Abstract
Objectives
we determined the yearly prevalence of single and multiple falls in persons with or at risk of knee osteoarthritis (OA) and persons undergoing knee arthroplasty over an 8-year period. We also compared annual fall rates among persons with and without knee arthroplasty to determine if fall rates are associated with knee arthroplasty.
Methods
we studied 4,200 persons from the Osteoarthritis Imitative (OAI), a National Institutes of Health funded prospective study of persons 45–79 years and conducted from 2004 to 2012. All either had knee OA or were at risk of developing knee OA but did not have knee arthroplasty. The surgical group comprised 413 persons who underwent knee arthroplasty. Key fall risk factors were assessed at yearly study visits. Graphical depictions illustrated single and multiple fall trajectories. Multinomial regression adjusted for potential confounders compared fall rates for those with and without knee arthroplasty.
Results
fall rate trajectories for the two samples were generally flat and fall rates were similar. For the arthroplasty sample, fall rates did not increase in the immediate perioperative period relative to earlier and later periods. No differences in fall rates were found among the arthroplasty and non-arthroplasty samples after adjustment for potential confounding (P > 0.05).
Conclusions
fall rates were generally stable and similar over an 8-year period among persons with and without knee arthroplasty. Clinicians should not assume that persons undergoing knee arthroplasty are at greater risk for falls either before or after surgery as compared to persons with or at risk for knee OA.
Keywords: older people, knee, osteoarthritis, falls, arthroplasty
Yearly prevalence of falls in community dwelling older persons is approximately 30% per year [1] with resultant injury in approximately a third of falls [2]. Direct and indirect costs of fall related injuries among older adults are formidable with over 23 billion United States (US) dollars in the United States in 2008 and 1.6 billion standardised US dollars in the United Kingdom [3].
Persons with osteoarthritis who have not undergone knee arthroplasty (KA) were found in a cross-sectional study to have a relatively high annual median fall prevalence of 36% of at least one fall per year which is 79% higher as compared to similarly aged persons without arthritis [4]. Females consistently show a higher fall risk and higher risk of injurious falls relative to males [5]. Additionally, persons with multiple falls appear to represent a separate phenotype and are likely to have greater injury risk [6, 7]. Swinkels and colleagues followed 99 KA patients for 1 year following surgery and found that 24 persons (24.2%) fell at least once during this period [8]. Of the 87 falls, 50 (57.5%) resulted in injury and 15 (17.2%) required medical care.
Given the prevalence, costs and consequences of falls among persons with osteoarthritis, a population with a particularly high fall risk, surprisingly little longitudinally-based epidemiologic data are available. For example, whether fall prevalence increases as persons age or progress toward or recover from KA is understudied. Healthcare practitioners would benefit from knowing whether fall prevalence varies over an extended period for persons with or at high risk for developing knee osteoarthritis (OA) or are undergoing KA to target fall prevention interventions during high-risk periods. Additionally, the Centers for Medicare and Medicaid Services (CMS) in the USA requires documentation of medical necessity for KA and this includes a history of falls [9]. Presumably, CMS assumes fall risk reduces following KA but we found no data to support this assertion.
The purposes of this paper are to: (1) determine annual fall prevalence trajectories over an 8-year period among persons with or at high risk for developing knee OA and among persons undergoing KA over a similar timeframe, and (2) compare annual one-time and multiple fall rates among persons in the year prior to and the year following KA to persons without arthroplasty after adjustment for potential confounding. Persons undergoing KA have more severe pain and disability prior to arthroplasty and are challenged to recover in the year following surgery. We therefore hypothesised that annual fall rates would be higher in the 2-year perioperative period for persons undergoing KA as compared to persons without arthroplasty.
Subjects and methods
Data source
The Osteoarthritis Initiative (OAI) is a prospective community-based National Institutes of Health and privately funded natural history multicenter prospective 9-year longitudinal study of persons with radiographic knee OA or at high risk for knee OA. Knee OA risk was determined by the presence of overweight or obesity, prior knee injury or surgery, knee symptoms or family history of knee replacement surgery. The study was approved by the Institutional Review Boards of four sites in the USA: (1) the University of Maryland in Baltimore, Maryland, (2) the Ohio State University in Columbus, Ohio, (3) the University of Pittsburgh in Pittsburgh, Pennsylvania and (4) Memorial Hospital of Rhode Island, in Pawtucket, Rhode Island.
