Abstract
Objective
The objective of this report is to describe measles activity in Canada during 2013, in order to support the documentation and maintenance of measles elimination status.
Methods
A descriptive analysis of measles counts and incidence by age group, immunization history, hospitalization and province/territory, as well as a summary of 2013 outbreaks, was conducted using enhanced measles data captured through the Canadian Measles and Rubella Surveillance System. Genotype information and phylogenetic analysis for 2013 were summarized.
Results
In 2013, 83 confirmed measles cases were reported in seven provinces/territories for an incidence rate of 2.4 per 1,000,000 population. Incidence was highest in the youngest age groups (< 1 year, 1 to 4 years). Burden of disease was highest in the youngest age groups and children 10 to 14 years. Three-quarters of cases had been inadequately immunized, and 10% were hospitalized. There were nine measles outbreaks reported in 2013, one of which consisted of 42 cases in a non-immunizing community in Alberta.
Discussion
2013 saw the fifth highest number of reported measles cases since 1998. While we continue to face challenges related to importation and heterogeneous immunization coverage, in 2013 Canada met or partially met all four criteria outlined by the Pan American Health Organization for measles elimination.
Introduction
The last reported case of endemic measles in Canada occurred in November 1997; Canada’s elimination status was achieved one year later in 1998 (1). The World Health Organization (WHO) Region of the Americas achieved elimination status in 2002, making it the first and only WHO Region to reach this goal. Elimination of measles is maintained as long as a single measles viral strain is not circulating continuously throughout Canada for a period of 12 months or more (2). Endemic measles activity persists across the European, African, Southeast Asian and Western Pacific regions (3). While endemic transmission has not been re-established in Canada, the possibility of importation of measles into the country remains, as a result of population exchange with endemic countries or countries experiencing measles outbreaks.
Subsequent outbreaks within Canada following a measles importation are often limited; however, there were large outbreaks of 94, 53, 82 and 678 cases in 2007, 2008, 2010 and 2011 (4,5). Transmission within Canada is associated with those who are under-or unimmunized and areas with suboptimal immunization coverage. While 2-dose immunization coverage in Canada is generally high (the 2011-12 Childhood National Immunization Survey estimated 2-dose coverage by age 7 years to be 94.9% [6]), it is not uniform across the country, within provinces and territories, or across sub-populations (e.g. religious communities that oppose vaccination). Given the lack of uniformity in coverage to achieve the ≥ 95% coverage recommended for measles herd immunity (6), the risk of domestic transmission following an importation of measles remains a reality.
As an ongoing component of Canada’s commitment to the maintenance and documentation of measles elimination status, the Public Health Agency of Canada (the Agency) conducts enhanced measles surveillance. The post-elimination Canadian measles epidemiology has been previously reported for 1998-2001 (1) and 2002 to 2011 (4). There were only 10 confirmed measles cases reported in Canada in 2012, the majority (n = 6, 60.0%) of them importations without secondary spread. Information on these cases is available elsewhere (7). The objective of this report, therefore, is to describe measles activity in Canada during 2013, in order to support the documentation and maintenance of measles elimination status.
Methods
Surveillance dataset
Enhanced measles surveillance is carried out in all provinces and territories through the Canadian Measles and Rubella Surveillance System. On a weekly reporting cycle, provinces and territories report cases of measles meeting the national case definition (8) to the Agency, including zero reporting, through a national case report form that is submitted by e-mail or fax. Three jurisdictions (British Columbia, Alberta, and Newfoundland and Labrador) are currently participating in the Measles and Rubella Surveillance pilot project, which provides real-time laboratory and epidemiological web-based reporting of suspect measles/rubella case investigations. Case details obtained from the national surveillance system case report forms and Measles and Rubella Surveillance web-based notifications were assessed against the national measles confirmed-case definition (laboratory confirmed or epidemiological link to a laboratory-confirmed case) before inclusion in the national database.
The objective of national measles surveillance is to continuously monitor the presence of measles virus in Canada in a timely way. To meet this objective, the Canadian Measles and Rubella Surveillance System captures cases that were communicable in Canada, regardless of country of residence. This allows accurate international and national reporting of the presence of measles virus in Canada, which is an essential criterion for measles elimination. However, this might result in case count discrepancies between federal and provincial/territorial surveillance systems, since some provincial/territorial systems do not include measles cases among foreign nationals.
This report includes enhanced data of confirmed measles cases, reported by the provinces and territories through both the national surveillance system and the surveillance pilot project, with rash onset during epidemiological weeks 1 to 52 for the 2013 reporting year (i.e. from December 30, 2012, to December 28, 2013). Probable cases (8) are not nationally notifiable and therefore are not included in this report.
Case report form
The Canadian Measles and Rubella Surveillance System case report form is one page in length and designed to meet the objectives of national surveillance. The form facilitates collection of information on case identifiers (date of birth or age, gender, health unit, city, forward sortation area, date reported to health unit and date investigation was started); background, exposure and clinical information (date of rash onset, hospitalization, source of exposure, vaccination history [date of each dose] and whether the case was outbreak associated); and laboratory information (results of laboratory tests).
