Abstract
OBJECTIVE
Our objective was to characterize diabetes-specific health-related quality of life (D-HRQOL) in a global sample of youth and young adults with type 1 diabetes (T1D) and to identify the main factors associated with quality of life.
RESEARCH DESIGN AND METHODS
The TEENs study was an international, cross-sectional study of youth, 8–25 years of age, with T1D. Participants (N = 5,887) were seen in clinical sites in 20 countries across 5 continents enrolled for 3 predetermined age groups: 8–12, 13–18, and 19–25 years of age. To assess D-HRQOL, participants completed the PedsQL Diabetes Module 3.0 and were interviewed about family-related factors. Specifics about treatment regimen and self-management behaviors were collected from medical records.
RESULTS
Across all age groups, females reported significantly lower D-HRQOL than did males. The 19–25-year age group reported the lowest D-HRQOL. Multivariate linear regression analyses revealed that D-HRQOL was significantly related to HbA1c; the lower the HbA1c, the better the D-HRQOL. Three diabetes-management behaviors were significantly related to better D-HRQOL: advanced methods used to measure food intake; more frequent daily blood glucose monitoring; and more days per week that youth had ≥30 min of physical activity.
CONCLUSIONS
In all three age groups, the lower the HbA1c, the better the D-HRQOL, underscoring the strong association between better D-HRQOL and optimal glycemic control in a global sample of youth and young adults. Three diabetes-management behaviors were also related to optimal glycemic control, which represent potentially modifiable factors for clinical interventions to improve D-HRQOL as well as glycemic control.
Introduction
Contemporary clinical trials of new medications and treatment technologies increasingly include patient-reported outcomes such as quality of life in addition to objective health outcomes (1). Subjective factors such as disease self-management burden or disease impact on social functioning are especially important for individuals with type 1 diabetes (T1D) because T1D is primarily a self-managed condition (2). The Pediatric Self-Management Framework (3) served as the theoretical model for this research on diabetes-specific health-related quality of life (D-HRQOL). The Pediatric Self-Management Framework is a comprehensive conceptual model of pediatric self-management that takes into account individual, family, and health care system influences that affect self-management and also describes the relationships among self-management behavior, adherence, and patient outcomes.
As intensive insulin regimens become the standard of care for youth with T1D, the burdens placed on the routines and relationships of youth and their families also increase (4). Consequently, national and international clinical practice guidelines are increasingly recommending that diabetes care providers use HRQOL instruments to assess and care for patients with diabetes (5,6).
For children and teens with a medical condition, HRQOL can include satisfaction with the current status and treatment of the condition; the impact of the condition on physical, social, and emotional functioning; and how much one worries about or is distressed by the condition (7). Instruments that measure HRQOL can capture the impact of having a chronic health condition in general (Generic HRQOL) or may emphasize the particular impact of a specific condition (e.g., diabetes) on everyday life (D-HRQOL). Higher levels of D-HRQOL (i.e., better life quality in relation to diabetes) predict key diabetes outcomes, including greater adherence to treatment recommendations and optimal glycemic control in youth with T1D (8–10), emphasizing its central role in diabetes management and control.
Although D-HRQOL has also been reported to be associated with adherence in youth with T1D, in these studies, adherence is usually measured as a unitary construct using a single score. D-HRQOL has not been examined in relationship to specific self-management behaviors. The identification of specific self-management behaviors that relate to D-HRQOL may help to fill an important gap in understanding the bidirectional relationship between higher D-HRQOL and better glycemic control. Most importantly, as conceptualized in the Pediatric Self-Management Framework (3), self-management behavior is one of the most proximal and potentially modifiable variables available to pediatric care providers as targets for interventions.
The focus of the present report is on the interrelationship between D-HRQOL and glycemic control as well as on the identification of individual, family, and diabetes self-management factors that are associated with optimal D-HRQOL in the global TEENs study. The primary aim of the TEENs study was to characterize diabetes-specific quality of life and glycemic control of a global sample of patients with T1D in three predetermined age groups (8–12, 13–18, and 19–25 years).
Research Design and Methods
The TEENs study was a global, observational, cross-sectional study of youth and young adults, 8–25 years of age, with T1D launched across 5 continents in 20 countries in 2012.
Recruitment Procedures
In each country, young persons enrolled in the TEENs study received their care in centers with at least 100 pediatric and/or young adult patients with T1D that were representative of the typical medical care delivered in their respective countries. At each of the study centers, the TEENs study protocol was approved by the appropriate Institutional Review Board or ethics review board. Signed written informed consent was obtained from the participant if applicable and from the parent(s)/guardian(s). Youth were enrolled sequentially or randomly to avoid selection bias, with a recruitment ratio of 25/50/25% for the 3 predetermined age groups (school age 8–12 years; adolescents 13–18 years; and young adults 19–25 years). Half of the intended sample included adolescents because of the focus on investigating diabetes management during this developmental stage, recognized for its physiologic and behavioral challenges affecting glycemic control. The recruitment period extended from 14 August 2012 until 6 September 2013.
Participants
Inclusion criteria were youth aged 8–25 years, with T1D diagnosed before 18 years of age and duration of diabetes of ≥1 year at enrollment. Participants had no major change in insulin regimen during the last 3 months (no transition between pump and injection therapy). Of the 5,968 participants who were screened, 5,887 were deemed eligible.
Measures
Demographic data, treatment characteristics, and self-management behavior data were collected by medical record review. Parents/guardians completed questionnaires and interviews; youth completed questionnaires and interviews.
Demographic Data
At each site, demographic data (race/ethnicity and date of birth) were captured from the youth’s medical record (except in France, where government regulations prohibit the collection of patient’s race/ethnicity information).
