporting the search results to the worksheets, and prompting clinicians to take action. This included booking ‘virtual appointments’, email notification, and written reminders:
‘I’m like a dog with a bone.’
(PA)
The management of clinical risk needs to be viewed as a task for the whole practice. The administrator needed perseverance to identify the best method of engaging clinicians to carry out these additional tasks. This was particularly the case when the tools were introduced. As time passed, rates of tool completion increased as they became part of regular GP work.
Changing GP behaviour in managing risk
There were clear benefits to patient care when the trigger tools identified a missed result or prompted a patient intervention. Alongside these benefits there were indications that the tools became embedded in routine clinical care, and began changing clinical behaviour.
GPs reported that the discipline of completing the tools encouraged them to look more holistically and in depth at the patient record, including looking at historical information to compare changes over time and build a more complete narrative about patient management:
‘… valuable in providing insight re more vulnerable patients where it is often more difficult to spot problems when they have a variety of problems and are on several medications [for example] dementia patients in nursing homes.’
(GP 4)
‘I’m looking at things more holistically now to try and get an overall picture of health and the medication they are on.’
(GP 5)
‘Before if it had come back with an eGFR of 70 I would have thought “that looks fine” but now I will look back and compare previous results and ask “why” a bit more.’
(GP 3)
DISCUSSION
Summary
This study demonstrates that developing an electronic search for pre-specified triggers can identify patients for review in key areas of patient risk in primary care. Running these tools in regular cycles identified a manageable number of cases for each clinician to review. This approach has the potential to embed a culture of ongoing attention to patient safety events, and engage busy GPs in reflective work around patient safety.
This represents a novel extension to the primary care trigger tool model, shifting the focus of the tools from a snapshot that estimates rates of harm, towards a safety net used as part of routine practice.
The types of patient safety events identified by the trigger tool searches were usually incidents of omission. These missed actions, such as monitoring, clinical reviews, or referrals, may individually appear small, but have the potential to lead to significant consequences for patients in the future. This element, which enabled patient safety issues to be remedied by simple actions before harm occurs, was most valued by the GPs in this study.
It was essential to have adequate administrative support to run searches, export the data to the worksheets, and prompt clinicians to undertake the reviews.
There were some concerns regarding patients who were identified through the trigger tool searches but for whom no case note review was conducted. However, the identification of a trigger does not necessarily mean there is a patient safety incident. The searches offered clinicians the opportunity to undertake a review, but it was not compulsory.
Strengths and limitations
By ensuring a simple review process, and not overloading clinicians with additional work, it was possible to engage with the professional motivation of clinicians. On average the trigger searches identified up to four patients a month for each GP to review, with most taking <4 minutes to complete. This was felt to be an acceptable amount of work by clinicians in this study.
Throughout the project period, 57% of patients identified through the trigger tool searches had a case note review. The lead administrator helped achieve a high level of clinician response by iteratively testing a range of methods to encourage clinicians to complete the reviews. Completion rates for the case note reviews improved over the course of the study, suggesting that once clinicians understood the process it became embedded as part of everyday practice.
The search ‘>75 years with low ferritin or haemoglobin’ that had the lowest yield of events (26%) identified a higher yield of safety events than the figure of 9% found in the existing published literature on primary care trigger tools.10 Across all five trigger searches, 53% of patients receiving a case note review required action to address possible safety events. This high yield of patient events identified from the five triggers was sufficient to highlight the benefits of an additional safety check on their work to the GPs in the study.
One limitation of this study is that it was undertaken at a single general practice. The widespread uptake of trigger searches will depend on the willingness of practices to invest time in the process and acknowledge the importance of identifying unrecognised patient safety events.
A major limitation is that using an automated approach such as used in this study depends on coded data. Many important patient safety events are not amenable to these methods; some may only be identifiable from free text in consultations, and others from an absence of text or data. Hence it is important to use a mixture of methods to identify and reflect on patient safety.
The project team provided training on the trigger tools for all the practice GPs. This stressed that the trigger tool was not a performance management tool for GPs but was a means of allowing GPs to take a dispassionate look at the care delivered to patients with more complex conditions. Some colleagues introduced a ‘fresh eyes’ approach whereby they undertook case note reviews with trainees, or other colleagues, to provide another clinician’s perspective on the clinical care delivered.
Implications for practice
From the outset this project was undertaken with the ambition of scaling up beyond a single practice. More than 550 case note reviews have now been undertaken to test proof of concept with the adapted trigger tool process, and the searches and worksheets are available for use by other practices using EMIS Web. Further trigger searches with associated reflective worksheets can be identified and developed by other practice teams.
The falling eGFR trigger tool is the first to be used beyond the pilot site. It is now used in GP practices across north-east London to identify patients with worsening kidney function who may benefit from a clinical review, either in primary care or by a nephrologist.