The data manager followed up with the reporting jurisdiction if information was missing on the form. At data entry, values coded as missing represented those that were blank on the form, and values coded as unknown represented those sought, but not available, from the reporting jurisdiction. A data validation process was conducted with provinces and territories in March 2014 for all measles cases reported nationally in 2013.
Genotyping
Measles virus genotyping was performed at the Public Health Agency of Canada’s National Microbiology Laboratory. Appropriate clinical specimens (respiratory specimens and/or urines) collected from suspect or confirmed measles cases were submitted by provincial laboratories. The WHO’s standardized genotyping regions of the 450 nucleotides encoding the carboxyl-terminus of the measles nucleoprotein, the N-450, and the full length hemagglutinin gene (H gene) (9) were amplified and sequenced from extracted nucleic acid. The sequences were aligned with WHO genotype reference sequences (10), and phylogenetic trees were generated using MEGA5 software (11).
Data management and statistical analysis
Data management was conducted with Microsoft Access 2010. Descriptive epidemiological analyses were conducted with SAS Enterprise Guide 5.1 (12). Distribution of confirmed measles cases by province and territory, age group, sex, immunization history and hospitalization were described. Case counts and proportions were calculated for categorical variables, and means/medians and ranges were calculated for continuous variables. Cases with missing or unknown responses were included in the denominators for proportions.
Incidence rates were generated using population estimates from Statistics Canada for 2013 (13). Rates were calculated per 1,000,000 population for consistency with the PAHO recommended indicator (2).
The National Advisory Committee on Immunization’s recommendations for measles immunization was used to determine whether cases’ immunization status was up to date for age with measles-containing vaccine (14). Children aged < 1 year and adults born before 1970 were considered up to date for age with 0 or more doses of measles-containing vaccine. Cases aged 1 to 6 years were considered up to date for age with one or more doses of measles-containing vaccine and those aged 7 years and older (but born in 1970 or later) were up to date with two or more doses.
Essential criteria for measles elimination
In order to continue documentation and verification of measles elimination in the Region of the Americas, the Pan-American Health Organization (PAHO) has developed four criteria that it considers essential for each Member State to meet (2):
Verify the interruption of endemic measles cases for a period of at least three years from the last known endemic case, in the presence of high-quality surveillance;
Implement and maintain high-quality surveillance sensitive enough to detect imported and import-related cases;
Verify the absence of endemic measles virus strains through viral surveillance; and
Verify adequate immunization in the population.
Canada’s performance towards maintenance of measles elimination was assessed against the four elimination criteria on the basis of the 2013 Canadian surveillance data.
This study was exempt from research ethics board approval because the data set was the result of public health surveillance.
Results
Overview
In 2013, a total of 83 confirmed measles cases were reported, for an overall incidence rate of 2.4 cases per 1,000,000 population. Of these cases, 53 (63.9%) were laboratory confirmed and 30 (36.1%) were epidemiologically linked to a laboratory-confirmed case.
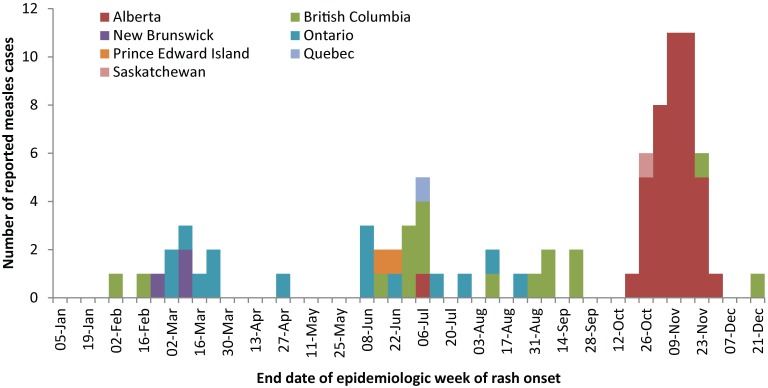
Measles cases were reported in seven provinces and territories over 28 weeks in 2013. The maximum number of cases that occurred per week was 11, in weeks 45 and 46. These were outbreak-associated cases that occurred during the peak of a large outbreak in Alberta (Figure 1).
Figure 1. Number of reported measles cases by epidemiological week of rash onset and reporting province or territory, Canada, 2013.
Age, gender and geographic distribution
The majority of measles cases reported were male (n = 45, 54.2%). Children aged 1 to 4 years and 10 to 14 years each represented the highest proportion of cases (n = 17 and 20.5% each), followed by 15 to 19 and 20 to 24 year olds (n = 11 and 13.3% each). Of the four cases aged 40 years and older, three were born before 1970, the birth year cut-off for presumed natural immunity (14).
While the burden of disease extended from those aged 1 to 24 years, the incidence rate was highest among the youngest age groups (10.5 per 1,000,000 for those < 1 year; 11.0 per 1,000,000 for those 1 to 4 years) (Table 1).
