Abstract
The Program for the Evaluation of the Enrichment of Relational Skills (PEERS), a social skills intervention for high functioning adolescents with autism spectrum disorder (ASD), has been proven efficacious in randomized control trials. However, the effectiveness of the PEERS program in community settings has not been studied. The present small-scale pilot study examined the effectiveness of the PEERS program in a community setting. Five adolescents and their caregivers participated in the PEERS intervention. Results indicated that the adolescents showed significant improvement in their social engagement, social cognition, social communication, social motivation, and knowledge of PEERS skills and concepts from pre- to post-intervention. Furthermore, adolescents showed significant reductions in their internalizing and autistic symptoms from pre- to post-intervention. The findings from this small-scale pilot study support the effectiveness of the PEERS program in community-based settings.
Keywords: Autism spectrum disorder, Social skills, Anxiety, Intervention, Community setting
Introduction
This report presents data from a small-scale pilot study of the PEERS Program, a social skills intervention for adolescents with autism spectrum disorder (ASD), addressing the need for evaluations of evidence-based social skills interventions in community-based settings. Additionally, this pilot study also examined whether PEERS would improve not only participants’ social skills but also their anxiety.
Autism Spectrum Disorder
Autism Spectrum Disorder (ASD) is a neurodevelopmental disorder that is characterized by deficits in social communication and social interaction as well as the presence of stereotyped and restricted patterns of behaviors and interests (American Psychiatric Association 2013). The severity of the symptoms associated with ASD varies significantly across individuals. Generally, individuals with ASD who have average or above average intelligence are referred to as “high functioning” (Gillberg 1998). In addition to impaired social functioning, high functioning youth with ASD often present with comorbid anxiety (e.g., Hallett et al. 2013). High functioning youth with ASD may have a better understanding of their behavioral abnormalities, which may cause them to be vulnerable to experiencing high levels of anxiety (Niditch et al. 2012).
As children reach adolescence, social interactions and peer relationships become increasingly important. However, for adolescents with ASD, social skills deficits may negatively impact their ability to successfully navigate social interactions and form relationships with their peers (Tse et al. 2007). Friendships provide adolescents with several potential benefits. For example, friends can provide emotional support to adolescents during difficult times and serve as a buffer against peer victimization and exclusion (Kenny et al. 2013). Because of their social skills deficits, individuals with ASD, particularly adolescents with ASD, are at risk for a host of negative outcomes such as peer rejection and internalizing problems (Kozlowski et al. 2012).
Effectiveness of Social Skills Interventions
Given that poor social functioning is a hallmark feature of ASD (Kozlowski et al. 2012), developing and testing the efficacy of social skills interventions for individuals with ASD is critical. While some social skills interventions have been proven to be efficacious in research settings using resource-intensive randomized controlled trials (RCTs), it is unclear whether the gains observed in these trials will generalize to routine community-based practice (Dingfelder and Mandell 2011). In general, many interventions for youth with ASD that are proven efficacious in research settings are not effectively implemented in community settings (Brookman-Frazee et al. 2010). Moreover, when interventions that have been proven to be efficacious in university-based RCTs are implemented in community settings, the outcomes tend to be less favorable than those found in controlled studies (Brookman-Frazee et al. 2010). Therefore, there is a growing need for studies examining the generalizability of evidence-based social skills interventions for youth with ASD using community-based studies. Additionally, Mandell and colleagues (2013) proposed that, compared to traditional university-based studies, community-based studies allow community practitioners to utilize the intervention, building capacity in community-based providers and increasing the chances that the organization will adopt the intervention at the conclusion of research participation.
The PEERS Program
The Program for the Evaluation and Enrichment of Relational Skills (PEERS; Laugeson et al. 2009) is a commercially-available and widely-implemented group social skills intervention for high functioning adolescents with ASD (i.e., adolescents diagnosed with ASD without cognitive impairment). The PEERS program is a manualized treatment, meaning that the content and structure of each session is provided to the clinician implementing the intervention. Additionally, scripts or suggested wording for implementation are generally available for each session. The PEERS program is a 14-week treatment that utilizes evidence-based strategies for teaching social skills (e.g., brief didactic instruction). The PEERS program is unique among manualized social skills interventions due to its inclusion of a parent-assisted component (Laugeson et al. 2012).
