ABSTRACT
Opsonizing antibody is a critical component of the host protective immune response against many respiratory pathogens. However, the role of antibodies in protection against pulmonary infection with highly virulent Francisella tularensis strain SchuS4 is unclear, and the mechanism that allows F. tularensis to evade antibody-mediated bacterial clearance is not fully understood. We have now found that depletion of alveolar macrophages reveals an otherwise cryptic protective effect of opsonizing antibody. While antibody opsonization alone failed to confer any survival benefit against SchuS4 lung infection, significant protection was observed when mice were depleted of alveolar macrophages prior to infection. Blood immune signature analyses and bacterial burden measurements indicated that the treatment regimen blocked establishment of productive, systemic infection. In addition, protection was found to be dependent upon neutrophils. The results show for the first time a protective effect of opsonizing antibodies against highly virulent F. tularensis SchuS4 pulmonary infection through depletion of alveolar macrophages, the primary bacterial reservoir, and prevention of systemic dissemination. These findings have important implications for the potential use of therapeutic antibodies against intracellular pathogens that may escape clearance by residing within mucosal macrophages.
KEYWORDS: Francisella tularensis, humoral immunity, lung infection, macrophages
INTRODUCTION
Several respiratory pathogens infect mucosal macrophages and thereby disrupt host immune defenses. For example, inhalation of very low numbers of Francisella tularensis bacteria (as few as 10 CFU) can result in high levels of lethality due to bacterial survival and replication within alveolar macrophages (1–5), ultimately leading to sepsis and systemic inflammation (6–9). The high rate of mortality from pneumonic tularemia has resulted in the classification of F. tularensis subsp. tularensis, e.g., F. tularensis strain SchuS4, as a tier 1 select agent (10, 11).
No licensed vaccine offering protection against F. tularensis exists. The so-called F. tularensis live vaccine strain (LVS), which was attenuated via serial passage through mice (12, 13), is considered to be unacceptable for use in humans due to concerns over safety and potential reversion to virulence. Investigations designed to develop a safer, more effective vaccine have been hampered by the limited efficacy of adaptive humoral immunity against F. tularensis. For example, it has been found that opsonization of LVS fails to facilitate bactericidal activity by unstimulated macrophages in vitro (14), and passive transfer of LVS-immune serum fails to protect against the fully virulent SchuS4 strain (14, 15). The failure of humoral immunity to control F. tularensis infection may be related to its intracellular lifestyle. F. tularensis is known to replicate within alveolar macrophages and infects these cells rapidly following inhalation (1, 16). During infection, F. tularensis subverts phagosomal maturation, escapes the phagosome, and replicates within the cytoplasm of the infected cell (3, 5, 17–19). Uptake by macrophages is facilitated by antibody opsonization without an increase in intracellular killing (20, 21).
In the current study, we examined the influence of alveolar macrophages on antibody-mediated protection against highly virulent F. tularensis strain SchuS4. We found that the presence of alveolar macrophages can impede antibody-mediated control of SchuS4 infection. In addition, we observed that neutrophils were required for the protective efficacy of opsonizing antibodies. Thus, factors favoring an environment low in alveolar macrophages and enriched for neutrophils early in infection can increase the ability of humoral immunity to control SchuS4 infection. These insights provide a proof of concept for a protective effect of humoral immunity against virulent F. tularensis strains, laying the groundwork for future research into therapeutic interventions that may bypass the detrimental effect of alveolar macrophages on humoral immunity.
RESULTS
Alveolar macrophage depletion exposes the protective effects of opsonizing antibodies against SchuS4 infection.
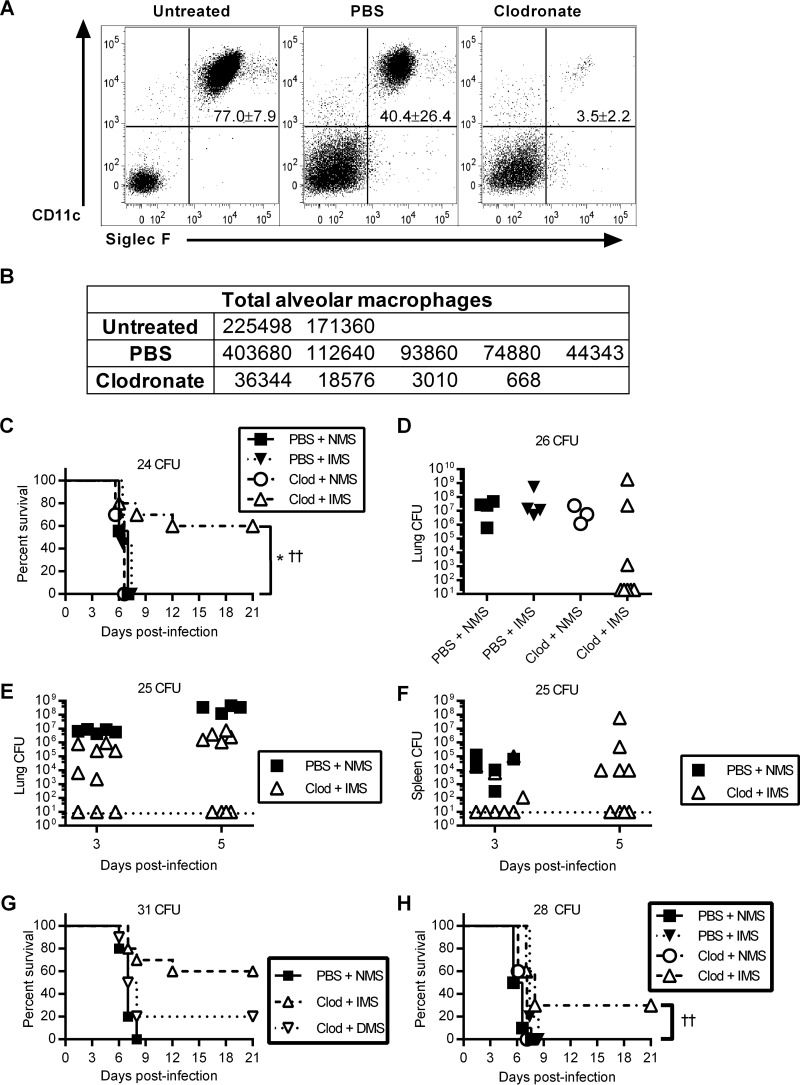
Passive transfer of F. tularensis-specific antibodies has been clearly shown to protect mice against LVS infection (14, 15, 22), and antibody has also been reported to play a role in protection against SchuS4 infection (23, 24). However, it has been difficult to protect mice against highly virulent SchuS4 lung infection using passive antibody therapy (14, 15). Since alveolar macrophages are prevalent in the lung and F. tularensis is an intracellular pathogen that replicates within macrophages, we reexamined the protective effects of opsonizing antibodies in the absence of alveolar macrophages. Mice were treated intranasally (i.n.) with liposomes containing clodronate to deplete alveolar macrophages. Control mice were treated with liposomes containing phosphate-buffered saline (PBS) (PBS-liposomes). Flow cytometric analysis of bronchoalveolar lavage fluid (BALF) confirmed that clodronate