Abstract
Background
The use of insecticides, through indoor residual spraying and long-lasting insecticide-treated nets (LLINs), is essential to control malaria vectors. However, the sustainability of these tools is challenged by the spread of insecticide resistance in Anopheles mosquitoes. This study was conducted to assess the susceptibility to insecticides and to determine the resistance mechanisms in malaria vectors in Dielmo, a rural area of western Senegal where LLINs were introduced a decade ago.
Methods
CDC bottle bioassays were used to determine the susceptibility of 2–5 day-old unfed Anopheles gambiae s.l. females to alphacypermethrin (12.5 µg/bottle), deltamethrin (12.5 µg/bottle), etofenprox (12.5 µg/bottle), lambdacyhalothrin (12.5 µg/bottle), permethrin (21.5 µg/bottle), DDT (100 µg/bottle), bendiocarb (12.5 µg/bottle), pirimiphos-methyl (20 µg/bottle) and fenitrothion (50 µg/bottle). The involvement of glutathione-S-transferases (GSTs) in insecticide resistance was assessed using a synergist, etacrynic acid (EA, 80 µg/bottle). Polymerase chain reaction (PCR) was used to investigate the presence of ‘knock-down resistance (kdr)’ mutation and to identify sibling species within the An. gambiae complex.
Results
CDC bottle bioassays showed that mosquitoes were fully susceptible to lambdacyhalothrin, bendiocarb and fenitrothion. Overall, mortality rates of 97, 94.6, 93.5, 92.1, and 90.1% were, respectively, observed for permethrin, deltamethrin, pirimiphos-methyl, etofenprox and alphacypermethrin. Resistance to DDT was observed, with a mortality rate of 62%. The use of EA significantly improved the susceptibility of An. gambiae s.l. to DDT by inhibiting GSTs (p = 0.03). PCR revealed that Anopheles arabiensis was the predominant species (91.3%; IC 95 86.6–94%) within An. gambiae complex from Dielmo, followed by Anopheles coluzzii (5.4%; IC 95 2.7–8.1%) and Anopheles gambiae s.s. (3.3%; IC 95 0.6–5.9%). Both 1014F and 1014S alleles were found in An. arabiensis population with frequencies of 0.08 and 0.361, respectively, and 0.233 and 0.133, respectively in An. coluzzii. In An. gambiae s.s. population, only kdr L1014F mutation was detected, with a frequency of 0.167. It was observed that some individual mosquitoes carried both alleles, with 19 specimens recorded for An. arabiensis and 2 for An. coluzzii. The presence of L1014F and L1014S alleles were not associated with resistance to pyrethroids and DDT in An. arabiensis.
Conclusions
The co-occurrence of 1014F and 1014S alleles and the probable involvement of GSTs enzymes in insecticide resistance in An. gambiae s.l. should prompt the local vector programme to implement non-pyrethroid/DDT insecticides alternatives.
Keywords: LLINs, Insecticide resistance, kdr, Metabolic resistance, Anopheles arabiensis, Anopheles coluzzii, Anopheles gambiae s.s., Vector control, Dielmo, Senegal
Background
The constant and significant decrease of malaria incidence reported during recent years has instilled a hope that malaria elimination is a feasible objective in several endemic areas. The current situation is driven by the combination of different malaria control strategies delivered through National Malaria Control Programmes (NMCPs) supported by financial partners [1]. The main tools used are artemisinin-based combination therapy (ACT) to treat Plasmodium infection, indoor residual spraying (IRS) and long-lasting insecticide-treated nets (LLINs) to control malaria vectors. Of these, the use of LLINs remains the most effective strategy to control malaria in endemic areas [2, 3]. During the period 2001–2015, malaria control tools have helped to prevent 633 million cases, and LLINs have been allocated a 69% share of that estimation, in contrast to 21% for ACT and 10% for IRS. In sub-Saharan Africa, 53% of the population at risk slept under LLINs [1]. However, the development of insecticide resistance in Anopheles populations is threatening the effectiveness of LLINs. Some studies have shown that resistant mosquitoes can blood-feed effectively despite the use of LLINs, even when net integrity is not compromised [4–6].
Insecticide resistance has been associated with the use of pesticides for agricultural purposes and for malaria vector control strategies, through IRS and LLINs [7, 8]. Pyrethroid resistance is commonly reported; in 2014, it was recorded in three-quarters of malaria-endemic countries [1]. This situation is alarming as pyrethroids are the only insecticides approved by the World Health Organization (WHO) for LLIN impregnation. Global efforts deployed to control malaria vectors through LLINs could be jeopardized by pyrethroid resistance. Target site resistance and metabolic resistance are the two major mechanisms typically assumed to be responsible for mosquito resistance to insecticides [9]. The voltage-gated sodium channel (VGSC), located in the insect’s nervous system, is the target site for pyrethroids and DDT. Mosquitoes resistant to these insecticides exhibit some modification of their VGSC, due to a mutation of the gene encoding this protein [10]. This target site resistance, better known as ‘knock-down resistance’ (kdr), results from a substitution of a leucine amino acid at codon 1014 by a phenylalanine (L1014F or kdr-west) or by a serine (L1014S or kdr-east). Kdr-west and kdr-east mutations were described for the first time in West [11] and East [12] Africa, respectively. However, recent findings suggest that the circulation of L1014F and L1014S alleles is not geographically limited and both mutations are today found in West and East African countries [13, 14].
Metabolic resistance is due to changes in the mosquito’s enzyme systems which results in rapid detoxification of the insecticide preventing it from reaching the site of action within the mosquito. Several families of enzymes, including cytochrome P450 monooxygenases (P450s), glutathione-S-transferases (GSTs) and carboxylesterases, are involved in mosquito metabolic resistance to insecticides [9, 15–27]. Some chemical compounds, such as piperonyl butoxide (PBO), S-S-S-tributylphosphorotrithioate (DEF) and etacrynic acid (EA), can be used as synergists to inhibit P450s, carboxylesterases and GSTs, respectively [28]. To deal with insecticide resistance, particularly in areas where insecticide-based tools have been implemented for several years, it is relevant to monitor the dynamics and the level of Anopheles susceptibility to insecticide while exploring insecticide resistance mechanisms. Dielmo village, in rural Senegal, has been under LLIN universal coverage since 2008. The use of LLINs in this setting has enabled the control of Anopheles gambiae sensu lato (s.l.) and Anopheles funestus, the main malaria vectors, and to reduce drastically malaria incidence; occasional malaria cases observed were attributed to a lack of LLIN use [29].
