Abstract
BACKGROUND
Greater ambulatory blood pressure variability (ABPV) is associated with end-organ damage and increased mortality. Age-related changes in the cardiovascular and autonomic nervous systems make age-associated increases in ABPV likely. Cross-sectional studies support this hypothesis, showing greater ABPV among older compared to younger adults. The only longitudinal study to examine changes in ABPV, however, found ABPV decreased over 5 years follow-up. This unexpected observation probably reflected the highly selected nature of the study participants.
METHODS
In this longitudinal study, we assessed changes in ABPV over 10 years in a community-cohort of older people. In addition, we examined the extent to which ABPV was predicted by demographics, cardiovascular risk factors, and medication. Clinical examination and 24-hour ambulatory blood pressure monitoring were carried out at baseline and at 10 years follow-up in 83 people, median age 70 years. ABPV was calculated using SD and coefficient of variation (Cv). Three time periods were examined: daytime, nighttime, and 24 hours.
RESULTS
Daytime and 24-hour, systolic and diastolic, SD, and Cv were significantly greater at follow-up than at baseline ( P < 0.001 in all cases). Mean BP did not change.
CONCLUSIONS
Multilevel modeling showed follow-up interval had a significant, positive effect on SD and Cv ( P < 0.004), independent of age, sex, and medication.
ABPV increased over a 10-year follow-up despite stable mean BP. ABPV may therefore be an additional target for treatment in older people. Future studies should examine what degree of ABPV is harmful and if control of ABPV reduces adverse outcome.
Keywords: aging, ambulatory blood pressure variability, blood pressure monitoring, hypertension, longitudinal study.
Ambulatory blood pressure monitors (ABPMs) record mean blood pressure (BP) and BP variability. Current UK guidelines recommend routine use of ABPM in the diagnosis of hypertension. 1 , 2 Mean ambulatory BP is a well-recognized predictor of cardiovascular and all-cause mortality. 3–8 More recently it has been recognized that ambulatory BP variability (ABPV) also carries important prognostic information independent of mean BP. Increased ABPV is associated with: carotid artery damage, progression of small vessel disease, cognitive decline, left ventricular hypertrophy, increased cardiovascular events, and increased all-cause mortality. 9–17
It is now widely accepted that mean systolic BP increases with age. However few studies have examined how ABPV changes as people get older. A small number of cross-sectional studies have found that ABPV is higher in older adults compared to younger adults. 10 , 18 , 19 This is in keeping with previous studies that have shown that increased ABPV is associated with decreased baroreceptor sensitivity 20–23 and that baroreceptor sensitivity decreases with age. 24 , 25 It is, therefore, surprising that the only longitudinal study to examine ABPV found ABPV decreased over a 5-year follow-up. 26
Great strides have been made in controlling mean BP. Mean BP and BP variability are correlated but it is not clear if control of mean BP inevitably stabilizes BP variability. Recent studies have suggested that calcium channel blockers and diuretics have greater impact on ABPV compared to other antihypertensive classes and animal studies have shown that reduction in ABPV to be associated with decreased end-organ damage. 27–29
These data suggest that monitoring and controlling ABPV maybe an additional method of moderating cardiovascular risk. It is therefore important to understand how ABPV changes overtime, its relationship to change in mean BP and if there are antihypertensive class effects on ABPV.
We hypothesize that age-related changes in the cardiovascular and autonomic nervous systems, resulting in decreased baroreflex sensitivity and increased neurocardiovascular instability, will result in increased ABPV over time and that Goldstein’s unexpected findings reflected an unrepresentative exceptionally healthy older population. 26
This longitudinal study aimed to assess changes in ABPV over a 10-year follow-up and examined if these changes were associated with mean BP or prescribed antihypertensive medication.
METHODS
Between April 2002 and October 2003, 353 community-dwelling people aged 65 years and older took part in the first phase of a longitudinal study examining neurocardiovascular function in older people. Participants were recruited from a single general practice in the North of England. Persons living in residential care were excluded. Full details of recruitment have been previously described elsewhere. 30
Participants were followed-up at 2, 5 and 10 years. Clinical examination and ambulatory BP monitoring was only included in the baseline assessment, in 2002, and the 2012 assessment.
Ambulatory blood pressure monitoring
Consenting participants were fitted with a 24-hour BP monitor (Spacelabs 90207; Spacelabs Medical, Redmond, WA). An appropriate sized cuff was fitted to the nondominant arm. Subjects were instructed to relax their arm when the cuff was inflating. Monitors were programmed to take a BP recording every 30 minutes during the day (7 am to 10 pm ) and every hour overnight (10 pm to 7 am ). If the monitor failed to obtain a BP recording on the first attempt, it would automatically retry the measurement 2 minutes later.
Three time periods were examined: daytime (10 am to 8 pm ), nighttime (midnight to 6 am ), and the full 24-hour period. 31 Only studies with at least 16 recordings within 24 hours were included in the analysis. Studies with 10 or more daytime recordings were deemed suitable for daytime analysis and studies with 5 or more nighttime recordings were deemed suitable for nocturnal analysis. 31
Mean systolic and diastolic BP were calculated for each time period. BP variability was calculated using the SD of the mean BPs. The coefficient of variation (Cv) of BP (SD/mean BP) was also calculated for each time period.
Clinical assessment
Past medical history was obtained by direct interview of subjects. Particular attention was paid to presence or absence of cardiovascular disease and risk factors. If participants were unsure of their past medical history, general practice medical notes were reviewed.