Of 17,457 persons screened, 4,796 were enrolled. Men and women aged 45–79 years were considered. The more common exclusion criteria were magnetic resonance imaging height and weight limitations (n = 2,328), recruitment thresholds for age and gender (n = 2,954) and dropouts prior to the enrollment visit (n = 4,381). The OAI website provides more detailed information (http://www.oai.ucsf.edu/).
Subjects
We divided subjects into two groups, the KA group and the non-arthroplasty group. All subjects (n = 413) who underwent KA over the 9-year study period comprised the arthroplasty group. Persons with hip arthroplasty (n = 183) were excluded.
For the non-arthroplasty group, data from all other subjects in the OAI were used (n = 4,200). Of the 4,200 persons who did not have either hip or KA over the study period, a total of 54.9% had no radiographic evidence of knee OA at baseline and the remaining 45.1% had a validated Kellgren and Lawrence (K&L) [10] grade of at least two at baseline, indicating the presence of radiographic OA in at least one knee. Radiographs were obtained yearly over the first 4 years on all subjects using a highly standardised, reliable and valid approach to position the standing subject's knees in approximately 20-degrees of flexion with equal distribution of the subject's body weight [11]. An extensive adjudication process was used for K&L grades for all knees over all time periods. Two central site readers and a third adjudicator, all either a rheumatologist or a musculoskeletal radiologist with extensive training and very high reliability [12] served as radiographic readers.
Because the KA sample had surgery at different time points over the course of the study (i.e. the surgeries were time varying), we selected the earliest arthroplasty for each subject (some had a later surgery) and then coded the data to allow for a group level graphical presentation of yearly fall rates from 4 years prior to surgery to 4 years after surgery. Subjects contributed varying years of falls data to the study because surgery dates varied. For example, subjects undergoing KA in year 1 were assessed for falls one time preoperatively and then yearly for 4 years postoperatively. We used this strategy to take full advantage of data from all KA procedures in OAI. Supplementary Figure 1, available at Age and Ageingonline illustrates the time points for data collection in both the arthroplasty and the non-arthroplasty samples.
Measurement of falls
Each year from baseline to year 4 and then at year 6 and year 8 visits, all participants were asked the following question via self-report: ‘During the past 12 months, have you fallen and landed on the floor or ground?’ Responses were either yes or no. If yes, the participant was asked: ‘How many times have you fallen in the past 12 months?’ Possible responses were one, two or three, four or five and six or more. For purposes of our study, yearly falls were categorised as either no falls, one fall per year or two or more falls per year. Self-report measures for falls over a 12-month period have strong validity with specificity ranging from 91% to 95% and sensitivity ranging from 80% to 89% when compared to prospective weekly reporting [13].
Predictors of fall risk
We derived key predictors of fall risk from published systematic review evidence on community dwelling middle-aged and older persons [7] and these included age, sex, opioid use during the prior month confirmed by patients bringing all medications to each study visit, repeated chair stand performance [14], physical activity scale for the elderly (PASE) a validated self-reported scale of overall activity level with higher scores indicating greater activity [15], the Center for Epidemiologic Studies Depression (CES-D) score a validated 20-item self-report scale of extent of depressive symptoms with scores from 0 to 60 and higher scores indicating greater symptoms [16], a validated modified Charlson comorbidity scale with higher scores indicating higher comorbidity [17], and walking aid use during indoor walking (yes or no). Prior history of falls, one of the most important predictors of future fall risk [7] was assessed by determining if the person reported falling at least once in the two years prior to the visit of interest.