Notwithstanding the collapse of malaria incidence in Dielmo through the long-term use of LLINs, there is little information on insecticide resistance in malaria vectors. The main purpose of this work was to investigate insecticide resistance in An. gambiae s.l. to insecticides, a decade since the introduction of LLINs in Dielmo.
Methods
Study area
The study was conducted in Dielmo, which is located in the Fatick region, 280 km from Dakar, in a Soudan-type climate area. Since 1990, a regular epidemiological survey has been conducted in this setting to understand the epidemiology of malaria [30]. In Dielmo, malaria vector control has always been based on LLIN universal coverage. This strategy was implemented in July 2008. Since then, it has been maintained through three LLIN general renewals, in 2011, 2014 and 2016. In Dielmo, IRS has never been introduced. In 2015, there were approximately 481 inhabitants distributed in 42 concessions. The rainy season usually lasts from July to October. In 2015, the first rains were recorded in July. August was the wettest month, followed by September, with respective monthly rainfalls of 262 and 225 mm. In October, rainfall of only 94 mm was recorded. Overall, in 2015, annual rainfall was estimated at 784 mm and the mean temperature ranged from 22 to 35 °C. The villagers are millet and groundnut farmers, but during the dry season, market gardening is practised along the swampy bank of a small permanent river, the Nema, around which market-garden wells or ceanes are dug for watering. In Dielmo, commercial pesticides including organophosphates (Dimethoate®, Pyrical 480EC®), organochlorine and pyrethroids, most often in combination (Callifan Super 40EC®), are used for agricultural purposes.
Anopheles immature stages collection and mosquito rearing
Surveys were carried out in September 2015 in Dielmo. During the study period, five breeding sites were identified in and around the village and were all used to collect Anopheles larvae and pupae. These breeding sites consisted of fresh water with vegetation, especially from the Gramineae family (Fig. 1). Larval collections were pooled in sampling containers and transferred to a local insectary for rearing. Larvae were fed with fishmeal (Tetramin Baby®). Pupae were daily collected and introduced into rearing cages using small plastic cups. At emergence, mosquito adults were fed using absorbent cotton soaked with 10% sucrose solution.
Fig. 1.
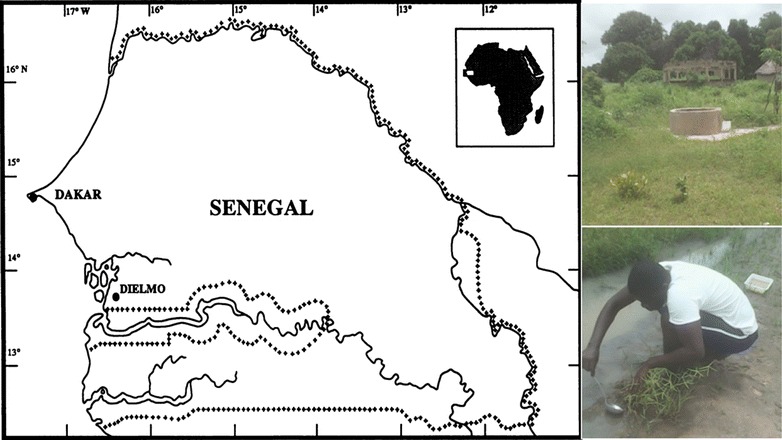
Map showing the location of Dielmo (study area), its aspect in the rainy season and one anopheline breeding site
Anopheles susceptibility to insecticides
The Centers for Disease Control and Prevention (CDC) bottle bioassays was used to assess Anopheles susceptibility to insecticides. Insecticides were provided by CDC in lyophilized forms or in hyper-concentrated formulations. In the laboratory, reconstitution or dilution was performed using acetone to obtain stock solutions of which 1 mL contained the diagnostic dose of the insecticide (expressed in µg/bottle). Stock solutions were then stored at 4 °C in foil-wrapped Falcon tubes before being transported into the field using an electric icebox. Wheaton glass (250 mL) bottles were coated using 1 ml of insecticide solution as described in the CDC protocol [28]. Five pyrethroid insecticides (Alphacypermethrin 12.5 µg/bottle, Deltamethrin 12.5 µg/bottle, Etofenprox 12.5 µg/bottle, Lambdacyhalothrin 12.5 µg/bottle and Permethrin 21.5 µg/bottle), one organochlorine (DDT 100 µg/bottle), one carbamate (Bendiocarb 12.5 µg/bottle) and two organophosphates (Pirimiphos-methyl 20 µg/bottle and Fenitrothion 50 µg/bottle) were tested. Bioassays were carried out on 2–5 day-old unfed females using the CDC bottle protocol [28, 31, 32]. Each insecticide molecule was tested in four replicates using 16–25 female mosquitoes for each replicate; a control bottle with 20–25 female mosquitoes was used in parallel. The temperature in the field testing room was 25 ± 3 °C and the relative humidity was 75 ± 10%. Mortality was recorded at 15-min intervals until insecticide-diagnostic time (DT) was reached. Mortality at DT represents the most critical value in CDC bottle bioassays and thus, in this study any 24-h holding period for mortality recording was not taken into account. The DT was 30 min for all insecticides except DDT which had a DT of 45 min [28]. A mosquito was considered dead if it could not stand or fly in coordinated way, especially when the bottle was gently rotated while making the count. When the DT of the insecticide being tested elapsed, mosquitoes were transferred to holding cartons and survivors were collected using an aspirator and then killed with chloroform. The number of dead mosquitoes for all replicates of each test was used to determine percentage mortality. Finally, both surviving and dead mosquitoes were individually stored in numbered Eppendorf tubes containing silica gel. A random sample of dead mosquitoes and survivors were used for species identification and the detection of kdr gene.
Detection of detoxification enzymes using synergist
In case mosquitoes displayed mortality rate below resistance threshold after exposure to DDT, complementary bioassays with synergist EA (80 µg/bottle) were performed according to CDC protocol [28], using another mosquito sample from the population previously tested. A batch of 100–125 unfed females was exposed to one bottle coated with EA (EA-exposed mosquitoes). Another batch with the same number of mosquitoes was used as a control and was exposed to one acetone-coated bottle (non-EA-exposed mosquitoes). After 1 h of exposure, mosquitoes from each batch were separately released into rearing cages. Then, EA-exposed and non-EA-exposed mosquitoes were in parallel exposed to DDT (100 µg/bottle) according to standard CDC bottle bioassay as above. Data comparisons were made between mortality rates from EA-exposed and non-EA-exposed mosquitoes.