Participants were asked to bring a list of all medications they were taking with them to the assessment. Use of cardioactive medication was defined as using any antihypertensive medication, diuretic, anti-anginal, or anti-arrhythmic. Height and weight were recorded and body mass index was calculated.
Follow-up examination
In 2011, surviving participants were invited to take part in a follow-up study if they remained registered with the participating general practice and had not withdrawn from the study at the 2-year or 5-year follow-up assessments. Ten-year follow-up included; clinical assessment and ambulatory BP, measured as described at baseline.
Ethical approval
Ethical approval for the baseline study was provided by the County Durham and Darlington Local Research Ethics Committee. Ethical approval for the follow-up study was granted by the National Research Ethics Service Committee North East-Newcastle and North Tyneside One. All participants gave written informed consent.
Analysis
Data were analyzed using Statistical Package for Social Science (SPSS) version 19 and R 32 with lme433 and lmerTest34 packages. For all tests, the level of statistical significance was set at <0.05.
Categorical data are displayed as frequency and percentage. Chi square and Fisher’s exact tests were used, as appropriate, to test for differences in the distribution of categorical data.
Normally distributed, continuous data are displayed using mean and SD. Nonparametric data are displayed using median and interquartile range. Normally distributed data from 2 unrelated samples were compared using the Student’s t -test for independent samples. Repeated measures from 2 related samples were compared using paired t -tests.
Multilevel modeling with test sessions grouped by participant was used to examine if BP variability was affected by session independent of age, sex, medication, and mean BP. The models included a random intercept term by participant.
RESULTS
Study participants
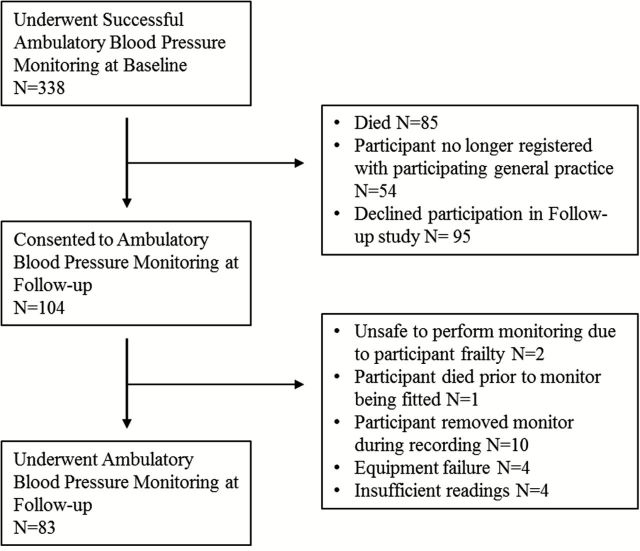
At baseline, 338 participants underwent ambulatory BP monitoring. At follow-up 104 of these participants consented to participation in the study, 83 of whom underwent successful repeat ambulatory BP monitoring. Figure 1 shows the details of recruitment. Participants lost to follow-up (either due to death or withdrawal from the study) were significantly older than participants who took part in the follow-up examination (median (interquartile range) 74 (69–78) vs. 70 (67–73), P < 0.001]. Prevalence of ischemic heart disease, diabetes, hypertension, use of tobacco, and use of antihypertensive medication at baseline did not significantly differ between groups ( Table 1 ). Class of antihypertensive medication prescribed did not differ between groups ( Supplementary Table 1 ). Participants lost to follow-up had significantly greater 24-hour and nighttime mean systolic BP, daytime systolic BP variability, and diastolic variability compared to those participating in the follow-up examination ( Table 1 ).
Figure 1.
Flow chart demonstrating recruitment.
Table 1.
Comparison of baseline characteristics for follow-up participants and those lost to follow up
| Dependent variable | Lost to follow-up N = 255 | Follow-up participants N = 83 | P |
|---|---|---|---|
| Age (median (IQR)) | 74.0 (69.0, 78.0) | 70.0 (67.0, 73.0) | <0.001 |
| BMI (median (IQR)) | 26.2 (24.0, 28.9) | 26.8 (24.7, 296) | 0.159 |
| Pack years (median (IQR)) | 4.0 (0, 25.0) | 3.5 (0, 21.8) | 0.791 |
| Male (frequency (%)) | 144 (56) | 46 (56) | 0.867 |
| IHD (frequency (%)) | 69 (27) | 16 (20) | 0.156 |
| Hypertension (frequency (%)) | 123 (48) | 37 (45) | 0.562 |
| Diabetes (frequency (%)) | 21 (8) | 2 (2) | 0.067 |
| Antihypertensive med (frequency (%)) | 119 (78) | 38 (46) | 0.889 |
| Baseline 24hr mean SBP (mean ± SD) | 130.49±13.98 | 126.40±14.27 | 0.021 |
| Baseline 24hr mean DBP (mean ± SD) | 71.98±7.30 | 72.18±9.67 | 0.861 |
| Baseline 24hr SD SBP (mean ± SD) | 13.95±3.75 | 12.95±3.29 | 0.032 |
| Baseline 24hr SD DBP (mean ± SD) | 9.68±2.23 | 9.34±2.37 | 0.227 |
| Baseline day SBP (mean ± SD) | 135.15±14.40 | 131.35±16.06 | 0.043 |
| Baseline day DBP (mean ± SD) | 75.73±7.95 | 76.46±10.91 | 0.581 |
| Baseline day SD SBP (mean ± SD) | 12.55±4.22 | 11.24±3.40 | 0.010 |
| Baseline day SD DBP (mean ± SD) | 8.36±2.39 | 7.71±2.24 | 0.032 |
| Baseline night mean SBP (mean ± SD) | 120.27±16.09 | 115.55±13.04 | 0.012 |
| Baseline night mean DBP (mean ± SD) | 64.34±8.32 | 63.55±8.69 | 0.483 |
| Baseline night SD SBP (mean ± SD) | 9.31±3.85 | 8.51±3.68 | 0.107 |
| Baseline night SD DBP (mean ± SD) | 7.13±3.07 | 6.73±2.77 | 0.303 |
Normally distributed data compared using Student’s T -test. Nonparametric data compared using Mann–Whitney U -test. Chi square test and Fisher’s exact test used for categorical data. Bold values indicate P -value <0.05.