treatment depleted approximately 90% of alveolar macrophages, as defined by the expression of CD11c and Siglec F, and reduced the levels of alveolar macrophages to 1 to 3% of all BALF cells (Fig. 1A and B). We also examined alveolar macrophages and interstitial macrophages (defined as CD11c− CD11b+ F4/80+ cells) in whole-lung digests and confirmed that alveolar macrophages were depleted but that interstitial macrophages were not (see Fig. S1 in the supplemental material). Although Siglec F is commonly used as an eosinophil marker, it can be employed in combination with CD11c to identify alveolar macrophages (25). Mice treated with PBS-liposomes exhibited similar total numbers of alveolar macrophages as untreated mice, although the specific macrophage population represented a lower percentage of total BALF cells due to the influx of other cells, including neutrophils (see below). We next opsonized F. tularensis SchuS4 with 10% immune mouse serum (IMS) or naive mouse serum (NMS) and used these preparations to i.n. challenge mice that had been treated with liposomal clodronate or PBS 24 h earlier. Consistent with our previous report (14), LVS-specific IMS failed to protect PBS-liposome-pretreated mice against i.n. SchuS4 challenge (Fig. 1C). In contrast, the combination of clodronate treatment and IMS opsonization resulted in 60% survival against an infectious dose of 24 CFU. All mice treated with IMS plus PBS-liposomes or with clodronate plus NMS succumbed to infection within 7 days and at the same time as the control group, i.e., mice treated with PBS-liposomes and challenged with NMS-opsonized bacteria. These results indicate that alveolar macrophage depletion facilitates antibody-mediated protection from lethal pneumonic tularemia.
FIG 1.
Opsonizing antibodies exert protective effects against pneumonic F. tularensis SchuS4 infection only in the absence of alveolar macrophages. (A and B) BALB/c mice were treated i.n. with clodronate (Clod) or PBS-liposomes or were left untreated 1 day prior to BALF collection. BALF was analyzed by flow cytometry for alveolar macrophages (CD11c+ SiglecF+ cells). (A) Representative flow plots are shown. Numbers at upper right represent events within gate as a percentage of all viable cells in the sample, with standard deviations. (B) The total number of alveolar macrophages was calculated for all mice. (C) Survival curves for F. tularensis SchuS4-infected mice with or without clodronate treatment and serum opsonization. BALB/c mice were treated i.n. with anionic liposomes containing clodronate or PBS 24 h prior to i.n. infection with the indicated dose of IMS-opsonized F. tularensis SchuS4 or NMS-opsonized F. tularensis SchuS4. Survival was monitored for 21 days. Each group contained 9 to 10 mice. The log-rank test was used for statistical analysis. *, P < 0.05 versus the clodronate + NMS and versus the PBS + IMS groups; ††, P < 0.01 versus the PBS + NMS group. These data are representative of those from four independent experiments. (D) BALB/c mice were treated and infected with the indicated dose of SchuS4, as described in the legend to panel C, and the lungs were harvested on day 5 postinfection to determine the bacterial burden by plating of lung tissue on Mueller-Hinton chocolate agar plates. (E and F) BALB/c mice were treated and infected with the indicated dose of F. tularensis SchuS4 as described in the legend to panel C. At the indicated time points, lungs (E) and spleens (F) were harvested and homogenized for enumeration of the bacterial burden, as described in the legend to panel D. The lines indicate the limit of detection, as defined by the lowest dilution plated for that time point. Five mice (PBS + NMS group) or 10 mice (clodronate + IMS group) were sacrificed at each time point. Results were analyzed by two-way ANOVA. In panels E and F, P was <0.001 between the PBS + NMS group and the clodronate + IMS group. Data represent those from two independent experiments. (G) Mice were treated and infected as described in the legend to panel C, and bacteria were opsonized with NMS, with IMS depleted of IgG (DMS), or with IMS run through a control column. Survival was monitored for 21 days. Five mice (PBS + NMS group) or 10 mice (clodronate + IMS and clodronate + DMS groups) were used in each group. (H) Mice were treated with clodronate and treated i.p. with 250 μl of NMS or IMS 24 h prior to infection. Survival was monitored for 21 days. Each group contained 10 mice. ††, P < 0.01 versus the PBS + NMS group and clodronate + NMS group.
We also observed that all the above-described groups exhibited high lung bacterial burdens on day 5, except for a number of mice in the liposomal clodronate-IMS treatment group (Fig. 1D). Similarly, on both days 3 and 5 after infection, we found that several mice from the clodronate-IMS treatment group had undetectable levels of lung and splenic bacteria, while others had bacteria at levels above the limit of detection, although they were still below the levels seen in liposomal PBS-treated control mice infected with NMS-opsonized bacteria, indicating a reduction of the burden but not the complete prevention of infection (Fig. 1E and F).