Data analysis
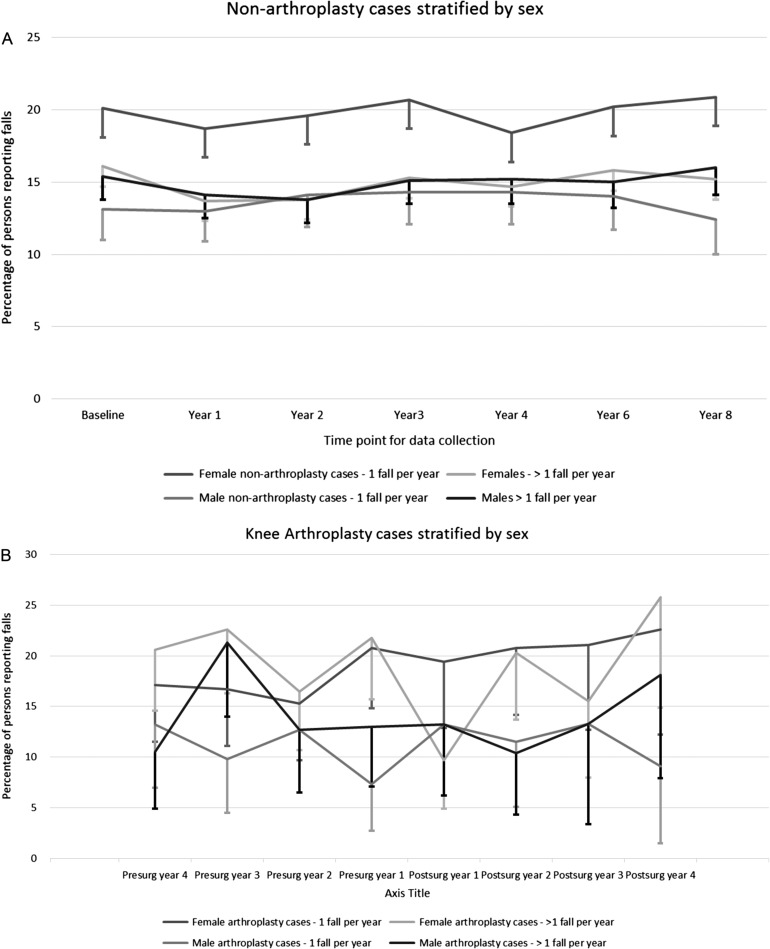
Descriptive data for the surgical and non-surgical samples are reported in Table 1. We used graphical depictions of one-time and multiple (n >= 2) yearly falls prevalence estimates with 95% confidence intervals for both the arthroplasty and non-arthroplasty samples. Because of substantial evidence, we reported fall rates stratified by sex [18, 19].
Table 1.
Baseline characteristics of non-arthroplasty and knee arthroplasty samples
| Non-arthroplasty cases | Knee arthroplasty cases | |
|---|---|---|
| n (%) or mean (sd) (N = 4,200) | n (%) or mean (sd) (N = 413) | |
| Baseline BMI | 28.4 (4.8) | 29.9 (4.7) |
| Missing | 4 | 0 |
| Female sex | 2,446 (58.2) | 251 (60.7) |
| African American race | 799 (19.0) | 52 (12.6) |
| Comorbidity Index | ||
| 0 | 3,137 (75.8) | 291 (70.6) |
| 1 | 622 (15.0) | 74 (18) |
| >1 | 378 (9.2) | 45 (11.4) |
| missing | 63 | 3 |
| Age in years | ||
| <=50 | 635 (15.1) | 22 (5.3) |
| 51–59 | 1,384 (32.9) | 110 (26.7) |
| 60–69 | 1,242 (29.6) | 164 (39.8) |
| 70–79 | 939 (22.4) | 117 (28.2) |
| Yearly falls | ||
| 0 | 2,757 (67.0) | 274 (67.2) |
| 1 | 707 (17.2) | 59 (14.5) |
| >1 | 652 (15.8) | 75 (18.3) |
| Missing | 84 | 5 |
| Opioid use (yes) | 194 (4.6) | 29 (7.0) |
| Missing | 12 | 0 |
| PASE score | 161.03 (82.43) | 160.64 (81.63) |
| Missing | 29 | 0 |
| CES-D score | 6.65 (7.06) | 6.07 (6.07) |
| Missing | 60 | 4 |
| History of falls (yes) | 1,359 (33.0) | 134 (32.8) |
| Missing | 4 | 4 |
BMI, body mass index (calculated as the weight in kilograms divided by height in meters squared); PASE, Physical Activity Scale for the Elderly; CES-D, Center for Epidemiologic Studies Depression Scale.