Abbreviations: IQR, interquartile range; BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; IHD, ischemic heart disease.
Median numbers of ABPM readings during the 24-hour period at baseline and follow-up was 37 (range 20–40) and 35 (range 18–40) respectively. For the daytime period median number of readings at baseline and follow-up were 19 (range 10–20) and 18 (range 10–20) respectively and for the nighttime period the median number was 6 (range 5–6) at both baseline and follow-up.
Changes in ambulatory blood pressure over time
Data from the 83 participants with BP recordings at baseline and follow-up were analyzed. Mean BP did not significantly differ between baseline and follow-up for any of the time periods examined ( Table 2 ). Twenty-four-hour and daytime systolic and diastolic BP SD were significantly greater at follow-up than at baseline ( Table 3 ). Similarly, 24-hour and daytime systolic and diastolic Cv were significantly greater at follow-up compared to baseline ( Table 3 ). None of the nighttime measures of variability significantly differed between baseline and follow-up.
Table 2.
Comparison of mean BP at baseline and follow-up
| Entire follow-up cohort | Participants not taking cardioactive medication | |||||||
|---|---|---|---|---|---|---|---|---|
| Dependent variable | Baseline | Follow-up | Baseline | Follow-up | ||||
| N | Mean ± SD | Mean ± SD | P | N | Mean ± SD | Mean ± SD | P | |
| 24hr mean systolic pressure | 83 | 126.40±14.27 | 123.69±11.80 | 0.139 | 19 | 119.68±11.59 | 126.63±13.00 | 0.004 |
| 24hr mean diastolic pressure | 83 | 72 .18±9.67 | 71.92±8.24 | 0.820 | 19 | 69.68±9.47 | 72.79±9.84 | 0.082 |
| Day mean systolic pressure | 76 | 131.18±16.16 | 127.71±12.25 | 0.060 | 17 | 125.35±11.26 | 133.53±12.74 | 0.005 |
| Day mean diastolic pressure | 76 | 77.96±11.05 | 75.18±8.33 | 0.120 | 17 | 74.88±10.25 | 77.94±9.00 | 0.126 |
| Night mean systolic pressure | 65 | 116.20±13.31 | 113.85±13.37 | 0.290 | 13 | 108.17±11.58 | 113.58±10.92 | 0.008 |
| Night mean diastolic pressure | 65 | 63.72±9.16 | 64.05±8.95 | 0.733 | 13 | 59.25±7.53 | 62.42±6.43 | 0.093 |
Paired T -tests used to compare mean BP at baseline and follow-up. Analysis shown for participants who had ABPM recordings at baseline and follow-up and a subset of patients who were not prescribed any cardioactive mediation at baseline or follow-up. Bold values indicate P -value <0.05.
Table 3.
Comparison of BP variability at baseline and follow-up
| Entire follow-up cohort | Participants not taking cardioactive medication | |||||||
|---|---|---|---|---|---|---|---|---|
| Dependent variable | Baseline | Follow-up | Baseline | Follow-up | ||||
| N | Mean ± SD | Mean ± SD | P | N | Mean | Mean | P | |
| 24hr SD SBP | 83 | 12.95±3.29 | 15.07±4.48 | <0.001 | 19 | 12.08±2.11 | 15.22±4.20 | 0.011 |
| 24hr SD DBP | 83 | 9.34±2.36 | 10.70±3.62 | 0.001 | 19 | 9.09±1.48 | 11.46±3.08 | 0.003 |
| 24hr Cv SBP | 83 | 0.10±0.02 | 0.12±0.04 | 0.002 | 19 | 0.10±0.02 | 0.12±0.03 | 0.031 |
| 24hr Cv DBP | 83 | 0.13±0.03 | 0.15±0.05 | 0.008 | 19 | 0.13±0.03 | 0.16±0.05 | 0.012 |
| Day SD SBP | 76 | 11.03±3.22 | 14.02±4.97 | <0.001 | 17 | 10.31±2.67 | 14.46±4.91 | <0.001 |
| Day SD DBP | 76 | 7.68±2.28 | 9.83±4.20 | <0.001 | 17 | 6.88±1.73 | 10.72±4.05 | 0.002 |
| Day Cv SBP | 76 | 0.08±0.03 | 0.11±0.04 | <0.001 | 17 | 0.08±0.02 | 0.10±0.03 | 0.018 |
| Day Cv DBP | 76 | 0.10±0.03 | 0.13±0.05 | <0.001 | 17 | 0.09±0.03 | 0.14±0.05 | 0.004 |
| Night SD SBP | 65 | 8.64±3.79 | 10.65±10.47 | 0.488 | 13 | 8.87±3.77 | 8.29±3.91 | 0.644 |
| Night SD DBP | 65 | 6.79±2.85 | 7.96±6.68 | 0.175 | 13 | 6.43±2.34 | 7.54±3.50 | 0.272 |
| Night Cv SBP | 65 | 0.07±0.03 | 0.09±0.10 | 0.115 | 13 | 0.08±0.03 | 0.07±0.03 | 0.431 |
| Night Cv DBP | 65 | 0.11±0.05 | 0.13±0.11 | 0.182 | 13 | 0.11±0.04 | 0.12±0.06 | 0.501 |
Paired T -tests used to compare BP variability at baseline and follow-up. Analysis shown for participants who had ABPM recordings at baseline and follow-up and a subset of patients who were not prescribed any cardioactive mediation at baseline or follow-up. Bold values indicate P -value <0.05.