D-HRQOL
All youth (8–25 years) completed the age-appropriate version of the PedsQL Diabetes Module 3.0 (11), the most widely used D-HRQOL measure in youth with T1D (12). The PedsQL Diabetes Module 3.0 has been translated into and validated in multiple languages. The questionnaire is composed of 28 items that are divided into 5 subscales: 1) diabetes symptoms (e.g., feeling hungry); 2) treatment barriers (e.g., embarrassment); 3) treatment adherence (e.g., hard to take blood glucose tests); 4) worry (e.g., going low); and 5) communication problems (e.g., hard for me to explain my illness to other people). Frequently, data from the PedsQL Diabetes Module 3.0 have been reported in terms of scores on the five subscales. However, recently, Hilliard et al. (13) reported that the α coefficients for the original five subscales are lower than desirable, ranging from 0.61 to 0.75. Moreover, the five subscales do not represent statistically distinct measurement factors. Two studies of youth with T1D, Nansel et al. (14) (N = 437) and Lawrence et al., the SEARCH Study Group (15) (N = 2,602), have recently tested the factor structure of the PedsQL Diabetes Module 3.0 and reported that the original five subscales were not supported by factor analyses nor did a clear factor structure emerge from principal components analysis. Both studies reported that a total PedsQL Diabetes Module score was the most psychometrically appropriate use of this measure as compared with analysis of subscale scores. Therefore, we used the total score on the PedsQL Diabetes Module 3.0 in the TEENs study because of its strong psychometric properties.
On the PedsQL Diabetes Module 3.0, the total score ranges between 0 and 100, and higher scores represent better D-HRQOL (16). Two age-specific versions of the PedsQL Diabetes Module 3.0 were used: 8–12 and 13–18 years. If a participant in the 8–12-year-old group had problems reading the questionnaire, an interviewer, not the parent, read the questionnaire to the child to avoid parent influence on the child’s responses. Participants in the 19–25-year-old group completed the 13–18-year-old version of the PedsQL Diabetes Module. All of the items on the Teen version of the Diabetes Module were also relevant to the young adult cohort.
Treatment Characteristics and Self-Management Behavior
Specifics about each youth’s regimen type (such as insulin delivery method and use of diabetes treatment technologies) and self-management behaviors (such as frequency of daily blood glucose monitoring, amount of physical activity, and dietary strategy [used to manage blood glucose]) were collected from medical records. Objective measures of self-management behaviors, such as blood glucose meter and pump downloads, were not possible because of the inconsistency in centers’ having the computers and software to collect these more objective measures.
Family Factors
To gather information about how parents and youth divided up responsibility for the diabetes tasks of administering insulin and monitoring blood glucose levels, two items were taken from the validated Diabetes Family Responsibility Questionnaire (17) and collected by participant interview. Participants were also interviewed about diabetes-specific family conflict based on two questions taken from the validated Revised Diabetes Family Conflict Scale (18). Because of the need to reduce response burden on participants, only two items were selected from each instrument. These items were selected because they focused on the two primary areas of diabetes management: insulin administration and blood glucose monitoring. In other words, diabetes family responsibility-sharing and diabetes family conflict were assessed with respect to insulin administration as well as to blood glucose monitoring. These interview questions based on items from the Diabetes Family Responsibility Questionnaire and Revised Diabetes Family Conflict Scale were translated using standard forward and backward translation methods.
Glycemic Control
HbA1c values were not measured in a central laboratory. However, all centers followed standardized procedures, including HbA1c measurement. At all TEENs study sites, glycemic control was measured uniformly using point of care A1cNow (Bayer) (reference range 4–6%) calibrated to Diabetes Control and Complications Trial (DCCT)/NGSP percentage numbers. HbA1c target definitions were based on International Society for Pediatric and Adolescent Diabetes standards for ages 8–12 and 13–18 years as <7.5% (58 mmol/mol) (19) or the ADA for ages 19–25 years, with the HbA1c target as <7% (53 mmol/mol) (20). Because the protocol called for research procedures to occur at the participants’ regular diabetes clinic appointment at all clinical sites, for the vast majority of youth, the HbA1c value used in data analysis was the one measured on the day of that clinic visit when study questionnaires and interviews were conducted.
Statistical Analysis
The primary research questions and main objective of the data analysis plan were to describe glycemic control, self-management behavior, as well as family and demographic factors associated with D-HRQOL. This was a hypothesis-generating research design rather than a hypothesis-testing design. The sample size justification was based on the expected precision of a two-sided 95% CI for a single proportion. A global precision including all of the countries was calculated. Assuming that patient at target for HbA1c named “glycemic control” was achieved in ∼40% of patients and assuming a nonevaluability rate (patients without full documentation of HbA1c) of ∼5% using the capillary method, the inclusion of 500 to 1,500 patients per country/region (e.g., group of countries) allowed us to calculate two-sided 95% CI with a precision between 2.5 and 4.4% (all age groups taken into account). With a recruitment ratio of 25, 50, and 25% in the different predefined age groups of 8–12, 13–18, and 19–25 years, respectively, the precision was between 5.1 and 8.8% in the age groups 8–12 and 19–25 years and between 3.6 and 6.2% in the age group 13–18 years. If the frequency of glycemic control was <40%, the precision was better.
Outcomes are analyzed according to age group. Multivariate linear regression was used to identify patient and family characteristics associated with D-HRQOL total score. In every multivariate analysis, region and age groups were the only covariates. Multivariate linear regression was also used to identify diabetes regimen and self-management behavior characteristics associated with D-HRQOL total score (with region and age group as covariates).
