Abstract
Background
We examined mammography use before and after Medicare eliminated cost sharing for screening mammography in January 2011.
Methods
Using National Health Interview Survey data, we examined changes in mammography use between 2010 and 2013 among Medicare beneficiaries aged 65–74 years. Logistic regression and predictive margins were used to examine changes in use after adjusting for covariates.
Results
In 2013, 74.7% of women reported a mammogram within 2 years, a 3.5 percentage point increase (95% confidence interval, −0.3, 7.2) compared with 2010. Increases occurred among women aged 65–69 years, unmarried women, and women with usual sources of care and 2–5 physician visits in the prior year. After adjustment, mammography use increased in 2013 versus 2010 (74.8% vs. 71.3%, P = 0.039). Interactions between year and income, insurance, race, or ethnicity were not significant.
Conclusions
There was a modest increase in mammography use from 2010 to 2013 among Medicare beneficiaries aged 65–74 years, possibly consistent with an effect of eliminating Medicare cost sharing during this time. Findings suggest that eliminating cost sharing might increase use of recommended screening services.
Keywords: mammography, Medicare, early detection of cancer, cost sharing
Medicare provides health care coverage to most Americans aged 65 years and older. Breast cancer has a substantial impact on the female Medicare population. Risk increases with age,1 with incidence rates considerably higher among women aged 65 years and older compared with younger women, and most breast cancer deaths occurring in this age group.2 Screening mammography increases early detection of breast cancer, which leads to earlier treatment, and reductions in mortality. Its use is recommended by the US Preventive Services Task Force (USPSTF) every 2 years for women aged 50–74 years.1 Thus many Medicare beneficiaries are eligible for screening.
For beneficiaries aged 65 years and older, Medicare Part B covers screening mammograms.3 Initially, coverage was subject to deductible and coinsurance.4 In 1997 legislation waived the deductible, but a 20% coinsurance remained,5,6 translating to approximately $15–$40 per mammography.7 Despite coverage, many women with Medicare coverage have not received a recent mammogram.8 Furthermore, cancer screening uptake is lower for some groups, with differences in use by race and ethnicity8 and type of Medicare coverage8,9 described. For example, among traditional Medicare beneficiaries, black, Hispanic, and Asian or Pacific Islander women were less likely to have had a recent mammogram than white women, although this was not found among those in Medicare health maintenance organizations.8
Multiple barriers to screening have been described, including access to and cost of screening services.10,11 Lower income and uninsured women are less likely than women with higher income or insurance coverage to use screening services.12,13 Cost may be a barrier to screening in the Medicare population as well, with Medicare beneficiaries without supplemental insurance to defray costs less likely to receive screening than those with supplemental coverage.4,9,14 Although some report no detrimental effect of cost sharing on recommended cancer screening use, including mammography,15,16 others indicate it may have a negative effect. Cost sharing has been associated with lower mammography use,17–19 and some suggest that negative effects of cost sharing may be greater for mammography than other preventive services19 and that deductibles or coinsurance might have a greater negative effect on mammography than other forms of cost sharing.19 Differences in cost sharing by type of Medicare coverage have also been suggested to possibly contribute to racial and ethnic differences in mammography use among beneficiaries.8
Beginning January 1, 2011, for services covered by Medicare, the Affordable Care Act required coverage without cost sharing for preventive services rated “A” (strongly recommended) or “B” (recommended) by the USPSTF, including screening mammography.20,21 The purpose of the current analysis was to examine whether mammography use increased after elimination of Medicare cost sharing for screening mammography and whether changes varied for different groups of women.
METHODS
We used data from the 2005, 2008, 2010, and 2013 National Health Interview Survey (NHIS), an annual survey administered through in-person interviews of a nationally representative sample of the civilian, noninstitutionalized US population. We used these survey years because these are the most recent years that provide information about USPSTF guideline-concordant mammography use. Response rates were 60.8%–69.0%. More information on the NHIS is available elsewhere (http://www.cdc.gov/nchs/nhis).
We included female Medicare beneficiaries without breast cancer history who were 65–74 years of age. Women in this age group without Medicare coverage were not included. Women with previous breast cancers were excluded because they would be subject to recommendations for annual surveillance mammography22 rather than general population screening which is the focus of this analysis.
We first examined the proportion of women in each year up-to-date with USPSTF guidelines for mammography screening. Our dependent variable was reporting having received a mammogram in the prior 2 years (recent mammogram), consistent with USPSTF recommendations.1 For 2010 (n = 1429) and 2013 (n = 2152), we compared mammography use by each factor within year using Pearson Wald F tests. In order to examine whether mammography use changed between 2010 and 2013, we calculated the difference between years in screening use with 95% confidence intervals (CI). To examine whether any changes were new in 2013 versus continuations of ongoing trends, we plotted the proportion of women up-to-date with mammography screening in 2005, 2008, 2010, and 2013.