Several clinical trials have demonstrated the efficacy of the PEERS program in improving the social functioning of adolescents with ASD. For example, Laugeson et al. (2009) found that, compared to a waitlist control group, adolescents who participated in the program showed increased knowledge of social skills, increased frequency of hosted get-togethers with peers, and improved overall social skills as reported by parents (Laugeson et al. 2009), and treatment gains were maintained five years later (Mandelberg et al. 2014). Another study found that adolescents participating in the program improved their social skills knowledge, social responsiveness, and overall social skills in the areas of social communication, social cognition, social awareness, social motivation, assertion, cooperation, and responsibility, while decreasing autistic mannerisms and increasing the frequency of peer interactions (Laugeson et al. 2012). To date, outcomes of the PEERS program have only been evaluated by the program’s developers at the site of program development or in university settings. Therefore, additional research to demonstrate the effectiveness of the PEERS program in community settings is urgently needed.
Additionally, while social skills interventions are not designed to target anxiety, social skills interventions may increase participants’ self-efficacy in social interactions, thereby reducing the anxiety that participants may feel in social interactions. As such, although the PEERS program was not developed to reduce participants’ anxiety symptoms, participants may experience less social anxiety after completing the program. However, only one study (Schohl et al. 2014) has evaluated the impact of the PEERS program on anxiety, indicating that participation in the program resulted in reductions in social anxiety symptoms. Therefore, the current small-scale community-based pilot study aimed to evaluate the effectiveness of the PEERS program not only on improving social skills, but also on reducing anxiety in high functioning adolescents with ASD.
Method
Participants
Participants included 5 middle and high school students with ASD and their caregivers. The adolescents were 13 to 15 years old (M = 13.4; SD = 0.89). All participants had a previous diagnosis of Autistic Disorder based on the Diagnostic and Statistical Manual of Mental Disorders (4th ed., text revision, DSM-IV-TR; American Psychiatric Association 2000) criteria, per parent report. The verbal IQs of the participants, as measured by the Kaufman Brief Intelligence Test-Second Edition (KBIT-2; Kaufman and Kaufman 2004), ranged from 77 to 141 (M = 97; SD = 25.23). Of the 4 male and 1 female participants, 2 of the participants identified as Caucasian, 1 as African American, 1 as Hispanic, and 1 as Asian. Four participants received special education services. Specific information about the special education services that the participants were receiving at school was not collected. Two participants had a co-morbid diagnosis of ADHD, one of whom was prescribed Vyvanse (lisdexamfetamine dimesylate).
Procedures
Participants were recruited from community healthcare providers throughout New Orleans, including the community-based site where the intervention was held. Specifically, letters were mailed to community providers and families who were previously seen at the site where the intervention took place. Eligibility requirements were that the adolescent: (a) was willing to participate in the treatment; (b) had at least one caregiver willing to participate in the treatment; (c) had a previous diagnosis of Autistic Disorder, Asperger’s Disorder, or Pervasive Developmental Disorder, NOS; (d) was between 13 and 17 years old; (e) had social problems as reported by themselves or their parents; (f) was fluent in English; and (g) had a verbal IQ greater than or equal to 70 on the KBIT-2 (Kaufman and Kaufman 2004). Participants were excluded if they had a history of a major mental illness (e.g., schizophrenia), or a visual or physical impairment that would prevent them from participating in outdoor sports activities.
Families interested in participating in the study contacted the site, were screened via telephone, and were invited to an in-person intake session during which caregivers and adolescents completed pre-test measures and adolescents were administered the KBIT-2. Of the 13 families that participated in the intake session, 5 teens were excluded due to having a verbal IQ lower than 70 on the KBIT-2, and 2 families withdrew prior to the start of the intervention due to logistical issues (i.e., lack of reliable transportation and caregiver’s work schedule impeding participation). Following intake, 6 participants began the 14-week PEERS intervention, provided at the community agency, which provides services to predominately low-income families.