Table 1. Confirmed measles cases and incidence rates (per 1,000,000 population) by age group, gender and reporting province or territory, Canada, 2013.
| Age group (years) | M | F | CA | BC | AB | SK | MB | ON | QC | NB | NS | PE | NL | YT | NT | N U | Overall inciden ce rate |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| < 1 | 4 | 0 | 4 | 2 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 10.5 |
| 1 to 4 | 12 | 5 | 17 | 1 | 6 | 0 | 0 | 7 | 1 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 11.0 |
| 5 to 9 | 6 | 3 | 9 | 0 | 7 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 4.8 |
| 10 to 14 | 6 | 11 | 17 | 1 | 15 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 9.1 |
| 15 to 19 | 5 | 6 | 11 | 0 | 9 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 5.0 |
| 20 to 24 | 4 | 7 | 11 | 5 | 5 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 4.5 |
| 25 to 29 | 2 | 2 | 4 | 3 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1.7 |
| 30 to 39 | 6 | 0 | 6 | 3 | 0 | 0 | 0 | 2 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1.3 |
| 40 to 59 | 0 | 4 | 4 | 2 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.4 |
| ≥60 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| TOTAL | 45 | 38 | 83 | 17 | 43 | 1 | 0 | 16* | 1 | 3 | 0 | 2 | 0 | 0 | 0 | 0 | 2.4 |
| Inciden ce rate | 2.6 | 2.1 | 2.4 | 3.7 | 10.7 | 0.9 | 0 | 1.2 | 0.1 | 4.0 | 0 | 13.8 | 0 | 0 | 0 | 0 | 2.6 |
M: male; F: female; CA: Canada *One Ontario case was a traveller from the Netherlands and is not included in Ontario’s provincial measles case counts of 15 for 2013.
Cases were reported in 7 of the 13 Canadian provinces and territories: Alberta (n = 43), British Columbia (n = 17), Ontario (n = 16), New Brunswick (n = 3), Prince Edward Island (n = 2), Quebec (n = 1) and Saskatchewan (n = 1). The incidence rate was highest in Prince Edward Island, given its small population, followed by Alberta, with 13.8 and 10.7 cases per 1,000,000 population respectively. The incidence for the each of the remaining provinces was less than 5.0 cases per 1,000,000 population (Table 1).
Immunization history
Of the 83 cases reported in 2013, 13.3% (n = 11) had an immunization status considered up to date for age (Table 2). These included four infants < 1 year who were too young to receive their first dose of measles-containing vaccine and one adult born before 1970. Conversely, 75.9% (n = 63) were not up to date for age at the time of infection and immunization status was unknown for 10.8% (n = 9); two of these were born before 1970 and are presumed to be immune regardless of immunization history.
Table2. Immunization status of confirmed measles cases by age group, Canada, 2013.
| Age group (years) | TOTAL | 0 doses | Up To Date with | One dose | Up To Date with | Two doses | Unknown |
|---|---|---|---|---|---|---|---|
| 0 doses | 1 dose | ||||||
| < 1 | 4 | 4 | 4 | 0 | - | 0 | 0 |
| 1 to 4 | 17 | 14 | 0 | 2 | 2 | 1 | 0 |
| 5 to 9 | 9 | 9 | 0 | 0 | - | 0 | 0 |
| 10 to 14 | 17 | 17 | 0 | 0 | - | 0 | 0 |
| 15 to 19 | 11 | 10 | 0 | 0 | - | 1 | 0 |
| 20 to 24 | 11 | 7 | 0 | 0 | - | 2 | 2 |
| 25 to 29 | 4 | 3 | 0 | 1 | 0 | 0 | 0 |
| 30 to 39 | 6 | 1 | 0 | 0 | - | 0 | 5 |
| 40 to 59 | 4 | 2 | 1 | 0 | - | 0 | 2 |
| ≥60 | 0 | 0 | - | 0 | - | 0 | 0 |
| Unknown | 0 | 0 | - | 0 | - | 0 | 0 |
| TOTAL | 83 | 67 | 5 | 3 | 2 | 4 | 9 |
Mirroring the age group distribution of the cases, inadequate immunization status was most commonly reported in the 10 to 14 and 1 to 4 year age groups (27.0% and 22.2% respectively), followed by the 5 to 9 and 15 to 19 year olds (14.3 and 15.9% respectively).
Hospitalization
Of the 83 reported cases, 9.6% (n = 8) were hospitalized (Table 3). Half of the infants < 1 year and 30% of cases among adults 25 to 39 years were hospitalized. Hospitalization was infrequent among cases 1 to 24 years of age.