Species identification and detection of kdr-w and kdr-e mutations
CTAB Method was used for extracting genomic deoxyribonucleic acid (DNA) from entire mosquitoes. The one-step polymerase chain reaction (PCR) technique using intentional mismatch primers (IMPs) described by Wilkins et al. [33] was used to identify the sibling species of the An. gambiae complex. L1014F (kdr-w) and L1014S (kdr-e) mutations were investigated using also IMP PCR primers [34]. A volume of 1–2 µL of DNA template was added to 23–25 µL PCR Master Mix containing Taq DNA Polymerase, Microbial DNA-free water, 5X Green GoTaq Buffer, 2.0–2.5 mM dNTP, 25 mM MgCl2 and 2.5–25 pmol/µL of specific primers. PCR amplification conditions in a Bio-Rad® Thermocycler were as follows: 95 °C for 5 min for 1 cycle, followed by [95 °C for 30 s, 58 °C (or 57/59 °C for kdr-e/kdr-w) for 30 s and 72 °C for 30 s] for 30 cycles (or 35 cycles for kdr-e and kdr-w), followed by 1 cycle of 72 °C for 5 min. PCR amplicons were migrated on 2% agarose gel mixed with fluorescent Gel Red DNA stain (BIOTIUM®). Specific target bands were visualized under UV light using a Bio-Rad®Gel Doc XR connected to computer running software (Quantity One, 4.6.6 Basic Version).
Data interpretation and statistical analysis
Percentage mortality was interpreted according to WHO criteria [35] to determine susceptibility status. Pearson’s Chi squared test was used to compare mortality rates. Allelic association studies were conducted using Fisher exact test and odds ratio test. A p value less than 5% was considered as significant. All statistical analyses and graphs were made using R software version 3.4.1 [36].
Results
Susceptibility to insecticides
A total of 834 An. gambiae s.l. female mosquitoes were tested with 9 insecticides. In the group of pyrethroids (Fig. 2), full mortality (100%) was only observed with lambdacyhalothrin (n = 91), after 30 min of exposure. Resistance was suspected with permethrin, deltamethrin, etofenprox, and alphacypermethrin, with mortality rates of 97% (n = 67), 94.6% (n = 110), 92.1% (n = 101), and 92.1% (n = 101), respectively, after 30 min of exposure (Fig. 2). Anopheles gambiae s.l. was resistant to DDT, with a mortality rate of 62% (n = 108), after 45 min of exposure (Fig. 2). Anopheles gambiae s.l. showed full mortality with fenitrothion (n = 74) and a probable resistance to pirimiphos-methyl with a mortality rate of 93.5% (n = 92) after 30 min. Full susceptibility (n = 100) was observed with bendiocarb (carbamate), after 30 min of exposure (Fig. 3). Globally, 205 control mosquitoes were used during the bioassays and no mortality was observed in control bottles.
Fig. 2.
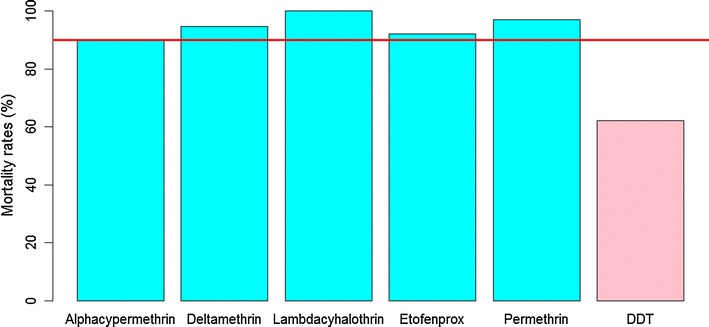
Mortality rates of Anopheles gambiae s.l. from Dielmo, after exposure to pyrethroids (alphacypermethrin 12.5 µg/bottle, deltamethrin 12.5 µg/bottle, etofenprox 12.5 µg/bottle, lambdacyhalothrin 12.5 µg/bottle, permethrin 21.5 µg/bottle) and DDT 100 µg/bottle (organochlorine). Percentage mortality was plotted after exposure at DT of each insecticide. The horizontal line indicates a 90% resistance threshold according to WHO criteria. Pyrethroids are represented by blue bars and organochlorine by pink bars
Fig. 3.
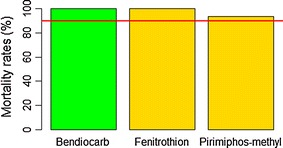
Mortality rates of Anopheles gambiae s.l. from Dielmo, after exposure to one carbamate (bendiocarb 12 µg/bottle) and organophosphorous insecticides (pirimiphos-methyl 20 µg/bottle and fenitrothion 50 µg/bottle). Percentage mortality was plotted after exposure at DT of each insecticide. The horizontal line indicates a 90% resistance threshold according to WHO criteria. Carbamate is represented by green bar and organophosphates by gold bars
Detection of detoxification enzymes with synergist
In the study, only EA (80 µg/bottle) which inhibits GSTs, was used as synergist for DDT-resistant mosquitoes. The prior exposure of mosquitoes to EA before testing with DDT increased significantly (χ2 = 4.6, df = 1, p = 0.03) the mortality rate (87%, n = 113) compared to the control mosquitoes exposed to only DDT (60.97%, n = 97). However, the mortality rate after pre-exposure to EA was still below the resistance threshold (Fig. 4).
Fig. 4.
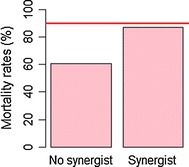
Effect of etacrynic acid (EA 80 µg/bottle) on DDT-resistant Anopheles gambiae s.l. from Dielmo. Mosquitoes from two separate batches were exposed to one acetone-coated bottle (no synergist) and to another EA-coated one (synergist) for 1 h, before being both tested with DDT-treated bottles for 45 min (DDT DT). Percentage mortality was plotted after exposure at DT of each insecticide. The horizontal line indicates a 90% resistance threshold according to WHO criteria
Species identification and detection of kdr-w and kdr-e mutations
A total of 280 An. gambiae s.l. females were analysed using IMPs-SNP PCR for species identification and detection of kdr-e and kdr-w alleles (Table 1). Results showed that 91.43% (IC 95 87.51–94.43%) of specimens were Anopheles arabiensis; 5.36% (IC 95 3.03–8.68%) were Anopheles coluzzii and 3.21% (IC 95 1.48–6.01%) were Anopheles gambiae sensu stricto (s.s.). No hybrid between An. gambiae s.s. and An. coluzzii was found.
Table 1.