To compare the yearly prevalence rates of one fall per year and >=2 yearly falls among arthroplasty and non-arthroplasty samples, we used two multinomial multivariable regression models. Predictor variables were age, sex, opioid use, chair stand performance, PASE score, CESD score, comorbidity, history of falls in the prior 2 years and walking aid use. KA status (yes or no) was also entered. All two-way interactions were tested and only significant interactions at P < 0.05 were retained. To minimise repeated statistical testing we compared prevalence estimates from the year 4 visit, the study mid-point, from the non-arthroplasty sample to two data collection sessions of falls data, the 1-year pre-operative and 1-year postoperative time points from the arthroplasty sample. We were interested in determining if KA status predicted fall risk after accounting for potential confounding. The KA status variable was considered significant at P < 0.025, after Bonferroni correction. The Pearson goodness of fit test was used to judge acceptability of the two models.
Results
Characteristics of both the arthroplasty and non-arthroplasty sample are reported in Table 1. Subjects in the arthroplasty samples were older (i.e, 63.9 (sd = 8.6) years) at baseline as compared to the non-arthroplasty sample (i.e. 60.8 (sd = 9.2) years). In addition, a smaller proportion of African Americans were in the arthroplasty sample as compared to the non-arthroplasty sample. Other characteristics were similar. We excluded the walking aid use variable from the analysis because only 1.5% of the sample reported using a walking aid.
Persons in the non-arthroplasty group reported annual single fall rates of approximately 20% for women as compared to 12% for men but annual fall rates of two or more were approximately equal and stable at approximately 15% for both sexes over the 8-year period (see Figure 1A).
Figure 1.
(A) Yearly prevalence of one-time and multiple fall rates over an 8-year period for persons in the non-arthroplasty group. Error bars represent lower bounds of 95% confidence intervals. (B) Yearly prevalence of one-time and multiple fall rates over an 8-year perioperative period for persons in the arthroplasty group. Error bars represent lower bounds of 95% confidence intervals.
Fall trajectories over an 8-year perioperative period among the sample of persons with KA fluctuated somewhat over time with women reporting one-time annual fall rates that ranged from 15% to 23% per year while for men, one-time annual fall rates fluctuated between 8% and 13% per year. Multiple annual falls showed a similar fluctuating trajectory to that for one-time falls with similar rates. Overall, fall rates did not show a consistent pattern of increasing or decreasing rates over the pre-operative or post-operative time period (see Figure 1B).
Non-arthroplasty as compared to arthroplasty annual fall rates
We reasoned that fall risk for persons undergoing KA would be highest in the year prior to surgery and the year following surgery, when pain and functional loss is highest and surgical recovery is the most challenging [20]. Multinomial regression analyses indicated that KA status (yes or no) was not a significant predictor of either a single yearly fall or multiple yearly falls, relative to no falls in either the first preoperative year (Model #1) or the first postoperative year (Model #2). Pearson goodness of fit tests were not significant (P = 0.54 for model #1 and P = 0.46 in model #2) indicating well-fitting models (see Table 2).
Table 2.