To establish that the protective effect of opsonization resulted from Ig rather than other serum components, such as complement, we infected clodronate-treated and PBS-treated mice with bacteria opsonized with NMS, IMS depleted of Ig (DMS), or IMS passed through a nondepleting control column (Fig. 1G). The IMS control conferred robust protection in combination with clodronate treatment, but DMS protected weakly, suggesting either the presence of residual Ig or a minor protective effect of non-Ig components that survived heat treatment. The ratio of surviving IMS-treated/DMS-treated mice (60%/20%) suggests that Ig is primarily responsible for the protective effect of opsonization.
Finally, we tested the protective combination of immune serum and alveolar macrophage depletion in a more physiologically relevant passive transfer experiment, to simulate the presence of circulating specific antibody in the blood like that in vaccinated individuals. We observed significant protection when immune serum was administered to clodronate-treated animals (Fig. 1H). Conversely, passive transfer of immune serum failed to protect alveolar macrophage-sufficient animals. These results indicate that in the absence of alveolar macrophages, immune serum can facilitate the clearance of bacteria from the lungs and decrease dissemination to other organs.
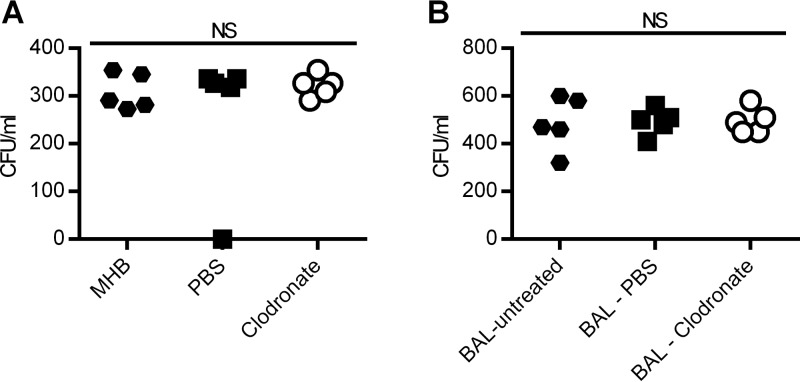
Since we observed an increased protective efficacy of opsonizing antibodies against SchuS4 infection in clodronate-treated mice, we wished to rule out a direct detrimental effect of clodronate on F. tularensis. We incubated F. tularensis SchuS4 in the presence or absence of liposomal clodronate to assess possible bactericidal effects (Fig. 2A). The concentration of liposomes in this assay is likely to be higher than the physiological concentrations in the lungs of mice at the time of infection, which would make any bactericidal activity readily apparent. In view of the possibility that clodronate-containing liposomes might break down after administration to animals or that they might elicit secretion of bactericidal factors by the host, we also compared incubation of F. tularensis SchuS4 with BALF from untreated mice with incubation of F. tularensis SchuS4 with BALF from mice treated with liposomal PBS or clodronate (Fig. 2B). In all cases, we detected no statistically significant difference in bacterial numbers, indicating that neither liposomal clodronate nor clodronate-treated BALF is directly bactericidal.
FIG 2.
Clodronate treatment does not result in a bactericidal alveolar environment. (A) F. tularensis SchuS4 bacteria were incubated at 37°C for 1 h at a density of 273 CFU/ml (60 CFU in 220 μl) in MHB medium alone or in MHB medium containing 20% clodronate-containing liposomes or PBS-containing liposomes. The bacterial burden per milliliter was assessed by plating following incubation. (B) BALB/c mice were treated i.n. with liposomal clodronate or PBS or were left untreated 1 day prior to collection of BALF. F. tularensis SchuS4 bacteria were incubated at 37°C for 1 h in sterile-filtered BALF at a density of 300 CFU/ml (60 CFU in 200 μl). The bacterial burden per milliliter was assessed by plating following incubation. NS, not significant by one-way ANOVA.
Antibody opsonization with alveolar macrophage depletion prevents systemic inflammation and sepsis.
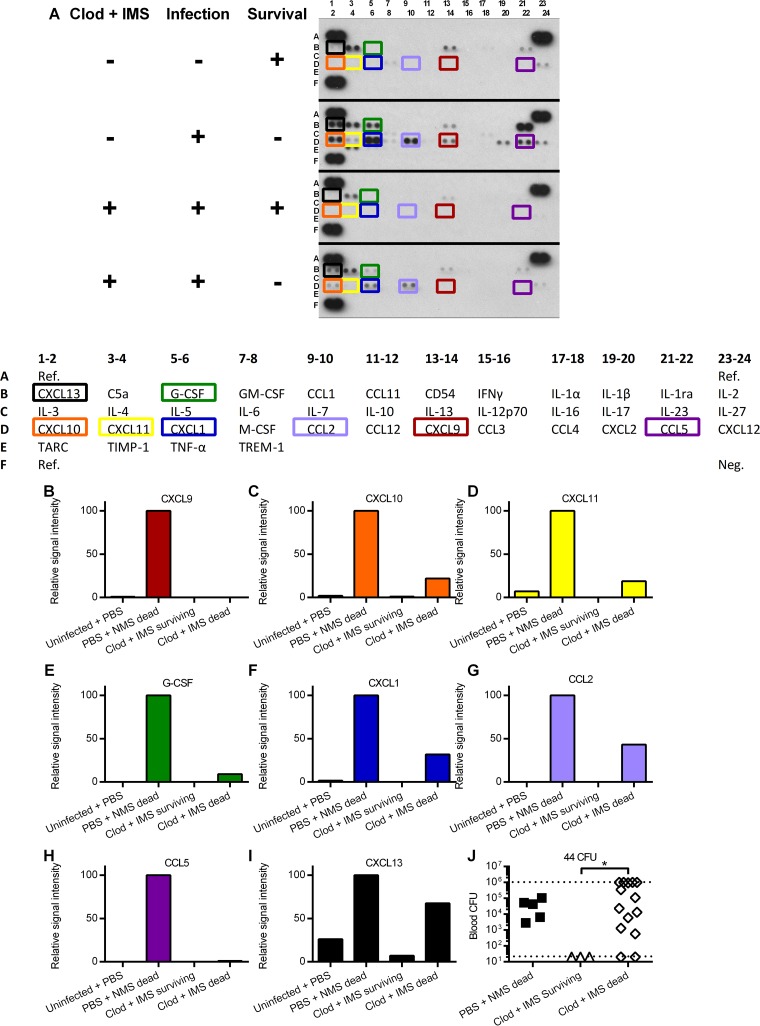
As seen above, following macrophage depletion and challenge with IMS-opsonized SchuS4, many, but not all, mice survived, and we could not predict which mice would ultimately survive or succumb to infection, thus hampering interpretation of the lung bacterial burden results. Thus, we examined cytokine expression and bacterial levels in the blood on day 5 after infection and then determined whether development of sepsis and a systemic cytokine storm would ultimately correlate with mortality. This was achieved by collecting serum from each mouse 5 days after infection and monitoring survival. At 21 days postinfection, serum pools were created on the basis of the animals' initial treatment regimen and ultimate survival status (serum pools were needed due to the relatively large volumes required