Results
Participant and Family Characteristics
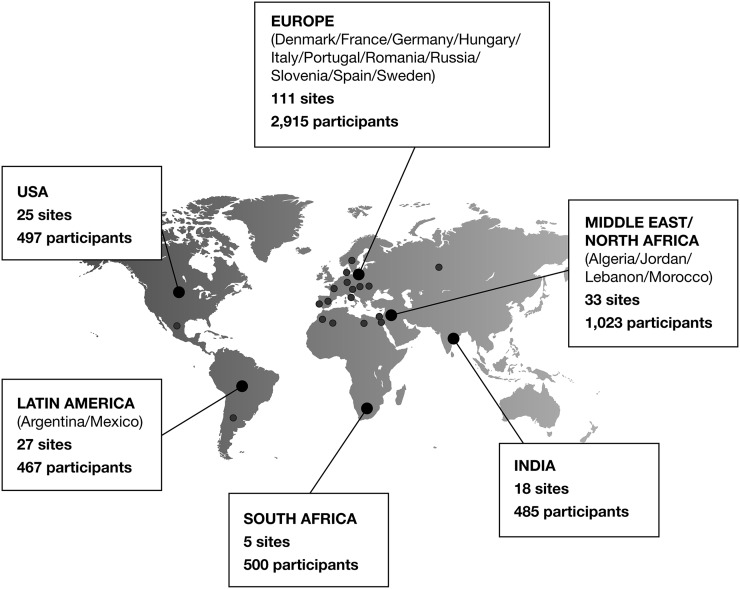
The geographic representation of participating countries, sites, and participants is illustrated in Fig. 1. The 5,887 TEENs participants were from 6 major regions, 5 continents, over 20 countries, and 219 centers worldwide. Countries were grouped into six regions according to health care delivery systems and status as developed or developing country.
Figure 1.
Geographic representation of countries, sites, and participants involved in the global TEENs study.
Characteristics of the global TEENs participants are reported in Table 1 and Supplementary Table 1. The mean ages of the 3 predetermined age groups (8–12, 13–18, and 19–25 years) were 10.3, 15.3, and 21.3 years, respectively. Males and females were represented equally in all three age groups. Three-fourths of the participants in each age group were Caucasian. As reported in Table 1, age at diabetes diagnosis (as a surrogate for diabetes duration) was not related to D-HRQOL.
Table 1.
Factors associated with D-HRQOL in multivariate linear regression
| Explanatory variable interpretation | 8–12years | 13–18 years | 19–25 years | All | Adjusted means (SE)* | Estimate (95% CI)* | P value* |
|---|---|---|---|---|---|---|---|
| Patient characteristics | |||||||
| Sex | <0.001 | ||||||
| n | 1,715 | 2,846 | 1,326 | 5,887 | |||
| Male (reference) | 51 | 52 | 51 | 51 | 70.2 (0.3) | 0.0 | |
| Female | 49 | 48 | 49 | 49 | 66.2 (0.3) | −4.0 (−4.7, −3.4) | <0.001 |
| BMI (kg/m2) | 0.040 | ||||||
| n | 1,711 | 2,842 | 1,320 | 5,873 | |||
| Underweight/normal (reference) | 71 | 74 | 71 | 73 | 68.7 (0.3) | 0.0 | |
| Overweight | 16 | 15 | 24 | 17 | 68.7 (0.4) | 0.0 (−0.9, 0.9) | 0.942 |
| Obese | 13 | 11 | 6 | 10 | 67.3 (0.6) | −1.4 (−2.6, −0.3) | 0.012 |
| Age at diagnosis (years) | 0.010 | ||||||
| n | 1,715 | 2,846 | 1,326 | 5,887 | |||
| ≥10 (reference) | 43 | 20 | 16 | 26 | 68.0 (0.4) | 0.0 | |
| <6 | 49 | 33 | 25 | 36 | 69.0 (0.4) | 0.9 (0.0, 1.8) | 0.050 |
| ≥6 to <10 | 8 | 47 | 59 | 39 | 67.6 (0.4) | −0.4 (−1.2, 0.4) | 0.344 |
| HbA1c (%) | <0.001 | ||||||
| n | 1,714 | 2,846 | 1,325 | 5,885 | |||
| <7.5 (reference) | 32 | 29 | 33 | 31 | 71.5 (0.4) | 0.0 | |
| ≥7.5 to <9.0 | 42 | 36 | 37 | 38 | 68.4 (0.4) | −3.2 (−4.0, −2.4) | <0.001 |
| ≥9.0 | 26 | 35 | 30 | 31 | 64.8 (0.4) | −6.8 (−7.7, −5.9) | <0.001 |
| Family characteristics | |||||||
| Person living with patient | 0.029 | ||||||
| n | 1,712 | 2,844 | 1,324 | 5,880 | |||
| Living with both parents (reference) | 85 | 82 | 67 | 79 | 66.9 (0.3) | 0.0 | |
| Only mother/only father | 13 | 15 | 12 | 13 | 65.7 (0.5) | −1.2 (−2.3, −0.2) | 0.018 |
| Alone + other | 3 | 4 | 22 | 8 | 65.9 (0.7) | −1.1 (−2.5, 0.3) | 0.127 |
| What is the highest level of education either of the patient’s parents/guardians completed? | <0.001 | ||||||
| n | 1,673 | 2,791 | 1,274 | 5,738 | |||
| Illiterate/primary (reference) | 16 | 17 | 21 | 17 | 65.2 (0.6) | 0.0 | |
| Secondary | 42 | 44 | 43 | 43 | 66.0 (0.4) | 0.7 (−0.3, 1.7) | 0.165 |
| University/higher | 42 | 40 | 37 | 40 | 67.3 (0.4) | 2.1 (1.1, 3.2) | <0.001 |
| Conflict for check and interpret blood glucose levels over the past month | <0.001 | ||||||
| n | 1,706 | 2,837 | 1,314 | 5,857 | |||
| Almost never (reference) | 54 | 48 | 67 | 54 | 67.8 (0.5) | 0.0 | |
| Sometimes + almost always | 46 | 52 | 33 | 46 | 64.5 (0.4) | −3.2 (−4.3, −2.2) | <0.001 |
| Conflict for select and give insulin doses over the past month | 0.254 | ||||||
| n | 1,706 | 2,837 | 1,314 | 5,857 | |||
| Almost never (reference) | 60 | 56 | 73 | 61 | 66.5 (0.4) | 0.0 | |
| Sometimes + almost always | 40 | 44 | 27 | 39 | 65.9 (0.5) | −0.6 (−1.7, 0.5) | 0.254 |
| Has the patient or his/her family members cut down or stopped working because of diabetes? | <0.001 | ||||||
| n | 1,704 | 2,832 | 1,315 | 5,851 | |||
| No (reference) | 82 | 89 | 91 | 88 | 67.5 (0.3) | 0.0 | |
| Yes | 18 | 11 | 9 | 12 | 64.8 (0.6) | −2.7 (−3.7, −1.6) | <0.001 |
Data are n or n (%) unless otherwise indicated. Boldface P values indicate overall factor is significantly related to HRQOL score.