We used multivariable logistic regression to determine whether mammography use changed between 2010 and 2013, after adjusting for potential differences in other factors between years. We included as covariates several socio-demographic factors shown in previous literature to be associated with cancer screening use, including age (65–69 y, 70–74 y), race (white, black, Asian, American Indian/Alaska Native), ethnicity (Hispanic, non-Hispanic), birthplace (born in US, foreign-born), marital status (married/living with partner, unmarried/not living with partner), and income (as a percentage of poverty thresholds).8,12,23 We also included measures of access to care, including type of insurance (Medicare with private supplement, Medicare and Medicaid, Medicare with other supplement, Medicare Advantage, traditional Medicare only), having a usual source of care (yes, no), and number of provider visits in the prior year (0, 1, 2–5, ≥6), and health status (excellent/very good/good, fair/poor) as these have also been shown to be related to screening use.7,12,24 Nonbreast cancer history (yes, no) was also included as a covariate given that prior experience with cancer may influence motivation to screen. Missing income data were imputed by National Center for Health Statistics (NCHS) using multiple imputation.25 The model included survey year and all other covariates as predictors. Results are presented as predictive margins, which represent the average predicted response if the entire sample had been in a given group.26 Thus, predictive margins, or adjusted percentages, account for covariates in the model. By including survey year in the model, we were able to calculate predictive margins separately for 2010 and 2013. This enabled us to examine whether mammography use changed over time after accounting for differences in other covariates between years. We hypothesized that elimination of cost sharing might have a greater effect on mammography use among those with lower income or no supplemental insurance. To examine these questions and whether cost sharing elimination would influence differences in use by race or ethnicity, we decided a priori to include in the model interactions between year and income, insurance, race, and ethnicity. Nonsignificant interaction terms were removed from the final model.
Because Medicare Advantage plans may not have been required to eliminate cost sharing for recommended preventive services until 2012,27 we also examined mammography use excluding Medicare Advantage enrollees. We weighted all statistics and used SUDAAN version 11.0.1 (Research Triangle Institute, Research Triangle Park, NC) and SAS version 9.3 (SAS Institute Inc., Cary, NC) to account for the complex survey design.
RESULTS
Most women were white, non-Hispanic, US-born, had usual sources of care, visited a physician at least twice the prior year, and reported at least good health (Table 1). Approximately 50%–55% of women had supplemental private insurance, 8%–9% had dual Medicare/Medicaid coverage, 13%–19% had Medicare Advantage, and 18%–21% had traditional Medicare only. Women were more likely to have higher income and Medicare Advantage in 2013 than in 2010.
TABLE 1.
Sociodemographic, Health and Health Care Access Characteristics of Female Medicare Beneficiaries Aged 65–74 Years, by Survey Year (Weighted Percentages)
| 2010 | 2013 | |||
|---|---|---|---|---|
|
|
|
|||
| n | % (95% CI) | n | % (95% CI) | |
| Total | 1429 | 100% | 2152 | 100% |
| Age (y) | ||||
| 65–69 | 757 | 54.1 (51.0–57.2) | 1195 | 56.6 (54.2–59.0) |
| 70–74 | 672 | 45.9 (42.8–49.0) | 957 | 43.4 (41.0–45.8) |
| Race | ||||
| White | 1101 | 85.2 (83.1–87.1) | 1692 | 83.9 (82.1–85.6) |
| Black | 253 | 10.7 (9.2–12.4) | 332 | 10.8 (9.5–12.3) |
| Asian | 63 | 3.4 (2.5–4.7) | 103 | 4.6 (3.6–5.8) |
| AIAN | 10 | * | 24 | * |
| Ethnicity | ||||
| Hispanic | 180 | 8.2 (6.8–9.7) | 236 | 8.0 (6.8–9.4) |
| Non-Hispanic | 1249 | 91.8 (90.3–93.2) | 1916 | 92.0 (90.6–93.2) |