The PEERS program
The PEERS program consisted of 14 weekly sessions that lasted 90 min each week. Parent and adolescent sessions were held concurrently in separate rooms. The adolescent group sessions involved didactic lessons on appropriate social skills, role-playing, behavioral rehearsal exercises, and performance feedback. The concurrent parent group sessions involved lessons on assisting teens in the completion of homework assignments, which were designed to allow the adolescents to practice their newly learned skills in natural settings. The didactic lessons involved the presentation of concrete rules and steps and included conversation skills, electronic communication, choosing appropriate friends, appropriate use of humor, entering and exiting a conversation, hosting get-togethers, good sportsmanship, handling teasing and bullying, handling disagreements, handling rumors and gossip. Both parent and adolescent sessions were co-facilitated. The parent sessions were facilitated by a master’s level doctoral student in a school psychology program and a post-doctoral fellow with a Ph.D. from a clinical psychology doctoral program. The adolescent sessions were facilitated by a licensed clinical psychologist and a post-doctoral fellow with a Ph.D. from a school psychology program. It is important to note that none of the group facilitators are certified PEERS providers (i.e., received training from PEERS certified trainers).
Both the parent and adolescent sessions began with a review of the homework assignments from the previous week. In the parent sessions, time was devoted to troubleshooting any issues that may have led to an inability to complete homework assignments. After homework review, the adolescents were presented with the didactic lesson for the week, role-plays of the social skills being taught. The adolescents practiced the newly learned skills in the session and received performance feedback from the adolescent group facilitators. After homework review, the parents were presented with the didactic lesion and provided with a handout that outlined the didactic lesson. Caregivers were also provided instruction on how to maximize their adolescent’s homework completion. At the end of both the parent and adolescent sessions, the homework assignments for the upcoming week were presented to the participants. After reviewing the homework assignments for the upcoming week, the parent and adolescent groups reunited in the same room and the co-facilitators of the adolescent group provided a brief review of the didactic lesson that was presented during the session as well as a review the homework assignments for the upcoming week.
Within the first three sessions of the intervention, the co-facilitators of the adolescent group developed concerns about one adolescent’s readiness and willingness to participate in the intervention. After discussing their concerns with the co-facilitators of the parent group, the facilitators met with the adolescent’s caregivers and suggested that the adolescent may be better served by receiving individual services. Therefore, the family withdrew from the study after attending the first four sessions of the intervention and pursued individualized services. As such, of the 6 families that were initially enrolled in the study, 5 families completed the study. Caregivers and adolescents completed the post-test measures 2 to 3 days after the last PEERS session.
Measures
Social Skills Improvement System (SSIS; Gresham and Elliot 2008)
The parent form of the SSIS was completed by caregivers at pre- and post-test to assess their adolescent’s social skills and problem behaviors. The SSIS yields standard scores for each major domain (i.e., social skills and problem behaviors) as well as scores for each of the subscales that comprise the major domains. The SSIS has good reliability (Gresham and Elliot 2008). Coefficient alphas for the scale scores (i.e., Social Skills and Problem Behaviors) were in the .90s. For the subscales, the coefficient alphas were in the .80s. Additionally, the SSIS demonstrates concurrent validity with the Behavior Assessment System for Children, Second Edition (Reynolds and Kamphaus 2004) and the Vineland Adaptive Behavior Scales, Second Edition (Sparrow et al. 2005).
Social Responsiveness Scale, Second Edition (SRS-2; Constantino and Gruber 2012)
The SRS-2 is a commonly used 65-item measure that assesses the severity of autism spectrum symptoms. The SRS-2 yields a total score and five subscale scores, with higher scores indicating greater autism related symptomatology. The SRS-2 has satisfactory reliability, with the coefficient alphas of the SRS Total score ranging from .93 to .97 for the normative and clinical samples (Booker and Starling 2011). The coefficient alphas of the subscales ranged from .77 (Social Awareness) to .90 (Autistic Mannerisms). Caregivers completed the SRS at pre- and post-test.
Test of adolescent social skills knowledge (TASSK; Laugeson et al. 2009)
The TASSK is a 26-item measure that was developed by the developers of the PEERS program. The TASSK was completed by the adolescents at pre- and post-test to test their knowledge of specific, key social skills that are taught during the intervention. Scores on the TASSK range from 0 to 26, with higher scores reflecting greater knowledge of the social skills taught during the intervention. The developers of the TASSK reported a coefficient alpha of 0.56 for the TASSK and indicated that this alpha is acceptable given the broad domain of questions on the measure (Laugeson et al. 2009).