Table 3. Hospitalization status of confirmed measles cases by age group, Canada, 2013.
| Age group (years) | TOTAL | Not hospitalized, no. (%) | Hospitalized no. (%) | Unknown no. (%) |
|---|---|---|---|---|
| < 1 | 4 | 2 (50.0) | 2 (50.0) | 0 (-) |
| 1 to 4 | 17 | 14 (82.4) | 2 (11.8) | 1 (5.9) |
| 5 to 9 | 9 | 9 (100.0) | 0 (-) | 0 (-) |
| 10 to 14 | 17 | 17 (100.0) | 0 (-) | 0 (-) |
| 15 to 19 | 11 | 10 (90.9) | 1 (9.1) | 0 (-) |
| 20 to 24 | 11 | 11 (100.0) | 0 (-) | 0 (-) |
| 25 to 29 | 4 | 3 (75.0) | 1 (25.0) | 0 (-) |
| 30 to 39 | 6 | 4 (66.7) | 2 (33.3) | 0 (-) |
| 40 to 59 | 4 | 4 (100.0) | 0 (-) | 0 (-) |
| ≥60 | 0 | 0 (-) | 0 (-) | 0 (-) |
| Unknown | 0 | 0 (-) | 0 (-) | 0 (-) |
| TOTAL | 83 | 74 (89.2) | 8 (9.6) | 1 (1.2) |
Molecular epidemiology
During 2013, specimens were available to determine the genotype for 50 of 83 (60.2%) reported cases of measles. Measles genotypes were D8 (n = 34), B3 (n = 13), H1 (n = 2) and D4 (n = 1).
Measles genotype D8 was detected in 34 cases and seven outbreaks (Table 4). In general, this genotype has been associated with endemic transmission in the Eastern Mediterranean region, primarily in the Southeast Asian region (15). The genotype D8 sequences identified could be further subdivided as four sequence variants (Figure 2): those that were identical to MVs/Taunton.GBR/27.12 (GenBank accession number JX984461) (n = 18), MVs/Frankfurt Main.DEU/17.11 (GenBank accession number KF683445) (n = 10), MVs/Swansea.GBR/4.13 (GenBank accession number KF214761) (n = 4) and MVi/Villupuram.Ind/03.07 (GenBank accession number FJ765078) (n = 2). The two cases that had sequences identical to MVi/Villupuram.Ind/03.07 were part of an outbreak that began as a result of an importation from Thailand (Table 4), where the sequence was circulating (GenBank accession numbers KC631635, KC631637-41). Measles sequences identical to MVs/Swansea.GBR/4.13 were detected in four cases, of which the two primary cases (MVs/New Brunswick.CAN/7.13 and MVs/Ontario.CAN/8.13, Figure 2) had returned from Mexico (Table 4). At the time, this sequence variant had been reported to the WHO measles sequence database, MeaNS (15), only from the UK (Kevin Brown, Public Health, England: personal communication, March 7, 2013), supporting the identification of a UK tourist as the index case.
Table 4. Summary of the nine measles outbreaks reported in Canada, 2013.
| # | Prov. | No. of cases |
Onset date range (duration in days; number of generations) |
Strain and sequence designation | Description |
|---|---|---|---|---|---|
| 1 | BC | 2 | January 31 to February 12 (13; 2 generations) |
D8 |
|
| 2 | NB and ON | 4 | February 19 to March 4 (14; 2 generations) |
D8 |
|
| 3 | ON | 5 | February 24 to March 21 (26; 3 generations) |
B3 |
|
| 4 | ON | 6 | June 8 to July 24 (47; 4 generations) |
D8 |
|
| 5 | PE | 2 | June 10 to June 22 (13; 2 generations) |
D8 |
|
| 6 | BC | 3 | June 10 to June 26 (17; 2 generations) |
D8 |
|
| 7 | BC | 4 | June 24 to July 6 (13; 2 generations) |
D8 |
|
| 8 | BC | 3 | September 2 to September 16 (15; 2 generations) |
B3 |
|
| 9 | AB | 42 | October 16 to November 25 (41; 4 generations) |
D8 |
|
MMR: measles mumps rubella vaccine.
Figure 2. Phylogenetic tree of measles N-450 sequences detected in Canada in 2013 (n = 50).