*Based on N = 5,741 (5,882) for patient (family) characteristics analysis, respectively.
Family factors are also reported in Supplementary Table 1 by age group and for the entire sample. Percentages of participants who lived with both parents were 85, 82, and 67% for the 8–12-, 13–18-, and 19–25-year-old groups, respectively. With respect to highest level of parental education in all three age groups, overall, ∼40% of the participants’ parents had reached high-school diploma level. With respect to participant or parent having to cut back or stop work because of diabetes, 18, 11, and 9% of families cut back or stopped work for the 8–12-, 13–18-, and 19–25-year-old groups, respectively. Concerning parent involvement in diabetes management, with advancing age of the youth, the percent of parental involvement decreased as expected. Overall, 46% of youth endorsed family conflict over monitoring blood glucose, and 39% of youth endorsed family conflict over giving insulin.
Diabetes Self-Management and Insulin Regimen Characteristics
Table 2 presents diabetes self-management and insulin regimen characteristics of the sample by age group and for the entire sample.
Table 2.
Diabetes regimen and self-management behavior characteristics associated with D-HRQOL in multivariate linear regression
| Explanatory variable interpretation | 8–12 years | 13–18 years | 19–25 years | All | Adjusted means (SE)* | Estimate (95% CI)* | P value* |
|---|---|---|---|---|---|---|---|
| Insulin regimen | 0.100 | ||||||
| n | 1,715 | 2,846 | 1,326 | 5,887 | |||
| Basal bolus regimen (reference) | 66.6 | 67.8 | 72.6 | 68.5 | 65.6 (0.7) | 0.0 | |
| Pump only | 25.6 | 24.7 | 19.5 | 23.8 | 66.5 (0.8) | 0.8 (−0.1, 1.7) | 0.081 |
| Any other insulin regimen | 7.8 | 7.5 | 7.8 | 7.7 | 64.8 (0.9) | −0.8 (−2.3, 0.6) | 0.270 |
| Methods used to measure food intake for diabetes management | <0.001 | ||||||
| n | 1,673 | 2,760 | 1,270 | 5,703 | |||
| Only avoids sugars/added sugars (reference) | 11 | 10 | 9 | 10 | 63.2 (0.9) | 0.0 | |
| Carbohydrate counting | 44 | 40 | 42 | 41 | 67.1 (0.7) | 3.9 (2.4, 5.5) | <0.001 |
| Carbohydrate exchanges/weighing/measuring | 15 | 15 | 8 | 13 | 66.3 (0.8) | 3.1 (1.5, 4.7) | <0.001 |
| Estimation based on experience | 31 | 36 | 42 | 36 | 66.0 (0.7) | 2.9 (1.4, 4.3) | <0.001 |
| On average in a 1-month period, about how many times per day is the participant checking his/her blood glucose with a blood glucose meter? | <0.001 | ||||||
| n | 1,708 | 2,822 | 1,316 | 5,846 | |||
| ≥0 to ≤2 (reference) | 13 | 23 | 40 | 24 | 63.3 (0.8) | 0.0 | |
| >2 to ≤4 | 32 | 44 | 41 | 40 | 65.7 (0.7) | 2.3 (1.3, 3.4) | <0.001 |
| >4 to ≤5 | 18 | 15 | 11 | 15 | 67.1 (0.8) | 3.8 (2.5, 5.0) | <0.001 |
| >5 | 38 | 18 | 8 | 22 | 66.5 (0.8) | 3.2 (2.0, 4.5) | <0.001 |
| Diabetic ketoacidosis | <0.001 | ||||||
| n | 1,715 | 2,845 | 1,326 | 5,886 | |||
| No (reference) | 94 | 94 | 94 | 94 | 67.3 (0.6) | 0.0 | |
| Yes | 6 | 6 | 6 | 6 | 64.0 (0.9) | −3.2 (−4.8, −1.7) | <0.001 |
| Severe hypoglycemia resulting in seizure or loss of consciousness | 0.086 | ||||||
| n | 1,714 | 2,845 | 1,326 | 5,885 | |||
| No (reference) | 98 | 98 | 96 | 97 | 66.6 (0.5) | 0.0 | |
| Yes | 3 | 2 | 4 | 3 | 64.7 (1.2) | −1.9 (−4.1, 0.3) | 0.086 |
| Number of days when the participant spent at least 30 min doing any physical activities or exercise per week | <0.001 | ||||||
| n | 1,687 | 2,812 | 1,301 | 5,800 | |||
| 0–2 (reference) | 33 | 38 | 44 | 38 | 64.5 (0.7) | 0.0 | |
| 3–7 | 67 | 62 | 56 | 62 | 66.7 (0.7) | 2.2 (1.5, 2.9) | <0.001 |
Data are n or n (%) unless otherwise indicated. Boldface P values indicate overall factor is significantly related to HRQOL score.