Allelic frequencies of 1014L, 1014F and 1014S in three sibling species of Anopheles gambiae complex in Dielmo
| Species | Genotypes | Total (N) | Alleles | 2N | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| LL | LF | LS | FS | FF | SS | 1014L | 1014F | 1014S | |||
| An. arabiensis | 128 (0.5000) | 2 (0.0077) | 28 (0.1081) | 19 (0.0742) | 10 (0.0391) | 69 (0.2664) | 256 (1.0000) | 286 (0.5586) | 41 (0.0801) | 185 (0.3613) | 512 (1.0000) |
| An. coluzzii | 9 (0.6000) | 1 (0.0667) | 0 (0.0000) | 2 (0.1333) | 2 (0.1333) | 1 (0.0667) | 15 (1.0000) | 19 (0.6333) | 7 (0.2333) | 4 (0.1333) | 30 (1.0000) |
| An. gambiae s.s. | 7 (0.7778) | 1 (0.1111) | 0 (0.0000) | 0 (0.0000) | 1 (0.1111) | 0 (0.0000) | 9 (1.0000) | 15 (0.8333) | 3 (0.1667) | 0 (0.0000) | 18 (1.0000) |
Figures in parenthesis indicate genotype or allelic frequencies
N number of samples characterized, L leucine, F phenylalanine, S serine
The results of genotyping and kdr alleles are shown in Table 1. In An. gambiae s.s. population, only L1014F mutation was found, at a frequency of 0.1667. Both L1014F and L1014S alleles were found in An. arabiensis and An. coluzzii populations. The frequency of L1014F allele was 0.233 and 0.080 in An. coluzzii and An. arabiensis, respectively. However, the frequency of L1014S allele was higher in An. arabiensis (0.361) compared to An. coluzzii (0.133). Furthermore, individual mosquitoes were observed carrying both kdr-w and kdr-e mutations (F/S), with 7.42% (IC 95 4.47–11.22%) and 13.33% (IC 95 1.66–4.05%) in An. arabiensis and An. coluzzii populations, respectively (Table 1).
Among the 280 individuals genotyped, 70 were alive after exposure to insecticides. Of these 70 individuals, 5 were exposed to pirimiphos-methyl and the 65 to pyrethroids and DDT. The genotyping result of 65 individuals exposed was as follows: 95.4% (IC 95 87.10–99.04%) were An. arabiensis and 4.6% (IC 95 0.96–12.90%) were An. coluzzii. Of the three An. coluzzii alive only one was homozygous for L1014F-kdr while the two remaining individuals were L1014F and L1014S free. Out of 62 An. arabiensis individuals alive, 6.4% (IC 95 1.78–15.70%) were homozygous for L1014F-kdr (FF), but there were 22.5% (IC 95 12.03–34.98%) homozygous (SS) and 19.3% (IC 95 10.42–31.37%) heterozygous (LS) individuals for L1014S-kdr. Finally, 4.8% (IC 95 1.01–13.50%) of An. arabiensis individuals alive were homozygous for both 1014F and 1014S alleles (FS), and 46.8% (IC 95 34.00–59.88%) were fully homozygous susceptible, e.g. L1014F and L1014S free (LL) (Fig. 5). Among An. arabiensis individuals alive after exposure to pyrethroids and DDT, some mosquitoes carried both L1014F and L1014S alleles in homozygous (FF, SS) and/or heterozygous (FS, LS) conditions, while others were kdr-free individuals. For permethrin, all surviving An. arabiensis individuals were homozygous susceptible (LL) (Fig. 5). To get a clear idea of the involvement of kdr mutation in An. arabiensis susceptibility, an allelic association analysis was performed on 201 individuals, including alive and dead mosquitoes exposed to pyrethroids and DDT (Table 2). No significant correlation was observed, neither between 1014F allele and the resistance to pyrethroids [(OR = 1.17 (0.36–3.88); p = 0.78] and DDT [(OR = 1.09 (0.38-3.17); p = 0.95], nor between 1014S allele and the resistance to pyrethroids [(OR = 1.38 (0.58–3.30); p = 0.46] and DDT [(OR = 1.09 (0.38–3.17); p = 0.87] (Table 2).
Fig. 5.
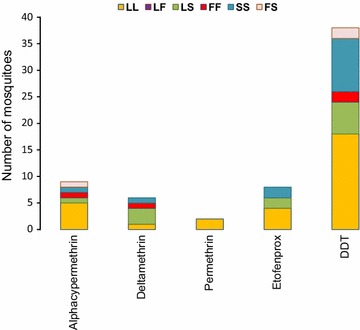
Distribution of susceptible and resistant alleles in Anopheles arabiensis individuals alive after exposure to pyrethroids and DDT. LL homozygous susceptible, LF heterozygous resistant for kdr-w, LS heterozygous resistant for kdr-e, FF homozygous resistant for kdr-w, SS homozygous resistant for kdr-e, FS heterozygous resistant for both kdr-w and kdr-e
Table 2.
Association of kdr alleles with pyrethroid and DDT resistance phenotype in Anopheles arabiensis in Dielmo
| Insecticides (N) | State | Genotype counts | Allelic association (additive model) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| LL | LF | FF | LS | SS | FS | Fisher exact test (p) | Odds ratio (95% CI) | ||||
| L vs F | L vs S | L vs F | L vs S | ||||||||
| Pyrethroids (140) | Alive | 11 | 0 | 2 | 6 | 4 | 2 | (0.787) | (0.463) | 1.17 (0.36–3.88) | 1.38 (0.58–3.30) |
| Dead | 64 | 2 | 3 | 8 | 27 | 11 | |||||
| DDT (61) | Alive | 20 | 0 | 2 | 6 | 10 | 2 | (0.953) | (0.873) | 1.06 (0.18–6.30) | 1.09 (0.38–3.17) |
| Dead | 10 | 1 | 1 | 3 | 6 | 0 | |||||
LL homozygous susceptible, LF heterozygous resistant for kdr-w, LS heterozygous resistant for kdr-e, FF homozygous resistant for kdr-w, SS homozygous resistant for kdr-e, FS heterozygous resistant for both kdr-w and kdr-e, L leucine, F phenylalanine, S serine
Discussion
In this study, the main issue was to determine insecticide resistance profile, as a backdrop to assessing LLIN vulnerability after a decade of use in Dielmo. In this study, the CDC bottle bioassays have been opted to establish a surveillance tool for detecting resistance to insecticides, but also for providing basic data for vector control routines in Dielmo. The choice for this tool was justified by its adaptability in the field [32], the good correlation of results with those collected from WHO standard assays [37] and its acknowledgement by WHO [35].
