Abstract
Objectives
To assess the characteristics of tetanus in previously immunized individuals.
Methods
A systematic literature search was undertaken using Ovid MEDLINE(R) and EMBASE databases for articles published between 1946 and September 3, 2013. The search strategy was developed using MESH terms for “tetanus”, “immunization” and “vaccination”. Inclusion criteria were articles in English or French that described at least one case of tetanus, immunization history and/or the results of anti-tetanus antibodies. Articles were reviewed for relevant references.
Results
51 unique articles published from1946-2013 were included in the review. The articles described 359 cases of clinical tetanus in individuals with prior receipt of one or more doses of tetanus toxoid vaccine and/or levels of tetanus antibody titres generally considered protective. Of the 210 cases that reported patient status at discharge, 180 (85.7%) survived with only three cases reporting residual deficits.
Conclusion
Tetanus spores are ubiquitous and this report clearly documents that tetanus cases can occur in individuals previously immunized with tetanus toxoid vaccine. Clinicians should not rule out tetanus when clinical symptoms suggest it, regardless of the vaccination history. When treated, the prognosis for tetanus is good. Further research is needed to assess the incidence of tetanus in partially- and fully-immunized populations and determine whether this is due to waning immunity of vaccine failure.
Introduction
A previously healthy 22 year-old man presented to an emergency department in Ontario, Canada with symptoms of spasm and trismus consistent with tetanus. Twenty-seven days prior to presentation, he reported a minor injury to the left great toe that appeared to form an abscess. He lanced the abscess himself, but the wound worsened whereupon he sought medical treatment. Medical treatment consisted of antibiotics followed by systemic steroids for a suspected allergic reaction to the antibiotics. Past medical history revealed five documented and appropriately spaced doses of tetanus toxoid-containing vaccine: Diphtheria, tetanus, pertussis (DTP) at 2, 4 and 6 months, Diphtheria, tetanus, acellular pertussis, inactivated polio (DTaP-IPV) at 18 months and Tetanus, diphtheria (reduced), acellular pertussis (reduced) (Tdap) at 14 years of age, nine years previously. There was no documentation of a pre-school booster typically given at 4-6 years. No additional tetanus-containing vaccine was given when he initially sought medical treatment. At the hospital, the patient was treated with tetanus immune globulin, antibiotics and supportive care. During his course in hospital, the patient improved and was discharged 20 days after admission, with a full recovery reported 12 weeks following initial presentation.
Tetanus is the clinical manifestation of infection with Clostridium tetani (1). The exotoxin produced by tetanus bacilli acts on the spinal cord and causes painful muscular contractions, especially of the neck and masseter muscles, thus the colloquial name “lockjaw” (2). More severe symptoms include respiratory problems, coma and death (2). Tetanus spores are ubiquitous in the environment and can infect any exposed wound (1). Prevention of tetanus is achieved through appropriate wound care and immunization (1).
Tetanus is rare in Canada with an average of four cases per year (range 1-10 per year) between 1990 and 2010 (3). Since the 1920s there has been a significant decrease in the number of deaths from tetanus due to the availability of vaccine and improvements in critical care (1,2). The case fatality rate due to tetanus in unvaccinated persons varies significantly from 10% to over 80% with the very young and elderly being at greatest risk (1,3,4).
In Canada, the routine immunization schedule consists of four doses of tetanus toxoid-containing vaccine, given at 2, 4, 6 and 12 to 23 months of age (typically at 18 months of age), with a booster dose at age 4-6 years (3). After the completion of the first three doses of tetanus toxoid, more than 99% of individuals will have evidence of a protective antibody titre (3). Although traditionally a tetanus antibody titre of >0. 01 IU/mL by mouse neutralization assay has been considered protective; some studies have suggested a higher correlate of protection, such as 0.1 IU/mL. is required (5-7). Observational studies have demonstrated the efficacy of pre- and post-wound exposure immunization regimens (3). Subsequent booster doses are recommended at 10-year intervals, although the most recent edition of the Canadian Immunization Guide indicates that new evidence on the optimal timing of booster doses is currently under review (3). Depending on the nature of the wound and prior immunization history, post-exposure immunization (active and passive) may also be indicated (3).
Nevertheless, tetanus may still occur post immunization. Given the above case of tetanus with a history of a complete and documented primary series of tetanus toxoid, along with a “booster” nine years prior to presentation, a systematic review was conducted to assess the characteristics of tetanus in previously immunized individuals.