Multinomial regression results using year 4 data from the non-arthroplasty sample and the first pre-operative year (Model #1) and first post-operative year (Model #2) for the arthroplasty sample
| Model #1 Year 4 non-KA to 1-year pre-op KAa |
Model #2 Year 4 non-KA to 1-year post-op KAa |
|||
|---|---|---|---|---|
| Beta | Odd Ratio (95% CI) | Beta | Odd Ratio (95% CI) | |
| 1 Fallb | ||||
| Age | 0.002 | 1.00 (0.99, 1.01) | 0.02 | 1.02 (1.01, 1.03)* |
| Male sex | −0.50 | 0.60 (0.49, 0.74)* | −0.19 | 0.83 (0.67, 1.02) |
| PASE scorea | 0 | 1.0 (0.99, 1.00) | 0.001 | 1.00 (1.00, 1.01) |
| Depressive symptoms | 0.001 | 1.00 (0.99, 1.02) | 0.01 | 1.01, (0.99, 1.02) |
| Repeated chair stand | −0.57 | 0.57 (0.28, 1.17) | −0.36 | 0.70, (0.34, 1.42) |
| No comorbidity | −0.20 | 0.82 (0.66, 1.01) | −0.02 | 0.98 (0.78, 1.23) |
| No narcotic use | −0.46 | 0.63 (0.41, 0.97)* | −0.26 | 0.77 (0.50, 1.19) |
| No prior falls | −0.88 | 0.41 (0.34, 0.50)* | −0.90 | 0.41 (0.33, 0.50)* |
| No knee replacement | −0.31 | 0.74 (0.47, 1.15)c | −0.25 | 0.78 (0.55, 1.20)c |
| 2 or more fallsb | ||||
| Age | −0.02 | 0.98 (0.97, 0.99)* | −0.01 | 0.99 (0.98, 1.01) |
| Male sex | −0.07 | 0.93 (0.74, 1.16) | 0.21 | 1.24 (0.99, 1.55) |
| PASE scorea | 0.001 | 1.00 (1.00, 1.00) | 0.002 | 1.00 (1.00, 1.00) |
| Depressive symptoms | 0.05 | 1.05 (1.04, 1.07)* | 0.04 | 1.04 (1.03, 1.05)* |
| Repeated chair stand | −0.28 | 0.76 (0.34, 1.70) | −0.49 | 0.62 (0.29, 1.32) |
| No comorbidity | −0.27 | 0.77 (0.60, 0.97)* | −0.17 | 0.80 (0.66, 1.08) |
| No narcotic use | −0.64 | 0.53 (0.34, 0.82)* | −0.11 | 0.89 (0.55, 1.44) |
| No prior falls | −1.81 | 0.16 (0.13, 0.21)* | −2.00 | 0.14 (0.10, 0.18)* |
| No knee replacement | 0.33 | 1.39 (0.91, 2.14)c | 0.41 | 0.67 (0.36, 1.23)c |
aKA, knee arthroplasty; PASE, Physical Activity Scale for the Elderly.
bIn the multinomial regression, the reference group is no falls and the 2 comparison groups or persons with 1 fall and persons with 2 or more falls.
cWhether a person had a knee replacement was not significantly associated with falls in either model.
*P < 0.05.
Discussion
Our study reports several new findings. First, while OA increases risk of falling [4], annual single and multiple fall rate trajectories among persons with or at risk for knee OA were highly stable over time. Second, persons undergoing KA also had stable trajectories albeit with greater fluctuation relative to the non-surgical sample but we did not find a pattern of increased fall rates as the surgery date neared or decreased fall rates as the patients recovered from surgery. Finally, pre-operative or post-operative fall rates among those with KA are the same as compared to persons with no arthroplasty, even after adjustment for potential confounding.
The lack of a difference in fall rates between persons with and without arthroplasty was a surprising finding. Many have presumed that muscle strength and joint proprioceptive deficits prior to and following surgery and pain and functional worsening prior to arthroplasty [21–23] would lead to increased fall rates relative to that seen in persons who do not undergo arthroplasty. Our data show that this is not the case. Fall rates among persons with KA are not significantly different as compared to persons without KA over the most critical 2-year perioperative period when joint impairments are at their worst and recovery is most challenging [20]. Clinicians should not assume that because of a worsening knee, a patient's fall risk is increased. Furthermore, patients should not be reassured that their fall risk will reduce with KA. Our data suggested a similar but stable postoperative fall risk compared to pre-operative levels. Our study provides reasonably definitive evidence over an extended follow-up period to suggest that fall rates among persons with KA and fall rates among persons with varying amounts of knee OA from none to severe but without a history of arthroplasty do not appreciably differ.
We stratified persons without arthroplasty into those with K&L of 1 or less (i.e. no radiographic knee OA) and those with K&L grades of 2 or higher and found no difference in annual fall rates among the two sub-groups (see Supplementary Figure 2, available at Age and Ageingonline). These data suggest that the severity of knee OA plays essentially no role in determining fall risk for persons not undergoing arthroplasty.