A further use of the adapted trigger tool is in demonstrating evidence of proactive and reflective patient care in the context of GP appraisal and practice reviews. Data from the worksheets can be anonymised and used as evidence of reflection for clinical appraisal. Such tools can be used as evidence of effective care and a patient safety culture for external reviews such as the Care Quality Commission practice inspections. Evidence based on the use of trigger tools was identified in the inspector’s 2016 report on the study practice as an example of effective care, and contributed to the practice achieving an outstanding rating in this domain.15
Acknowledgments
Thanks to staff at the Clinical Effectiveness Group who provided technical support for the searches and tools, and to GPs and staff at Jubilee Street Practice for giving trigger tools a try.
Funding
This project was supported by a Tower Hamlets Clinical Commissioning grant to promote innovation and quality improvement.
Ethical approval
Ethical approval was not required for this observational study because all patient data are Read coded non-identifiable data with results published in aggregate form.
Provenance
Freely submitted; externally peer reviewed.
Competing interests
All authors have current or recent clinical posts at the study practice.
Discuss this article
Contribute and read comments about this article: bjgp.org/letters
REFERENCES
- 1.Health Foundation. Evidence scan: levels of harm in primary care. London: Health Foundation; 2011. [Google Scholar]
- 2.Panesar SS, deSilva D, Carson-Stevens A, et al. How safe is primary care? A systematic review. BMJ Qual Saf. 2016;25(7):544–553. doi: 10.1136/bmjqs-2015-004178. [DOI] [PubMed] [Google Scholar]
- 3.Cox SJ, Holden JD. A retrospective review of significant events reported in one district in 2004–2005. Br J Gen Pract. 2007;57(542):732–736. [PMC free article] [PubMed] [Google Scholar]
- 4.Phillips CB, Pearce CM, Hall S, et al. Can clinical governance deliver quality improvement in Australian general practice and primary care? A systematic review of the evidence. Med J Aust. 2010;193(10):602–607. doi: 10.5694/j.1326-5377.2010.tb04071.x. [DOI] [PubMed] [Google Scholar]
- 5.Panesar S, Diaper M, Forsyth D, et al. Don’t let primary care patients slip through the nets. Health Service Journal. 2015 https://www.hsj.co.uk/commissioning/dont-let-primary-care-patients-slip-through-the-nets/5078203.article (accessed 12 Feb 2018) [Google Scholar]
- 6.de Wet C, Bowie P. Screening electronic patient records to detect preventable harm: a trigger tool for primary care. Qual Prim Care. 2011;19(2):115–125. [PubMed] [Google Scholar]
- 7.Griffin FA, Resar RK. IHI global trigger tool for measuring adverse events. 2nd edn. Cambridge, MA: Institute for Healthcare Improvement; 2009. IHI Innovation Series white paper. [Google Scholar]
- 8.Sharek PJ. The emergence of the trigger tool as the premier measurement strategy for patient safety. AHRQ WebM&M. 2012;2012(5):120. [PMC free article] [PubMed] [Google Scholar]
- 9.NHS Education for Scotland The primary care trigger tool: practical guidance for GP teams. Reviewing electronic patient records to detect avoidable harm. 2010 http://www.nes.scot.nhs.uk/media/6361/Primary%20Care%20Trigger%20Tool%20-%20Practical%20Guidance.pdf (accessed 19 Feb 2018) [Google Scholar]
- 10.de Wet C, Bowie P. The preliminary development and testing of a global trigger tool to detect error and patient harm in primary-care records. Postgrad Med J. 2009;85(1002):176–180. doi: 10.1136/pgmj.2008.075788. [DOI] [PubMed] [Google Scholar]
- 11.Royal College of General Practitioners. Patient safety toolkit for general practice. 2017 http://www.rcgp.org.uk/clinical-and-research/toolkits/patient-safety.aspx (accessed 12 Feb 2018) [Google Scholar]
- 12.Hibbert P, Williams H. The use of a global trigger tool to inform quality and safety in Australian general practice: a pilot study. Aust Fam Physician. 2014;43(10):723–726. [PubMed] [Google Scholar]
- 13.Schildmeijer K, Nilsson L, Perk J, et al. Strengths and weaknesses of working with the Global Trigger Tool method for retrospective record review: focus group interviews with team members. BMJ Open. 2013;3(9):e003131. doi: 10.1136/bmjopen-2013-003131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hibbert PD, Molloy CJ, Hooper TD, et al. The application of the Global Trigger Tool: a systematic review. Int J Qual Health Care. 2016;28(6):640–649. doi: 10.1093/intqhc/mzw115. [DOI] [PubMed] [Google Scholar]
- 15.Care Quality Commission. Inspection summary: Jubilee Street Practice. 2016 http://www.cqc.org.uk/location/1-565816951/inspection-summary#effective (accessed 12 Feb 2018) [Google Scholar]