Methods
A systematic literature search was undertaken using Ovid MEDLINE(R) and EMBASE databases for articles published between 1946 and September 3, 2013. The search strategy was developed in MEDLINE using the following MESH terms: tetanus/, tetanus toxoid/, diagnosis/, diagnosis, differential/, immunization/, vaccination/. The controlled vocabulary was supplemented by the use of related keywords to increase the specificity of the search: “fully”, “preexisting”, “previous* “, “prior”, “presen*”, “protective”, “active”, “antibodies”, immune*”, “vaccine*”. The search terms were combined using Boolean operators. No limits were applied to search in MEDLINE. The search in EMBASE, after the controlled vocabulary was translated to Emtree terms, was limited to non-MEDLINE content.
Abstracts were screened for the article being written in either English or French and a diagnosis of tetanus in one or more individuals. Abstracts meeting both screening criteria were obtained for full text review. Two authors (JPH, SEW) reviewed the articles for inclusion in the review.
In order to be included in the review, the article had to describe at least one case of tetanus, the immunization history of a fully or partially immunized case and/or present the results of anti-tetanus antibodies and be written in either English or French. The formal search was supplemented by PubMed snowball searches performed on articles meeting pre-specified inclusion criteria. In addition, a review of references from each relevant article was undertaken.
Relevant data, including number of tetanus cases, age, sex, antibody titre, clinical outcome, historic tetanus toxoid immunization, including number of doses and timing were abstracted and collated (Microsoft Excel 2010, Redmond, WA). One author (JPH) abstracted the data which was reviewed for accuracy by a second author (SEW). Discrepancies (which were rare) were resolved through consensus.
A formal quality assessment of individual articles was not undertaken. The retrieved articles included case reports, case series or surveillance reports. To the authors’ knowledge, there is no validated tool for quality appraisal of these study designs. However, studies that were missing relevant data were excluded as per a priori inclusion and exclusion criteria. As this was a narrative synthesis of the literature, funnel plots and statistical assessments of heterogeneity were not appropriate measures of publication bias.
Results
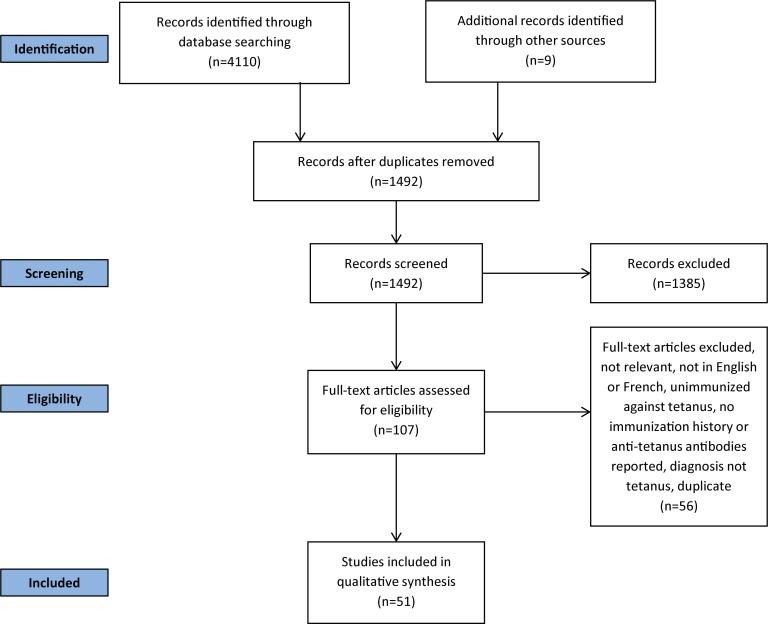
Over 4000 articles were initially identified. Fifty-one unique articles were included in the review. Figure 1 summarizes the literature search results.
Figure 1.
Literature search results
In the 51 studies that were included there were 359 cases of clinical tetanus in individuals with prior receipt of one or more doses of tetanus toxoid vaccine and/or levels of tetanus antibody titres generally considered protective (8,9). The majority of studies (n=25) were based on data from the United States. Of 47 cases where age and sex were described, 26 (39.4%) were male with a median age of 26 years (range 1-79 years). Fourteen cases had tetanus antibody titres drawn prior to administration of antitoxin, while the remaining 345 cases had immunization confirmed on record review. All cases of tetanus were diagnosed based on clinically compatible symptoms and signs. The isolation of Clostridium tetani was not reported in any case.
Vaccination histories of cases were reviewed within the case reports. While inclusion criteria required all cases to have received one or more doses, only 175 (48.7%) reported the exact number of doses. Ninety-four cases (26.2% of total cases) received three or more doses suggesting the primary series may have been completed, although it was not possible to assess the interval between doses. With respect to doses which occurred beyond early childhood and were described as “boosters” but which may or may not have been preceded by a complete primary vaccine series, 57 cases (15.9%) received a booster dose of tetanus toxoid within the last 10 years, 54 cases (15.0%) received a booster dose 10 or more years in the past and 248 cases (69.1%) last received a booster at an unknown interval (or no booster was given), or the case was not eligible for a booster (e.g. based on a historic policy or age) (data not shown). As more than half of the cases did not report the number of doses of tetanus toxoid received and there were a small number of deaths (n=30), it was not possible to analyze survival data by number of doses.