Quality of play questionnaire (QPQ; Frankel and Mintz 2011)
The QPQ was developed through factor analysis and includes two items that measure the frequency of hosted and invited get-togethers that an adolescent has had over the previous month. Because the total get-togethers variable only consists of two items, coefficient alpha was not computed in the current study. The QPQ was completed by caregivers and adolescents at pre- and post-test.
Screen for Child Anxiety Related Disorders (SCARED; Birmaher et al. 1997)
The SCARED is a 41-item measure that assesses anxiety symptoms in children and adolescents and has five scales that are designed to map onto specific DSM-IV-TR anxiety disorders (i.e., generalized anxiety disorder, panic disorder, social anxiety, and separation anxiety disorder) as well as symptoms related to school phobias. In addition to the five scale scores, the SCARED yields a total score that can range from 0 to 82, with higher scores reflecting greater levels of anxiety. The SCARED has adequate internal consistency, with coefficient alphas for the total score and the five scale scores ranging from .74 to .93 (Birmaher et al. 1997). The SCARED also demonstrates good discriminate validity within anxiety disorders and between anxiety disorders and other disorders. Adolescents completed the SCARED at pre- and post-test.
Treatment Fidelity
Treatment fidelity was monitored in vivo by two research assistants, with one research assistant monitoring treatment fidelity in the parent sessions and one research assistant monitoring treatment fidelity in the adolescent sessions. Additionally, the co-facilitators of the parent session and one co-facilitator of the adolescent groups monitored treatment fidelity in vivo. Treatment fidelity was monitored through weekly fidelity checklists that were created from the treatment manual. The fidelity checklists outlined the specific events that should have occurred during a given treatment session (e.g., therapist reviewed homework assignments with the participants – followed by a list of the homework assignments from the previous session). The research assistants and the facilitators circled “yes” if the event happened during the session and “no” if the event did not occur during the session.
The percentage of agreement between the facilitators and the research assistants were calculated separately for the parent and adolescent groups by dividing the total number of agreements by the total number of data points for each of the groups. There was perfect agreement between the fidelity ratings of the co-facilitators of the parent group and the research assistant who monitored treatment fidelity in the parent sessions. For the adolescent sessions, there was only one instance in which the research assistant and the co-facilitator of the teen group disagreed on whether or not an event occurred during a session, resulting in 99% agreement between the two raters (i.e., the ratings were consistent for 84 out of 85 data points). The facilitators of the parent and adolescent sessions delivered the intervention with a high level of integrity, with fidelity checks yielding 100% fidelity in the parent sessions (i.e., all of the events outlined in the fidelity checklists occurred during each of the 14 sessions) and 99% fidelity in the adolescent sessions (i.e., all but one of the events outlined in the fidelity checklists occurred in each of the 14 sessions).
Results
Results from paired samples t-tests are presented in Table 1. Adolescents’ social engagement significantly increased from pre- to post-intervention. Internalizing symptoms, measured by the SSIS Internalizing scale, and autism symptomatology, measured by the SSIS Autism Spectrum scale and the SRS-2, showed a significant improvement from pre- to post-intervention. Additionally, there were significant improvements in adolescents’ social cognition, social communication, and social motivation, as measured by the SRS-2, from pre- to post-intervention. Adolescents’ knowledge of the specific social skills taught during the intervention significantly improved, as measured by the TASSK. Given the small sample size, sensitivity analyses were conducted to determine whether one participant was driving the significant results (see Table 2). Effect sizes were also evaluated. For the variables of interest, the strength of the effect sizes for the mean change scores on the outcome variables in this study were small to large and, with the exception of self-control, were in the expected direction (see Table 1). Moreover, most effect sizes were comparable to the effect sizes for the mean change scores calculated from the published PEERS efficacy studies (Laugeson et al. 2009; Schohl et al. 2014). Notably, the intervention had a large effect on not only the number of get-togethers that adolescents hosted, but also the number of get-togethers that the adolescents were invited to from pre- to post-intervention.
Table 1.