for the blot assay, and this therefore precluded statistical analysis). In the group treated with clodronate and challenged with IMS-opsonized bacteria, increased levels of several cytokines were seen in animals that ultimately succumbed to infection, a pattern that was similar to that for the infected group treated with PBS-liposomes, which likewise failed to survive infection (Fig. 3A to I). These cytokines included CXCL9, CXCL10, and CXCL11, all of which are secreted in response to gamma interferon (IFN-γ) (26–28); granulocyte colony-stimulating factor (G-CSF) and CXCL-1, which promote granulopoiesis and stimulation of neutrophils (29–31); and CCL2, CCL5, and CXCL13, which recruit or activate monocytes, NK cells, T cells, and B cells (32–35). In contrast, mice that ultimately survived following clodronate treatment and challenge with IMS-opsonized bacteria yielded a day 5 cytokine signature that most closely resembled that of uninfected animals. Similarly, bacteria were undetectable in the blood of mice that ultimately survived but were present in most mice that eventually succumbed to infection (Fig. 3J). It has been found that live F. tularensis SchuS4 can be recovered from the spleens of LVS-vaccinated BALB/c mice that survive virulent SchuS4 challenge (36; unpublished observations). However, at 21 days after alveolar macrophage depletion, we could not detect any bacteria in the spleens of mice that survived SchuS4 challenge, and these animals remained fully susceptible to rechallenge with SchuS4 (data not shown). Thus, antibody-mediated protection in the absence of alveolar macrophages appears to be associated with the prevention of disseminated infection and a systemic cytokine storm.
FIG 3.
Mice protected after alveolar macrophage depletion and bacterial opsonization do not show evidence of systemic infection. (A to I) BALB/c mice were treated i.n. with anionic liposomes containing clodronate or PBS 24 h prior to i.n. infection with 11 CFU of IMS-opsonized or NMS-opsonized F. tularensis SchuS4. Survival was monitored for 21 days. Blood was drawn from uninfected mice and from mice on day 5 following infection (day 6 following clodronate treatment) and frozen for later analysis. On day 21 following infection, the samples were pooled according to the survival status and the treatment conditions of the mice and analyzed for relative cytokine levels using a membrane-bound capture antibody array. Data are for 3 mice in the PBS + NMS dead group, 4 mice in the clodronate + IMS dead group, or 5 mice in the uninfected and clodronate + IMS surviving groups. (A) A Proteome Profiler (R&D Systems) film exposure of the array membranes for the four serum pools. Dark spots in the lower right and upper corners of each membrane are reference points for orientation. A key to the contents of the profiler is shown below. GM-CSF, granulocyte-macrophage colony-stimulating factor; M-CSF, macrophage colony-stimulating factor; TARC, thymus- and activation-regulated chemokine; TIMP-1, tissue inhibitor of metalloproteinases 1; TNF-α, tumor necrosis factor alpha. TREM-1, triggering receptor expressed on myeloid cells 1. The other abbreviations are defined in the text. (B to I) Quantification of the signal intensities for select cytokines detected in panel A. Values are relative to the signal intensity of the PBS + NMS dead group. (J) BALB/c mice were treated i.n. with anionic liposomes containing clodronate or PBS 24 h prior to i.n. infection with the indicated dose of IMS-opsonized F. tularensis SchuS4 or NMS-opsonized F. tularensis SchuS4. Survival was monitored for 21 days. Blood was drawn from mice on day 5 following infection (day 6 following clodronate treatment) for enumeration of the bacterial burden. The lines indicate the limits of detection, as defined by the highest and lowest dilutions plated. There were 5 mice per group for the PBS-treated group, 3 mice per group for the surviving clodronate-treated group, and 14 mice per group for the nonsurviving clodronate-treated group. *, P < 0.05 by the Kruskal-Wallis test and by Dunn's multiple-comparison test. The Kruskal-Wallis and Dunn's tests were chosen because the data did not exhibit a normal distribution.
