Abstract
Purpose This study aims to compare the outcomes and complications of our technique for nonspanning total wrist arthrodesis using a locking plate with the standard carpometacarpal spanning technique.
Methods A retrospective review of charts was performed to identify patients who underwent total wrist arthrodesis by the senior author (S.W.W.). We compared the outcomes of 15 cases of nonspanning wrist fusion with a 2.4/2.7 mm locking T plate to 11 cases of spanning wrist fusion with a 2.7/3.5 mm locking compression plate. Minimum follow-up was 3 months. Indications for fusion included rheumatoid arthritis, posttraumatic arthritis, Kienböck's disease, primary osteoarthritis, juvenile inflammatory arthropathy, psoriasis, brachial plexopathy, failed hemi or total wrist arthroplasty, failed four-corner fusion, and failed proximal row carpectomy. The primary outcome was fusion. Secondary outcomes included time to union, patient-rated wrist evaluation score, numerical rating scale pain score, grip strength, and complications.
Results All the wrists got fused. There were no significant differences in objective and subjective outcomes between cohorts. There were three complications (27%) in the spanning group, including tendon rupture and peri-implant fracture at the third metacarpal. This was compared with three complications (20%) in the nonspanning group, consisting of hardware removal.
Discussion We achieved similar fusion rates employing both spanning and nonspanning total wrist arthrodesis techniques, without necessitating carpometacarpal arthrodesis in the latter. Complications associated with our method were comparably less severe than those reported in the literature. We advocate nonspanning arthrodesis as an alternative method for total wrist fusion with a high union rate and minimal risk of complications at the carpometacarpal joint.
Level of Evidence Therapeutic level IV.
Keywords: total wrist arthrodesis, nonspanning, spanning, carpometacarpal, complications
Techniques for total wrist arthrodesis vary widely. 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 High fusion rates and excellent mechanical stability have made internal fixation with compression plating from the third metacarpal to the radius the standard gold technique when treating patients who require fusion for degenerative, posttraumatic, rheumatoid, or paralytic conditions. 1 2 3 4 5 6 7 8 10 11 13 14 16 18 However, inclusion of the carpometacarpal (CMC) joint within the fusion mass remains a matter of considerable controversy. 1 2 3 4 5 6 7 8 9 10 13 16 17 18
Several authors have recommended simultaneous arthrodesis of the second and/or third CMC joint at the time of total wrist arthrodesis with a spanning plate, 2 4 5 6 7 10 16 18 to obtain rigid fixation across the fusion mass. Arthrodesis of the CMC joint is thought to potentially prevent micromotion at the CMC joint which can theoretically lead to hardware failure. 2 4 9 10 19 Conversely, painful CMC nonunion after spanning arthrodesis has been reported, 1 3 6 7 with one study reporting nonunion of the third CMC joint in up to 43% of patients. 1 As such, other authors have advocated total wrist arthrodesis using a spanning plate, without formally attempting to fuse the CMC joint, arguing that simply bridging the joint using the compression plate is sufficient. 1 8 11 Nevertheless, hardware-related complications are well reported in the literature, 1 3 consistent with concerns of hardware fatigue and failure over a mobile articulation. 6 13 While biomechanical testing has recently been reported for commercially available nonspanning plates, 20 we were unable to locate studies reporting on outcomes for nonspanning total wrist arthrodesis.
Our technique for nonspanning total wrist arthrodesis uses a low-profile t -shaped locking compression plate which does not span the CMC joint. The purpose of this study was to compare the fusion rate of our technique for nonspanning total wrist arthrodesis with the standard spanning arthrodesis technique. We hypothesized that the fusion rates would be similar, with a lower complication profile for the nonspanning technique.