Mean pre- and post-intervention scores, standard deviations, and effect sizes for outcome variables (N = 5)
| Outcome | Pre-test | Post-test | t | Cohen’s d | ||
|---|---|---|---|---|---|---|
|
| ||||||
| M (SD) | M (SD) | Current Study | Laugeson et al. (2009) | Schohl et al. (2014) | ||
| SSiS Social Skills | 77.8 (13.4) | 85.2 (20.7) | 1.89 | 0.42 | 0.89 | 0.71 |
| SSiS Problem Behaviors | 123.8 (14.0) | 113.8 (10.3) | −1.77 | 0.82 | 0.47 | |
| SSiS Communication | 11.4 (2.3) | 13 (3.5) | 1.97 | 0.54 | ||
| SSiS Cooperation | 11 (2.3) | 12.4 (2.6) | 1.36 | 0.57 | ||
| SSiS Assertion | 10.2 (7.1) | 12 (6.0) | 1.23 | 0.27 | ||
| SSiS Responsibility | 11 (1.9) | 11 (4.5) | 0 | 0 | ||
| SSiS Empathy | 9 (2.6) | 12 (4.5) | 2.12 | 0.81 | ||
| SSiS Engagement | 7 (3.9) | 10.4 (4.9) | 2.92* | 0.77 | ||
| SSiS Self-Control | 11.4 (1.1) | 9.8 (3.3) | −0.85 | 0.65 | ||
| SSiS Externalizing | 9.8 (4.3) | 8.6 (2.1) | −0.53 | 0.36 | ||
| SSiS Bullying | 2.2 (1.9) | 1.4 (1.7) | −0.75 | 0.44 | ||
| SSiS Hyperactivity/Inattention | 10 (5.0) | 7.6 (2.6) | −1.31 | 0.61 | ||
| SSiS Internalizing | 12 (4.1) | 8.2 (4.8) | −2.73* | 0.85 | ||
| SSiS Autism Spectrum | 22.6 (5.1) | 16.4 (7.0) | −4.84** | 1.01 | ||
| SRS-2 Total | 79.8 (11.9) | 66.2 (12.4) | −5.87** | 1.12 | 1.38 | |
| SRS-2 Social Awareness | 68.2 (10.5) | 64 (6.6) | −1.36 | 0.48 | ||
| SRS-2 Social Cognition | 73.2 (11.8) | 61.6 (11.5) | −3.02* | 0.99 | 1.09 | |
| SRS-2 Social Communication | 80.4 (9.4) | 64.6 (12.8) | −6.18** | 1.41 | 0.81 | |
| SRS-2 Social Motivation | 73.8 (12.7) | 63.6 (12.3) | −4.05* | 0.82 | 0.72 | |
| SRS-2 Restricted Interests/Behaviors | 78.2 (16.0) | 68.8 (14.3) | −2.39 | 0.62 | 2.25 | |
| SCARED Total | 16 (14.8) | 9.4 (7.9) | −1.66 | 0.56 | ||
| TASSK | 11.4 (6.3) | 20.2 (1.3) | 3.64* | 1.92 | 3.21 | 2.96 |
| QPQ-P: Hosted Get-Togethers | 0.5 (1.0) | 2.75 (2.2) | 2.64 | 1.31 | 0.91 | |
| QPQ-A: Hosted Get-Togethers | 0.4 (0.9) | 3 (2.9) | 2.15 | 1.21 | 1.14 | 0.69 |
| QPQ-P: Invited Get-Togethers | 0 (0) | 1.40 (1.14) | 2.75 | 1.74 | 0.29 | |
| QPQ-A: Invited Get-Togethers | 0 (0) | 1.20 (1.30) | 2.06 | 1.30 | 0.72 | |
On the SRS-2, higher scores indicate greater autism symptomatology. Cohen’s d: small (0.2), medium (0.5), and large (0.8)
p < .05,
p < .01
Table 2.