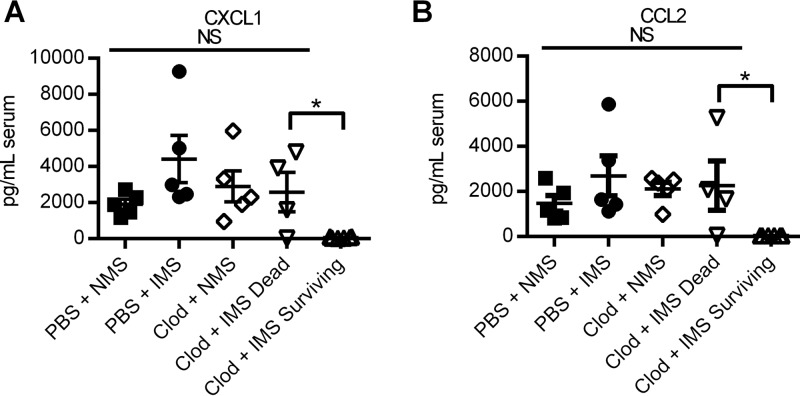
To confirm the results obtained in the cytokine blot analysis, we quantified by enzyme-linked immunosorbent assay (ELISA) the expression of two chemokines that showed differential production: CXCL1 (Fig. 4A) and CCL2 (Fig. 4B). Expression of these chemokines was consistent with the findings of the qualitative blot analysis; elevated serum levels of both mediators were associated with mortality, and low or undetectable levels were associated with survival, regardless of the initial conditions of infection or treatment. These results confirm the association of systemic inflammation, particularly that involving neutrophil and monocytic chemoattractive chemokines, with a lethal outcome.
FIG 4.
Elevated chemokine levels in serum are associated with mortality following F. tularensis SchuS4 infection. (A and B) Serum samples from individual mice used in the assay whose results are shown in Fig. 1G were analyzed by ELISA to determine the concentrations of CXCL1 (A) and CCL2 (B). *, P < 0.05 by Student's t test; NS, not significant by one-way ANOVA. Data are representative of those from two independent experiments.
Neutrophils contribute to opsonization-mediated protection only in the absence of alveolar macrophages.
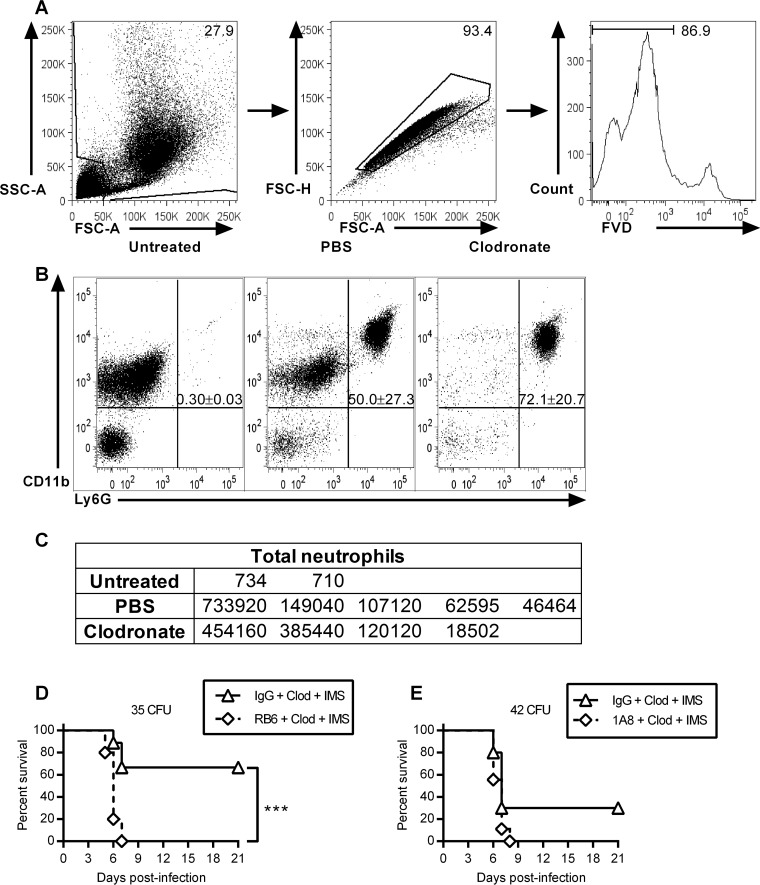
The finding of elevated chemotactic cytokine levels in mice destined to succumb to infection is consistent with existing evidence indicating that neutrophils can play a detrimental role in F. tularensis infection (37). However, early recruitment of neutrophils to the lungs has also been associated with survival from F. tularensis LVS pulmonary infection (38). Furthermore, we observed that i.n. liposome treatment increased the total numbers of neutrophils (defined as Ly6G+ CD11b+ cells) to ≥105 in the lung, resulting in neutrophil levels approaching 80% of total BALF cells (Fig. 5A to C). Increases in neutrophil numbers were seen following treatment with either liposomal PBS or clodronate, indicating that the liposome inoculation itself led to enhanced neutrophil expression in the lung, a finding consistent with the previous reports of others (39). The neutrophil increase following liposomal PBS treatment was accompanied by a decrease in the percentages of alveolar macrophages but not actual macrophage numbers (Fig. 1A and B). However, infection was controlled only by IMS-liposomal clodronate and not by IMS-liposomal PBS, indicating that alveolar macrophages may be impeding the neutrophil-mediated clearance of opsonized bacteria. We hypothesized that the combination of clodronate treatment and SchuS4 antibody opsonization might promote host survival by redirecting the bacteria away from their primary replicative site within alveolar macrophages and toward recruited, phagocytic myeloid cells. To test this possibility, infected mice were treated with a depleting anti-GR1 (RB6-8C5) monoclonal antibody (MAb) or a neutrophil-specific anti-Ly6G (1A8) MAb. Treatment with either antibody consistently reduced neutrophil levels to <10% of total BALF cells (data not shown). Again, a proportion of neutrophil-sufficient mice survived SchuS4 challenge doses of 35 CFU (Fig. 5D) and 42 CFU (Fig. 5E) following the combination of clodronate treatment and challenge with IMS-opsonized bacteria. However, this protection was completely eliminated by depletion of cells with either the RB6-8C5 or 1A8 MAb. We conclude that in pneumonic F. tularensis infection, alveolar macrophages play a detrimental role in antibody-mediated protection, while lung neutrophils must be present for antibody-mediated protection.