Abbreviations: Cv, coefficient of variation; DBP, diastolic blood pressure; SBP, systolic blood pressure.
Changes in comorbidities and use of medication over follow-up
Comorbidities and medication use at baseline and follow-up were compared for the 83 individuals who underwent ABPM at both examinations. There was a significant increase in the number of individuals reporting a past medical history of hypertension at follow-up compared to baseline (60% vs. 37% respectively, P = 0.005). Similarly, the number of individuals diagnosed as diabetic had increased (2% vs. 15%, P = 0.001).
The percentage of patients taking antihypertensive medication increased from 46% at baseline to 69% at follow-up ( P = 0.003). Examining use of individual antihypertensive medication classes showed that there was a significant increase in the number of participants prescribed calcium channel blockers (14% vs. 30% ( P = 0.015)), angiotensin 2 receptor blockers (4% vs. 17% ( P = 0.005)) and diuretics (17% vs. 36% ( P = 0.005)). Use of angiotensin converting enzyme inhibitors (29% vs. 13% ( P = 0.013)) and beta-blockers (24% vs. 17% ( P = 0.183)) had decreased.
To examine if increased use of cardioactive medication may account for the increase in ABPV, a subgroup of 19 patients not taking cardioactive medication at baseline or at follow-up were examined. These patients had no history of cardiovascular disease or diabetes. Twenty-four-hour and daytime systolic and diastolic BP SD were significantly greater at follow-up than at baseline in this subgroup ( Table 3 ). Similarly, the Cv significantly increased between baseline and follow-up ( Table 3 ). Twenty-four-hour, daytime, and nighttime mean systolic BP were also significantly greater at follow-up than at baseline in this subgroup ( Table 2 )
Predictors of ABPM variables
Finally multilevel modeling was used to examine if association between session and BP variability was independent of potential confounders. The initial model included; age at baseline, sex, use of antihypertensive medication, mean BP, and follow-up interval represented by months between ABPM recordings. An interaction term sex × months between recordings was also added to the model to examine if the effect differed for men and women. Results are shown in ( Table 4 ). Follow-up interval had a significant, positive effect on the 24-hour and daytime BP variability, measured by BP SD, independent of participant age, sex, and use of antihypertensive medication. The interaction between sex and follow-up interval was of borderline significance in models of 24-hour and daytime systolic SD ( P = 0.078 and P = 0.055 respectively), suggesting a trend toward greater BP variability in women.
Table 4.
Multilevel modeling examining association between interval between examinations and BP variability
| Model | Dependent variable | Significant fixed effects | B | SE | DF | T | P |
|---|---|---|---|---|---|---|---|
| Model 1 | 24hr SD SBP | 24hr mean SBP | 0.056 | 0.0218 | 166 | 2.575 | 0.012 |
| Years since baseline | 0.590 | 0.0759 | 87 | 7.775 | <0.001 | ||
| Model 2 | 24hr SD DBP | 24hr mean DBP | 0.095 | 0.0323 | 166 | −1.867 | <0.004 |
| Years since baseline | 0.270 | 0.0903 | 166 | 2.984 | <0.004 | ||
| Model 3 | 24hr Cv SBP | Years since baseline | 2.812e − 03 | 6.409e − 04 | 84 | 4.386 | <0.001 |
| Model 4 | 24hr Cv DBP | Years since baseline | 3.082e − 03 | 9.015e − 04 | 84 | 3.419 | <0.001 |
| Age at baseline | 1.770e − 03 | 8.228e − 04 | 82 | 2.151 | 0.03 | ||
| Model 5 | Day SD SBP | Years since baseline | 0.460 | 0.096 | 86 | 4.779 | <0.001 |
| Daytime mean SBP | 0.054 | 0.024 | 155 | 2.248 | 0.026 | ||
| Model 6 | Day SD DBP | Years since baseline | 0.289 | 0.079 | 89 | 3.654 | <0.001 |
| Daytime mean DBP | 0.094 | 0.028 | 139 | 3.296 | 0.001 | ||
| Model 7 | Day Cv SBP | Years since baseline | 3.212e − 03 | 7.700e − 04 | 84 | 4.172 | <0.001 |
| Model 8 | Day Cv DBP | Years since baseline | 3.786e − 03 | 1.026e − 03 | 86 | 3.689 | <0.001 |
Linear mixed effects models examining relationship between years, between assessments, and blood pressure variability. In all models fixed effects entered were; age at baseline, sex, use of antihypertensive medication, years between baseline and follow-up assessment and interaction term sex × years since baseline. As random effects, we had intercepts for subjects. P -values were obtained by maximum likelihood t -tests. This table shows the terms in each model significantly associated with BP variability measure as defined in column 2.