Methods
After obtaining institutional review board approval, a retrospective review was conducted to identify patients who underwent total wrist arthrodesis using either a spanning or nonspanning technique by one hand surgeon at our institution. Between March 2002 and July 2011, 12 spanning total wrist arthrodeses (11 patients) were performed before the senior author (S.W.W.) changed techniques. A total of 15 nonspanning arthrodeses (15 patients) were performed between January 2011 and March 2016. We compared the outcomes between these two samples of convenience. The primary outcome was fusion. Secondary outcomes included time to union (weeks), numerical rating scale (NRS) pain score (1–10), patient-rated wrist evaluation (PRWE) score, grip strength, and complications, including neuropathy, tendinopathy, hardware removal, hardware loosening or breakage, and peri-implant fracture. Fusion was assessed in each case by the treating surgeon using clinical and radiographic criteria. Time to union was classified as successful fusion by a time interval (e.g., 6 weeks). Grip strength data were collected from last clinical examination. All patients were contacted by phone postoperatively to administer the PRWE and NRS and to inquire about subsequent surgery. Raw continuous data between cohorts were compared using a Student's t -test. Fischer's exact test was used to compare differences in raw categorical data.
Surgical Technique
Spanning Arthrodesis Technique
Indications for total wrist arthrodesis are well described in the literature. 2 4 6 8 9 10 11 12 13 14 15 16 17 A longitudinal incision is made on the dorsum of the wrist, just ulnar to Lister's tubercle, down to the level of the extensor retinaculum. The retinaculum is incised longitudinally along the border of the third compartment, and the extensor pollicis longus tendon is identified and retracted radially. The wrist capsule is then opened longitudinally, and the wrist flexed to provide access to the radiocarpal joint. Rongeurs are used to denude the articular surfaces and decorticate subchondral bone from the radiocarpal, midcarpal, and third CMC joints. In patients who have undergone a prior proximal row carpectomy (PRC) or patients with inflammatory disease and proximal row bone loss, the radiocapitate articulation is decorticated. 13
A groove is made along the middle of the distal radius using a rongeur and curette to provide placement for the plate. A 9-hole 2.7/3.5 mm locking compression plate (Synthes, Paoli, PA) is placed over the dorsal distal radius, capitate, and the shaft of the third metacarpal. Fluoroscopy in the anteroposterior and lateral planes is performed to confirm appropriate plate position before two self-tapping 2.7 mm screws are inserted into the metacarpal shaft and one into the base. The plate is fixed to the radial shaft using three 3.5 mm cortical screws. A final screw is placed obliquely through the capitate. The extensor retinaculum and wrist capsule are irrigated and closed with nonabsorbable sutures, and the incision is closed in layers over a suction drain. Patients are immobilized in a cast or removable splint anywhere from 2 to 6 weeks.
Nonspanning Arthrodesis Technique
Given the unproven benefits of spanning arthrodesis and the development of low-profile locking plate technology, the authors developed and initiated a technique to spare the CMC joints and enable a modest amount of postoperative CMC motion. Briefly, the wrist is incised, and the intercarpal and radiocarpal joints are exposed and decorticated as described above. A 2.4/2.7 mm volar distal radius locking compression plate (Synthes) is then contoured to achieve the desired wrist posture (usually 10–20 degrees of wrist extension). The contoured plate is applied directly to the dorsal surface of the distal carpal row and anchored into the trapezoid, capitate, and hamate using multiple fixed angles 2.4 mm locking screws ( Fig. 1 ). It is helpful to place a 27-gauge needle into the CMC joint during plate and screw placement to avoid screw penetration into the CMC joints. Care is taken to prevent plate impingement on the metacarpal bases. Fluoroscopy is performed to confirm plate position before securing the plate proximally to the distal radius shaft with both nonlocking and locking 2.7 mm screws using standard AO compression technique. Irrigation, closure, and postoperative splinting proceed according to the protocol described earlier.
Fig. 1.