FIG 5.
Depletion of neutrophils abrogates the protection conferred by alveolar macrophage ablation and bacterial opsonization. (A to C) BALF was collected 24 h after treatment with clodronate or PBS-liposomes. (A) Gating strategy for cytometric analysis of populations for which the results are shown in panel B. SSC, side scatter; FSC, forward scatter. Numbers in top right corners represent the percentages of events on the graph within gate. FVD, fixable viability dye. (B) Representative flow cytometry plots showing increased lung neutrophil expression. Numbers at upper right represent events within gate as a percentage of all viable cells in the sample, with standard deviations. (C) Total neutrophils were calculated for all mice. (D) BALB/c mice were treated i.p. with the RB6-8C5 MAb or the IgG isotype control and i.n. with anionic liposomes containing clodronate 24 h prior to i.n. infection with the indicated dose of IMS-opsonized F. tularensis SchuS4. The RB6-8C5 MAb or the IgG isotype control was administered again i.p. on the day of infection. Survival was monitored for 21 days. (E) Mice were treated i.p. with the 1A8 MAb or the IgG isotype control and i.n. with anionic liposomes containing clodronate 24 h prior to i.n. infection with the indicated dose of IMS-opsonized F. tularensis SchuS4. The 1A8 MAb or the IgG isotype control was administered again i.p. on the day of infection. Survival was monitored for 21 days. P values were determined by the log-rank test. ***, P < 0.001. Data represent the results from two independent experiments.
DISCUSSION
It has been reported that the antibody response to F. tularensis is not sufficient to protect against infection with highly virulent strains (14, 15). Although the passive transfer of immune serum has been shown to extend the time to death in subcutaneous infection, it fails to influence the course of i.n. infection (24). We now provide evidence indicating that difficulties in passive immunization against pulmonary SchuS4 infection are due the presence of detrimental alveolar macrophages. Indeed, in the absence of alveolar macrophages, humoral immune-mediated protection became apparent. We also report that neutrophils, and not alveolar macrophages, are required for the clearance of antibody-opsonized SchuS4 in the lungs.
We considered the possibility that clodronate treatment and IMS opsonization led to enhanced survival by preventing systemic bacterial spread and/or lethal septic shock. Measurement of the bacterial burden early after infection revealed a striking dichotomy wherein some animals contained no detectable bacteria in the lungs or spleen, while others had significant bacterial levels. Although that pattern was consistent with the levels of survival observed (∼50%), the analysis could not distinguish which animals would ultimately survive and which would succumb to infection. To overcome this limitation, mice were bled on day 5 after infection and then monitored for survival over the remaining 16 days. The results showed that on day 5, none of the animals which ultimately survived had detectable levels of bacteria in the blood, suggesting that the clodronate/opsonization treatment either prevented initial lung infection or perhaps caused the bacteria to be sequestered in the lung without spread into the bloodstream. On the other hand, most mice that ultimately succumbed did show evidence of blood-borne bacteria. These blood samples were also used to obtain cytokine/chemokine expression signatures, and consistent with the bacterial burden results, it was found that surviving mice, like uninfected mice, expressed minimal levels of serum cytokines on day 5. Conversely, mice destined to succumb to infection produced cytokines at levels similar to those in untreated, infected mice that died. Interestingly, the immune mediators that were elevated in animals destined to die included neutrophil-attracting chemokines.
Antibody opsonization was ineffective in the presence of macrophages, consistent with earlier findings that the passive transfer of immune serum did not protect against SchuS4 pulmonary infection (14, 15, 24). It is not surprising that immune serum fails to protect in the absence of other treatments, given that opsonization increases the uptake of F. tularensis by macrophages in vitro but does not facilitate intracellular killing in the absence of IFN-γ stimulation (14). Nevertheless, the presence of antibody in the airway is associated with protection against a variety of respiratory infections (40–43), including infection with SchuS4 (23, 24), and Fc receptors are essential for the control of many pulmonary pathogens, including intracellular pathogens (44, 45). Our results show that in the absence of alveolar macrophages, F. tularensis becomes more susceptible to control by antibody-mediated mechanisms at the mucosal surface.
Alveolar macrophages are the primary phagocytic cells in the lungs and one of the earliest lines of defense against respiratory pathogens (46, 47). It is perhaps counterintuitive that depletion of these cells could enhance defense against a respiratory infection; however, the capacity of F. tularensis to subvert the function of pulmonary immune cells is well documented (48–50). It may be that in lethal infection, alveolar macrophages contribute more to the detriment than to the defense of the host.
We recently showed a protective function for alveolar macrophages in naive mice infected with sublethal doses of the attenuated strain F. tularensis LVS (51). Although the present work utilized a preopsonization model of adaptive immunity and involved a more virulent strain, our finding of a beneficial role for alveolar macrophage depletion stands in apparent opposition to our prior results. However, the observed discrepancy is not necessarily surprising, given the previous findings of others indicating that SchuS4 not only is more pathogenic than LVS but also possesses immunosuppressive mechanisms that LVS does not. For example, it has been shown that interleukin-17 (IL-17) expression is upregulated in the BALF and that the IL-17 receptor is essential for protection following infection with LVS but not with SchuS4 (52). Additionally, SchuS4 has been reported to downregulate production of the inflammatory cytokines IL-18 and IFN-α and to upregulate production of the anti-inflammatory cytokines IL-10 and transforming growth factor β (TGF-β), as well as the Th2-associated cytokine IL-13, while LVS does not (53). It is further possible that the attenuated strain LVS has an extracellular replicative phase that is subject to macrophage killing. Indeed, it has been reported by multiple groups that various F. tularensis strains can be detected in vivo in an extracellular state (54, 55).