The high survival in published case reports suggest milder disease that is associated with better prognosis in individuals with a history of tetanus immunization (3,4,10-13). This is in keeping with an attenuation of clinical severity in immunized hosts that is recognized in other vaccine-preventable diseases (14-16).
Of the 180 of 210 (85.7%) cases that reported on clinical outcome survived to discharge and in cases that were followed beyond discharge, all except three (17-19) had complete resolution of symptoms. While survival generally appeared to improve over time, 42% of studies (n=149) did not report the clinical outcome so it was not possible to study survival trends as they related to other factors (e.g. systematic improvements in critical care over time and increased implementation of a 3–dose primary immunization series). The studies are summarized in Tables 1 and 2.
Table 1. Case reports of tetanus in individuals with complete data (detailed information on tetanus immunization history or tetanus antibody and clinical outcome).
| Author / country | Study design/ number of cases (n) | Age (years) and sex1 | Risk factors for tetanus2 | Vaccination history3 | Tetanus antibody titre at diagnosis4 | Patient outcome5 |
|---|---|---|---|---|---|---|
| Abrahamian (8) / United States | Case report/ n=1 | 45 M | IDU | ? | ++ | - |
| Atabek (9)/Turkey | Case report/ n=1 | 7 F | Laceration | ++ | ? | + |
| Aydin-Teke (20) / Turkey | Case report/ n=1 | 15 M | Injury | ++ | ? | + |
| Bardenheier (12) / United States | Surveillance/ n=31 | ? | ? | + (n=15) ++ (n=16) |
? | + (n=30) - (n=1) |
| Berger (21)/ United States | Case report/ n=1 | 25 F | IDU | ? | + | + |
| Boyd (22)/ Europe and Africa | Retrospective surveillance/ n=16 | ? | ? | +/++ | ? | + (n=11) - (n=5) |
| Boyer (23)/France | Case review/ n=10 | ? | ? | +/++ | ? | + (n=2) - (n=8) |
| Coniglione (24)/ United States | Case report/ n=1 | 29 M | Injury | ++ | ++ | + |
| Crone (17)/ United States | Case report/ n=3 | 29 M 42 F 57 F |
? IDU Reused syringe |
++ + + |
++ (n=3) | + - +(deficits) |
| de la Chapelle (25)/France | Case report/ n=1 | 52 M | Injury, IS | ? | ++ | + |
| Dyce (18)/ United States | Case report/ n=1 | 24 F | Piercing | ++ | ? | +(deficits) |
| Faust (26)/ United States | Hospital surveillance/ n=1 | 5 M | ? | + | ? | + |
| Fiorillo (27) / Canada | Case report/ n=1 | 10 M | Injury | ++ | ++ | + |
| Hall (28) / United States | Case report/ n=2 | ? | ? | + (n=2) | ? (n=2) | + (n=1) - (v1) |
| Hedrick (29) / United States | Case report/ n=2 | 10 M 45 M |
Injury ? |
++ + |
? (n=2) | + (n=2) |
| Hopkins (this report) / Canada | Case report/ n=1 | 22 M | Injury, IS | ++ | ? | + |
| König (30) / Germany | Case report/ n=1 | 14 M | Injury | ++ | ? | + |
| Livorsi (31) / United States | Case report/ n=1 | 44 M | Injury | ? | ++ | + |
| Lodha (32) / India | Case report/ n=2 | 3 F 4. 5 M |
? (n=2) | ? ++ |
? (n=2) | + (n=2) |
| Long (33) / United States | Surveillance/ n=6 | ? | Injury | ++ (n=6) | ? | + (n=3) - (n=3) |
| Loscalzo (34) / United States | Case report/ n=1 | 23 F | Piercing | ++ | ? | + |
| Luisto (35) / Finland | Retrospective case series/ n=5 | 5 M 10 F 12 M 13 F 15 F |
Animal bite Infection Injury Injury Burn |
++ ++ ++ ++ ? |
? (n=5) | + (n=5) |
| Newton-John (13) / Australia | Case series/ n=19 | ? | ? | ++ (n=13) + (n=6) |
? | + (n=17) - (n=2) |
| Otero-Maldonado (19) / Puerto Rico | Case report and surveillance/ n=7 | 67 M ? (n=6) |
Injury ? (n=6) |
+ ? (n=6) |
? (n=7) | +(deficits) + (n=5), - (n=1) |
| Pascual (11) / United States | Surveillance/ n=30 | ? | ? | + (n=10) ++ (n=20) |
? (n=30) | + (n=10) + (n=19), - (n=1) |
| Passen (36) / United States | Case report/ n=1 | 35 M | Injury | ++ | ++ | + |
| Peterson (37) / Sweden | Case report/ n=1 | 12 M | Injury | ++ | ++ | + |
| Spittle (38) / New Zealand | Case report/ n=1 | 25 F | Injury | ++ | ? | + |
| Tiwari (4) / United States | Surveillance/ n=55 | ? | ? | + (n=26) ++ (n=29) |
? (n=55) | + (n=17), - (n=3),? (n=6) + (n=24), - (n=1),? (n=4) |
| Vieria (39) / Australia | Case report/ n=1 | 18 M | Injury | ++ | ? | + |
1 M (male), F (female),? (unknown/not reported) 2 ? (unknown/not reported) 3 ++ (3 or more doses), + (1 or 2 doses),? (exact number of doses not reported) 4 ++ (>0. 1 IU/ml), + (0. 01-0. 09 IU/ml),?=not measured 5 + (alive at discharge), - (deceased),? (unknown/not reported) IDU = injection drug use IS = immunosuppression
Table 2. Case reports of tetanus in individuals lacking complete data (detailed) information on tetanus immunization history and/or clinical outcome).