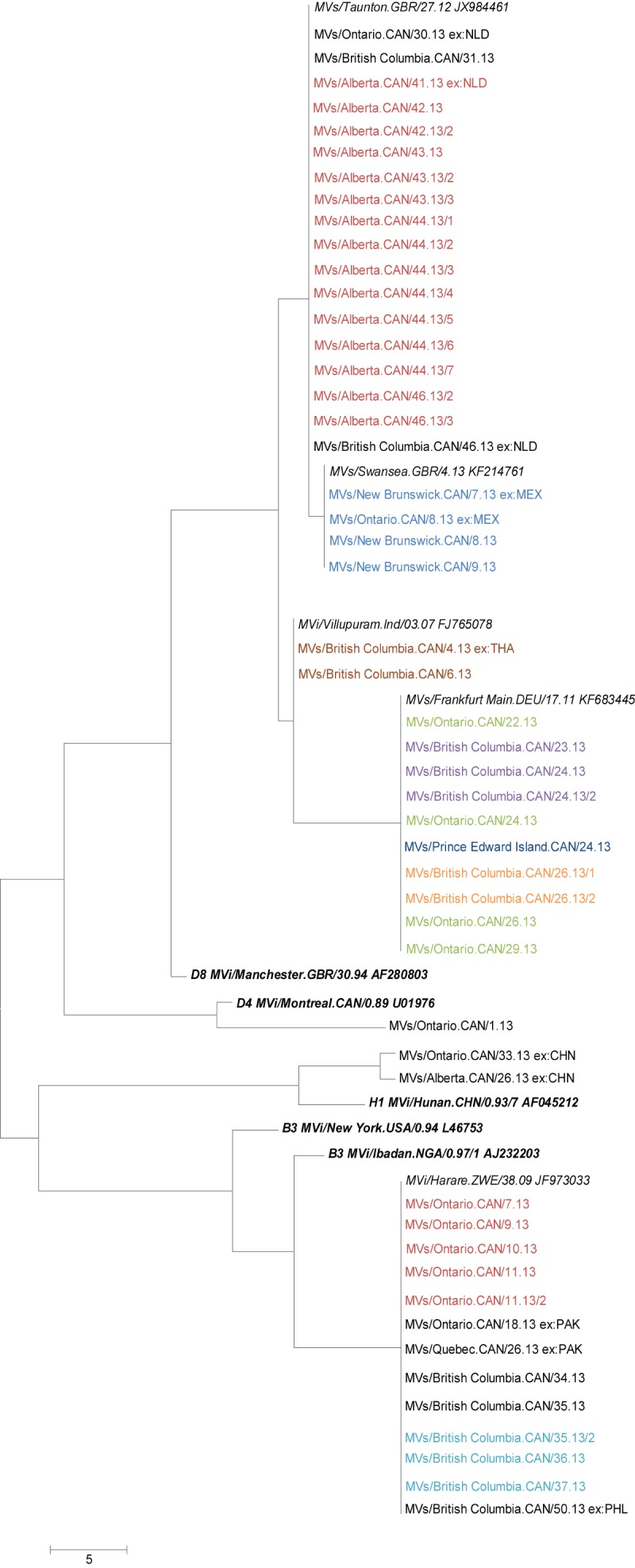
Each entry represents a sequence from an individual measles case. Phylogenetic trees demonstrate the relatedness of genetic sequences. Sequences on the same vertical line are identical. The length of horizontal lines separating sequences or branches of sequences is proportional to the number of differences (measured in single nucleotides) between the sequences (scale shown at the bottom left). WHO reference sequences (10) are shown in bold, italic font. Relevant sequence variants are shown in italics. These are identified within the WHO measles sequence database, MeaNS (accessible at http://www.who-measles.org/Public/Web_Front/sequence.php), and represent prevalent sequences within the database (10) Canadian sequences are shown in regular font and are identified by their WHO name, which indicates province and week of rash onset or specimen collection. Cases of imported virus are identified with “ex:< 3 letter country code>.” Outbreaks are represented by colour fonts: sequences with the same colour, within the same genotype, are from the same outbreak.
In the months of June and July, four outbreaks occurred simultaneously in three provinces: Ontario, Prince Edward Island and British Columbia (n = 2), and sequences identical to MVs/Frankfurt Main.DEU/17.11 was identified from all four outbreaks (Figure 2). At the time of the outbreaks, the MVs/Frankfurt Main.DEU/17.11 sequence variant was circulating in the European region (GenBank accession numbers KF269094, KJ690815, KF290740, KF715463, KF269089) and detected in the United States (GenBank accession number KF385861). Sequencing of the secondary WHO genotyping region, the H gene, did not differentiate the four outbreaks (Figure 3).
Figure 3.