We considered the possibility that our macrophage-depleting drug, clodronate, may possess some bactericidal activity. We tested for such activity by incubating F. tularensis SchuS4 in the presence of clodronate-containing liposomes. The conditions of this experiment are likely to involve concentrations of liposomes in excess of those that are present in the lungs at the time of infection, which would exacerbate any potential bactericidal effect. In view of the possibility that clodronate-containing liposome treatment results in the presence of other bactericidal factors in the lungs, such as free clodronate or secreted factors, we also incubated F. tularensis SchuS4 in sterile-filtered BALF from mice that had been treated with clodronate-containing liposomes. As extraction of BALF requires insufflation of fluid into the lungs, some dilution of any such factors necessarily occurred; this is an unavoidable consequence of such an assay. The fact that we saw not only no reduction in bacterial numbers but also an increase in bacteria under all conditions suggests that the potency of any bactericidal effect of clodronate must be negligible, even in view of the slightly diluted working material.
We found that neutrophils were crucial for survival from SchuS4 infection following clodronate/opsonization treatment. Furthermore, i.n. liposome treatment, even treatment with PBS-liposomes, resulted in increased numbers of neutrophils in the lungs, consistent with the findings of others utilizing pulmonary administration of liposomal preparations (39, 56, 57). It is unlikely that the recruitment of neutrophils is protective on its own; neutrophils recruited by PBS-liposomes were unable to control the infection, implying a necessity for the depletion of macrophages, in addition to neutrophil recruitment. We propose that an intact neutrophil population must exist for protection and that the protection observed following macrophage depletion involved neutrophil killing of antibody-opsonized F. tularensis. In support of this, antibody opsonization is known to enhance neutrophil phagocytosis of F. tularensis, and indeed, opsonization with complement or antibodies may be required for neutrophil-mediated control of F. tularensis infection (58–60). The finding that survival from pneumonic SchuS4 infection was dependent on neutrophils is novel because while neutrophils have been implicated in protection against intradermal F. tularensis infection (61), these cells have typically been perceived to be either unimportant or actually detrimental during respiratory infection (37, 62). Previous studies involved the use of nonopsonized F. tularensis or complement-opsonized F. tularensis and reported little or no NADPH oxidase activity after F. tularensis exposure. However, other experiments involving exposure of human neutrophils to F. tularensis that had been opsonized with complement-depleted serum from immunized individuals demonstrated enhanced NADPH oxidase activity (58, 59, 63). The potential role of NADPH in the protection seen in our study is under investigation.
The mechanism by which alveolar macrophages impede neutrophil-mediated protection remains to be determined. Multiple mechanisms may contribute to this effect simultaneously. One intriguing possibility is that F. tularensis bacteria that enter neutrophils are effectively sequestered from preferred hosts and are unable to replicate as efficiently as they would in alveolar macrophages or other cell types. It should be noted that although neutrophils have been observed to contain F. tularensis at later stages of respiratory infection (1) and to evade killing by cultured neutrophils (60), it has never been established that F. tularensis is actually capable of replicating within neutrophils. In fact, F. tularensis appears to maintain a stable population in isolated neutrophils (60), and recruitment of mature neutrophils has been associated with survival from LVS infection (64). In contrast, the capacity of F. tularensis to replicate within alveolar macrophages is well-known (3, 4, 65). Given that alveolar macrophages are the predominant cell type in healthy lungs (1, 16), sequestration within neutrophils may only play a major role in control of infection when the relative abundance of alveolar macrophages to neutrophils is reversed, as is the case with clodronate treatment.
Alternately, or perhaps in combination with the effect described above, alveolar macrophages may exert a suppressive effect on neutrophils, either directly or through interaction with local T cells. Alveolar macrophages are frequently described as having an immunosuppressive phenotype (66–69) and are a source of the immunomodulatory cytokine TGF-β (70, 71). TGF-β is known to have immunosuppressive effects on T cells and monocytes (72), but TGF-β receptors are also present on neutrophils (73), suggesting the possibility of direct action. Alveolar macrophages may also act as a source of prostaglandin E2 (74), which is known to have a suppressive effect on neutrophil activity (75–77). Future experiments using conditional TGF-β or prostaglandin E2 knockouts, antibody neutralization of these molecules, or antibody blocking of the cognate receptors could address the potential role of immunomodulatory signaling in F. tularensis infection.
In conclusion, our results show that the protective role of specific antibodies against a highly virulent intracellular bacterial pathogen is subverted by alveolar macrophages but can be enhanced by neutrophils. The approach of depleting the alveolar macrophage replication niche together with antibody opsonization appeared to prevent the systemic dissemination of disease and the consequent septic shock. Our results indicate that survival is dependent upon the presence of neutrophils and provide support for a critical role of humoral immunity in resistance against F. tularensis. These findings advance our understanding of the interaction between intracellular pathogens and the milieu of the infected lung.
Our findings may ultimately provide novel insight into immunotherapy approaches for protection against highly virulent pulmonary infections. Alveolar macrophage depletion is not likely to be a viable strategy for treating pulmonary tularemia in humans. However, the observation that alveolar macrophages inhibit serum-mediated protection suggests that future strategies could deliberately target F. tularensis for uptake by neutrophils rather than macrophages. Such strategies might include controlled recruitment of neutrophils or immunomodulatory therapies to alter the phenotype of alveolar macrophages and render them more conducive to bacterial clearance.
MATERIALS AND METHODS
Ethics statement.
All animal procedures followed the guidelines in the Guide for the Care and Use of Animals, 8th ed., of the National Research Council (78) and were approved by the Institutional Animal Care and Use Committee of Albany Medical College (protocol 15-04001). All of the described work was performed in a CDC-approved animal biosafety level 3 facility.
Bacteria.
F. tularensis SchuS4 was originally obtained from the U.S. Army Medical Research Institute for Infectious Diseases (Frederick, MD). F. tularensis LVS was obtained from Karen Elkins, FDA, Bethesda, MD. F. tularensis was grown in Mueller-Hinton broth (MHB; Becton Dickinson) supplemented with IsoVitaleX (Becton Dickinson). The bacteria were grown to log phase at 37°C and stored frozen at −80°C.