| Author/ country | Study design/ number of cases (n) | Age (years) and sex1 | Risk factors for tetanus2 | Vaccination history3 | Tetanus antibody titre at diagnosis4 | Patient outcome5 |
|---|---|---|---|---|---|---|
| Bankole (40) / Nigeria | Case series/ n=11 | ? | ? | ? | ? | ? |
| Beltran (41) / United States | Case report/ n=1 | 58 M | Animal bite | ? | ++ | ? |
| Bunch (42) / United States | Case series/ n=5 | 53 F 59 F 62 F 65 F 75 F |
? Injury Infection Laceration Laceration |
? (n=5) | ? (n=5) | + (n=5) |
| Christensen (43) / United States | Case report/ n=1 | 10 M | Injury | + | ? | ? |
| Culbertson (44) / United States | Case report/ n=1 | 41 M | Burn, lacerations | ? | ? | + |
| deSouza (45) / India | Case control/ n=1 | ? | ? | + | ? | ? |
| Earis (46) / United Kingdom | Case report/ n=1 | 66 F | Fungating tumour | ? | ? | + |
| Edsall (47) / multiple | Review of previously published cases6/ n=4 | ? | ? | ? (n=4) | ? | + (n=3) - (n=1) |
| Ferris (48) / United Kingdom | Case report/ n=1 | 17 M | Trauma | ? | ? | + |
| Geeta (49) / India | Case series/ n=12 | 1 M ? (n=11) |
? | ++ + (n=11) |
? | ? |
| Hahn (50) / United States | Case report/ n=1 | 58 M | ? | ? | ? | + |
| Henderson (51) / United States | Case series/ n=5 | ? | Various injuries; IDU | ? | ? | ? |
| Iqbal (52) / Pakistan | Case series/ n=10 | ? | ? | ? | ? | ? |
| Lee (53) / Taiwan | Case series/ n=2 | 3 ? 5 ? |
? (n=2) | ? (n=2) | ? (n=2) | ? (n=2) |
| Masthi (54) / India | Case series/ n=2 | ? | ? | ? | ? | ? |
| O’Malley (55) / United States | Case report/ n=1 | 27 F | Piercing | ? | ++ | ? |
| Orwitz (56) / United States | Case report/ n=1 | 79 M | Infection | ? | ? | ? |
| Percy (57) / United States | Case series/ n=1 | ? | ? | + | ? | ? |
| Quackenbush (58) / United States | Case report/ n=1 | 44 F | Injury | ? | ? | + |
| Rushdy (10) / United Kingdom | Surveillance report/n=5 | ? | ? | ? | ? | ? |
| Shimoni (59) / Israel | Case report/ n=1 | 34 M | ? | ? | ? | + |
| Srigley (60) / Canada | Case report/ n=1 | 78 F | Injury | ? | ? | - |
1 M (male), F (female),? (unknown/not reported) 2 ? (unknown/not reported) 3 ++ (3 or more doses), + (1 or 2 doses),? (exact number of doses not reported) 4 ++ (>0. 1 IU/ml), + (0. 01-0. 09 IU/ml),?=not measured 5 + (alive at discharge), - (deceased),? (unknown/not reported) 6 Studies described in table (p. 127). Original studies were obtained where possible (Long, Hall, Boyd, Boyer, Christensen). Remaining studies were not indexed in PubMed, MEDLINE or EMBASE. The Journal of the American Medical Association (JAMA) was contacted for the original reference list which was excluded from the published manuscript due to length, but no copy was archived. Cases summarized here are from Moss and Hedrick. IDU = injection drug use IS = immunosuppression
Discussion
To the authors’ knowledge, this is the first systematic review which assesses the occurrence of tetanus in previously immunized individuals. Since 1946, at least 359 cases of tetanus have been described in previously immunized individuals and of those whose outcomes were reported, there was a survival rate of 85.7% with few cases reporting residual deficits at discharge. In cases that reported the number of doses of tetanus toxoid previously received by individuals, the clinical severity of disease appeared to be less compared to those who received fewer previous doses (although this could not be studied systematically due to the small number of deaths and cases symptomatic at discharge).