*Based on N = 5,460.
HbA1c Target Attainment and Distribution by Age Group
HbA1c target attainments by age group and for the entire sample as well as mean HbA1c by age group and for the entire sample are reported in Supplementary Fig. 1. Only 31.9% of 8–12-year-old youth achieved HbA1c target, 29.1% of 13–18-year-olds achieved HbA1c target, and 18.4% of the young adult group achieved HbA1c target.
Diabetes Quality of Life Reported by Youth With T1D
Table 3 reports the median as well as lowest and highest tertiles in the distribution of D-HRQOL total scores by age group and overall. Table 3 also reports the number (percentage) of youth according to quartiles classification based on the overall population. Higher mean scores represent better D-HRQOL. The 19–25-year-old group of young adults reported the lowest D-HRQOL compared with the two younger age groups.
Table 3.
Participant self-report, D-HRQOL total score, for the eligible population
| 8–12 years (N = 1,715) | 13–18 years (N = 2,846) | 19–25 years (N = 1,326) | Total (N = 5,887) | |||||
|---|---|---|---|---|---|---|---|---|
| Total scale score (child) | ||||||||
| N | 1,690 | 2,806 | 1,260 | 5,756 | ||||
| Mean (SD) | 71.91 (13.18) | 70.09 (13.68) | 67.83 (14.25) | 70.13 (13.74) | ||||
| 95% CI | 71.28; 72.54 | 69.58; 70.59 | 67.05; 68.62 | 69.77; 70.48 | ||||
| Median | 73.21 | 71.43 | 69.20 | 71.43 | ||||
| Q1; Q3 | 63.39; 82.14 | 61.61; 80.36 | 58.93; 78.57 | 61.61; 80.36 | ||||
| Total score (in quartiles) | ||||||||
| N | 1,690 | 2,806 | 1,260 | 5,756 | ||||
| <61.61 | 335 (19.8%) | 692 (24.7%) | 373 (29.6%) | 1,400 (24.3%) | ||||
| ≥61.61 to <71.43 | 396 (23.4%) | 668 (23.8%) | 317 (25.2%) | 1,381 (24.0%) | ||||
| ≥71.43 to <80.36 | 463 (27.4%) | 739 (26.3%) | 317 (25.2%) | 1,519 (26.4%) | ||||
| ≥80.36 | 496 (29.3%) | 707 (25.2%) | 253 (20.1%) | 1,456 (25.3%) | ||||
Quartiles for total score in classes are based on total eligible population.
Factors Associated With Total D-HRQOL Scores in Multivariate Linear Regression
Table 1 reports demographic and family factors associated with total D-HRQOL scores (adjusted for age group and region) in a multivariate linear regression analysis.
Across all age groups, females with T1D reported lower D-HRQOL than males with T1D (66.2 [SE 0.3] vs. 70.2 [SE 0.3]; P < 0.001).
In multivariate linear regression analyses controlling for age group and region, mean total D-HRQOL scores revealed that D-HRQOL was significantly related to HbA1c: the lower the HbA1c, the better the D-HRQOL (HbA1c <7.5%, D-HRQOL = 71.5 [SE.4]; HbA1c ≥7.5 to <9%, D-HRQOL = 68.4 [0.4]; and HbA1c >9.0%, D-HRQOL = 64.8 [0.4]; P < 0.001).
Level of parental education was significantly related to D-HRQOL, as the higher the level of parental education, the better the D-HRQOL. As reported in Table 1, the presence of diabetes-specific family conflict over blood glucose monitoring was significantly related to poorer D-HRQOL (P < 0.001). Also, if a parent or participant had to reduce or stop working because of diabetes, the participant reported lower D-HRQOL (P < 0.001).
Results of analyses to explore the relationship between highest level of parental education and D-HRQOL indicated that the higher the level of education attained by the parent, the better the youth’s D-HRQOL (P < 0.001). Furthermore, for families in which extra income was needed to cover the medical costs of diabetes, participants reported significantly lower D-HRQOL (P < 0.001).
Diabetes Regimen and Self-Management Behavior Characteristics Associated With Total D-HRQOL Scores in Multivariate Linear Regression
Table 2 reports the diabetes-management characteristics associated with D-HRQOL total scores (adjusted for age group and region) in multivariate linear regression analysis. Three diabetes-management factors were significantly related to D-HRQOL: among methods used to measure food intake, advanced diet methods (e.g., carbohydrate counting compared with avoiding simple sugars) was related to better D-HRQOL (P < 0.001); more frequent daily blood glucose monitoring was related to better D-HRQOL (P < 0.001); and more days per week (3–7 compared with 0–2 days/week) in which youth had 30 min of physical activity was related to better D-HRQOL (P < 0.001).
Conclusions
The TEENs study has provided the largest and best-characterized evaluation of diabetes-specific quality of life in a global, contemporary sample of 8–25-year-olds with T1D to date. Results indicated that there is a linear relationship between quality of life and HbA1c, with youth who attain an HbA1c target of <7.5% reporting the highest quality of life; youth with HbA1c >7.5 and <9.0% reporting significantly lower quality of life; and youth in the worst control with HbA1c >9.0% reporting quality of life that is significantly lower than each of the other two HbA1c groups. It is highly likely that this is a bidirectional relationship with HbA1c and diabetes quality of life interrelated. No statement of causality can be made from the TEENs cross-sectional data. A longitudinal report by Hilliard et al. (8) documented that in a sample of U.S. teens with T1D, quality of life predicted HbA1c. More longitudinal studies are needed to clarify any causal relationships between D-HRQOL and glycemic control.