| Foreign-born status | ||||
| Born in US | 1202 | 87.8 (85.7–89.6) | 1819 | 86.3 (84.4–88.1) |
| Foreign-born | 227 | 12.3 (10.6–14.3) | 332 | 13.9 (12.1–15.8) |
| Marital status† | ||||
| Married | 559 | 53.4 (50.4–56.5) | 912 | 57.8 (55.3–60.2) |
| Unmarried | 866 | 46.6 (43.5–49.6) | 1238 | 42.2 (39.8–44.7) |
| Income (% poverty threshold) | ||||
| < 139 | 392 | 20.9 (18.2–23.9) | 517 | 18.2 (16.2–20.4) |
| 139–250 | 354 | 23.5 (20.9–26.3) | 513 | 23.9 (21.5–26.4) |
| 251–400 | 334 | 25.8 (22.7–29.2) | 469 | 21.9 (19.5–24.5) |
| > 400 | 348 | 29.7 (26.2–33.4) | 653 | 36.0 (33.4–38.8) |
| Health insurance | ||||
| Medicare+private | 685 | 54.2 (51.1–57.3) | 1012 | 49.5 (46.9–52.1) |
| Medicare+Medicaid‡ | 180 | 8.6 (7.1–10.4) | 249 | 8.8 (7.5–10.3) |
| Medicare+other§ | 43 | * | 81 | 4.4 (3.2–5.9) |
| Medicare Advantage only | 204 | 13.4 (11.5–15.7) | 363 | 19.0 (16.9–21.3) |
| Traditional Medicare|| only | 307 | 20.4 (18.1–22.8) | 429 | 18.4 (16.3–20.7) |
| Usual source of care | ||||
| Yes | 1358 | 96.9 (95.8–97.7) | 2058 | 95.9 (94.7–96.9) |
| No | 53 | 3.1 (2.3–4.2) | 85 | 4.1 (3.1–5.3) |
| # Physician visits prior year | ||||
| None | 107 | 6.4 (5.1–8.0) | 146 | 6.8 (5.6–8.3) |
| 1 | 137 | 10.4 (8.5–12.7) | 254 | 10.9 (9.4–12.7) |
| 2–5 | 652 | 48.2 (45.1–51.4) | 970 | 46.4 (43.8–49.1) |
| ≥6 | 504 | 34.9 (31.9–38.2) | 746 | 35.8 (33.2–38.4) |
| Health status | ||||
| Excellent/very good/good | 1093 | 80.4 (78.1–82.5) | 1722 | 81.0 (79.0–82.9) |
| Fair/Poor | 335 | 19.6 (17.5–21.9) | 429 | 19.0 (17.1–21.0) |
| Cancer history¶ | ||||
| Yes | 109 | 8.8 (7.2–10.7) | 198 | 10.0 (8.4–11.9) |
| No | 1320 | 91.6 (89.8–93.1) | 1954 | 90.4 (88.6–92.0) |
Estimate suppressed because denominator <50 and/or relative SE > 30%.
Includes married or living with partner versus unmarried/not living with partner.
Includes those with other state-sponsored insurance.
Includes military plans, other government plans, or Indian Health Service.
Includes Medicare Part A and/or Part B.
Excludes breast cancer or nonmelanoma skin cancer.
AIAN indicates American Indian/Alaska Native; CI, confidence interval.
Data Source: CDC/NCHS, National Health Interview Survey, 2010 and 2013.
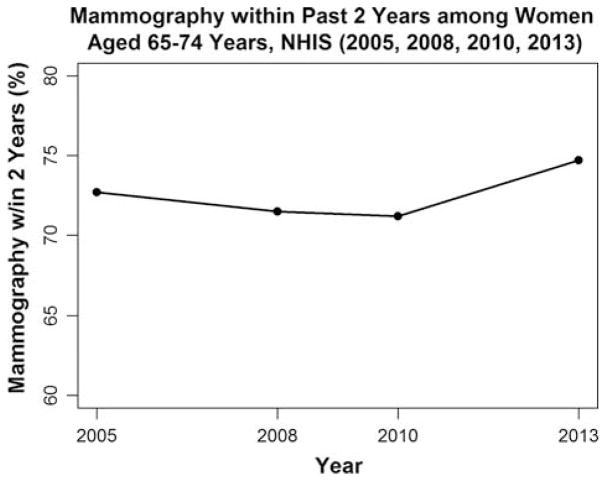
Compared with earlier years, in 2013 mammography use seems to have increased (Fig. 1). Overall, 74.7% reported having a recent mammogram in 2013 (Table 2). This reflects a 3.5 percentage point increase (95% CI, −0.3 to 7.2) compared with 2010. Women aged 65–69 years experienced a 6.1 percentage point increase, leading to a difference in mammography use by age in 2013 (76.9% vs. 71.8%, P = 0.027) not present in 2010. Non-Hispanic women experienced a 4.0 percentage point increase (95% CI, 0.0–8.0). In both years, unmarried women had lower mammography use than married women, although use for unmarried women increased 5.3 percentage points (95% CI, 0.5–10.1) in 2013. In both years, use was also directly related to income, and dual Medicare/Medicaid coverage or traditional Medicare only was associated with lower use than supplemental private insurance or Medicare Advantage. No clear changes over time by income or insurance were present. Mammography use among women lacking a usual source of care was low, however, numbers were small and estimates imprecise. There was a modest increase in use for women with usual sources of care. Fewer than 2 physician visits the prior year and fair/poor health status were associated with lower mammography use in both years, with particularly low uptake for those with no visits (30%–35%). Women with 2–5 visits experienced a 7.0 percentage point increase over time; those with at least good health experienced a 3.5 percentage point increase (95% CI, −0.6 to 7.5). In multivariable analysis (Table 3), mammography use was significantly higher in 2013 than 2010 (predictive margins 74.8% vs. 71.3%, P = 0.039). No interactions were significant.