A previous review found a similar relationship between the number of doses and clinical severity. A review of 175 tetanus cases reported through routine surveillance between 1984 and 2000 in England and Wales found that clinical severity was greater in those with no previous history of immunization (although this did not reach statistical significance (p=0. 068)) (10).
Potential explanations for the occurrence of clinical tetanus in the setting of past immunization could include: waning of vaccine-derived immunity; vaccine failure; the presence of an unrecognized immunodeficiency resulting in sub-optimal immune response to active vaccination; or compromised vaccine storage and handling resulting in reduced immunogenicity of the vaccine product. Alternatively, the burden of tetanus exotoxin may exceed an individual’s immune response which may be additionally influenced by factors that cause immune suppression, such as chronic diseases or medications.
Limitations of this review include: the inability to assess how frequent this phenomenon is due to the lack of a denominator; potential publication bias; and incomplete data (e.g. survival). In addition, the inherent limitations of case studies and surveillance reports include: collection of source information (e.g. recall bias if self-reported, data quality and consistency if taken from databases; under-reporting or ability to capture all cases in a surveillance system); and a lack of a consistent clinical definition for tetanus in case reports created challenges in interpretation of the data.
Nonetheless, this study contributes significantly as it is possibly the first systematic review which summarizes the characteristics of tetanus in cases previously immunized with tetanus toxoid. Other strengths of this study include: the systematic methodology used to identify relevant studies; and the inclusion of articles from multiple countries, studies from 1946 through 2013 and studies in two languages.
Attenuation of disease severity in immunized hosts suggests the potential for under-reporting if the person does not present for medical care as well as the possibility of delayed diagnosis, although this was not consistently described in the included articles. This has important implications for the surveillance of vaccine-preventable diseases and clinical practice.
Future research directions might focus on understanding the incidence of tetanus in those with previous vaccination with tetanus toxoid and whether this is due to waning immunity or vaccine failure, the optimum timing of tetanus toxoid boosters and further research into the cut-off and role of anti-tetanus antibodies in determining immunity to tetanus.
Conclusions
Tetanus is a rare, but potentially lethal disease and Clostridium tetani are ubiquitous in the environment. A completed primary vaccine series and appropriate boosters clearly do not confer protective immunity in all recipients; however the survival rate is high in those with previously documented doses of tetanus toxoid. Clinicians should maintain a high index of clinical suspicion for tetanus when the clinical symptoms suggest it, regardless of vaccination history.
Acknowledgements
The authors express their sincere thanks to Public Health Ontario Library Services, in particular Beata Pach, for assistance with the systematic search and retrieval of literature and to Dr. Shelley Deeks for her helpful comments on an earlier draft of the manuscript.
Footnotes
Conflict of interest: There are no conflicts of interests to declare.
Funding: No funds were received for this study
References
- 1.American Public Health Association. Tetanus. In: Heymann DL, editor. Control of communicable diseases manual, 19th Ed. Washington, D. C.: American Public Health Association; 2008. 602-8. [Google Scholar]