Our finding that youth who report (on the PedsQL Diabetes Module 3.0) feeling more burdened by daily diabetes treatment tasks (like checking blood glucose) are characterized by checking blood glucose less frequently (as measured by medical chart review) and by poorer glycemic control (as measured by HbA1c) documents the interconnectedness of diabetes burden, self-management behaviors, and biological outcomes in this global sample of youth with T1D. These interrelationships highlight potential points for intervention—by reducing diabetes burden, youth may check blood glucose levels more frequently, which has been documented to correlate with better glycemic control (21).
With respect to D-HRQOL in the global TEENs population, it is significant that across age groups, females with T1D consistently reported lower D-HRQOL than did their male peers. This finding is consistent with results from the multinational Hvidore Study (9) as well as the SEARCH study (15) of youth with T1D in which females also reported lower D-HRQOL on the PedsQL Diabetes module. Other investigations of quality of life in youth with T1D have reported that girls with T1D reported significantly lower quality of life than did boys with T1D of the same age (22,23). Grey et al. (22) proposed that girls worried more about diabetes than boys did; and Wiebe et al. (23) suggested that adolescent girls with T1D are more demanding of themselves than are their male counterparts. Similarly, Eiser et al. (24) reported that young adult females with T1D reported a more negative quality of life compared with young adult males with T1D. Empirical studies with youth with other chronic illnesses have also reported lower quality of life in girls. With a sample of adolescents with epilepsy, girls with high seizure severity were at highest risk for poor quality of life (25). In a sample of adolescents with chronic pain, females reported significantly lower quality of life than males (26). Furthermore, in a large study of HRQOL in healthy youth across 12 European countries, with increasing age, HRQOL declined significantly more for girls than for boys (27).
Clearly, the poorer self-reported D-HRQOL reported by adolescent girls and young adult females with T1D in the TEENs study points to an important area of marked vulnerability for adolescent and young adult females with T1D that requires increased research and improved clinical interventions.
Across all age groups, the report of diabetes-specific family conflict was significantly related to poorer D-HRQOL. This implies that clinicians should pay attention to the building up or existing presence of diabetes-specific family conflict during routine clinic visits and engage the parent and youth in discussions to diffuse the conflict and build family teamwork around diabetes management or, if the diabetes family conflict is extremely severe, to refer the family for family therapy. Mental health factors (anxiety, depression, and eating disorders) also contribute to poor D-HRQOL. In the SEARCH study, the PedsQL Diabetes Module total score was 20 points lower in youth with moderate to severe depressive symptoms compared with youth with no or minimal depressive symptoms (17).
The most important contribution of the findings reported in this study might be in the data on the significant relationships among three specific diabetes self-management behaviors and D-HRQOL. First, the finding that increased frequency of daily self-monitoring of blood glucose is significantly related to optimal D-HRQOL is consistent with the growing body of evidence that frequency of daily self-monitoring blood glucose is related to optimal glycemic as well as psychosocial outcomes (21,28). Secondly, the finding that among methods used to measure food intake in a global sample of youth with T1D, carbohydrate counting was related to better D-HRQOL. Educating youth and parents to quantify food intake to facilitate accurate adjustment of insulin may be a potential path to improve D-HRQOL. Third, the results from this global sample indicated that youth who exercised more days per week at least 30 min per day had better D-HRQOL is important in that this is a diabetes self-management strategy that can be encouraged for youth with T1D even in the most resource-restricted countries. In the current sample of 5,887 youth with T1D, there was a significant relationship between higher quality of life and youth who checked blood glucose more frequently, exercised more days/week, or used advanced methods to measure food intake. This association between higher quality of life and increased use of contemporary diabetes-management strategies is a relationship, and highly likely a bidirectional relationship, and not a causal pathway.
The current research is limited in that it used a cross-sectional design carried out in larger centers. The centers were not selected at random but on their capacity to recruit a high number of participants and fulfill requirements for completing questionnaires. Youth who took part in this research in each of the participating countries received their diabetes health care in larger centers that cared for >100 pediatric patients annually with T1D. Thus, the results of this study need to be verified using a different global strategy for possibly sampling smaller, less experienced clinical sites across different sites in different countries. Secondly, only age grouping and region were used as covariates in the multivariate analyses. Other potentially important covariates such as parental educational level and sex were not used. Thirdly, self-management behavior was based on documentation in the youth’s medical record rather than more objective measures. Objective measures of self-management behaviors, such as blood glucose meter and pump downloads, were not possible because of the inconsistency in centers’ having the computers and software to collect these objective measures. A potential limitation of this study is the lack of a central laboratory for measuring HbA1c values, although all centers followed standardized procedures using a study-provided point of care A1cNow (Bayer; reference range 4–6%) calibrated to DCCT/NGSP percentage numbers. This unified approach to HbA1c measurement using a point-of-care assay is similar to HbA1c measurement using a central laboratory.
Finally, because of the cross-sectional design of the current study, it will be important to test the hypotheses generated in this study in a longitudinal study of global youth with T1D. However, given the enormous expense and feasibility challenges in tracking a global sample of youth with T1D, the results from the cross-sectional TEENs study are important with respect to calling for prioritization of the immediate development of effective clinical interventions to optimize glycemic control and D-HRQOL of youth with T1D, especially for adolescent and young adult females with T1D.