From the bioassays, it was observed that An. gambiae s.l. was susceptible to lambdacyhalothrin whereas suspected resistance to other pyrethroids including permethrin, deltamethrin, etofenprox, and alphacypermethrin was observed. In Dielmo, LLIN universal coverage started in 2008 and was maintained with three general renewals, in 2011, 2014 and 2016. This long pyrethroid-based vector control could explain the reduced susceptibility to permethrin, deltamethrin, etofenprox, and alphacypermethrin. However, this situation does not appear to affect the downward trend in malaria incidence in Dielmo [29, 38]. In many sites of high or moderate pyrethroid resistance, the effectiveness of LLINs in malaria control has been maintained [29, 38–43] even if this pattern differs from other studies that have shown the failure of LLINs to control pyrethroid-resistant mosquitoes [4, 6, 44]. Also, in Dielmo, An. gambiae s.l. was resistant to DDT. Anopheles resistance to DDT has often been linked to its historical use for vector-borne diseases and crop pest control. Despite having been abandoned, DDT could persist in the environment due to its decades of widespread use in public health and agriculture. Indeed, DDT was found in high concentrations in many western African plant species, such Mangifera indica [45–47], which is also abundant in Dielmo. On the other hand, the Dielmo villagers are engaged in traditional farming and market gardening which could involve use of commercial pesticides comprising organophosphates, organochlorine and pyrethroids. Therefore, selection pressure from agricultural activities, even with low amounts of insecticides, could trigger the development of mosquito resistance to DDT, pirimiphos-methyl and some pyrethroids in Dielmo, as it was observed in many African countries [8, 48–50]. The susceptibility of An. gambiae s.l. to bendiocarb and fenitrothion is probably linked to the fact that these molecules are not used for vector control in Dielmo. In this area, the use of LLINs has been the main strategy for controlling malaria vectors for several years, and no IRS programme has been set up for public health purposes. Therefore, the low or almost non-existent selection pressure could explain the full susceptibility of mosquito populations to carbamates, some organophosphates and some pyrethroids.
PCR-based identification of species revealed that An. arabiensis was the predominant species within An. gambiae complex. The other sibling species, An. coluzzii and An. gambiae s.s. were found at low levels. This finding is in line with the Dielmo species composition described nearly 20 years ago [51] and recently confirmed despite the implementation of LLINs in this study area [52]. In this study, both 1014F and 1014S alleles were found in An. arabiensis and An. coluzzii populations while in An. gambiae s.s. only1014F was found. This confirms the recent findings on the co-occurrence of these alleles in An. arabiensis in Senegal [14] and reinforces the perception that the distribution of kdr alleles should no longer be considered as being confined to some specific geographical areas [13, 53]. This is the first report of 1014S (kdr-e) allele in An. coluzzii from Senegal. However, 1014F and 1014S alleles are carried essentially by An. arabiensis, which is the principal vector in the study area. In An. arabiensis, the frequency of 1014S allele (36%) is in same range as those described in this species from Dakar urban area [14]. The high level of 1014S allele frequency being recorded in Dielmo could mean that the circulation of this allele has been overlooked or underestimated as it was considered until recently that this mutation is absent in western African region. The lack of historical data does not allow estimating when this allele has emerged in Dielmo. However, one cannot rule out that the widespread implementation of LLINs since 2008 has fostered the emergence of kdr-e mutation. Indeed, it is known that Anopheles insecticide resistance can increase considerably over a relatively short period [54].
Furthermore, the frequency of L1014F (kdr-w) allele in An. arabiensis (8%) was relatively low compared to many West African countries [55–59]. All the same, a similar trend was found in An. arabiensis population from an area close to Dielmo [60]. Particular attention should be paid to the dynamics of these two alleles as they have not yet approached fixation in the Anopheles population and some individuals are carrying both alleles. However, although present in Anopheles populations, kdr mutation was not strongly associated with phenotype resistance, neither to pyrethroids nor to DDT. Indeed, half of the dead individuals exposed to pyrethroids and DDT were positively genotyped for kdr mutation. This indicates that the occurrence of kdr mutation is not fully predictive of the resistance to pyrethroids and DDT in An. gambiae s.l. from Dielmo. It is thus likely that other mechanisms, in addition to kdr mutation, are involved in mosquito resistance to pyrethroids and DDT. This hypothesis was confirmed by use of the synergist EA, implicating GSTs in DDT resistance. Indeed, GST-based resistance is considered the major mechanism of DDT resistance in anopheline species [9, 15, 61, 62] and has been reported in African An. arabiensis populations [15, 62]. However, the EA did not fully restore the susceptibility of mosquitoes to DDT; it is therefore likely that additional mechanisms, other than target site (kdr) and GSTs, are involved in DDT resistance. It would be relevant to measure esterases and P450s activities, as well as cuticular resistance, to clarify this point.
Conclusion
In Dielmo, despite a long period of LLIN coverage, the level of pyrethroid resistance in An. gambiae s.l. population was still low compared to some malaria-endemic regions in West Africa. Furthermore, to manage insecticide resistance in Dielmo, it is recommended to implement a second line of vector control based on non-pyrethroid/DDT insecticides. However, molecular and biochemical monitoring is needed to better elucidate the different mechanisms involved in insecticide resistance in Anopheles populations in Dielmo.
Authors’ contributions
SD, SS, OT, and CS designed the study. SD, LK, ND, OF, and CS supervised the study. OT carried out the field collections with assistance of CB, and performed the experiments. OT and SD analysed the data and wrote the manuscript. All authors read and approved the final manuscript.
Acknowledgements
We thank Dr. Ellen Dotson and Dr. William G. Brogdon (CDC) for helpful advice on CDC bottle bioassays and the supply of reagents and insecticides. We thank Dr. Badara Samb (LEVP-UCAD) and Hubert Bassene (URMITE-IRD) for additional PCR reagents. We thank Dr. Ibrahima Dia (Institut Pasteur Dakar) for helpful scientific advice and Essoham Ali (URMITE-IRD) for help in data analysis. We are grateful to Dielmo villagers for their cooperation.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The study was approved by the Ministry of Health of Senegal and the assembly of the Dielmo population.