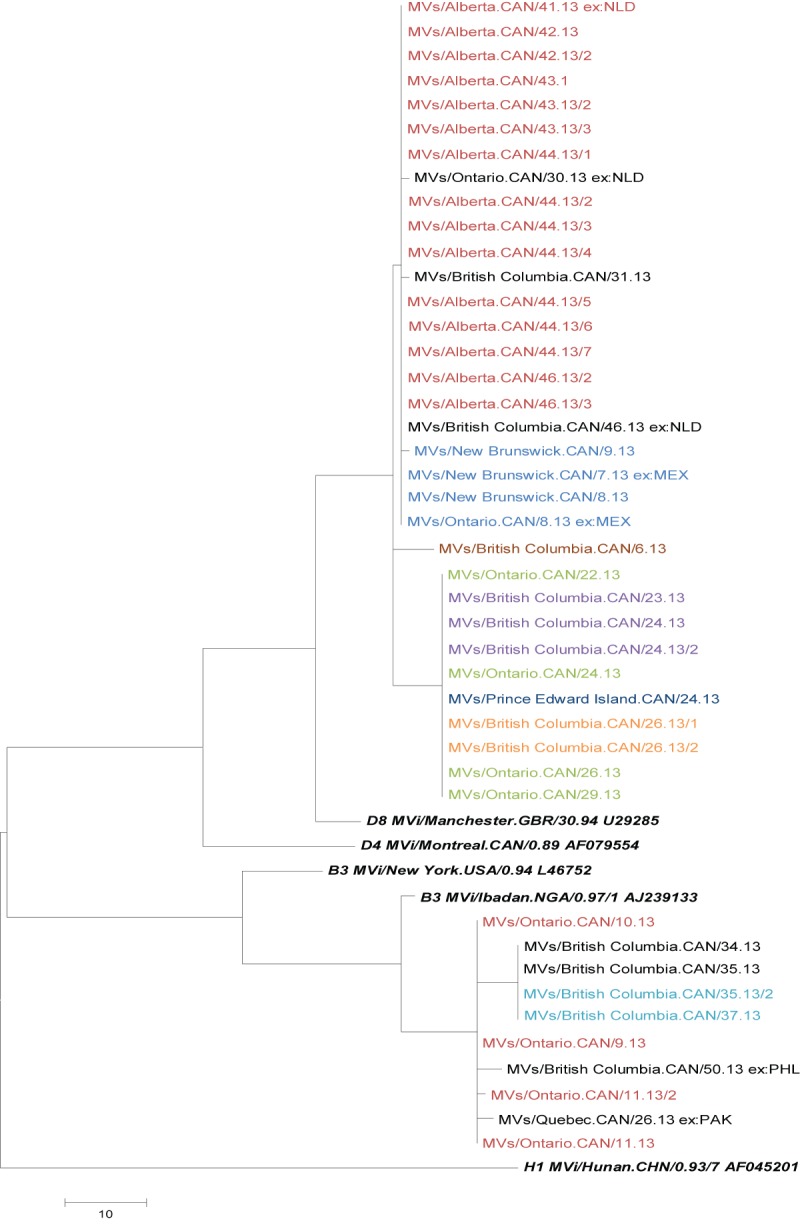
Phylogenetic tree of measles H gene sequences detected in Canada in 2013 (n = 43)
WHO reference sequences (10) are shown in bold, italic font. Canadian sequences are shown in regular font and are identified by their WHO name, which indicates province and week of rash onset or specimen collection. Cases of imported virus are identified with “ex:< 3 letter country code>.” Outbreaks are represented by colour fonts: sequences with the same colour, within the same genotype, are from the same outbreak.
The majority of the D8 sequences in 2013 were identical to the MVs/Taunton.GBR/27.12 sequence variant (n = 18), and all 18 were linked to the Netherlands (Figure 2), where the same sequence variant was associated with an ongoing outbreak (Susan Hahné, RIVM -Centre for Infectious Disease Control, the Netherlands: personal communication, June 12, 2013). Fifteen were associated with the Alberta outbreak, and the remaining three were unrelated importations. Two of the separate importations had distinct H gene sequences (MVs/Ontario.CAN/30.13 and MVs/British Columbia.CAN/31.13, Figure 3).
Measles genotype B3 was detected in 13 cases and was associated with two outbreaks whose origin could not be determined (Table 4, Figure 2). Genotype B3 has been associated with endemic transmission throughout the African region as well as a number of countries in the Eastern Mediterranean region (15). All Canadian B3 viruses sequenced were identical to the MVi/Harare.ZWE/38.09 sequence variant (GenBank accession number JF973033). At the time of the first outbreak in Ontario, this sequence variant was circulating in the Eastern Mediterranean region (GenBank accession numbers KC737549 and KF145165). Two sporadic cases were imported from Pakistan between outbreaks. At the time of the fourth outbreak in British Columbia, in the fall of 2013, this sequence variant was being reported from the Western Pacific and European regions in addition to the Eastern Mediterranean region (GenBank accession numbers KJ690812-4, KF468720, AB854746-7 and KF740427). At the end of the year, this sequence variant was also imported from the Philippines. Although all genotype B3 cases were identical at the primary genotyping region, the N-450 (Figure 2), the outbreaks and sporadic cases were distinguished by H gene sequencing (Figure 3).
Genotypes H1 (n = 2) and D4 (n = 1) were detected in three sporadic cases in 2013 (Figure 2). Genotype H1 was twice imported from the Western Pacific region, where it is endemic (15). Genotype D4 has been associated with endemic transmission in the Eastern Mediterranean, Southeast Asian and European regions (15). The source of the D4 case was unknown, although it was identical to a sequence variant circulating in the European region, MVs/Manchester.GBR/10.09 (GenBank accession numbers GQ370461, KC709569 and KF831037).
Summary of 2013 Canadian measles outbreaks
Nationally, an outbreak is defined as two or more cases of measles linked by person, place and time (16). In 2013, there were nine outbreaks composed of 71 cases. Of the remaining 12 non-outbreak-associated cases, seven were importations, and there was insufficient information to associate five cases with an existing outbreak.
Key characteristics of the reported outbreaks are included in Table 4. Outbreaks are presented in chronological order of rash onset of the index case. When the nature of the epidemiological links between outbreak-associated cases was not clearly described on the national case report form, this is specified in the table.