Abbreviations: DBP, diastolic blood pressure; SBP, systolic blood pressure; Cv, coefficient of variation.
The analysis was repeated with Cv as the dependent variable and age at baseline, sex, use of antihypertensive medication, follow-up interval and sex × follow-up interval an interaction term. Follow-up interval was a significant and positive predictor of 24 hour and daytime but not nighttime Cv.
The models were rerun adding body mass index, history of diabetes, alcohol consumption, and smoking history (in pack/years) to the model as predictors. None of these variables were significant predictors of BP variability and did not alter the fit of the model (data not shown).
Analysis was also repeated substituting number of antihypertensive medications for use of antihypertensive medication. This did not significantly alter the model or significant predictors.
Finally, analysis was run with use of individual antihypertensive medication (ace inhibitor, ARB, alpha-blocker, beta antagonist, diuretic, and calcium channel blocker) replacing use of any hypertensive medication. Follow-up interval remained a significant predictor of BP variability measure as either SD or Cv. Individual medication classes did not have a significant effect on BP variability ( Supplementary Table 2 ).
DISCUSSION
In this study, we have shown that 24-hour and daytime ABPV (measured as SD or Cv) increased among community-dwelling older people over a 10-year follow-up interval, whereas mean BP did not significantly change. Over recent decades, great strides have been made in controlling mean BP. It is therefore interesting to find, that even when mean BP is stable, BP variability increases. BP variability has been identified as a risk factor for cardiovascular disease and mortality independent of the mean BP. 9–17 To date, very little attention has been paid to monitoring or controlling ABPV and it remains unknown what degree of BP variability is harmful.
It has been suggested that ABPV may be an additional target for treatment over and above mean BP. 35 Animal model shows that control of BP variability is associated with reduced end-organ disease. 36 In this study use of antihypertensive medication was not associated with BP variability, nor were specific antihypertensive classes associated with BP variability. Previous studies have shown that calcium channel blockers and diuretics have greater effect on BP variability compared to other antihypertensive. 27–29 Failure to reproduce this finding here may reflect type 2 error resulting from the relatively small number of participants taking each class of medication.
Our observation that BP variability increases over a 10-year follow-up is in contrast to the findings of Goldstein et al . who reported that ABPV among older people decreased over a 5-year follow-up. 26 Goldstein et al .’s cohort was highly selected and was unrepresentative of the general older population. Participants with a history of hypertension, obesity, impaired cognitive abnormalities, or psychiatric disorders were excluded from the Goldstein study. In contrast, the population examined here was more typical of the general older population. It must still, however, be acknowledged that there was high attrition in this study. The individuals participating in the follow-up study were, in general, younger, with lower mean BP and lower BP variability than participants lost to follow-up, suggesting follow-up participant may represent a selected cohort at lower cardiovascular risk.
Although our findings are not in keeping with Goldstein et al .’s findings, they are in keeping with cross-sectional studies showing a relationship between age and ABPV. 10 , 18 , 19 Sakakura et al . compared BP variability among a group of 101 younger elderly (aged 61–79) and 101 older elderly (aged ≥80). BP variability was significantly greater among the older group compared to the “young elderly.” 10 Cicconetti et al . found that BP variability is greater among older hypertensive patients compared to younger hypertensive patients and that age and BP variability were significantly correlated in men and women. 19
It is not surprising that BP variability increases with age. Increased ABPV is associated with decreased baroreceptor sensitivity and arterial compliance. 20–23 Both baroreceptor sensitivity and arterial compliance decrease with age. 24 , 25 Interestingly nocturnal BP variability did not significantly change. This may reflect type II error. Only 65 individuals met the criteria for inclusion in the nocturnal analysis (≥5 ABP readings) compared to the 76 who met the criteria for daytime analysis. Alternatively the greater increase in daytime BP variability compared to nighttime variability may reflect BP lability in response to physical and mental exertion during waking hours. At both time points BP variability was greater during the daytime than at nighttime. Conditions associated with exaggerated changes in BP in response to day-to-day activities, e.g., orthostatic hypotension and postprandial hypotension all become more common in later life. 30 , 37 , 38 Age has also been associated with greater BP variability in response to mental stress. 39 It is possible, that these fluctuations in BP in response to normal activities of daily living have greater influence on daytime ABPV than nocturnal ABPV.
Although ABPV increased over 10 years, mean BP did not significantly change over the follow-up period. The stability of mean systolic or diastolic BP over the 10-year follow-up period is interesting. Most studies using casual or ambulatory BP monitoring show an increase in BP with increasing age. The absence of an increase in mean BP in this cohort may reflect changes in the management of hypertension over the last 10 years, including; better detection of hypertension, increasing use of antihypertensive medication, and tighter BP control among older hypertensive patients. At baseline, the most up-to-date UK hypertension guidelines recommended antihypertensive drug therapy for all individuals with sustained BP >160/100 and treatment of individual with BP >140/90 according to target organ damage and 10-year coronary heart disease risk. 40 Low dose thiazide diuretics and beta-blockers were the preferred first-line antihypertensives. Over the intervening 10 years, between the baseline and follow-up assessment, there have been significant changes to the UK guidelines on the management of hypertension. The 2011 National Institute for Health and Care Excellence hypertension guidelines advocated widespread use of ABPM to confirm hypertension in all individuals with office BP >140/90. 2 Calcium channel blockers and thiazide-like diuretics are now recommended as first-line management for people aged above 55. In addition, the guidelines recommend that individuals aged above 80 years are offered the same antihypertensive drug treatment as people aged 55–80. 2 These changes are reflected in the changes to prescribing patterns observed in this study. This move toward more accurate diagnosis of hypertension and tighter control of BP in all age groups may account for failure of this study to reproduce the increase in mean BP observed in other studies. Mean BP did increase among the 19 individuals not taking cardioactive medication, supporting the suggestion, that the lack of a significant increase in mean BP among the wider study population may be due to the increased use of effective antihypertensive medication.