- 2.Public Health Agency of Canada. Tetanus. 2012 [updated 2012-11-23; cited 2013 2013-05-03]; http://www.phac-aspc.gc.ca/im/vpd-mev/tetanus-eng.php
- 3.Public Health Agency of Canada. Tetanus toxoid. 2012. In: Canadian Immunization Guide [Internet]. Public Health Agency of Canada. http://www.phac-aspc.gc.ca/publicat/cig-gci/p04-tet-eng.php
- 4.Tiwari T, Clark TA, Messonnier NE, Thomas CG; Centers for Disease Control and Prevention (CDC). Tetanus surveillance --- United States, 2001-2008. MMWR Morb Mortal Wkly Rep 2011. Apr;60(12):365–9. [PubMed] [Google Scholar]
- 5.Plotkin SA. Vaccines: correlates of vaccine-induced immunity. Clin Infect Dis 2008. Aug;47(3):401–9. 10.1086/589862 [DOI] [PubMed] [Google Scholar]
- 6.Plotkin SA. Correlates of protection induced by vaccination. Clin Vaccine Immunol 2010. Jul;17(7):1055–65. 10.1128/CVI.00131-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McComb JA. The prophylactic dose of homologous tetanus antitoxin. N Engl J Med 1964. Jan;270(4):175–8. 10.1056/NEJM196401232700404 [DOI] [PubMed] [Google Scholar]
- 8.Abrahamian FM, Pollack CV Jr, LoVecchio F, Nanda R, Carlson RW. Fatal tetanus in a drug abuser with “protective” antitetanus antibodies. J Emerg Med 2000. Feb;18(2):189–93. 10.1016/S0736-4679(99)00192-4 [DOI] [PubMed] [Google Scholar]
- 9.Atabek ME, Pirgon O. Tetanus in a fully immunized child. J Emerg Med 2005. Oct;29(3):345–6. 10.1016/j.jemermed.2005.06.005 [DOI] [PubMed] [Google Scholar]
- 10.Rushdy AA, White JM, Ramsay ME, Crowcroft NS. Tetanus in England and Wales, 1984-2000. Epidemiol Infect 2003. Feb;130(1):71–7. 10.1017/S0950268802007884 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pascual FB, McGinley EL, Zanardi LR, Cortese MM, Murphy TV. Tetanus surveillance--United States, 1998--2000. MMWR Surveill Summ 2003. Jun;52(3 SS03):1–8. [PubMed] [Google Scholar]
- 12.Bardenheier B, Prevots DR, Khetsuriani N, Wharton M. Tetanus surveillance--United States, 1995-1997. MMWR CDC Surveill Summ 1998. Jul;47(2 SS-2):1–13. [PubMed] [Google Scholar]
- 13.Newton-John HF. Tetanus in Victoria, 1957-1980. Review of 106 patients managed in one hospital. Med J Aust 1984. Feb;140(4):194–200. [PubMed] [Google Scholar]
- 14.van den Hoek A, Sonder GJ, Scholing M, Gijselaar D, van Binnendijk RS. Two cases of mild IgM-negative measles in previously vaccinated adults, the Netherlands, April and July 2011. Euro Surveill 2011. Dec;16(48):1–3. [PubMed] [Google Scholar]
- 15.Rota JS, Hickman CJ, Sowers SB, Rota PA, Mercader S, Bellini WJ. Two case studies of modified measles in vaccinated physicians exposed to primary measles cases: high risk of infection but low risk of transmission. J Infect Dis 2011. Jul;204 Suppl 1:S559–63. 10.1093/infdis/jir098 [DOI] [PubMed] [Google Scholar]
- 16.Chaves SS, Zhang J, Civen R, Watson BM, Carbajal T, Perella D et al. Varicella disease among vaccinated persons: clinical and epidemiological characteristics, 1997-2005. J Infect Dis 2008. Mar;197 Suppl 2:S127–31. 10.1086/522150 [DOI] [PubMed] [Google Scholar]
- 17.Crone NE, Reder AT. Severe tetanus in immunized patients with high anti-tetanus titers. Neurology 1992. Apr;42(4):761–4. 10.1212/WNL.42.4.761 [DOI] [PubMed] [Google Scholar]
- 18.Dyce O, Bruno JR, Hong D, Silverstein K, Brown MJ, Mirza N. Tongue piercing. The new “rusty nail”? Head Neck 2000. Oct;22(7):728–32. [DOI] [PubMed] [Google Scholar]
- 19.Otero-Maldonado M, Bosques-Rosado M, Soto-Malavé R, Deliz-Roldán B, Bertrán-Pasarell J, Vargas Otero P. Tetanus is still present in the 21st century: case report and review of literature. Bol Asoc Med P R 2011. Apr-Jun;103(2):41–7. [PubMed] [Google Scholar]
- 20.Aydin-Teke T, Bayhan GI, Afşarlar CE, Oz FN, Akansel AR, Tanir G. A report of two pediatric tetanus cases. Turk J Pediatr 2011. Jul-Aug;53(4):437–40. [PubMed] [Google Scholar]