Our study has several strengths including the large sample of persons who did not undergo arthroplasty and the reasonably large sample of KA cases. In addition, the length of the study period provides significantly more longitudinal data relative to previously published studies of arthroplasty patients or persons with knee OA [8]. However, because of the time varying nature of the sample of arthroplasty cases, sample sizes particularly for the later postoperative years 3 (n = 135) and 4 (n = 117) were small. Because subjects were not seen for a yearly visit in OAI in years 5 and 7, falls data were not collected in these years which explained the great majority of missing falls data in the arthroplasty sample. As can be seen in Figure 1B, the 95% confidence intervals are fairly large and particularly so for these later postoperative data points. Despite the small sample sizes, the point estimates for KA fall rates were similar for all yearly comparisons. Additionally, because KA was time varying, some subjects reporting falls in the first postoperative session may have had their falls just prior to surgery which adds potential error to the estimates. A substantial number of subjects were excluded from OAI because of MRI-based height/weight restrictions and this likely reduces generalisability. Missing falls data was minimal, particularly in the non-arthroplasty sample, but likely contributed some bias particularly for the postoperative falls data in the arthroplasty data where 43% of subjects had missing falls data. Finally, data collection at 12-month time intervals likely introduces recall bias for falls and likely underreporting but this approach was shown in a recent systematic review to have substantial validity [13].
In conclusion, our longitudinal natural history study provides new information to inform clinicians of the annual fall prevalence and trajectories over multiple years among persons with KA and persons with or at high risk of developing knee OA. Key findings are that annual fall rates are generally stable over an 8-year perioperative period for persons treated with KA and persons with no arthroplasty. Differences in fall rates between these groups, while traditionally assumed to be present, were not found. Persons with KA show no substantial change in single or multiple fall prevalence over an 8-year perioperative period.
Key points.
Fall trajectories were stable and flat over the 8-year study period.
Fall rates among persons with and without knee arthroplasty were not significantly different.
Fall rates prior to and following knee arthroplasty were stable and did not worsen in the early pre- and post-operative periods.
Conflicts of interest
None declared.
Funding
The Osteoarthritis Initiative (OAI) is a public–private partnership comprised of five contracts (N01-AR-2-2258, N01-AR-2-2259, N01-AR-2-2260, N01-AR-2-2261 and N01-AR-2-2262) funded by the National Institutes of Health, a branch of the Department of Health and Human Services, and conducted by the OAI Study Investigators. Private funding partners include Merck Research Laboratories; Novartis Pharmaceuticals Corporation, GlaxoSmithKline; and Pfizer, Inc. Private sector funding for the OAI is managed by the Foundation for the National Institutes of Health. This manuscript was prepared using an OAI public use data set and does not necessarily reflect the opinions or views of the OAI investigators, the NIH, or the private funding partners. The investigators of the current study are not members of the OAI investigative team.
Supplementary Material
Reference
- 1. O'Loughlin JL, Robitaille Y, Boivin JF, Suissa S.. Incidence of and risk factors for falls and injurious falls among the community-dwelling elderly. Am J Epidemiol 1993; 137: 342–54. [DOI] [PubMed] [Google Scholar]
- 2. Sterling DA, O'Connor JA, Bonadies J.. Geriatric falls: injury severity is high and disproportionate to mechanism. J Trauma 2001; 50: 116–9. [DOI] [PubMed] [Google Scholar]
- 3. Davis JC, Robertson MC, Ashe MC, Liu-Ambrose T, Khan KM, Marra CA.. International comparison of cost of falls in older adults living in the community: a systematic review. Osteoporos Int 2010; 21: 1295–306. [DOI] [PubMed] [Google Scholar]
- 4. Barbour KE, Stevens JA, Helmick CG et al. Falls and fall injuries among adults with arthritis – United States, 2012. MMWR Morb Mortal Wkly Rep 2014; 63: 379–83. [PMC free article] [PubMed] [Google Scholar]
- 5. Talbot LA, Musiol RJ, Witham EK, Metter EJ.. Falls in young, middle-aged and older community dwelling adults: perceived cause, environmental factors and injury. BMC Public Health 2005; 5: 86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Nevitt MC, Cummings SR, Kidd S, Black D.. Risk factors for recurrent nonsyncopal falls. A prospective study. JAMA 1989; 261: 2663–8. [PubMed] [Google Scholar]
- 7. Deandrea S, Lucenteforte E, Bravi F, Foschi R, La VC, Negri E.. Risk factors for falls in community-dwelling older people: a systematic review and meta-analysis. Epidemiology 2010; 21: 658–68. [DOI] [PubMed] [Google Scholar]
- 8. Swinkels A, Newman JH, Allain TJ.. A prospective observational study of falling before and after knee replacement surgery. Age Ageing 2009; 38: 175–81. [DOI] [PubMed] [Google Scholar]
- 9. Center for Medicare and Medicaid Services Documenting Medical Necessity for Major Joint Replacement (Hip and Knee). 8-19-2015. Center for Medicare and Medicaid Services. https://www.cms.gov/outreach-and-education/medicare-learning-network-mln/mlnmattersarticles/downloads/se1236.pdf.