FIGURE 1.
Mammography trends among Medicare beneficiaries aged 65–74 years. NHIS indicates National Health Interview Survey.
TABLE 2.
Proportion of Female Medicare Beneficiaries Aged 65–74 Years Reporting Having Received a Mammogram Within the Prior 2 Years, by Sociodemographic, Health and Health Care Access Factors, and Survey Year (Weighted Percentages)
| 2010 | 2013 | ||||
|---|---|---|---|---|---|
|
|
|
||||
| n | % (95% CI) | n | % (95% CI) | Δ (95% CI) | |
| Total | 1300 | 71.2 (68.0–74.2) | 2090 | 74.7 (72.3–77.0) | 3.5 (−0.3 to 7.2) |
| Age (y) | P = 0.7565 | P = 0.0270 | |||
| 65–69 | 691 | 70.8 (66.3–75.0) | 1160 | 76.9 (73.8–79.8) | 6.1 (0.9–11.3) |
| 70–74 | 609 | 71.7 (67.7–75.3) | 930 | 71.8 (68.1–75.2) | 0.1 (−4.9 to 5.1) |
| Race | P = 0.3480 | P = 0.7594 | |||
| White | 1015 | 71.9 (68.4–75.2) | 1649 | 74.8 (72.0–77.4) | 2.9 (−1.2 to 7.0) |
| Black | 216 | 69.0 (61.9–75.4) | 319 | 73.8 (67.5–79.3) | 4.8 (−4.0 to 13.6) |
| Asian | 58 | 60.1 (46.2–72.5) | 97 | 73.3 (61.0–82.8) | 13.2 (−6.1 to 32.5) |
| AIAN | 9 | * | 24 | * | * |
| Ethnicity | P = 0.2766 | P = 0.6034 | |||
| Hispanic | 164 | 75.5 (66.4–82.8) | 230 | 73.1 (66.7–78.7) | −2.4 (−12.8 to 7.9) |
| Non-Hispanic | 1136 | 70.9 (67.5–74.0) | 1860 | 74.8 (72.2–77.3) | 4.0 (0.0 to 8.0) |
| Foreign-born status | P = 0.6951 | P = 0.6799 | |||
| Born in US | 1093 | 71.4 (68.0–74.6) | 1770 | 74.9 (72.2–77.4) | 3.5 (−0.5 to 7.5) |
| Foreign-born | 207 | 69.8 (61.9–76.7) | 319 | 73.5 (67.1–79.1) | 3.7 (−5.7 to 13.1) |
| Marital status† | P = 0.0001 | P = 0.0031 | |||
| Married | 518 | 76.4 (72.0–80.3) | 891 | 77.7 (74.1–80.9) | 1.3 (−3.9 to 6.5) |
| Unmarried | 779 | 65.3 (61.1–69.2) | 1197 | 70.6 (67.4–73.5) | 5.3 (0.5–10.1) |
| Income (% poverty threshold) | P < 0.0001 | P < 0.0001 | |||
| < 139 | 336 | 59.1 (51.8–66.0) | 495 | 61.2 (55.7–66.4) | 2.1 (−6.7 to 10.9) |
| 139–250 | 323 | 64.0 (57.3–70.2) | 500 | 69.8 (63.9–75.0) | 5.8 (−2.2 to 13.8) |
| 251–400 | 313 | 72.4 (65.5–78.5) | 456 | 75.2 (69.4–80.1) | 2.7 (−5.3 to 10.7) |
| > 400 | 328 | 83.4 (77.9–87.6) | 639 | 84.4 (80.1–87.9) | 1.0 (−4.8 to 6.9) |
| Health insurance | P < 0.0001 | P < 0.0001 | |||
| Medicare+private | 631 | 77.7 (73.3–81.6) | 990 | 81.3 (78.0–84.2) | 3.6 (−1.5 to 8.7) |
| Medicare+Medicaid‡ | 163 | 56.1 (47.0–64.9) | 243 | 63.2 (55.1–70.7) | 7.1 (−4.7 to 18.9) |
| Medicare+other§ | 38 | * | 74 | 80.9 (68.9–89.0) | * |
| Medicare Advantage only | 193 | 73.9 (66.5–80.1) | 352 | 74.7 (68.4–80.1) | 0.8 (−8.2 to 9.8) |
| Traditional Medicare|| only | 268 | 56.9 (49.9–63.5) | 415 | 61.9 (56.0–67.4) | 5.0 (−3.6 to 13.6) |
| Usual source of care | P < 0.0001 | P < 0.0001 | |||
| Yes | 1252 | 72.6 (69.4–75.5) | 2006 | 76.9 (74.5–79.2) | 4.3 (0.6–8.1) |
| No | 48 | * | 84 | 23.2 (13.8–36.2) | * |
| # Physician visits in prior year | P < 0.0001 | P < 0.0001 | |||
| None | 96 | 34.9 (24.5–47.0) | 140 | 30.0 (21.5–40.0) | −4.9 (−20.1 to 10.2) |
| 1 | 132 | 60.3 (50.2–69.6) | 249 | 66.3 (58.3–73.4) | 6.0 (−6.5 to 18.5) |
| 2–5 | 596 | 74.1 (69.4–78.3) | 956 | 81.1 (77.6–84.1) | 7.0 (1.5–12.5) |
| ≥6 | 474 | 77.2 (72.6–81.2) | 733 | 77.6 (73.8–81.1) | 0.4 (−5.0 to 5.9) |
| Health status | P = 0.0007 | P = 0.0002 | |||
| Excellent/very good/good | 1002 | 73.7 (70.2–76.9) | 1678 | 77.2 (74.5–79.6) | 3.5 (−0.6 to 7.5) |
| Fair/poor | 297 | 60.2 (53.0–67.0) | 411 | 64.0 (57.8–69.8) | 3.8 (−5.2 to 12.9) |
| Cancer history¶ | P = 0.9561 | P = 0.4670 | |||
| Yes | 104 | 71.0 (60.7–79.5) | 189 | 77.3 (68.8–84.0) | 6.3 (−5.1 to 17.8) |
| No | 1196 | 71.3 (68.0–74.3) | 1901 | 74.4 (72.0–76.7) | 3.2 (−0.7 to 7.1) |
Estimate suppressed because of denominator <50 and/or relative SE > 30%.