Participants’ difference scores on selected outcomes
| Participant | SSiS Internalizing |
SSiS Autism Spectrum |
SSiS Total |
SRS- 2 Total |
TASSK | QPQ-P: Hosted Get- Togethers |
QPQ-A Hosted Get- Togethers |
QPQ-P: Invited Get- Togethers |
QPQ-A: Invited Get- Togethers |
|---|---|---|---|---|---|---|---|---|---|
| 1 | −9.00 | −10.00 | 11.00 | −16.00 | 3.00 | 4 | 7 | 3 | 3 |
| 2 | −2.00 | −4.00 | 3.00 | −6.00 | 14.00 | 3 | 3 | 2 | 2 |
| 3 | −4.00 | −6.00 | 10.00 | −20.00 | 3.00 | 0 | 0 | 0 | 0 |
| 4 | −1.00 | −3.00 | −5.00 | −12.00 | 13.00 | 0 | 1 | 1 | 1 |
| 5 | −3.00 | −8.00 | 18.00 | −14.00 | 11.00 | 2 | 2 | 1 | 0 |
Difference scores measure change in scores from pre- to post-test
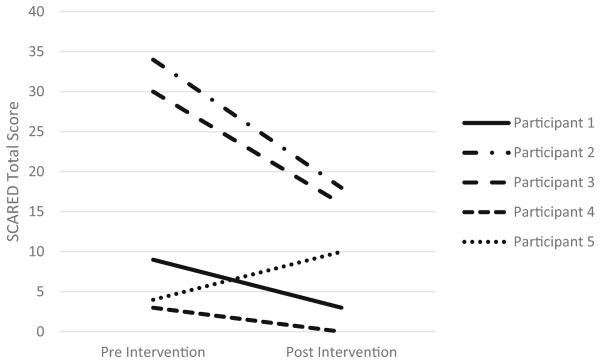
While the paired-samples t-test failed to reveal a significant decrease in pre- to post-anxiety as measured by the SCARED, SCARED Total scores generally decreased for most participants (see Fig. 1). Furthermore, the two participants with clinical levels of anxiety (i.e., a SCARED Total score > 25) prior to the intervention reported non-clinical levels of anxiety at post-test.
Fig. 1.
Participants’ changes in SCARED scores from pre- to post-PEERS intervention; scores >25 indicate clinical levels of anxiety
Additionally, when families completed post-test measures, caregivers reported that they were highly satisfied with the content and the delivery of the intervention. For example, one caregiver reported that her community had very few resources to support her family and adolescent and as a result, she was unable to obtain high-quality treatment for her adolescent in their small community. This family drove two hours roundtrip to participate in the intervention and expressed interest in participating in future social skills groups at the community agency.
Discussion
This independent small-scale pilot study, utilizing community providers to deliver the PEERS intervention in a community setting that provides assessment and intervention services to youth with ASD, provides preliminary support for the effectiveness of the PEERS program in community-based care for improving the social functioning of high functioning adolescents with ASD. Most of the published efficacy trials of the PEERS program were conducted by the developers of the PEERS programs (Laugeson et al. 2009, 2012), conducted at universities (e.g., Karst et al. 2015), or were delivered by at least one group facilitator who was certified in providing PEERS (e.g., Schohl et al. 2014). To our knowledge, this study is the first pilot effectiveness study to be reported in the literature that was conducted in a community setting by providers who were neither affiliated with the developers of the PEERS program nor certified in providing PEERS. Notably, effect sizes for changes in outcomes, including social skills, problem behaviors, and autism symptom severity, were largely comparable to findings reported in the university-based RCTs. Finally, participant feedback and facilitator fidelity suggest that the PEERS program is both acceptable to families seeking treatment in the community and that the intervention can be provided at a high rate of fidelity by providers in community-based settings.
Although reducing anxiety is not a direct target of the PEERS program, our findings are consistent with the findings of Schohl et al. (2014), which indicated that participation in the PEERS program also leads to reductions in social anxiety. However, Schohl et al. (2014) only measured social anxiety, whereas our measure of anxiety assessed several types of anxiety, including social anxiety. In the current study, four of the five participants demonstrated a decrease in their total anxiety score from pre- to post-test. Further analysis of the SCARED scores of these four participants showed reductions in social and separation anxiety for all four participants, panic symptoms for two of the four participants, generalized anxiety for one of the four participants, and school avoidance for two of the four participants. It is important to note that one participant showed an increase in anxiety from pre- to post-test. Specifically, the adolescent’s total SCARED score increased from 4 to 10. Notably, the adolescent experienced an increase in generalized anxiety, separation anxiety, and school avoidance but no increase in social anxiety. It is possible that the increase in anxiety for this adolescent was due to other factors such as the presence of family stressors.