- 10. Kellgren JH, Lawrence JS.. Radiological assessment of osteo-arthrosis. Ann Rheum Dis 1957; 16: 494–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kothari M, Guermazi A, von IG et al. Fixed-flexion radiography of the knee provides reproducible joint space width measurements in osteoarthritis. Eur Radiol 2004; 14: 1568–73. [DOI] [PubMed] [Google Scholar]
- 12. Felson DT. Central Reading of Knee X-rays for K-L Grade and Individual Radiographic Features of Knee OA. 2011.
- 13. Ganz DA, Higashi T, Rubenstein LZ.. Monitoring falls in cohort studies of community-dwelling older people: effect of the recall interval. J Am Geriatr Soc 2005; 53: 2190–4. [DOI] [PubMed] [Google Scholar]
- 14. Gill S, McBurney H.. Reliability of performance-based measures in people awaiting joint replacement surgery of the hip or knee. Physiother Res Int 2008; 13: 141–52. [DOI] [PubMed] [Google Scholar]
- 15. Washburn RA, McAuley E, Katula J, Mihalko SL, Boileau RA.. The physical activity scale for the elderly (PASE): evidence for validity. J Clin Epidemiol 1999; 52: 643–51. [DOI] [PubMed] [Google Scholar]
- 16. Radloff LS. The CES-D scale: a self report depression scale for research in the general population. Appl Psychol Meas 1977; 1: 385–401. [Google Scholar]
- 17. Katz JN, Chang LC, Sangha O, Fossel AH, Bates DW.. Can comorbidity be measured by questionnaire rather than medical record review. Med Care 1996; 34: 73–84. [DOI] [PubMed] [Google Scholar]
- 18. Chang VC, Do MT.. Risk factors for falls among seniors: implications of gender. Am J Epidemiol 2015; 181: 521–31. [DOI] [PubMed] [Google Scholar]
- 19. Dore AL, Golightly YM, Mercer VS et al. Lower-extremity osteoarthritis and the risk of falls in a community-based longitudinal study of adults with and without osteoarthritis. Arthritis Care Res (Hoboken) 2015; 67: 633–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Riddle DL, Perera RA, Stratford PW, Jiranek WA, Dumenci L.. Progressing toward, and recovering from, knee replacement surgery: a five-year cohort study. Arthritis Rheum 2013; 65: 3304–13. [DOI] [PubMed] [Google Scholar]
- 21. Levinger P, Menz HB, Wee E, Feller JA, Bartlett JR, Bergman NR.. Physiological risk factors for falls in people with knee osteoarthritis before and early after knee replacement surgery. Knee Surg Sports Traumatol Arthrosc 2011; 19: 1082–9. [DOI] [PubMed] [Google Scholar]
- 22. Levinger P, Menz HB, Morrow AD et al. Lower limb proprioception deficits persist following knee replacement surgery despite improvements in knee extension strength. Knee Surg Sports Traumatol Arthrosc 2012; 20: 1097–103. [DOI] [PubMed] [Google Scholar]
- 23. Schache MB, McClelland JA, Webster KE.. Lower limb strength following total knee arthroplasty: a systematic review. Knee 2014; 21: 12–20. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.