Includes married or living with partner versus unmarried/not living with partner.
Includes those with other state-sponsored insurance.
Includes military plans, other government plans, or Indian Health Service.
Includes Medicare Part A and/or Part B.
Excluding breast cancer or nonmelanoma skin cancer.
AIAN indicates American Indian/Alaska Native; CI, confidence interval.
Data Source: CDC/NCHS, National Health Interview Survey, 2010 and 2013.
TABLE 3.
Adjusted Proportions of Female Medicare Beneficiaries Aged 65–74 Years Reporting Having Received a Mammogram Within the Prior 2 Years, 2010 and 2013
| %* | 95% CI | P | |
|---|---|---|---|
| Year | |||
| 2010 | 71.3 | 68.3–74.2 | 0.0388 |
| 2013 | 74.8 | 72.6–76.9 | |
Adjusted for age, race, ethnicity, birthplace, marital status, income, insurance, usual source of care, number of visits in prior year, health status, and cancer history.
Data Source: CDC/NCHS, National Health Interview Survey, 2010 and 2013.
Excluding Medicare Advantage enrollees (not shown), before adjustment mammography use increased 4.2 percentage points (95% CI, 0.3–8.0). This increase persisted in multivariable analysis (predictive margins 75.0% vs. 70.9%, P = 0.025).
DISCUSSION
Among female Medicare beneficiaries 65–74 years old, there was a 3.5 percentage point increase in mammography use in 2013 compared with 2010 that was not attributable to differences between years in multiple population socio-demographic, health, and health care access factors. Given the lack of a previous increase in mammography use in this age group or among all age-eligible women since the early-mid 2000s,12,13,28 a small increase is notable. Our trends analysis indicates that although the increase in 2013 is fairly small, it seems to be new compared with earlier years which may support a possible effect from eliminating cost sharing in 2011. However, findings are from a single data year early after the Medicare change. Continued monitoring is needed to confirm findings and if so, to determine whether use will continue to increase.
The finding of increased mammography use is consistent with previous literature on the effect of cost sharing and its elimination on cancer screening use. Although not supported by some,15,16 multiple studies have concluded that cost sharing has a negative effect on use of mammography or other cancer screening tests or preventive services,10,17–19,29 and the effect may be greater for mammography than for other preventive services.19 Elimination of cost sharing has also been associated with increases in use.24,30 Several earlier studies included adults aged younger than 65 years. However, elderly adults may be more susceptible to effects of cost sharing, given that they may be more likely to have chronic conditions which increase out-of-pocket costs for other services.17 Specific to the Medicare population, among Medicare-managed care plan enrollees, mammography use declined between 2002 and 2004 for women enrolled in plans that instituted cost sharing during this time period compared with a modest increase in plans that did not.17 Furthermore, mammography use increased among Medicare fee-for-service beneficiaries after waiver of the Medicare deductible for mammography in 1997.24 Our finding of increased mammography use among Medicare beneficiaries, particularly younger beneficiaries, in 2013 is consistent with these earlier findings about effects of reducing out-of-pocket costs on screening, and expands the evidence to include the recent elimination of Medicare cost sharing for mammography screening. Our findings may suggest that cost may have remained a barrier to screening for some women even after previous reductions in cost sharing.