In conclusion, in this well-characterized global cohort of 5,887 participants 8–25 years of age with T1D in the TEENs study, in each age group, the lower the HbA1c, the better the patient-reported outcome of D-HRQOL. With respect to other factors significantly related to D-HRQOL, lower level of parental education was related to poorer D-HRQOL; the presence of diabetes-specific family conflict was related to poorer D-HRQOL; and when a parent or participant had to reduce or stop working because of diabetes, the participant reported lower D-HRQOL. Three diabetes self-management behaviors were significantly related to better quality of life: increased frequency of daily blood glucose monitoring, use of carbohydrate counting, and greater number of days per week of exercise for ≥30 min. Finally, young adults, 19–25 years of age, reported lower quality of life compared with the 13–18- and 8–12-year-old groups, and females in every age group reported lower quality of life than their male counterparts, calling attention to the vulnerability to poorer D-HRQOL in young adults and females with T1D.
Supplementary Material
Article Information
Acknowledgments. The multidisciplinary Steering Committee of the TEENs study thanks the participants and families, the study coordinators, and investigators from 219 centers in 20 countries for the efforts and commitment to this study as well as the sponsor, Sanofi Diabetes, for the financial support to perform this investigation.
Duality of Interest. Funding for the TEENs study was provided by Sanofi Diabetes. B.J.A. reports participation in advisory boards for Sanofi, research support from the National Institutes of Health, JDRF, The Leona M. and Harry B. Helmsley Charitable Trust, and consultancy for Sanofi. L.M.L. reports consultancy for Eli Lilly and Company, Sanofi, Novo Nordisk, AstraZeneca, Menarini, Johnson & Johnson, LifeScan/Animas, Roche Diagnostics, Oshadi, Dexcom, and Boehringer Ingelheim. C.D. is a full-time employee of Sanofi and shareholder. T.D. reports consultancy and participation in advisory boards for Sanofi, Novo Nordisk, Eli Lilly and Company, AstraZeneca, Roche, Unomedical, and Medtronic. M.P. reports paid lecturing for Johnson & Johnson (Animas), Sanofi, Medtronic, and Roche; stock ownership in CGM3 Ltd.; participation in advisory boards for Bristol-Myers Squibb, Sanofi, Medtronic, Eli Lilly and Company, and AstraZeneca; consultancy for Andromeda; and commercially sponsored research for Medtronic, Novo Nordisk, Eli Lilly and Company, Merck, Sanofi, Andromeda, and Dexcom. C.Maz. reports participation in the Type 1 Diabetes Advisory Board for Sanofi. R.H. reports participation in advisory boards for Eli Lilly and Company, Novo Nordisk, and Abbott and speaker honoraria for Novo Nordisk, Eli Lilly and Company, Sanofi, Roche, Medtronic, Dexcom, Menarini, and Abbott. S.W. reports participation in an advisory board for Sanofi and consultancy for Sanofi and Eli Lilly and Company. R.W.B. reports participation in advisory boards for Sanofi, consultancy for Animas, and research funding from Sanofi. F.C.-G. is an employee of Atlanstat. C.Mat. reports participation in advisory panels for Novo Nordisk, Sanofi, Merck Sharp & Dohme, Eli Lilly and Company, Novartis, Bristol-Myers Squibb, AstraZeneca, Pfizer, Johnson & Johnson, and MannKind; research support from Novo Nordisk, Sanofi, Merck Sharp & Dohme, Eli Lilly and Company, and Novartis; and participation in speaker bureaus for Novo Nordisk. No other potential conflicts of interest relevant to this article were reported.
Author Contributions. B.J.A. wrote and edited the manuscript. L.M.L., C.D., T.D., M.P., C.Maz., R.H., S.W., R.W.B., and C.Mat. reviewed and edited the manuscript. F.C.-G. performed statistical analyses and reviewed and edited the manuscript. B.J.A. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Prior Presentation. Parts of this study were presented in abstract form at the 74th Scientific Sessions of the American Diabetes Association, San Francisco, CA, 13–17 June 2014, at the 40th International Society for Pediatric and Adolescent Diabetes Congress, Toronto, Ontario, Canada, 3–6 September 2014, and at the World Diabetes Congress, Vancouver, British Columbia, Canada, 30 November to 4 December 2015.
Footnotes
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc16-1990/-/DC1.