Funding
This work was supported by the Unité de Recherche sur les Maladies Infectieuses et Tropicales Emergentes (URMITE), UMR 198, Campus UCAD/IRD de Hann, BP 1386. The funding body had no role in the design of the study and collection, analysis and interpretation of data and in writing the manuscript.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Abbreviations
- ACT
artemisinin-based combination therapy
- CDC
Centers for Disease Control and Prevention
- CTAB
cetyltrimethyl ammonium bromide
- P450s
cytochrome P450 monooxygenases
- DDT
dichlorodiphenyltrichloroethane
- DEF
S-S-S-tributylphosphorotrithioate
- DNA
deoxyribonucleic acid
- DT
diagnostic time
- EA
etacrynic acid
- GSTs
glutathione-S-transferases
- IMPs
intentional mismatch primers
- IRS
indoor residual spraying
- kdr
knockdown resistance
- LLINs
long-lasting insecticide-treated nets
- NMCP
National Malaria Control Programme
- PBO
piperonyl butoxide
- PCR
polymerase chain reaction
- SNP
single nucleotide polymorphism
- VGSC
voltage-gated sodium channel
- WHO
World Health Organization
References
- 1.WHO . World malaria report 2016. Geneva: World Health Organization; 2016. [Google Scholar]
- 2.Lengeler C. Insecticide-treated bed nets and curtains for preventing malaria. Cochrane Database Syst Rev. 2004;(2):CD000363. [DOI] [PubMed]
- 3.Diop F, Richard V, Diouf B, Sokhna C, Diagne N, Trape JF, et al. Dramatic declines in seropositivity as determined with crude extracts of Plasmodium falciparum schizonts between 2000 and 2010 in Dielmo and Ndiop, Senegal. Malar J. 2014;13:83. doi: 10.1186/1475-2875-13-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Asidi A, N’Guessan R, Akogbeto M, Curtis C, Rowland M. Loss of household protection from use of insecticide-treated nets against pyrethroid-resistant mosquitoes, Benin. Emerg Infect Dis. 2012;18:1101–1106. doi: 10.3201/eid1807.120218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mathanga DP, Mwandama DA, Bauleni A, Chisaka J, Shah MP, Landman KZ, et al. The effectiveness of long-lasting, insecticide-treated nets in a setting of pyrethroid resistance: a case–control study among febrile children 6 to 59 months of age in Machinga District, Malawi. Malar J. 2015;14:457. doi: 10.1186/s12936-015-0961-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.N’Guessan R, Corbel V, Akogbeto M, Rowland M. Reduced efficacy of insecticide-treated nets and indoor residual spraying for malaria control in pyrethroid resistance area, Benin. Emerg Infect Dis. 2007;13:199–206. doi: 10.3201/eid1302.060631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hemingway J, Jayawardena KG, Herath PR. Pesticide resistance mechanisms produced by field selection pressures on Anopheles nigerrimus and A. culicifacies in Sri Lanka. Bull World Health Organ. 1986;64:753–758. [PMC free article] [PubMed] [Google Scholar]
- 8.Reid MC, McKenzie FE. The contribution of agricultural insecticide use to increasing insecticide resistance in African malaria vectors. Malar J. 2016;15:107. doi: 10.1186/s12936-016-1162-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hemingway J, Hawkes NJ, McCarroll L, Ranson H. The molecular basis of insecticide resistance in mosquitoes. Insect Biochem Mol Biol. 2004;34:653–665. doi: 10.1016/j.ibmb.2004.03.018. [DOI] [PubMed] [Google Scholar]
- 10.Davies TGE, Field LM, Usherwood PNR, Williamson MS. DDT, pyrethrins, pyrethroids and sodium channels. IUBMB Life. 2007;59:151–162. doi: 10.1080/15216540701352042. [DOI] [PubMed] [Google Scholar]
- 11.Martinez-Torres D, Chandre F, Williamson MS, Darriet F, Berge JB, Devonshire AL, et al. Molecular characterization of pyrethroid knockdown resistance (kdr) in the major malaria vector Anopheles gambiae s.s. Insect Mol Biol. 1998;7:179–184. doi: 10.1046/j.1365-2583.1998.72062.x. [DOI] [PubMed] [Google Scholar]
- 12.Ranson H, Jensen B, Vulule JM, Wang X, Hemingway J, Collins FH. Identification of a point mutation in the voltage-gated sodium channel gene of Kenyan Anopheles gambiae associated with resistance to DDT and pyrethroids. Insect Mol Biol. 2000;9:491–497. doi: 10.1046/j.1365-2583.2000.00209.x. [DOI] [PubMed] [Google Scholar]
- 13.Kabula B, Kisinza W, Tungu P, Ndege C, Batengana B, Kollo D, et al. Co-occurrence and distribution of East (L1014S) and West (L1014F) African knock-down resistance in Anopheles gambiae sensu lato population of Tanzania. Trop Med Int Health. 2014;19:331–341. doi: 10.1111/tmi.12248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ndiath MO, Cailleau A, Orlandi-Pradines E, Bessell P, Pages F, Trape JF, et al. Emerging knock-down resistance in Anopheles arabiensis populations of Dakar, Senegal: first evidence of a high prevalence of kdr-e mutation in West African urban area. Malar J. 2015;14:364. doi: 10.1186/s12936-015-0898-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hemingway J, Malcom CA, Kissoon KE, Boddington RG, Curtis CF, Hill N. The biochemistry of insecticide resistance in Anopheles sacharovi; comparative study with a range of insecticide susceptible and resistant Anopheles and Culex species. Pest Biochem Physiol. 1985;24:68–76. doi: 10.1016/0048-3575(85)90115-4. [DOI] [Google Scholar]
- 16.Hemingway J, Ranson H. Insecticide resistance in insect vectors of human disease. Annu Rev Entomol. 2000;45:371–391. doi: 10.1146/annurev.ento.45.1.371. [DOI] [PubMed] [Google Scholar]