- 21.Berger SA, Cherubin CE, Nelson S, Levine L. Tetanus despite preexisting antitetanus antibody. JAMA 1978. Aug;240(8):769–70. 10.1001/jama.1978.03290080059029 [DOI] [PubMed] [Google Scholar]
- 22.Boyd JS. Tetanus in the African and European theatres of war, 1939-1945. Lancet 1946. Jan;1(6387):113–9. 10.1016/S0140-6736(46)91262-7 [DOI] [PubMed] [Google Scholar]
- 23.Boyer J, Corre-Hurst L, Sapin-Jaloustre H, Tissier M. Le tétanos en milieu urbain; conditions d’apparition; déductions prophylactiques. Presse Med 1953. May;61(34):701–3. [PubMed] [Google Scholar]
- 24.Pryor T, Onarecker C, Coniglione T. Elevated antitoxin titers in a man with generalized tetanus. J Fam Pract 1997. Mar;44(3):299–303. [PubMed] [Google Scholar]
- 25.de La Chapelle A, Lavabre O, Pinsard M, Delamonica J, Relyveld EH. Tetanus in a renal transplant recipient exhibiting the presence of circulating antitetanus antibodies determined by ELISA. Biomed Pharmacother 2002. Jun;56(4):208–10. 10.1016/S0753-3322(02)00180-4 [DOI] [PubMed] [Google Scholar]
- 26.Faust RA, Vickers OR, Cohn I Jr. Tetanus: 2,449 cases in 68 years at Charity Hospital. J Trauma 1976. Sep;16(9):704–12. 10.1097/00005373-197609000-00004 [DOI] [PubMed] [Google Scholar]
- 27.Fiorillo L, Robinson JL. Localized tetanus in a child. Ann Emerg Med 1999. Apr;33(4):460–3. 10.1016/S0196-0644(99)70314-8 [DOI] [PubMed] [Google Scholar]
- 28.Hall WW. The U.S. Navy’s war record with tetanus toxoid. Ann Intern Med 1948. Feb;28(2):298–308. 10.7326/0003-4819-28-2-298 [DOI] [PubMed] [Google Scholar]
- 29.Hedrick EC. Tetanus: two cases in immunized persons. Calif Med 1953. Jul;79(1):49–50. [PMC free article] [PubMed] [Google Scholar]
- 30.König K, Ringe H, Dorner BG, Diers A, Uhlenberg B, Müller D et al. Atypical tetanus in a completely immunized 14-year-old boy. Pediatrics 2007. Nov;120(5):e1355–8. 10.1542/peds.2006-3386 [DOI] [PubMed] [Google Scholar]
- 31.Livorsi DJ, Eaton M, Glass J. Generalized tetanus despite prior vaccination and a protective level of anti-tetanus antibodies. Am J Med Sci 2010. Feb;339(2):200–1. 10.1097/MAJ.0b013e3181c2f534 [DOI] [PubMed] [Google Scholar]
- 32.Lodha R, Sareen A, Kumar RM, Arora NK. Tetanus in immunized children. Indian Pediatr 2000. Feb;37(2):223–4. [PubMed] [Google Scholar]
- 33.Long AP. Immunization to tetanus. 2009 2009 Jun 1. In: Medical Science Publication No 4 [Internet]. U. S. Army Medical Department. http://history.amedd.army.mil/booksdocs/korea/recad2/ch6-6.html
- 34.Loscalzo IL, Ryan J, Loscalzo J, Sama A, Cadag S. Tetanus: a clinical diagnosis. Am J Emerg Med 1995. Jul;13(4):488–90. 10.1016/0735-6757(95)90150-7 [DOI] [PubMed] [Google Scholar]
- 35.Luisto M, Iivanainen M. Tetanus of immunized children. Dev Med Child Neurol 1993. Apr;35(4):351–5. 10.1111/j.1469-8749.1993.tb11648.x [DOI] [PubMed] [Google Scholar]
- 36.Passen EL, Andersen BR. Clinical tetanus despite a protective level of toxin-neutralizing antibody. JAMA 1986. Mar;255(9):1171–3. 10.1001/jama.1986.03370090093029 [DOI] [PubMed] [Google Scholar]
- 37.Peterson HI. A case of tetanus in spite of active toxoid prophylaxis. Acta Chir Scand 1965. Feb;129:235–7. [PubMed] [Google Scholar]
- 38.Spittle BJ, Pollock M, O’Donnell TV. Tetanus occurring in spite of active immunisation. N Z Med J 1973. Apr;77(491):250–1. [PubMed] [Google Scholar]
- 39.Vieira BI, Dunne JW, Summers Q. Cephalic tetanus in an immunized patient. Clinical and electromyographic findings. Med J Aust 1986. Aug;145(3-4):156–7. [DOI] [PubMed] [Google Scholar]
- 40.Bankole IA, Danesi MA, Ojo OO, Okubadejo NU, Ojini FI. Characteristics and outcome of tetanus in adolescent and adult patients admitted to the Lagos University Teaching Hospital between 2000 and 2009. J Neurol Sci 2012. Dec;323(1-2):201–4. 10.1016/j.jns.2012.09.017 [DOI] [PubMed] [Google Scholar]