Although women in our sample were insured and in 2013 were not required to pay out-of-pocket for screening mammography, one quarter of women of screening age did not report having a recent mammogram in 2013. Furthermore, except for unmarried women increases were not observed among groups experiencing screening disparities in 2010 (women with lower income, dual Medicare/Medicaid coverage, or traditional Medicare only, no usual source of care, <2 visits, or fair/poor health status). For measures such as eliminating cost sharing to have the intended effect of increasing access to and utilization of recommended services, beneficiaries must be aware of and understand cost sharing exemptions applicable to them. A study of consumer-directed health plan beneficiaries found that most did not understand that preventive tests were exempted from cost sharing, and for some this created barriers to seeking recommended care.31 Whether this is also an issue for Medicare beneficiaries is uncertain. Additional barriers beyond cost may also exist for some women. Multiple barriers to screening have been described, including patient, provider, and practice or organizational factors. For women, factors such as knowledge, attitudes, awareness, and availability of screening may influence use.32,33 Not receiving a provider recommendation for screening is commonly reported among those not screened,34 and competing demands for provider time may also be an issue.35 Practice or organizational systems to prompt, encourage, and support providers in delivering or referring patients for screening are effective in increasing cancer screening use.32,36 In the current analysis, increases in mammography use did occur among those who had usual sources of care and visited a physician 2–5 times within the prior year. These findings suggest that increases occurred among women who access the health care system and have opportunities to receive recommendations and screening referrals.
Given our study design, we cannot be certain that eliminating cost sharing caused the increase in mammography use. Other temporally related factors may have contributed. Beyond eliminating cost sharing for screening mammography, the Affordable Care Act effected other changes in Medicare during this time, including eliminating cost sharing for the “Welcome to Medicare” physical, and establishing an annual wellness visit free from cost sharing that might include developing personal screening schedules for beneficiaries.20,21 Screening use might have been influenced indirectly through enhanced access to and discussion with providers as a result of these changes rather than directly through reduced mammography cost. Furthermore, USPSTF updated mammography screening guidelines in November 2009. However, the update is unlikely to have played a substantial role in our findings. The increased mammography use was driven by an increase among women in their 60s; no increase was found for women aged 70–74 years. However, guidelines were essentially unchanged for women in their 60s, making it unlikely that revised guidelines contributed to findings.1,37 Evidence from survey data in earlier years suggests that mammography use did not change after the 2009 USPSTF update.23,38
Findings need to be interpreted in light of several limitations. First, our study did not include a comparison group to account for trends unrelated to changes in cost sharing policies. We did not compare mammography use with changes in other cancer screening tests recommended in this age group (eg, colorectal cancer screening) because this screening was also subject to changes in Medicare cost sharing during this time.7,24 We did not separately examine women with Medicare Part A only who may be less likely to receive mammography,39 because there were <30 such women for each year. Second, elimination of cost sharing for some Medicare Advantage plans may not have occurred until 201227 potentially biasing findings toward the null. Exclusion of these beneficiaries did not substantially change findings. Third, data were self-reported. However, we do not expect any differences in mammography reporting to vary by year. Fourth, 2010 and 2013 NHIS response rates were approximately 61% although weights included adjustments for nonresponse. Furthermore, some subgroups were small, leading to wide CIs, estimate imprecision, and reduced power to detect change over time. Percentages in the figure were unadjusted. However, for 2010 and 2013, unadjusted percentages were within 0.2 percentage points of adjusted percentages. Finally, diagnostic mammograms might have been included possibly leading to overestimates of screening use
In summary, there was a modest increase in mammography use from 2010 to 2013 among Medicare beneficiaries aged 65–74 years, which could be consistent with an effect of eliminating cost sharing within Medicare during this time. Findings suggest that eliminating cost sharing might increase use of recommended screening services. For mammography, this increase translates into an additional 390,758 women aged 65–74 years reporting a recent mammogram in 2013 compared with 2010. Continued monitoring of mammography use and confirmation of findings is needed. Our findings for 2013 reflect the initial 2-year screening interval after the change in cost sharing and are therefore relatively short-term results. Lack of increased mammography use for some groups may reflect nonfinancial barriers to care. Future efforts to identify and address such barriers may further increase recommended screening use in this population.
Footnotes
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention or the National Cancer Institute.
All authors are federal government employees.
The National Health Interview Survey and manuscript preparation were funded by the US government.