A number of limitations should be acknowledged. This was a post hoc analysis from a large study designed to look at a number of aspects of neurocardiovascular function in older people. Attrition over the 10-year follow-up was high. This resulted in a relatively small follow-up sample that was younger and fitter at baseline compared to the original cohort. The small follow-up population may have resulted in type 2 error particularly when examining the influence of medication class on BP variability where the numbers in each group were small. Conversely the selection bias of younger fitter individuals may have led to an underestimation of changes in ABPV as ABPV would be expected to increase more in participants with greater burden of cardiovascular disease.
One of the challenges of comparing ambulatory BP studies is the variety of methodologies used to collect BP data. In this study, we used fixed periods for daytime and nighttime. This method meant data from morning and late evening periods were not included in the analysis of daytime and nighttime data. It could be argued that such methods risk excluding important contributions to BP variability such as the morning surge. However, using narrow fixed time periods avoids errors due to inaccuracies in patients’ diaries and differences in patients wake sleep patterns associated with age. The use of fixed day/night windows is now recommended. 41
Debate has long existed on the number of recordings required for satisfactory ABPM recordings. Since the inception of this study in 2002, international efforts have been made to standardize ABPM protocols. In 2013, the European Society of Cardiology (ESC) released a position paper suggesting BP readings should be made at 30-minute intervals and that recordings required at least 20 valid daytime readings (0900 to 2100) and 7 valid nighttime readings (0100 to 0600). 41 Although the shorter daytime window used in this study and the decision to record BP hourly overnight meant our protocol did not quite reach current ESC criteria, the majority of participants had 18 or more daytime recordings and 6 or more nocturnal recordings at both assessments. Suggesting that although the studies original criteria only demanded a 50% successful inflation rate the vast majority of patients had well above the 70% successful inflation rate suggested by the recently published ESC guidelines. 41
It should also be noted that if hypertension was diagnosed on baseline ambulatory BP monitoring it was essential for ethical reasons that the participants general practitioner was informed and BP monitored and treated as appropriate. It is therefore possible that changes in mean BP and BP variability are not representative of those seen in an unmonitored population. However, since 2004, general practitioners in the UK have been financially incentivized to identify and effectively manage hypertension in their patients. It is, therefore, likely that the monitoring of BP that participants received as a result of participating in this study is not too different from that offered to the general population.
The underlying mechanisms causing ABPV to increase over time were not examined in this study. Future work will examine the contribution of baroreceptor sensitivity, arterial stiffening and response to physical and mental stress.
These limitations aside, this study is the first to observe that ABPV increased over a 10-year follow-up. This was despite stable mean BP and independent of medication. These findings are important as increased ABPV is associated with adverse cardiovascular outcomes and has recently been suggested as an additional target for treatments aimed at reducing cardiovascular risk. 35 If ABPV is to become a target for treatment, further studies are needed to determine how different antihypertensive classes effect ABPV and what degree of ABPV should be considered harmful.
DISCLOSURE
The authors declared no conflict of interest.
Supplementary Material
SUPPLEMENTARY MATERIAL
Supplementary materials are available at American Journal of Hypertension ( Supplementary Data ).
ACKNOWLEDGMENTS
We thank Jessie Pairman and Katherine Wilton for their help with patient assessment and data collection. This work was supported by the Health Foundation, London, England, Research into Ageing Fund; a fund set up and managed by Age UK, the British Geriatric Society, and the NIHR Newcastle Biomedical Research Centre in Ageing & Chronic Disease.