- 41.Beltran A, Go E, Haq M, Clarke HB, Zaman M, Recco RA. A case of clinical tetanus in a patient with protective antitetanus antibody level. South Med J 2007. Jan;100(1):83. 10.1097/SMJ.0b013e31802e2717 [DOI] [PubMed] [Google Scholar]
- 42.Bunch TJ, Thalji MK, Pellikka PA, Aksamit TR. Respiratory failure in tetanus: case report and review of a 25-year experience. Chest 2002. Oct;122(4):1488–92. 10.1378/chest.122.4.1488 [DOI] [PubMed] [Google Scholar]
- 43.Christensen NA, Thurber DL. Clinical experience with tetanus: 91 cases. Proc Staff Meet Mayo Clin 1957. Apr;32(7):146–58. [PubMed] [Google Scholar]
- 44.Culbertson TA, Kalliainen LK, Buchele BA. Tetanus and the plastic surgeon. Ann Plast Surg 2004. Aug;53(2):162–5. 10.1097/01.sap.0000110753.26286.f6 [DOI] [PubMed] [Google Scholar]
- 45.deSouza CE, Karnad DR, Tilve GH. Clinical and bacteriological profile of the ear in otogenic tetanus: a case control study. J Laryngol Otol 1992. Dec;106(12):1051–4. 10.1017/S0022215100121735 [DOI] [PubMed] [Google Scholar]
- 46.Earis JE, Hillis AN, Macaulay MB. Tetanus: an unusual source and site of infection. J Infect 1983. Jul;7(1):72–3. 10.1016/S0163-4453(83)91111-8 [DOI] [PubMed] [Google Scholar]
- 47.Edsall G. Specific prophylaxis of tetanus. J Am Med Assoc 1959. Sep;171(4):417–27. 10.1001/jama.1959.73010220003012 [DOI] [PubMed] [Google Scholar]
- 48.Ferris DM. A case of tetanus modified by previous immunization, presenting as a psychiatric condition. Nurs Times 1968. Aug;64(34):1139–40. [PubMed] [Google Scholar]
- 49.Geeta MG, Krishnakumar P, Mathews L. Intrathecal tetanus immunoglobulins in the management of tetanus. Indian J Pediatr 2007. Jan;74(1):43–5. 10.1007/s12098-007-0025-y [DOI] [PubMed] [Google Scholar]
- 50.Hahn BJ, Erogul M, Sinert R. Case report of tetanus in an immunized, healthy adult and no point of entry. J Emerg Med 2004. Oct;27(3):257–60. 10.1016/j.jemermed.2004.03.015 [DOI] [PubMed] [Google Scholar]
- 51.Henderson SO, Mody T, Groth DE, Moore JJ, Newton E. The presentation of tetanus in an emergency department. J Emerg Med 1998. Sep-Oct;16(5):705–8. 10.1016/S0736-4679(98)00082-1 [DOI] [PubMed] [Google Scholar]
- 52.Iqbal S, ul Iman N, ur Rahman S, Haroon M, Zaheer Z, ur Rahman N, et al. Trends of tetanus patients in North of Pakistan. J Med Sci (Peshawar, Print) 2012;20(2):90–3. http://www.jmedsci.com/admin/uploadpic/JMS-11-april2012-vol20no2.pdf [Google Scholar]
- 53.Lee HC, Ko WC, Chuang YC. Tetanus of the elderly. J Microbiol Immunol Infect 2000. Sep;33(3):191–6. [PubMed] [Google Scholar]
- 54.Masthi NR, Bharat G, Aswini, Chitra, Arul PP. A clinico epidemiological study of tetanus cases admitted to epidemic disease hospital, Bangalore. Indian J Public Health 2008. Oct-Dec;52(4):210–1. [PubMed] [Google Scholar]
- 55.O’Malley CD, Smith N, Braun R, Prevots DR. Tetanus associated with body piercing. Clin Infect Dis 1998. Nov;27(5):1343–4. 10.1093/clinids/27.5.1343 [DOI] [PubMed] [Google Scholar]
- 56.Orwitz JI, Galetta SL, Teener JW. Bilateral trochlear nerve palsy and downbeat nystagmus in a patient with cephalic tetanus. Neurology 1997. Sep;49(3):894–5. 10.1212/WNL.49.3.894 [DOI] [PubMed] [Google Scholar]
- 57.Percy AS, Kukora JS. The continuing problem of tetanus. Surg Gynecol Obstet 1985. Apr;160(4):307–12. [PubMed] [Google Scholar]
- 58.Quackenbush P, Tuorinsky S, Rabb R. Tetanus diagnosis sometimes elusive. Nurse Pract 2003. Nov;28(11):50–3. 10.1097/00006205-200311000-00015 [DOI] [PubMed] [Google Scholar]
- 59.Shimoni Z, Dobrousin A, Cohen J, Pitlik S. Tetanus in an immunised patient. BMJ 1999. Oct;319(7216):1049. 10.1136/bmj.319.7216.1049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Srigley JA, Haider S, Johnstone J. A lethal case of generalized tetanus. CMAJ 2011. Jun;183(9):1045–8. 10.1503/cmaj.101121 [DOI] [PMC free article] [PubMed] [Google Scholar]