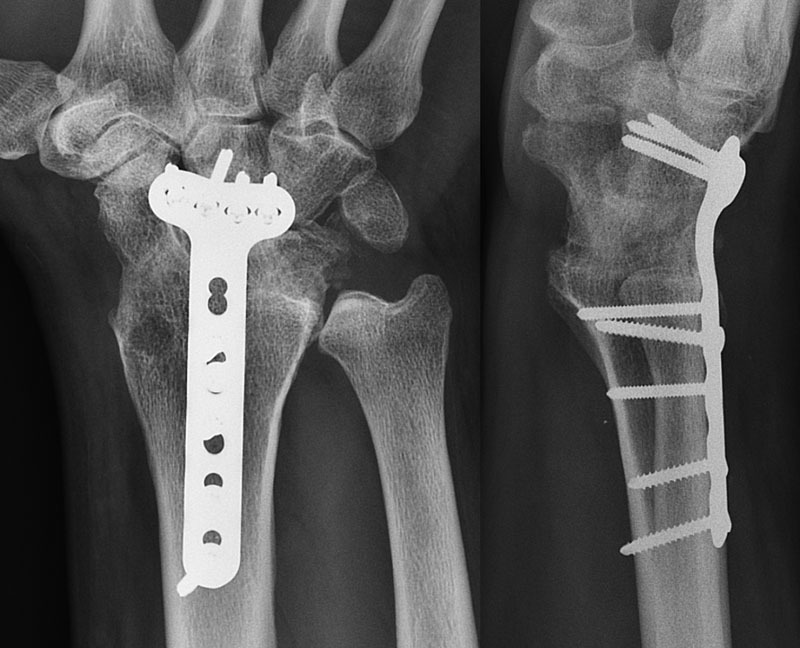
Posteroanterior and lateral radiographs 6 months postoperatively demonstrate solid right total wrist fusion in this 39-year-old male patient using a 2.4/2.7 mm locking compression plate.
Results
Outcomes
Table 1 compares objective and subjective outcomes of each technique. There were no significant differences in union rate, time to union, PRWE, NRS score, or length of follow-up ( p > 0.05). Out of 12, 11 arthrodeses (11 patients) in the spanning 2.7/3.5 mm plate group had minimum 3-months follow-up, and 6 were males while 5 were females. The average age of the spanning group was 60 ± 17 years. Average clinical follow-up was 29 ± 36 months. Out of 15, 15 arthrodeses (15 patients) in the nonspanning 2.4/2.7 mm plate group had an adequate follow-up, and 7 patients were males while 8 were females. The average age was 59 ± 12 years, and the average clinical follow-up was 13 ± 15 months.
Table 1. Comparison of outcomes for spanning and nonspanning total wrist arthrodesis.
| Spanning arthrodesis ( n = 11) |
Nonspanning arthrodesis ( n = 15) |
p -Value | |
|---|---|---|---|
| Fusion rate (%) | 100 | 100 | > 0.05 |
| Average time to union, range (wk) | 7.3 (5–12) | 7 (5–11) | > 0.05 |
| PRWE, range | 34.6 (9–77.5) | 25.9 (7.5–43) | > 0.05 |
| VAS pain score, range | 1.5 (0–7) | 0.8 (0–5) | > 0.05 |
| Grip strength, range (kg) | 35 (20–55) | ||
| Relative grip strength compared with contralateral (%) | 60 | ||
| Complications (%) | 3 (27%) | 3 (20%) | > 0.05 |
| ROH | 1 | 2 | |
| HWR breakage | 0 | 1 | |
| Tendinopathy | 1 | 0 | |
| Peri-implant fracture | 1 | 0 |
Abbreviations: HWR, hardware; PRWE, patient-rated wrist evaluation; ROH, removal of hardware; VAS, visual analog scale.
p < 0.05 denotes statistical significance.