References
- 1.US Preventive Services Task Force. [Accessed January 29, 2015];Final recommendation statement: breast cancer screening. Available at: http://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/breast-cancer-screening.
- 2.US Cancer Statistics Working Group. United States Cancer Statistics: 1999–2011 Incidence and Mortality Web-based Report. Atlanta: US Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute; 2014. [Google Scholar]
- 3.Medicare.gov. Your Medicare coverage: is my test, item or service covered? [Accessed January 29, 2015];Mammograms. Available at: http://www.medicare.gov/coverage/mammograms.html#1368.
- 4.Blustein J. Medicare coverage, supplemental insurance, and the use of mammography by older women. N Engl J Med. 1995;332:1138–1143. doi: 10.1056/NEJM199504273321706. [DOI] [PubMed] [Google Scholar]
- 5.US Government Accountability Office. [Accessed January 29, 2015];Medicare preventive services: most beneficiaries receive some but not all recommended services. Available at: http://www.gao.gov/new.items/d041004t.pdf.
- 6.Medicare Benefit Policy Manual. [Accessed January 29, 2015];Chapter 15 – Covered Medical and Other Health Services. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/bp102c15.pdf.
- 7.Salloum RG, Kohler RE, Jensen GA, et al. US Preventive Services Task Force recommendations and cancer screening among female Medicare beneficiaries. J Womens Health (Larchmt) 2014;23:211–217. doi: 10.1089/jwh.2013.4421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ayanian JZ, Landon BE, Zaslavsky AM, et al. Racial and ethnic differences in use of mammography between Medicare advantage and traditional Medicare. J Natl Cancer Inst. 2013;105:1891–1896. doi: 10.1093/jnci/djt333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schneider EC, Rosenthal M, Gatsonis CG, et al. Is the type of Medicare insurance associated with colorectal cancer screening prevalence and selection of screening strategy? Med Care. 2008;46:S84–S90. doi: 10.1097/MLR.0b013e31817fdf80. [DOI] [PubMed] [Google Scholar]
- 10.Rezayatmand R, Pavlova M, Groot W. The impact of out-of-pocket payments on prevention and health-related lifestyle: a systematic literature review. Eur J Public Health. 2013;23:74–79. doi: 10.1093/eurpub/cks034. [DOI] [PubMed] [Google Scholar]
- 11.Breslow RA, Rimer BK, Baron RC, et al. Introducing the community guide’s reviews of evidence on interventions to increase screening for breast, cervical, and colorectal cancers. Am J Prev Med. 2008;35:S14–S20. doi: 10.1016/j.amepre.2008.04.005. [DOI] [PubMed] [Google Scholar]
- 12.Sabatino SA, White MC, Thompson TD, et al. Cancer screening test use—United States, 2013. MMWR Morb Mortal Wkly Rep. 2015;64:464–468. [PMC free article] [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention (CDC) Cancer screening—United States, 2010. MMWR Morb Mortal Wkly Rep. 2012;61:41–45. [PubMed] [Google Scholar]
- 14.Carrasquillo O, Lantigua RA, Shea S. Preventive services among Medicare beneficiaries with supplemental coverage versus HMO enrollees, Medicaid recipients, and elders with no additional coverage. Med Care. 2001;39:616–626. doi: 10.1097/00005650-200106000-00009. [DOI] [PubMed] [Google Scholar]
- 15.Busch SH, Barry CL, Vegso SJ, et al. Effects of a cost-sharing exemption on use of preventive services at one large employer. Health Aff (Millwood) 2006;25:1529–1536. doi: 10.1377/hlthaff.25.6.1529. [DOI] [PubMed] [Google Scholar]
- 16.Liang SY, Phillips KA, Tye S, et al. Does patient cost sharing matter? Its impact on recommended versus controversial cancer screening services. Am J Manag Care. 2004;10:99–107. [PubMed] [Google Scholar]
- 17.Trivedi AN, Rakowski W, Ayanian JZ. Effect of cost sharing on screening mammography in Medicare health plans. N Engl J Med. 2008;358:375–383. doi: 10.1056/NEJMsa070929. [DOI] [PubMed] [Google Scholar]
- 18.Guy GP., Jr The effects of cost sharing on access to care among childless adults. Health Serv Res. 2010;45:1720–1739. doi: 10.1111/j.1475-6773.2010.01162.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Solanki G, Schauffler HH. Cost-sharing and the utilization of clinical preventive services. Am J Prev Med. 1999;17:127–133. doi: 10.1016/s0749-3797(99)00057-4. [DOI] [PubMed] [Google Scholar]
- 20.Health Policy Brief: Preventive Services Without Cost Sharing, Health Affairs. 2010 Dec 28; http://www.healthaffairs.org/healthpolicybriefs/brief.php?brief_id=37.