- 17.Choi KS, Christian R, Nardini L, Wood OR, Agubuzo E, Muleba M, et al. Insecticide resistance and role in malaria transmission of Anopheles funestus populations from Zambia and Zimbabwe. Parasit Vectors. 2014;7:464. doi: 10.1186/s13071-014-0464-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chouaibou M, Zivanovic GB, Knox TB, Jamet HP, Bonfoh B. Synergist bioassays: a simple method for initial metabolic resistance investigation of field Anopheles gambiae s.l. populations. Acta Trop. 2014;130:108–111. doi: 10.1016/j.actatropica.2013.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Djouaka R, Irving H, Tukur Z, Wondji CS. Exploring mechanisms of multiple insecticide resistance in a population of the malaria vector Anopheles funestus in Benin. PLoS ONE. 2011;6:e27760. doi: 10.1371/journal.pone.0027760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Edi CV, Djogbenou L, Jenkins AM, Regna K, Muskavitch MA, Poupardin R, et al. CYP6 P450 enzymes and ACE-1 duplication produce extreme and multiple insecticide resistance in the malaria mosquito Anopheles gambiae. PLoS Genet. 2014;10:e1004236. doi: 10.1371/journal.pgen.1004236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jones CM, Haji KA, Khatib BO, Bagi J, Mcha J, Devine GJ, et al. The dynamics of pyrethroid resistance in Anopheles arabiensis from Zanzibar and an assessment of the underlying genetic basis. Parasit Vectors. 2013;6:343. doi: 10.1186/1756-3305-6-343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kloke RG, Nhamahanga E, Hunt RH, Coetzee M. Vectorial status and insecticide resistance of Anopheles funestus from a sugar estate in southern Mozambique. Parasit Vectors. 2011;4:16. doi: 10.1186/1756-3305-4-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Koffi AA, Ahoua Alou LP, Adja MA, Chandre F, Pennetier C. Insecticide resistance status of Anopheles gambiae s.s. population from M’Be: a WHOPES-labelled experimental hut station, 10 years after the political crisis in Côte d’Ivoire. Malar J. 2013;12:151. doi: 10.1186/1475-2875-12-151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mawejje HD, Wilding CS, Rippon EJ, Hughes A, Weetman D, Donnelly MJ. Insecticide resistance monitoring of field-collected Anopheles gambiae s.l. populations from Jinja, eastern Uganda, identifies high levels of pyrethroid resistance. Med Vet Entomol. 2013;27:276–283. doi: 10.1111/j.1365-2915.2012.01055.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mulamba C, Riveron JM, Ibrahim SS, Irving H, Barnes KG, Mukwaya LG, et al. Widespread pyrethroid and DDT resistance in the major malaria vector Anopheles funestus in East Africa is driven by metabolic resistance mechanisms. PLoS ONE. 2014;9:e110058. doi: 10.1371/journal.pone.0110058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nwane P, Etang J, Chouasmall yi UM, Toto JC, Koffi A, Mimpfoundi R, et al. Multiple insecticide resistance mechanisms in Anopheles gambiae s.l. populations from Cameroon, Central Africa. Parasit Vectors. 2013;6:41. doi: 10.1186/1756-3305-6-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Witzig C, Parry M, Morgan JC, Irving H, Steven A, Cuamba N, et al. Genetic mapping identifies a major locus spanning P450 clusters associated with pyrethroid resistance in kdr-free Anopheles arabiensis from Chad. Heredity (Edinb) 2013;110:389–397. doi: 10.1038/hdy.2012.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Brogdon WG, Chan A. Guideline for evaluating insecticide resistance in vectors using CDC bottle bioassay. Atlanta: CDC Stacks_Public Health Publications; 2012. p. 28. [Google Scholar]
- 29.Wotodjo AN, Richard V, Boyer S, Doucoure S, Diagne N, Toure-Balde A, et al. The implication of long-lasting insecticide-treated net use in the resurgence of malaria morbidity in a Senegal malaria endemic village in 2010–2011. Parasit Vectors. 2015;8:267. doi: 10.1186/s13071-015-0871-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Trape JF, Rogier C, Konate L, Diagne N, Bouganali H, Canque B, et al. The Dielmo project: a longitudinal study of natural malaria infection and the mechanisms of protective immunity in a community living in a holoendemic area of Senegal. Am J Trop Med Hyg. 1994;51:123–137. doi: 10.4269/ajtmh.1994.51.123. [DOI] [PubMed] [Google Scholar]
- 31.Brogdon WG, McAllister JC. Simplification of adult mosquito bioassays through use of time-mortality determinations in glass bottles. J Am Mosq Control Assoc. 1998;14:159–164. [PubMed] [Google Scholar]
- 32.Zamora Perea E, Balta Leon R, Palomino Salcedo M, Brogdon WG, Devine GJ. Adaptation and evaluation of the bottle assay for monitoring insecticide resistance in disease vector mosquitoes in the Peruvian Amazon. Malar J. 2009;8:208. doi: 10.1186/1475-2875-8-208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wilkins EE, Howell PI, Benedict MQ. IMP PCR primers detect single nucleotide polymorphisms for Anopheles gambiae species identification, Mopti and Savanna rDNA types, and resistance to dieldrin in Anopheles arabiensis. Malar J. 2006;5:125. doi: 10.1186/1475-2875-5-125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Huynh LY, Sandve SR, Hannan LM, Van Ert M, Gimnig JE. Fitness costs of pyrethroid insecticide resistance in Anopheles gambiae. In: Annual meeting of the society for the study of evolution, Christchurch, New Zealand. 2007.
- 35.WHO . Test procedures for insecticide resistance monitoring in malaria vector mosquitoes. Geneva: World Health Organization; 2013. [Google Scholar]
- 36.R Core Team. R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. 2017. https://www.R-project.org/. Accessed 12 Sept 2017.