Indications for operative treatment are detailed in Table 2 . In the spanning group, the autogenous bone graft was used in 10 of 11 cases: distal radius (8), iliac crest (1), and carpal bones (1). The femoral head allograft was used in one case. Eighteen concurrent procedures were performed, including Darrach's excision (4), flexor tenotomy (4), PRC (3), extensor tendon transfer (3), extensor tenosynovectomy (2), retinaculum reconstruction with extensor carpi radialis longus tendon (1), and extensor tenolysis (1). In the nonspanning group, the autogenous bone graft was used in 15 of 15 cases: distal radius (10), proximal tibia (2), iliac crest (1), ulnar head (1), and carpal bones (1). A total of 26 concurrent procedures were performed: extensor tendon transfer (4), radial styloidectomy (4), Darrach excision (3), triquetrum excision (3), carpal tunnel release (2), contracture release (2), scaphoidectomy (2), extensor tendon transposition (1), extensor tenosynovectomy (1), median nerve neurolysis (1), open relocation of the radiocarpal joint (1), posterior interosseous neurectomy (1), and ulnar styloidectomy (1).
Table 2. Surgical indications by cohort ( n = 26) .
| Indication | Spanning ( n = 11) | Nonspanning ( n = 15) |
|---|---|---|
| Rheumatoid arthritis | 4 (36%) | 3 (20%) |
| Psoriasis | 1 (9%) | 0 (0%) |
| Scapholunate advanced collapse | 1 (9%) | 0 (0%) |
| Scaphoid nonunion advanced collapse | 0 (0%) | 1 (7%) |
| Kienböck's disease | 1 (9%) | 0 (0%) |
| Juvenile inflammatory arthropathy | 0 (0%) | 0 (0%) |
| Brachial plexopathy | 0 (0%) | 1 (7%) |
| Primary arthritis | 0 (0%) | 0 (0%) |
| Failed 4-corner-arthrodesis | 0 (0%) | 6 (40%) |
| Failed proximal row carpectomy | 2 (18%) | 4 (27%) |
| Failed hemi- or total arthroplasty | 2 (18%) | 0 (0%) |
Six of the 11 spanning total wrist fusion patients were successfully contacted at average 106 ± 21 months postoperatively; three patients were disconnected, one patient had moved, and one elderly patient had died of unrelated causes. The average PRWE score in the spanning group was 34.6 (range, 9–77.5). Average NRS was 1.5 (range, 1–7). No grip strength data were available in this cohort for comparison. All 11 wrists fused after undergoing spanning total wrist arthrodesis by an average of 7 weeks (range, 5–12) on plain radiographic assessment.
Twelve of the 15 nonspanning wrist fusion patients were successfully contacted by phone at an average of 30 ± 19 months postoperatively; three patients did not respond after three contact attempts at least 1 week apart. The average PRWE score in the nonspanning group was 25.9 (range, 7.5–43). Average final NRS score was 0.8 (range, 0–5). Grip strength data were available on six patients in this group. In the fused wrist, mean grip strength was 35 kg (range, 20–55), compared with 58 kg (60%) of the contralateral wrist (range, 25–100). Fusion was achieved in 15 of 15 wrists by an average of 7 weeks (range, 5–11) using the same clinical and radiographic criteria.
Complications
In the spanning 2.7/3.5 mm plate group, complications occurred in three wrists (27%) at 7.5 ± 6.1 months. Plate removal was performed in one patient with painful hardware. One patient underwent index to middle end-to-side flexor digitorum profundus tenodesis following attritional rupture at 12 weeks. A different patient sustained open displaced peri-implant fractures of the third metacarpal and radius shaft at the screw and plate interfaces after falling from his roof and underwent open reduction and internal fixation. One patient with painful metacarpal screw back out declined hardware removal.
In the nonspanning 2.4/2.7 mm plate group, complications occurred in three wrists (20%) at 5.8 ± 3.3 months. Plate removal was performed for CMC impingement in one, screw breakage at the capitatotrapezoid articulation in one, and screw removal was performed for prominent hardware in one. The same patient who underwent hardware removal for CMC impingement also underwent ulnar styloidectomy for ulnar impingement and ulnar styloid fracture nonunion, and subsequently pisiform excision for pisotriquetral arthritis. Two patients reported third CMC pain of insufficient severity to require further intervention. One rheumatoid arthritis patient expressed a desire for wrist range of motion and was successfully revised to a total wrist arthroplasty 15 months postoperatively. No other patient in either group reported subsequent surgery on the operative wrist. There was no statistical difference in complication rate or time to complication ( p > 0.05).