- 21.Congressional Research Service. [Accessed February 11, 2015];Medicare provisions in the patient protection and Affordable Care Act (PPACA): summary and timeline. Available at: https://www.aamc.org/download/133858/data/crstimeline.pdf.pdf.
- 22.Network NCC. [Accessed October 19, 2015];NCCN Clinical Practice Guidelines in Oncology: Breast Cancer. Available at: http://www.nccn.org.
- 23.Howard DH, Adams EK. Mammography rates after the 2009 US Preventive Services Task Force breast cancer screening recommendation. Prev Med. 2012;55:485–487. doi: 10.1016/j.ypmed.2012.09.012. [DOI] [PubMed] [Google Scholar]
- 24.Goodwin SM, Anderson GF. Effect of cost-sharing reductions on preventive service use among Medicare fee-for-service beneficiaries. Medicare Medicaid Res Rev. 2012;2 doi: 10.5600/mmrr.002.01.a03. 002.01.a03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.National Center for Health Statistics. Survey Description, National Health Interview Survey. Hyattsville, MD: National Center for Health Statistics; 2013. [Google Scholar]
- 26.Graubard BI, Korn EL. Predictive margins with survey data. Biometrics. 1999;55:652–659. doi: 10.1111/j.0006-341x.1999.00652.x. [DOI] [PubMed] [Google Scholar]
- 27.US Department of Health and Human Services. [Accessed March 30, 2015];The Affordable Care Act: Strengthening Medicare in 2011. Available at: http://www.cms.gov/apps/files/MedicareReport2011.pdf.
- 28.National Center for Health Statistics. Health, United States, 2013: With Special Feature on Prescription Drugs. Hyattsville, MD: National Center for Health Statistics; 2014. [PubMed] [Google Scholar]
- 29.Solanki G, Schauffler HH, Miller LS. The direct and indirect effects of cost-sharing on the use of preventive services. Health Serv Res. 2000;34:1331–1350. [PMC free article] [PubMed] [Google Scholar]
- 30.Meeker D, Joyce GF, Malkin J, et al. Coverage and preventive screening. Health Serv Res. 2011;46:173–184. doi: 10.1111/j.1475-6773.2010.01188.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Reed ME, Graetz I, Fung V, et al. In consumer-directed health plans, a majority of patients were unaware of free or low-cost preventive care. Health Aff (Millwood) 2012;31:2641–2648. doi: 10.1377/hlthaff.2012.0059. [DOI] [PubMed] [Google Scholar]
- 32.Sabatino SA, Lawrence B, Elder R, et al. Effectiveness of interventions to increase screening for breast, cervical, and colorectal cancers: nine updated systematic reviews for the guide to community preventive services. Am J Prev Med. 2012;43:97–118. doi: 10.1016/j.amepre.2012.04.009. [DOI] [PubMed] [Google Scholar]
- 33.DuBard CA, Schmid D, Yow A, et al. Recommendation for and receipt of cancer screenings among medicaid recipients 50 years and older. Arch Intern Med. 2008;168:2014–2021. doi: 10.1001/archinte.168.18.2014. [DOI] [PubMed] [Google Scholar]
- 34.Meissner HI, Breen N, Taubman ML, et al. Which women aren’t getting mammograms and why? (United States) Cancer Causes Control. 2007;18:61–70. doi: 10.1007/s10552-006-0078-7. [DOI] [PubMed] [Google Scholar]
- 35.Meissner HI, Klabunde CN, Breen N, et al. Breast and colorectal cancer screening: US primary care physicians’ reports of barriers. Am J Prev Med. 2012;43:584–589. doi: 10.1016/j.amepre.2012.08.016. [DOI] [PubMed] [Google Scholar]
- 36.Baron RC, Melillo S, Rimer BK, et al. Intervention to increase recommendation and delivery of screening for breast, cervical, and colorectal cancers by healthcare providers a systematic review of provider reminders. Am J Prev Med. 2010;38:110–117. doi: 10.1016/j.amepre.2009.09.031. [DOI] [PubMed] [Google Scholar]
- 37.US Preventive Services Task Force. Screening for breast cancer: recommendations and rationale. Am Fam Physician. 2002;65:2537–2545. [PubMed] [Google Scholar]
- 38.Pace LE, He Y, Keating NL. Trends in mammography screening rates after publication of the 2009 US Preventive Services Task Force recommendations. Cancer. 2013;119:2518–2523. doi: 10.1002/cncr.28105. [DOI] [PubMed] [Google Scholar]
- 39.Adams EK, Bayakly AR, Berzen AK, et al. Enhancing screening and early detection among women transitioning to Medicare from the NBCCEDP in Georgia. Cancer Causes Control. 2015;26:795–803. doi: 10.1007/s10552-015-0560-1. [DOI] [PMC free article] [PubMed] [Google Scholar]