- 37.Aizoun N, Osse R, Azondekon R, Alia R, Oussou O, Gnanguenon V, et al. Comparison of the standard WHO susceptibility tests and the CDC bottle bioassay for the determination of insecticide susceptibility in malaria vectors and their correlation with biochemical and molecular biology assays in Benin, West Africa. Parasit Vectors. 2013;6:147. doi: 10.1186/1756-3305-6-147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wotodjo AN, Diagne N, Gaudart J, Richard V, Raoult D, Sokhna C. Malaria risk factors in Dielmo, a Senegalese malaria-endemic village, between October and November of 2013: a case–control study. Am J Trop Med Hyg. 2015;92:565–568. doi: 10.4269/ajtmh.14-0485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kawada H, Ohashi K, Dida GO, Sonye G, Njenga SM, Mwandawiro C, et al. Preventive effect of permethrin-impregnated long-lasting insecticidal nets on the blood feeding of three major pyrethroid-resistant malaria vectors in western Kenya. Parasit Vectors. 2014;7:383. doi: 10.1186/1756-3305-7-383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lindblade KA, Mwandama D, Mzilahowa T, Steinhardt L, Gimnig J, Shah M, et al. A cohort study of the effectiveness of insecticide-treated bed nets to prevent malaria in an area of moderate pyrethroid resistance, Malawi. Malar J. 2015;14:31. doi: 10.1186/s12936-015-0554-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sovi A, Azondekon R, Aikpon RY, Govoetchan R, Tokponnon F, Agossa F, et al. Impact of operational effectiveness of long-lasting insecticidal nets (LLINs) on malaria transmission in pyrethroid-resistant areas. Parasit Vectors. 2013;6:319. doi: 10.1186/1756-3305-6-319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Strode C, Donegan S, Garner P, Enayati AA, Hemingway J. The impact of pyrethroid resistance on the efficacy of insecticide-treated bed nets against African anopheline mosquitoes: systematic review and meta-analysis. PLoS Med. 2014;11:e1001619. doi: 10.1371/journal.pmed.1001619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tokponnon FT, Ogouyemi AH, Sissinto Y, Sovi A, Gnanguenon V, Cornelie S, et al. Impact of long-lasting, insecticidal nets on anaemia and prevalence of Plasmodium falciparum among children under five years in areas with highly resistant malaria vectors. Malar J. 2014;13:76. doi: 10.1186/1475-2875-13-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Haji KA, Khatib BO, Smith S, Ali AS, Devine GJ, Coetzee M, et al. Challenges for malaria elimination in Zanzibar: pyrethroid resistance in malaria vectors and poor performance of long-lasting insecticide nets. Parasit Vectors. 2013;6:82. doi: 10.1186/1756-3305-6-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Diouf A, Diop YM, Ndiaye B, Fall M, Sarr D, Thiam A, et al. Mango leaves (Manguifera indica, Anacardiacea) used as biomarker of pollution by pp’Dichlorodiphenyltrichloroethane (pp’DDT) Dakar Med. 2000;45:122–125. [PubMed] [Google Scholar]
- 46.Marco JA, Kishimba MA. Organochlorine pesticides and metabolites in young leaves of Mangifera indica from sites near a point source in Coast region, Tanzania. Chemosphere. 2007;68:832–837. doi: 10.1016/j.chemosphere.2007.02.026. [DOI] [PubMed] [Google Scholar]
- 47.Samir SR, Leo MLN. Pesticides: evaluation of environmental pollution. Boca Raton: CRC Press; 2012. [Google Scholar]
- 48.Chouaibou M, Etang J, Brevault T, Nwane P, Hinzoumbe CK, Mimpfoundi R, et al. Dynamics of insecticide resistance in the malaria vector Anopheles gambiae s.l. from an area of extensive cotton cultivation in Northern Cameroon. Trop Med Int Health. 2008;13:476–486. doi: 10.1111/j.1365-3156.2008.02025.x. [DOI] [PubMed] [Google Scholar]
- 49.Diabate A, Baldet T, Chandre F, Akogbeto M, Guiguemde TR, Darriet F, et al. The role of agricultural use of insecticides in resistance to pyrethroids in Anopheles gambiae s.l. in Burkina Faso. Am J Trop Med Hyg. 2002;67:617–622. doi: 10.4269/ajtmh.2002.67.617. [DOI] [PubMed] [Google Scholar]
- 50.Tia E, Akogbeto M, Koffi A, Toure M, Adja AM, Moussa K, Yao T, Carnevale P, Chandre E. Pyrethroid and DDT resistance of Anopheles gambiae s.s. (Diptera: Culicidae) in five agricultural ecosystems from Côte-d’Ivoire. Bull Soc Pathol Exot. 2006;99:278–282. [PubMed] [Google Scholar]
- 51.Fontenille D, Lochouarn L, Diagne N, Sokhna C, Lemasson JJ, Diatta M, et al. High annual and seasonal variations in malaria transmission by anophelines and vector species composition in Dielmo, a holoendemic area in Senegal. Am J Trop Med Hyg. 1997;56:247–253. doi: 10.4269/ajtmh.1997.56.247. [DOI] [PubMed] [Google Scholar]
- 52.Sougoufara S, Harry M, Doucoure S, Sembene PM, Sokhna C. Shift in species composition in the Anopheles gambiae complex after implementation of long-lasting insecticidal nets in Dielmo, Senegal. Med Vet Entomol. 2016;30:365–368. doi: 10.1111/mve.12171. [DOI] [PubMed] [Google Scholar]
- 53.Verhaeghen K, Van Bortel W, Roelants P, Backeljau T, Coosemans M. Detection of the East and West African kdr mutation in Anopheles gambiae and Anopheles arabiensis from Uganda using a new assay based on FRET/Melt Curve analysis. Malar J. 2006;5:16. doi: 10.1186/1475-2875-5-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Antonio-Nkondjio C, Tene Fossog B, Kopya E, Poumachu Y, Menze Djantio B, Ndo C, et al. Rapid evolution of pyrethroid resistance prevalence in Anopheles gambiae populations from the cities of Douala and Yaounde (Cameroon) Malar J. 2015;14:155. doi: 10.1186/s12936-015-0675-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Cisse MB, Keita C, Dicko A, Dengela D, Coleman J, Lucas B, et al. Characterizing the insecticide resistance of Anopheles gambiae in Mali. Malar J. 2015;14:327. doi: 10.1186/s12936-015-0847-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Dabire RK, Namountougou M, Diabate A, Soma DD, Bado J, Toe HK, et al. Distribution and frequency of kdr mutations within Anopheles gambiae s.l. populations and first report of the ace.1 G119S mutation in Anopheles arabiensis from Burkina Faso (West Africa) PLoS ONE. 2014;9:e101484. doi: 10.1371/journal.pone.0101484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Edi CV, Koudou BG, Jones CM, Weetman D, Ranson H. Multiple-insecticide resistance in Anopheles gambiae mosquitoes, Southern Côte d’Ivoire. Emerg Infect Dis. 2012;18:1508–1511. doi: 10.3201/eid1809.120262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Namountougou M, Simard F, Baldet T, Diabate A, Ouedraogo JB, Martin T, et al. Multiple insecticide resistance in Anopheles gambiae s.l. populations from Burkina Faso, West Africa. PLoS ONE. 2012;7:e48412. doi: 10.1371/journal.pone.0048412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Yadouleton AW, Padonou G, Asidi A, Moiroux N, Bio-Banganna S, Corbel V, et al. Insecticide resistance status in Anopheles gambiae in southern Benin. Malar J. 2010;9:83. doi: 10.1186/1475-2875-9-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.el Niang HA, Konate L, Diallo M, Faye O, Dia I. Patterns of insecticide resistance and knock down resistance (kdr) in malaria vectors An. arabiensis, An. coluzzii and An. gambiae from sympatric areas in Senegal. Parasit Vectors. 2016;9:71. doi: 10.1186/s13071-016-1354-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Che-Mendoza A, Patricia Penilla R, Rodriguez DA. Insecticide resistance and glutathione S-transferase in mosquitoes: a review. Afr J Biotech. 2009;8:1386–1387. [Google Scholar]
- 62.Gunasekaran K, Muthukumaravel S, Sahu SS, Vijayakumar T, Jambulingam P. Glutathione S transferase activity in Indian vectors of malaria: a defense mechanism against DDT. J Med Entomol. 2011;48:561–569. doi: 10.1603/ME10194. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.