Discussion
Complications involving the CMC joint after either attempted arthrodesis or plate bridging without arthrodesis are well reported. 1 3 6 7 13 21 Nagy and Büchler 1 found 20 of 47 wrists (43%) developed nonunion at the third CMC joint after attempted spanning total wrist arthrodesis using a dynamic compression plate. Out of 20, 11 nonunions were painful and 8 required subsequent surgery. 1 Hastings et al 6 reported 3 of 57 (5%) wrists developed painful third CMC nonunion after attempted spanning total wrist arthrodesis and underwent revision arthrodesis. In a series looking at 122 total wrist arthrodeses, Berling et al 3 reported that 20 wrists (16%) experienced hardware-related complications including screw fracture, plate loosening, and plate fracture. Seven of 20 complications occurred in wrists in which the CMC was included in the attempted arthrodesis, and 6 of these 7 patients progressed to third CMC nonunion.
In 34 wrists in which the third CMC joint was bridged with a compression plate but not arthrodesed during total wrist arthrodesis, Nagy and Büchler 1 reported two instances (6%) of hardware fatigue and breakage over the CMC joint. Zachary and Stern reported peri-implant metacarpal fracture in 2 of 73 (3%). 21 Berling et al 3 reported that out of 20 complications in their same series of 122 arthrodeses, 13 occurred in wrists in which the CMC was not included in the fusion mass. Overall, hardware-related complications in 19 of 20 wrists (95%) were attributed to micromotion at the CMC after either plate bridging (13 wrists) or attempted CMC arthrodesis that progressed to nonunion (6 wrists). 3
Fixed angle technology has enabled enhanced stability with a smaller plate and screw constructs ( Fig. 2 ). The advent of 2.4/2.7 mm fixed angle locking plates for distal radius fixation presented an opportunity to fuse the wrist with a lower profile implant and spare the CMC joint as well as the third metacarpal. In this study, we demonstrated a 100% fusion rate in a wide variety of diagnoses while sparing the CMC joints. Our high fusion rate is comparable to the 95% fusion rate (510/539) reported in the wrist literature. 2 4 5 6 7 8 11 18 21 22 23 24 25 26 27 28 29 Avoidance of CMC fusion with this alternative and intuitive technique has the advantage of preserving some CMC motion, which is important to grip strength, and may be of benefit in daily and recreational activities. 29 30 Furthermore, use of a low-profile nonspanning plate may lower complication rates and have cosmetic appeal to patients. Finally, avoidance of an implant in the third metacarpal theoretically facilitates subsequent metacarpophalangeal joint implant placement in patients with rheumatoid arthritis.
Fig. 2.

Commonly utilized plates for total wrist fusion are depicted. The preferred instrumentation for the nonspanning technique, the Synthes 2.4/2.7 mm volar distal radius locking compression plate, is situated rightmost, and is notably smaller compared with the other compression devices.
In our study, complications occurred in 3 of 15 in the nonspanning arthrodesis group (20%), consistent with 3 7 or better than 1 6 18 21 rates reported in other series, compared with 3 of 11 (27%) in the spanning arthrodesis group. Although there was no statistical difference in the rates of complication, the severity of complications (metacarpal fracture, tendon rupture) was considerably greater in the spanning plate group. Importantly, while no complications occurred at the CMC in our spanning cohort, the reported rates in the literature for CMC nonunion with spanning arthrodesis (19%, Table 3 ) strongly argue for a technique with modern instrumentation that avoids the risk of this complication entirely.