More than half (n = 42) of the outbreak-associated cases in 2013 was the result of a large outbreak in Alberta from October 16 to November 25 (duration: 40 days). This outbreak occurred in a non-immunizing community as a result of an importation from the Netherlands. The majority of the cases were male, median age was 13 years, and all cases were unimmunized. Additional details regarding this outbreak are provided elsewhere (17).
The following outbreak summary excludes the Alberta outbreak cases so as to not skew the results. The median number of cases per outbreak was 3.5 (the mean was similar at 3.6). The median duration from onset dates of the index case and last outbreak-associated cases was 14.5 days (or one incubation period from infection to rash onset) (18). The majority of the outbreaks (75.0%, n = 6) were limited to two generations of spread (median: 2). While outbreaks 3 and 4 (Ontario) were more extensive temporally, they were restricted to only five and six cases respectively. The origin of three outbreaks could not be determined.
Canadian measles in the global context
Of the 83 reported cases in 2013, 14.5% (n = 12) were classified as imported and 54.2% (n = 45) were epidemiologically linked to an imported case. Source of exposure could not be identified for 8.4% (n = 7), and 22.9% (n = 19) were epidemiologically linked to a case whose source of exposure was unknown.
The suspected country of exposure was identified for all importations. The 12 importations were acquired from the European Region (Austria/Italy/France [n = 1] and the Netherlands [n = 3]), the Western Pacific Region (China [n = 1], the Philippines [n = 1], and Taiwan [n = 1]), the Eastern Mediterranean Region (Pakistan [n = 2]), the Southeast Asian Region (Thailand [n = 1]) and the Region of the Americas (Mexico [n = 2]).
All importations were the result of a Canadian travelling to a measles-endemic country or being exposed to other travellers from measles-endemic countries (e.g. exposure to UK resident in Mexico). One importation was the result of a foreign national traveling to Canada while the infection was communicable.
Maintenance of measles elimination
PAHO’s four essential criteria for measles elimination are listed in Table 5 with a description of the indicator used to measure them and a summary of how the measles surveillance data support Canada’s ongoing efforts to sustain its elimination status.
Table 5. Pan American Health Organization essential criteria for the elimination of measles.
| Criterion (16) | Indicator | Description |
|---|---|---|
| Verify the interruption of endemic measles cases for a period of at least 3 years from the last known endemic case, in the presence of high-quality surveillance | Zero cases of endemic transmission |
Criterion met Documentation and verification of interruption of endemic measles in Canada from 1998 to 2011 are provided elsewhere (1,4). Molecular and epidemiological surveillance will continue through 2014 to ensure that there is no persistent circulation of the viral strains identified in 2013 for a period equal to or greater than 12 months. |
| Implement and maintain high-quality surveillance sensitive enough to detect imported and import-related cases | > 2 suspect cases per 100,000 population adequately investigated |
Criterion partially met Data to support this indicator not available nationally. However, a national estimate was determined from the Measles and Rubella Surveillance pilot project data for the 2011 reporting year. The national measles-like illness investigation rate was 19 per 100,000 population. Note: this indicator was estimated during an outbreak year (Quebec 2011). Comparatively, the national estimate during the 2006 non-outbreak year was 12 per 100,000 population. |
| Verify the absence of endemic measles virus strains through viral surveillance | Measles genotype assessed in 80% of outbreaks |
Criterion met The measles genotype was identified in 100% of the outbreaks in 2013. |
| Verify adequate immunization in the population | 95% of population cohorts aged 1 to 40 years have received a measles-containing vaccine |
Criterion partially met Data to support this indicator not available nationally for all age groups. The most recent national immunization coverage survey estimated first dose measles-containing vaccine coverage among 2 year olds to be 95.2% and second dose measles-containing vaccine coverage among 7 year olds to be 94.9% in 2011 (19). However, according to epidemiological investigation of recent outbreaks and communication with provinces and territories we know that immunization coverage is heterogeneous across Canada, and there are areas with lower (and higher) coverage. |
Discussion
This report summarizes the epidemiology of measles in Canada in 2013. Although measles has been eliminated in Canada, we continue to see cases of disease. While the 83 reported cases in 2013 represent the fifth highest number annually since 1998, eight of the nine outbreaks were highly restricted in their case distribution by either person or time (i.e. small number of cases or short outbreak duration). These findings suggest a possible combination of prompt and effective public health intervention and/or high immunization coverage among contacts. However, the large outbreak in the non-immunizing community in Alberta highlights the ongoing challenges in maintaining measles elimination in a country with heterogeneous immunization coverage.
In 2013, Canada had a number of importations, all from countries with endemic measles or outbreaks. All but one of these importations were by Canadians who acquired the disease while travelling abroad (the other was a foreign resident who travelled to Canada while communicable), emphasizing the continued importance of ensuring that all Canadians are adequately immunized, particularly before travelling.
Four measles genotypes were observed in 2013, D8 being the most prevalent and geographically represented (five provinces reported cases associated with this genotype).