The current study has several limitations that should be considered. First, our findings are limited because this study lacked a control group, which hinders our ability to confidently state that the intervention resulted in the differences in participants’ pre- and post-intervention scores, as other factors may have led to the observed treatment gains. Future studies should utilize more rigorous methodologies so causal statements between the intervention and the outcomes can be made. Second, our pilot study had a small sample size, resulting in insufficient statistical power to detect smaller effects that may be clinically meaningful. Thus, follow-up studies with larger samples are needed to detect smaller effects. Third, and in line with base rates of ASD, our sample was predominantly male. Future studies should include a more diverse sample of participants. Fourth, we did not collect observational data or data to examine if the treatment gains observed were maintained and generalized across settings. Caregiver ratings of the adolescents’ behavior may have been biased due their participation in the intervention, thus observations of the adolescents’ social behaviors in naturalistic settings would allow researchers to obtain more objective ratings of the adolescents’ behaviors. Future community-based studies should include observational measures and long-term follow-up measures to assess the validity, maintenance, and generalization of treatment gains. Finally, the lack of at least one certified PEERS provider may have impacted the delivery of the intervention (i.e., the delivery of the intervention may have differed from how providers who have been trained in the PEERS program typically deliver the intervention). However, in light of these limitations, our findings are promising and lend support for the effectiveness of the PEERS program in routine clinical practice.
Acknowledgments
The authors would like to thank Claire Burns and Morgan Sexton for serving as coaches in the treatment sessions and assisting with monitoring treatment fidelity.
Footnotes
Compliance with Ethical Standards
Ethical Approval All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent During the in-person intake session and prior to the completion of pre-test measures, consent and assent forms were reviewed and completed with interested participants.
Conflict of Interest Trenesha Hill declares that she has no conflict of interest. Sarah Gray declares that she has no conflict of interest. Courtney Baker declares that she has no conflict of interest. Koren Boggs declares that she has no conflict of interest. Elizabeth Carey declares that she has no conflict of interest. Corinn Johnson declares that she has no conflict of interest. Jodi Kamps declares that she has no conflict of interest. R. Enrique Varela declares that he has no conflict of interest.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5. Washington, DC: Author; 2013. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 2000. text rev. [Google Scholar]
- Birmaher B, Khetarpal S, Brent D, Cully M, Balach L, Kaufman J, Neer SM. The screen for child anxiety related emotional disorders (SCARED): Scale construction and psychometric characteristics. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36(4):545–553. doi: 10.1097/00004583-199704000-00018. [DOI] [PubMed] [Google Scholar]
- Booker KW, Starling L. Test review: Social responsiveness scale by J. N. Constantino and C. P. Gruber. Assessment for Effective Intervention. 2011;36(3):192–194. doi: 10.1177/1534508410380134. [DOI] [Google Scholar]
- Brookman-Frazee LI, Taylor R, Garland AF. Characterizing community-based mental health services for children with autism spectrum disorders and disruptive behavior problems. Journal of Autism and Developmental Disorders. 2010;40(10):1188–1201. doi: 10.1007/s10803-010-0976-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Constantino JN, Gruber CP. Social responsiveness scale – Second edition (SRS-2) Torrance, CA: Western Psychological Services; 2012. [Google Scholar]