Table 3. Reported complications for spanning wrist arthrodesis.
| Complication type | n (%) | Reference |
|---|---|---|
| Flexor or extensor tendinopathy | 19/176 (11%) | 2 5 6 7 28 |
| Peripheral neuropathy | 18/222 (8%) | 6 7 8 21 |
| Radiocarpal nonunion | 29/539 (5%) | 2 4 6 7 8 11 18 21 22 23 24 25 26 27 28 29 |
| CMC nonunion | 26/136 (19%) | 1 3 22 25 |
| Peri-implant fracture | CMC 8/269 (3%) |
3 5 6 21 |
| Radiocarpal 4/97 (4%) |
8 21 25 | |
| Hardware breakage | CMC 16/156 (10%) |
1 3 |
| Radiocarpal 2/140 (1%) |
3 18 | |
| Hardware removal | 152/596 (26%) | 1 2 3 4 5 7 8 11 18 21 22 25 27 28 |
Abbreviation: CMC, carpometacarpal.
Previous authors have questioned whether the failure to fuse the CMC at the time of total wrist arthrodesis may result in long-term complications. 4 9 10 19 Joseph et al 19 postulated that the second and third metacarpals might be particularly vulnerable to bending torques during wrist flexion, possibly contributing to excessive CMC motion, and subsequent ligamentous laxity. Urbaniak 10 hypothesized that CMC mobility might increase following total wrist arthrodesis if the CMC is not included, adding to arguments that increased stress distally after total wrist arthrodesis may cause CMC joint capsule loosening and crepitus. 9 10 19 However, to our knowledge no data are available in the literature to support these propositions.
Nagy and Büchler 1 reported that 33 of their 34 patients remained asymptomatic at the CMC on stress and motion with 4.2 years of follow-up (range, 2–15) following spanning total wrist fusion without formal CMC arthrodesis. The one patient in their series with third CMC pain after hardware removal also presented with pain and excessive motion at all CMC joints and the general laxity of the upper extremity. O'Bierne et al 8 found no problems at the CMC joint with 45 months follow-up (range, 12–96) in 41 wrists. Similarly, in 11 wrists fused using 4.0 mm interfragmentary cancellous screws without CMC fusion, Rayan 9 did not observe any long-term complications at the CMC joint with 24 to 44 months of follow-up. Bolano and Green 4 reported two patients who developed painful CMC motion following PRC and radiocapitohamate arthrodesis using Kirschner-wires followed up to 30 months on average. However, they do not report if these patients presented with arthritic CMC articulations preoperatively and do not comment on ligamentous laxity. These observations suggest that painful CMC motion following nonspanning total wrist arthrodesis is not attributable to increased torsional stress and is more likely related to incidental preexisting conditions.
We acknowledge several important limitations to our study, including its retrospective design and the lack of preoperative grip strength and PRWE data. Not all patients were reached postoperatively for PRWE and NRS data collection. The follow-up obtained on our patients is relatively short to assess long-term complications, although there was no significant difference between cohorts in time to complication and this was confirmed with medium-term phone-follow-up. Finally, the reported numbers are also somewhat small compared with other series. Nevertheless, this is a proof of concept case series, and our data in this small cohort support further development of this technique and larger studies. In consideration of the simplicity of the described technique and its mechanical advantages, we favor nonspanning total wrist arthrodesis with a smaller fixed angle locking plate as a successful and simple alternative to traditional compression plating techniques with comparable outcomes.
Conflict of Interest None.
Note
This study was approved by the Hospital for Special Surgery's Institutional Review Board (#2015–396) on November 24, 2015.