Canada met or partially met all four criteria for measles elimination in 2013. Epidemiological and molecular measles surveillance was able to confirm the absence of circulation of any one dominant viral strain, although ongoing surveillance is required to ensure that this is sustained. While suspect case investigations are not captured at the national level, the proxy indicator measured through the Measles and Rubella Surveillance pilot project indicates an investigation rate in excess of the minimum required. Finally, despite national coverage estimates of 95%, pockets of people and groups within the population remain susceptible.
Limitations
Outcome information (e.g. duration of hospitalization, complications or death) on measles cases is not captured through national surveillance. Therefore, characterization of measles cases by severity of disease is not possible. Immunization status was unknown for 11% of cases, which limits our ability to fully understand the distribution of disease by immunization history.
The ability to collect detailed immunization histories of cases may be a challenge at the local level, where information is primarily gathered and submitted to provincial and then federal authorities for surveillance purposes. Improving the collection of immunization history in case reports should be explored.
Acknowledgements
We gratefully acknowledge the contribution of our provincial and territorial measles partners for providing data to the Canadian Measles and Rubella Surveillance System, for their input towards the format of this report and for their content review.
Footnotes
Conflicts of interest: There are no conflicts of interest to declare.
Funding: This work was supported by the Public Health Agency of Canada.
References
- 1.King A, Varughese P, De Serres G, Tipples GA, Waters J; Working Group on Measles Elimination. Measles elimination in Canada. J Infect Dis 2004. May;189 Suppl 1:S236–42. 10.1086/378499 [DOI] [PubMed] [Google Scholar]
- 2.Pan-American Health Organization (PAHO). Plan of Action: Documentation and verification of measles, rubella and congenital rubella syndrome elimination in the region of the Americas. Technical document. 2010.
- 3.World Health Organization. Global measles and rubella strategic plan 2012-2020. http://www.refworks.com/refworks2/default.aspx?r=references|MainLayout:init
- 4.Public Health Agency of Canada. Elimination of measles, rubella and congenital rubella syndrome in Canada: Documentation and verification report. 2011.
- 5.De Serres G, Markowski F, Toth E, Landry M, Auger D, Mercier M et al. Largest measles epidemic in North America in a decade--Quebec, Canada, 2011: contribution of susceptibility, serendipity, and superspreading events. J Infect Dis 2013. Mar;207(6):990–8. 10.1093/infdis/jis923 [DOI] [PubMed] [Google Scholar]
- 6.van Boven M, Kretzschmar M, Wallinga J, O’Neill PD, Wichmann O, Hahné S. Estimation of measles vaccine efficacy and critical vaccination coverage in a highly vaccinated population. J R Soc Interface 2010. Nov;7(52):1537–44. 10.1098/rsif.2010.0086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Public Health Agency of Canada. Counts of reported cases of measles over time in Canada, both sexes, all ages, from 1924 to 2012. http://dsol-smed.phac-aspc.gc.ca/dsol-smed/ndis/charts.php?c=pl
- 8.Public Health Agency of Canada. Case definitions for diseases under national surveillance. CCDR. 2009. [Google Scholar]
- 9.World Health Organization. Expanded Programme on Immunization (EPI). Standardization of the nomenclature for describing the genetic characteristics of wild-type measles viruses. Wkly Epidemiol Rec 1998. Aug;73(35):265–9. [PubMed] [Google Scholar]
- 10.World Health Organization. Measles virus nomenclature update: 2012. Wkly Epidemiol Rec 2012. Mar;87(9):73–81.22462199 [Google Scholar]
- 11.Tamura K, Peterson D, Peterson N, Stecher G, Nei M, Kumar S. MEGA5: molecular evolutionary genetics analysis using maximum likelihood, evolutionary distance, and maximum parsimony methods. Mol Biol Evol 2011. Oct;28(10):2731–9. 10.1093/molbev/msr121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.SAS. Enterprise guide 5.1. 2013;5.1.
- 13.Statistics Canada, demography division, demographic estimates section, July population estimates, 2013 final intercensal estimate.
- 14.National Advisory Committee on Immunization (NACI). Statement on measles-mumps-rubella-varicella vaccine. 2010. [DOI] [PMC free article] [PubMed]
- 15.Rota PA, Brown K, Mankertz A, Santibanez S, Shulga S, Muller CP et al. Global distribution of measles genotypes and measles molecular epidemiology. J Infect Dis 2011. Jul;204 Suppl 1:S514–23. 10.1093/infdis/jir118 [DOI] [PubMed] [Google Scholar]
- 16.Public Health Agency of Canada. Guidelines for the prevention and control of measles outbreaks in Canada. Can Commun Dis Rep 2013;39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kershaw T, Suttorp V, Simmonds K, St. Jean T. Outbreak of measles in a non-immunizing population, Alberta, october-november, 2013. Can Commun Dis Rep 2014;40(12):219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Heymann D, editor. Control of communicable diseases manual. 19th ed. Washington, DC: American Public Health Association; 2008. [Google Scholar]
- 19.Public Health Agency of Canada. Immunizaiton coverage in Canada (2002-2012). http://www.phac- aspc.gc.ca/im/nics-enva/icc-cvc-eng.php