REFERENCES
- 1. Pickering TG, Shimbo D, Haas D . Ambulatory blood-pressure monitoring . N Engl J Med 2006. ; 354 : 2368 – 2374 . [DOI] [PubMed] [Google Scholar]
- 2. National Institute for Health and Clinical Excellence . Hypertension Clinical Management of Primary Hypertension in Adults. Clinical Guidelines . National Institute of Clinical Excellence; : London, UK: , CG127 2011. < http:/guidance.nice.org.uk/CG127/Guidance/pdf/English >. 2011. . [Google Scholar]
- 3. Staessen JA, Thijs L, Fagard R, O’Brien ET, Clement D, de Leeuw PW, Mancia G, Nachev C, Palatini P, Parati G, Tuomilehto J, Webster J , Investigator SHET. Predicting cardiovascular risk using conventional vs ambulatory blood pressure in older patients with systolic hypertension . JAMA 1999. ; 282 : 539 – 546 . [DOI] [PubMed] [Google Scholar]
- 4. Burr ML, Dolan E, O'Brien EW, O'Brien ET, McCormack P . The value of ambulatory blood pressure in older adults: the Dublin outcome study . Age Ageing 2008. ; 37 : 201 – 206 . [DOI] [PubMed] [Google Scholar]
- 5. Ohkubo T, Imai Y, Tsuji I, Nagai K, Watanabe N, Minami N, Itoh O, Bando T, Sakuma M, Fukao A, Satoh H, Hisamichi S, Abe K . Prediction of mortality by ambulatory blood pressure monitoring versus screening blood pressure measurements: a pilot study in Ohasama . J Hypertens 1997. ; 15 : 357 – 364 . [DOI] [PubMed] [Google Scholar]
- 6. Salles GF, Cardoso CR, Muxfeldt ES . Prognostic influence of office and ambulatory blood pressures in resistant hypertension . Arch Intern Med 2008. ; 168 : 2340 – 2346 . [DOI] [PubMed] [Google Scholar]
- 7. Dawes MG, Coats AJ, Juszczak E . Daytime ambulatory systolic blood pressure is more effective at predicting mortality than clinic blood pressure . Blood Press Monit 2006. ; 11 : 111 – 118 . [DOI] [PubMed] [Google Scholar]
- 8. Hansen TW, Jeppesen J, Rasmussen S, Ibsen H, Torp-Pedersen C . Ambulatory blood pressure monitoring and risk of cardiovascular disease: a population based study . Am J Hypertens 2006. ; 19 : 243 – 250 . [DOI] [PubMed] [Google Scholar]
- 9. Shintani Y, Kikuya M, Hara A, Ohkubo T, Metoki H, Asayama K, Inoue R, Obara T, Aono Y, Hashimoto T . Ambulatory blood pressure, blood pressure variability and the prevalence of carotid artery alteration: the Ohasama study . J Hypertens 2007. ; 25 : 1704 – 1710 . [DOI] [PubMed] [Google Scholar]
- 10. Sakakura K, Ishikawa J, Okuno M, Shimada K, Kario K . Exaggerated ambulatory blood pressure variability is associated with cognitive dysfunction in the very elderly and quality of life in the younger elderly . Am J Hypertens 2007. ; 20 : 720 – 727 . [DOI] [PubMed] [Google Scholar]
- 11. Yamaguchi Y, Wada M, Sato H, Nagasawa H, Koyama S, Takahashi Y, Kawanami T, Kato T . Impact of ambulatory blood pressure variability on cerebral small vessel disease progression and cognitive decline in community-based elderly Japanese . Am J Hypertens 2014. ; 27:1257–1267. [DOI] [PubMed] [Google Scholar]
- 12. Mancia G Parati G Hennig M Flatau B Omboni S Glavina F Costa B Scherz R Bond G Zanchetti A , on behalf of the Ei. Relation between blood pressure variability and carotid artery damage in hypertension: baseline data from the European Lacidipine Study on Atherosclerosis (ELSA) . J Hypertens 2001. ; 19 : 1981 – 1989 . [DOI] [PubMed] [Google Scholar]
- 13. Ozawa M, Tamura K, Okano Y, Matsushita K, Ikeya Y, Masuda S, Wakui H, Dejima T, Shigenaga A-I, Azuma K . Blood pressure variability as well as blood pressure level is important for left ventricular hypertrophy and brachial-ankle pulse wave velocity in hypertensives . Clin Exp Hypertens 2009. ; 31 : 669 – 679 . [DOI] [PubMed] [Google Scholar]
- 14. Eto M, Toba K, Akishita M, Kozaki K, Watanabe T, Kim S, Hashimoto M, Ako J, Iijima K, Sudoh N . Impact of blood pressure variability on cardiovascular events in elderly patients with hypertension . Hypertens Res 2005. ; 28 : 1 – 7 . [DOI] [PubMed] [Google Scholar]
- 15. Kikuya M, Hozawa A, Ohokubo T, Tsuji I, Michimata M, Matsubara M, Ota M, Nagai K, Araki T, Satoh H . Prognostic significance of blood pressure and heart rate variabilities the Ohasama study . Hypertension 2000. ; 36 : 901 – 906 . [DOI] [PubMed] [Google Scholar]
- 16. Poortvliet RK, Ford I, Lloyd SM, Sattar N, Mooijaart SP, de Craen AJ, Westendorp RG, Jukema JW, Packard CJ, Gussekloo J, de Ruijter W, Stott DJ . Blood pressure variability and cardiovascular risk in the PROspective Study of Pravastatin in the Elderly at Risk (PROSPER) . PLoS One 2012. ; 7 : e52438 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Parati G, Valentini M . Blood pressure variability: its measurement and significance in hypertension . Curr Hypertens Rep 2006. ; 8 : 199 – 204 . [DOI] [PubMed] [Google Scholar]
- 18. Jaquet F, Goldstein IB, Shapiro D . Effects of age and gender on ambulatory blood pressure and heart rate . J Hum Hypertens 1998. ; 12 : 253 – 257 . [DOI] [PubMed] [Google Scholar]
- 19. Cicconetti P, Cacciafesta M, Migliori M, Di Gioacchino CF, Vetta F, Chiarotti F, Marigliano V . Influence of sex and age on blood pressure variability . Arch Gerontol Geriatr 2000. ; 30 : 225 – 236 . [DOI] [PubMed] [Google Scholar]