References
- 1.Nagy L, Büchler U. AO-wrist arthrodesis: with and without arthrodesis of the third carpometacarpal joint. J Hand Surg Am. 2002;27(06):940–947. doi: 10.1053/jhsu.2002.35885. [DOI] [PubMed] [Google Scholar]
- 2.Weiss A P, Hastings H., II Wrist arthrodesis for traumatic conditions: a study of plate and local bone graft application. J Hand Surg Am. 1995;20(01):50–56. doi: 10.1016/S0363-5023(05)80058-9. [DOI] [PubMed] [Google Scholar]
- 3.Berling S E, Kiefhaber T R, Stern P J. Hardware-related complications following radiocarpal arthrodesis using a dorsal plate. J Wrist Surg. 2015;4(01):56–60. doi: 10.1055/s-0034-1400069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bolano L E, Green D P. Wrist arthrodesis in post-traumatic arthritis: a comparison of two methods. J Hand Surg Am. 1993;18(05):786–791. doi: 10.1016/0363-5023(93)90043-3. [DOI] [PubMed] [Google Scholar]
- 5.Hartigan B J, Nagle D J, Foley M J. Wrist arthrodesis with excision of the proximal carpal bones using the Ao/ASIF wrist fusion plate and local bone graft. J Hand Surg [Br] 2001;26(03):247–251. doi: 10.1054/jhsb.2000.0488. [DOI] [PubMed] [Google Scholar]
- 6.Hastings H, II, Weiss A-PC, Quenzer D, Wiedeman G P, Hanington K R, Strickland J W. Arthrodesis of the wrist for post-traumatic disorders. J Bone Joint Surg Am. 1996;78(06):897–902. doi: 10.2106/00004623-199606000-00013. [DOI] [PubMed] [Google Scholar]
- 7.Houshian S, Schrøder H A. Wrist arthrodesis with the AO titanium wrist fusion plate: a consecutive series of 42 cases. J Hand Surg [Br] 2001;26(04):355–359. doi: 10.1054/jhsb.2001.0600. [DOI] [PubMed] [Google Scholar]
- 8.O'Bierne J, Boyer M I, Axelrod T S. Wrist arthrodesis using a dynamic compression plate. J Bone Joint Surg Br. 1995;77(05):700–704. [PubMed] [Google Scholar]
- 9.Rayan G M. Wrist arthrodesis. J Hand Surg Am. 1986;11(03):356–364. doi: 10.1016/s0363-5023(86)80142-3. [DOI] [PubMed] [Google Scholar]
- 10.Urbaniak J R. New York, NY: Churchill Livingstone; 1983. Arthrodesis of the hand and wrist; pp. 2371–2386. [Google Scholar]
- 11.Bracey D J, McMurtry R Y, Walton D. Arthrodesis in the rheumatoid hand using the AO technique. Orthop Rev. 1980;9:65–69. [Google Scholar]
- 12.Onuma K, Shintani R, Fujimaki H et al. Total wrist arthrodesis with wrist fusion rod in patients with rheumatoid arthritis. Eklem Hastalik Cerrahisi. 2015;26(01):41–48. doi: 10.5606/ehc.2015.10. [DOI] [PubMed] [Google Scholar]
- 13.Stanley J. Philadelphia, PA: Elsevier; 2010. Arthroplasty and arthrodesis of the wrist; pp. 429–463. [Google Scholar]
- 14.Hayden R J, Jebson P J. Wrist arthrodesis. Hand Clin. 2005;21(04):631–640. doi: 10.1016/j.hcl.2005.08.004. [DOI] [PubMed] [Google Scholar]
- 15.Pham T T, Lenoir H, Coulet B, Wargny M, Lazerges C, Chammas M. Proximal row carpectomy in total arthrodesis of the rheumatoid wrist. Orthop Traumatol Surg Res. 2015;101(08):919–922. doi: 10.1016/j.otsr.2015.09.032. [DOI] [PubMed] [Google Scholar]
- 16.Rauhaniemi J, Tiusanen H, Sipola E. Total wrist fusion: a study of 115 patients. J Hand Surg [Br] 2005;30(02):217–219. doi: 10.1016/j.jhsb.2004.11.008. [DOI] [PubMed] [Google Scholar]