- Dingfelder H, Mandell D. Bridging the research-to-practice gap in autism intervention: An application of diffusion of innovation theory. Journal of Autism and Developmental Disorders. 2011;41(5):597–609. doi: 10.1007/s10803-010-1081-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frankel F, Mintz J. Maternal reports of play dates of clinic referred and community children. Journal of Child and Family Studies. 2011;20(5):623–630. doi: 10.1007/s10826-010-9437-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillberg C. Asperger syndrome and high-functioning autism. The British Journal of Psychiatry: The Journal of Mental Science. 1998;172:200–209. doi: 10.1192/bjp.172.3.200. [DOI] [PubMed] [Google Scholar]
- Gresham F, Elliott S. Social skills improvement system rating scales manual. Minneapolis, MN: NCS Pearson; 2008. [Google Scholar]
- Hallett V, Lecavalier L, Sukhodolsky DG, Cipriano N, Aman MG, McCracken JT, et al. Exploring the manifestations of anxiety in children with autism spectrum disorders. Journal of Autism and Developmental Disorders. 2013;43(10):2341–2352. doi: 10.1007/s10803-013-1775-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karst JS, Van Hecke AV, Carson AM, Stevens S, Schohl K, Dolan B. Parent and family outcomes of PEERS: A social skills intervention for adolescents with autism spectrum disorder. Journal of Autism and Developmental Disorders. 2015;45(3):752–765. doi: 10.1007/s10803-014-2231-6. [DOI] [PubMed] [Google Scholar]
- Kaufman AS, Kaufman NL. Kaufman brief intelligence test. 2. Bloomington, MN: Pearson; 2004. [Google Scholar]
- Kenny R, Dooley B, Fitzgerald A. Interpersonal relationships and emotional distress in adolescence. Journal of Adolescence. 2013;36(2):351–360. doi: 10.1016/j.adolescence.2012.12.005. [DOI] [PubMed] [Google Scholar]
- Kozlowski AM, Matson JL, Belva BC. Social skills differences between the autism spectrum disorders. Journal of Developmental and Physical Disabilities. 2012;24(2):125–134. doi: 10.1007/s10882-011-9260-2. [DOI] [Google Scholar]
- Laugeson EA, Frankel F, Gantman A, Dillon AR, Mogil C. Evidence-based social skills training for adolescents with autism spectrum disorders: The UCLA PEERS program. Journal of Autism and Developmental Disorders. 2012;42(6):1025–1036. doi: 10.1007/s10803-011-1339-1. [DOI] [PubMed] [Google Scholar]
- Laugeson EA, Frankel F, Mogil C, Dillon AR. Parent-assisted social skills training to improve friendships in teens with autism spectrum disorders. Journal of Autism and Developmental Disorders. 2009;39(4):596–606. doi: 10.1007/s10803-008-0664-5. [DOI] [PubMed] [Google Scholar]
- Mandelberg J, Frankel F, Cunningham T, Gorospe C, Laugeson EA. Long- term outcomes of parent-assisted social skills intervention for high-functioning children with autism spectrum disorders. Autism. 2014;18(3):255–263. doi: 10.1177/1362361312472403. [DOI] [PubMed] [Google Scholar]
- Mandell DS, Stahmer AC, Shin S, Xie M, Reisinger E, Marcus SC. The role of treatment fidelity on outcomes during a randomized field trial of an autism intervention. Autism. 2013;17(3):281–295. doi: 10.1177/1362361312473666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niditch LA, Varela RE, Kamps JL, Hill T. Exploring the association between cognitive functioning and anxiety in children with autism spectrum disorders: The role of social understanding and aggression. Journal of Clinical Child and Adolescent Psychology. 2012;41(2):127–137. doi: 10.1080/15374416.2012.651994. [DOI] [PubMed] [Google Scholar]
- Reynolds CR, Kamphaus RW. Behavior assessment system for children. 2. Circle Pines, MN: AGS; 2004. [Google Scholar]
- Schohl KA, Van Hecke AV, Carson AM, Dolan B, Karst J, Stevens S. A replication and extension of the PEERS intervention: Examining effects on social skills and social anxiety in adolescents with autism spectrum disorders. Journal of Autism and Developmental Disorders. 2014;44(3):532–545. doi: 10.1007/s10803-013-1900-1. [DOI] [PubMed] [Google Scholar]
- Sparrow SS, Cicchetti DV, Balla DA. Vineland adaptive behavior scales: Second edition (Vineland II), survey interview form/caregiver rating form. Livonia, MN: Pearson Assessments; 2005. [Google Scholar]
- Tse J, Strulovitch J, Tagalakis V, Meng L, Fombonne E. Social skills training for adolescents with asperger syndrome and high-functioning autism. Journal of Autism and Developmental Disorders. 2007;37(10):1960–1968. doi: 10.1007/s10803-006-0343-3. [DOI] [PubMed] [Google Scholar]