- 20. Siche JP, Herpin D, Asmar RG, Poncelet P, Chamontin B, Comparat V, Gressin V, Boutelant S, Mallion JM . Non-invasive ambulatory blood pressure variability and cardiac baroreflex sensitivity . J Hypertens 1995. ; 13 : 1654 – 1659 . [PubMed] [Google Scholar]
- 21. Mancia G, Parati G, Pomidossi G, Casadei R, Di Rienzo M, Zanchetti A . Arterial baroreflexes and blood pressure and heart rate variabilities in humans . Hypertension 1986. ; 8 : 147 – 153 . [DOI] [PubMed] [Google Scholar]
- 22. Imai Y, Aihara A, Ohkubo T, Nagai K, Tsuji I, Minami N, Satoh H, Hisamichi S . Factors that affect blood pressure variability. A community-based study in Ohasama, Japan . Am J Hypertens 1997. ; 10 : 1281 – 1289 . [DOI] [PubMed] [Google Scholar]
- 23. Ichihara A, Kaneshiro Y, Takemitsu T, Sakoda M, Hayashi M . Ambulatory blood pressure variability and brachial-ankle pulse wave velocity in untreated hypertensive patients . J Hum Hypertens 2006. ; 20 : 529 – 536 . [DOI] [PubMed] [Google Scholar]
- 24. Kardos A, Watterich G, de Menezes R, Csanády M, Casadei B, Rudas L . Determinants of spontaneous baroreflex sensitivity in a healthy working population . Hypertension 2001. ; 37 : 911 – 916 . [DOI] [PubMed] [Google Scholar]
- 25. Monahan KD . Effect of aging on baroreflex function in humans . Am J Physiol Regul Integr Comp Physiol 2007. ; 293 : R3 – R12 . [DOI] [PubMed] [Google Scholar]
- 26. Goldstein IB, Shapiro D, Guthrie D . A 5-year follow-up of ambulatory blood pressure in healthy older adults . Am J Hypertens 2003. ; 16 : 640 – 645 . [DOI] [PubMed] [Google Scholar]
- 27. Zhang Y, Agnoletti D, Safar ME, Blacher J . Effect of antihypertensive agents on blood pressure variability: the Natrilix SR versus candesartan and amlodipine in the reduction of systolic blood pressure in hypertensive patients (X-CELLENT) study . Hypertension 2011. ; 58 : 155 – 160 . [DOI] [PubMed] [Google Scholar]
- 28. Hocht C, Del Mauro JS, Bertera FM, Taira CA . Drugs affecting blood pressure variability: an update . Curr Pharm Des 2015. ; 21 : 744 – 755 . [DOI] [PubMed] [Google Scholar]
- 29. Webb AJ, Rothwell PM . Effect of dose and combination of antihypertensives on interindividual blood pressure variability: a systematic review . Stroke 2011. ; 42 : 2860 – 2865 . [DOI] [PubMed] [Google Scholar]
- 30. Kerr SR, Pearce MS, Brayne C, Davis RJ, Kenny RA . Carotid sinus hypersensitivity in asymptomatic older persons: implications for diagnosis of syncope and falls . Arch Intern Med 2006. ; 166 : 515 – 520 . [DOI] [PubMed] [Google Scholar]
- 31. Staessen JA, Bieniaszewski L, O'Brien E, Gosse P, Hayashi H, Imai Y, Kawasaki T, Otsuka K, Palatini P, Thijs L, Fagard R . Nocturnal blood pressure fall on ambulatory monitoring in a large international database. The "Ad Hoc' Working Group . Hypertension 1997. ; 29 : 30 – 39 . [DOI] [PubMed] [Google Scholar]
- 32. R Core Team . R: A language and environment for statistical computing . R Foundation for Statistical Computing; : Vienna, Austria: , 2012. < http://www.R-project.org/ >. [Google Scholar]
- 33. Bates D, Maechler M, Bolker B, Walker S . Lme4: linear mixed-effects models using Eigen and S4 . R package version 1.0, 2014. < http://cran.r-project.org/web/packages/lme4/ >.
- 34. Kuznetsova A, Brockhoff P, Christensen R . lmerTest: Tests for random and fixed effects for linear mixed effect models (lmer objects of lme4 package) . R package 2.0–11, 2014. < http://cran.r-project.org/web/packages/lmerTest/ >.
- 35. Schillaci G, Pucci G, Parati G . Blood pressure variability: an additional target for antihypertensive treatment? Hypertension 2011. ; 58 : 133 – 135 . [DOI] [PubMed] [Google Scholar]
- 36. Su D-F . Treatment of hypertension based on measurement of blood pressure variability: lessons from animal studies . Curr Opin Cardiol 2006. ; 21 : 486 – 491 . [DOI] [PubMed] [Google Scholar]
- 37. Low PA . Prevalence of orthostatic hypotension . Clin Autonom Res 2008. ; 18 ( Suppl 1 ): 8 – 13 . [DOI] [PubMed] [Google Scholar]
- 38. Luciano GL, Brennan MJ, Rothberg MB . Postprandial hypotension . Am J Med 2010. ; 123 : 281 e281 – 286 . [DOI] [PubMed] [Google Scholar]
- 39. Uchino BN, Berg CA, Smith TW, Pearce G, Skinner M . Age-related differences in ambulatory blood pressure during daily stress: evidence for greater blood pressure reactivity with age . Psychol Aging 2006. ; 21 : 231 – 239 . [DOI] [PubMed] [Google Scholar]
- 40. Ramsay LE, Williams B, Johnston GD, MacGregor GA, Poston L, Potter JF, Poulter NR, Russell G . British Hypertension Society guidelines for hypertension management 1999: summary . BMJ 1999. ; 319 : 630 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. O’Brien E, Parati G, Stergiou G, Asmar R, Beilin L, Bilo G, Clement D, de la Sierra A, de Leeuw P, Dolan E . European Society of Hypertension position paper on ambulatory blood pressure monitoring . J Hypertens 2013. ; 31 : 1731 – 1768 . [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.