- 17.Pardini A G, Jr, Pádua Gonçalves R F, Freitas A D, Chaves A B. Wrist arthrodesis with minimal internal fixation preserving the carpometacarpal joints. Rev Bras Ortop. 2015;45(01):67–71. doi: 10.1016/S2255-4971(15)30219-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sagerman S D, Palmer A K. Wrist arthrodesis using a dynamic compression plate. J Hand Surg [Br] 1996;21(04):437–441. doi: 10.1016/s0266-7681(96)80041-6. [DOI] [PubMed] [Google Scholar]
- 19.Joseph R B, Linscheid R L, Dobyns J H, Bryan R S. Chronic sprains of the carpometacarpal joints. J Hand Surg Am. 1981;6(02):172–180. doi: 10.1016/s0363-5023(81)80172-4. [DOI] [PubMed] [Google Scholar]
- 20.Passin S, Pochlatko N, Ebi D, Spiegel A, Sauerbier M. Biomechanical testing of a new total wrist arthrodesis plate [in German] Handchir Mikrochir Plast Chir. 2015;47(01):32–37. doi: 10.1055/s-0034-1398547. [DOI] [PubMed] [Google Scholar]
- 21.Zachary S V, Stern P J. Complications following AO/ASIF wrist arthrodesis. J Hand Surg Am. 1995;20(02):339–344. doi: 10.1016/S0363-5023(05)80037-1. [DOI] [PubMed] [Google Scholar]
- 22.del Pino J G. A new total wrist fusion locking plate for patients with small hands or with failed partial wrist fusion: preliminary experience. J Wrist Surg. 2014;3(02):148–153. doi: 10.1055/s-0033-1351657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Terzis J K, Barmpitsioti A. Wrist fusion in posttraumatic brachial plexus palsy. Plast Reconstr Surg. 2009;124(06):2027–2039. doi: 10.1097/PRS.0b013e3181bcefe0. [DOI] [PubMed] [Google Scholar]
- 24.Wright C S, McMurtry R Y. AO arthrodesis in the hand. J Hand Surg Am. 1983;8(06):932–935. doi: 10.1016/s0363-5023(83)80099-9. [DOI] [PubMed] [Google Scholar]
- 25.Wang T, Chan C M, Yu F, Li Y, Niu X. Does wrist arthrodesis with structural iliac crest bone graft after wide resection of distal radius giant cell tumor result in satisfactory function and local control? Clin Orthop Relat Res. 2017;475(03):767–775. doi: 10.1007/s11999-015-4678-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Adams B D, Kleinhenz B P, Guan J J. Wrist arthrodesis for failed total wrist arthroplasty. J Hand Surg Am. 2016;41(06):673–679. doi: 10.1016/j.jhsa.2016.02.012. [DOI] [PubMed] [Google Scholar]
- 27.Giuffre J L, Bishop A T, Spinner R J, Kircher M F, Shin A Y. Wrist, first carpometacarpal joint, and thumb interphalangeal joint arthrodesis in patients with brachial plexus injuries. J Hand Surg Am. 2012;37(12):2557–630. doi: 10.1016/j.jhsa.2012.09.017. [DOI] [PubMed] [Google Scholar]
- 28.Clarkson P W, Sandford K, Phillips A E et al. Functional results following vascularized versus nonvascularized bone grafts for wrist arthrodesis following excision of giant cell tumors. J Hand Surg Am. 2013;38(05):935–9400. doi: 10.1016/j.jhsa.2012.12.026. [DOI] [PubMed] [Google Scholar]
- 29.Larsson S E. Compression arthrodesis of the wrist. A consecutive series of 23 cases. Clin Orthop Relat Res. 1974;(99):146–153. doi: 10.1097/00003086-197403000-00018. [DOI] [PubMed] [Google Scholar]
- 30.Abbott L C, Saunders J BDM, Bost F C. Arthrodesis of the wrist with the use of grafts of cancellous bone. J Bone Joint Surg Am. 1942;24:883–898. [Google Scholar]