References
- 1.Lohr KN, Zebrack BJ. Using patient-reported outcomes in clinical practice: challenges and opportunities. Qual Life Res 2009;18:99–107 [DOI] [PubMed] [Google Scholar]
- 2.Rubin RR, Peyrot M. Quality of life and diabetes. Diabetes Metab Res Rev 1999;15:205–218 [DOI] [PubMed] [Google Scholar]
- 3.Modi AC, Pai AL, Hommel KA, et al. . Pediatric self-management: a framework for research, practice, and policy. Pediatrics 2012;129:e473–e485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Laffel LMB, Connell A, Vangsness L, Goebel-Fabbri A, Mansfield A, Anderson BJ. General quality of life in youth with type 1 diabetes: relationship to patient management and diabetes-specific family conflict. Diabetes Care 2003;26:3067–3073 [DOI] [PubMed] [Google Scholar]
- 5.Silverstein J, Klingensmith G, Copeland K, et al.; American Diabetes Association . Care of children and adolescents with type 1 diabetes: a statement of the American Diabetes Association. Diabetes Care 2005;28:186–212 [DOI] [PubMed] [Google Scholar]
- 6.Delamater AM. Psychological care of children and adolescents with diabetes. Pediatr Diabetes 2009;10(Suppl. 12):175–184 [DOI] [PubMed] [Google Scholar]
- 7.Varni JW, Limbers CA, Burwinkle TM. Impaired health-related quality of life in children and adolescents with chronic conditions: a comparative analysis of 10 disease clusters and 33 disease categories/severities utilizing the PedsQL 4.0 Generic Core Scales. Health Qual Life Outcomes 2007;5:43–57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hilliard ME, Mann KA, Peugh JL, Hood KK. How poorer quality of life in adolescence predicts subsequent type 1 diabetes management and control. Patient Educ Couns 2013;91:120–125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hoey H, Aanstoot HJ, Chiarelli F, et al. . Good metabolic control is associated with better quality of life in 2,101 adolescents with type 1 diabetes. Diabetes Care 2001;24:1923–1928 [DOI] [PubMed] [Google Scholar]
- 10.Hood KK, Beavers DP, Yi-Frazier J, et al. . Psychosocial burden and glycemic control during the first 6 years of diabetes: results from the SEARCH for Diabetes in Youth study. J Adolesc Health 2014;55:498–504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Varni JW, Burwinkle TM, Jacobs JR, Gottschalk M, Kaufman F, Jones KL. The PedsQL in type 1 and type 2 diabetes: reliability and validity of the Pediatric Quality of Life Inventory Generic Core Scales and type 1 Diabetes Module. Diabetes Care 2003;26:631–637 [DOI] [PubMed] [Google Scholar]
- 12.de Wit M, Delemarre-van de Waal HA, Pouwer F, Gemke RJBJ, Snoek FJ. Monitoring health related quality of life in adolescents with diabetes: a review of measures. Arch Dis Child 2007;92:434–439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hilliard ME, Lawrence JM, Modi AC, et al.; SEARCH for Diabetes in Youth Study Group . Identification of minimal clinically important difference scores of the PedsQL in children, adolescents, and young adults with type 1 and type 2 diabetes. Diabetes Care 2013;36:1891–1897 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nansel TR, Weisberg-Benchell J, Wysocki T, Laffel L, Anderson B; Steering Committee of the Family Management of Diabetes Study . Quality of life in children with type 1 diabetes: a comparison of general and diabetes-specific measures and support for a unitary diabetes quality-of-life construct. Diabet Med 2008;25:1316–1323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lawrence JM, Yi-Frazier JP, Black MH, et al.; SEARCH for Diabetes in Youth Study Group . Demographic and clinical correlates of diabetes-related quality of life among youth with type 1 diabetes. J Pediatr 2012;161:201–207.e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Varni JW, Curtis BH, Abetz LN, Lasch KE, Piault EC, Zeytoonjian AA. Content validity of the PedsQL™ 3.2 Diabetes Module in newly diagnosed patients with type 1 diabetes mellitus ages 8-45. Qual Life Res 2013;22:2169–2181 [DOI] [PubMed] [Google Scholar]
- 17.Anderson BJ, Auslander WF, Jung KC, Miller JP, Santiago JV. Assessing family sharing of diabetes responsibilities. J Pediatr Psychol 1990;15:477–492 [DOI] [PubMed] [Google Scholar]
- 18.Hood KK, Butler DA, Anderson BJ, Laffel LMB. Updated and revised Diabetes Family Conflict Scale. Diabetes Care 2007;30:1764–1769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rewers M, Pihoker C, Donaghue K, Hanas R, Swift P, Klingensmith GJ. Assessment and monitoring of glycemic control in children and adolescents with diabetes. Pediatr Diabetes 2009;10(Suppl. 12):71–81 [DOI] [PubMed] [Google Scholar]
- 20.American Diabetes Association Standards of medical care in diabetes--2011. Diabetes Care 2011;34(Suppl. 1):S11–S61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Anderson BJ, Vangsness L, Connell A, Butler D, Goebel-Fabbri A, Laffel LMB. Family conflict, adherence, and glycaemic control in youth with short duration Type 1 diabetes. Diabet Med 2002;19:635–642 [DOI] [PubMed] [Google Scholar]
- 22.Grey M, Boland EA, Yu C, Sullivan-Bolyai S, Tamborlane WV. Personal and family factors associated with quality of life in adolescents with diabetes. Diabetes Care 1998;21:909–914 [DOI] [PubMed] [Google Scholar]
- 23.Wiebe DJ, Berg CA, Korbel C, et al. . Children’s appraisals of maternal involvement in coping with diabetes: enhancing our understanding of adherence, metabolic control, and quality of life across adolescence. J Pediatr Psychol 2005;30:167–178 [DOI] [PubMed] [Google Scholar]
- 24.Eiser C, Flynn M, Green E, et al. . Quality of life in young adults with type 1 diabetes in relation to demographic and disease variables. Diabet Med 1992;9:375–378 [DOI] [PubMed] [Google Scholar]
- 25.Austin JK, Huster GA, Dunn DW, Risinger MW. Adolescents with active or inactive epilepsy or asthma: a comparison of quality of life. Epilepsia 1996;37:1228–1238 [DOI] [PubMed] [Google Scholar]
- 26.Hunfeld JA, Perquin CW, Duivenvoorden HJ, et al. . Chronic pain and its impact on quality of life in adolescents and their families. J Pediatr Psychol 2001;26:145–153 [DOI] [PubMed] [Google Scholar]
- 27.Michel G, Bisegger C, Fuhr DC, Abel T; KIDSCREEN group . Age and gender differences in health-related quality of life of children and adolescents in Europe: a multilevel analysis. Qual Life Res 2009;18:1147–1157 [DOI] [PubMed] [Google Scholar]
- 28.Laffel LMB, Vangsness L, Connell A, Goebel-Fabbri A, Butler D, Anderson BJ. Impact of ambulatory, family-focused teamwork intervention on glycemic control in youth with type 1 diabetes. J Pediatr 2003;142:409–416 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.