Mice.
BALB/c mice were purchased from Taconic and housed under conventional specific-pathogen-free conditions. They were provided food and water ad libitum.
Infections.
Mice were anesthetized by intraperitoneal (i.p.) inoculation of 100 μl PBS containing 20 mg/ml ketamine and 5 mg/ml xylazine and then inoculated i.n. with bacteria from frozen stocks in a volume of 40 to 50 μl/mouse in PBS. All samples used for infection were simultaneously plated on chocolate agar to confirm the number of CFU.
Opsonization.
SchuS4, diluted to the concentration to be used for infection, was incubated for 30 min at room temperature in PBS containing 10% pooled, heat-inactivated serum from naive BALB/c mice (NMS) or BALB/c mice that had been immunized with live LVS (IMS). All IMS samples used for the study had an anti-LVS antibody titer of >1,800.
Serum Ig depletion.
Cyanogen bromide-activated Sepharose 4B beads (Sigma) were coupled with goat anti-mouse Ig or normal goat IgG as a control according to the manufacturer's instructions (Southern Biotech). Two hundred microliters of IMS was incubated with the beads overnight at 4°C on an end-to-end mixer. The beads were centrifuged on the following day, and the supernatants were stored at −80°C.
Passive serum transfer.
Mice were immunized by i.n. infection with a sublethal (<100 CFU) dose of F. tularensis LVS, followed 5 weeks later by an i.n. boost with 1,000 CFU of LVS. Immunized mice and naive mice were sacrificed 1 week later, and blood was collected by cardiac puncture. Pooled IMS and NMS were administered to naive mice i.p. in a volume of 250 μl 24 h prior to i.n. infection with F. tularensis SchuS4.
Bacterial burden analysis.
Mice were sacrificed at the time points described elsewhere in the article by i.p. injection of pentobarbital, followed by cervical dislocation. Lungs and spleens were harvested and homogenized in 1 ml of PBS using a minibeadbeater. Homogenates were centrifuged, and the supernatants were plated on chocolate agar for enumeration. Blood was collected into microcentrifuge tubes containing 25 μl of 3.33 mg/ml heparin, equivalent to 600 USP units/ml.
Macrophage depletion.
Lung macrophages were depleted by liposomal clodronate treatment. Clophosome anionic liposomes containing either clodronate or PBS (FormuMax) were administered i.n. to anesthetized mice in 50-μl volumes 24 h before infection. Macrophage depletion was confirmed by flow cytometry analysis of BALF. Lung cells were stained with an allophycocyanin-conjugated anti-CD11c MAb (clone N418; BioLegend), a phycoerythrin (PE)-conjugated anti-Siglec F MAb (clone E50-2440; BD Pharmingen), and a peridinin chlorophyll protein-Cy5.5-conjugated anti-F4/80 MAb (clone BM8; eBioscience) to identify alveolar macrophage populations and with a fluorescein isothiocyanate-conjugated anti-CD11b MAb (clone M170; eBioscience) and a PE-Cy7-conjugated anti-Ly6G MAb (clone 1A8; BioLegend) to identify neutrophil populations. Dead cells were excluded by staining with eFluor780 fixable viability dye (eBioscience) in PBS, followed by washing twice in PBS containing 10% fetal bovine serum (FBS). The cells were subsequently stained with antibodies for 30 min on ice in PBS–10% FBS and washed twice with PBS–10% FBS. Stained cells were analyzed using a FACSCanto flow cytometer, and the data were evaluated using FlowJo software (TreeStar).
Neutrophil depletion.
Myeloid cells were depleted by inoculation of the RB6-8C5 GR1-specific MAb (BioXCell) or the 1A8 Ly6G-specific MAb (BioXCell). Depleting antibodies or Ig isotype controls were administered i.p. in two 100-μg doses at 24 h prior to infection and on the day of infection. Neutrophil depletion was confirmed by flow cytometry, as described above.
Cytokine analyses.
Sera were collected on day 5 following infection. Serum cytokines in pooled samples were assessed using a Proteome Profiler mouse cytokine array panel A (R&D Systems) according to the manufacturer's instructions. Serum pools were needed due to the relatively large volumes required for this assay. The blots were analyzed using ImageJ software (NIH) with a MicroArray Profile plug-in (OptiNav). Data represent gray values from image negatives with the background subtracted. The levels of selected serum chemokines were also measured using nonpooled samples from individual mice and DuoSet ELISA kits (R&D Systems) according to the manufacturer's instructions.
Statistical analyses.
Survival results were analyzed by Mantel-Cox log-rank tests with Bonferroni corrections where appropriate. Bacterial burden levels were analyzed by two-way analysis of variance (ANOVA), with multiple comparisons for treatment conditions being performed using the Bonferroni correction. ELISA and in vitro clodronate bactericidal results were analyzed by one-way ANOVA and Student's t test. For single-time-point bacterial burden analyses, the Kruskal-Wallis test was performed with Dunn's multiple-comparison test. All statistics were determined using GraphPad Prism (version 6) software, with statistical significance considered to be a P value of <0.05.
Supplementary Material
ACKNOWLEDGMENTS
We are indebted to Greg Hurteau, Sean Roberts, and Sharon Salmon for technical assistance.
This work was supported by NIH grant PO1 A1056320.
The funders had no role in study design, data collection and interpretation, or the decision to submit the work for publication.
Footnotes
Supplemental material for this article may be found at https://doi.org/10.1128/IAI.00787-17.
REFERENCES
- 1.Hall JD, Woolard MD, Gunn BM, Craven RR, Taft-Benz S, Frelinger JA, Kawula TH. 2008. Infected-host-cell repertoire and cellular response in the lung following inhalation of Francisella tularensis Schu S4, LVS, or U112. Infect Immun 76:5843–5852. doi: 10.1128/IAI.01176-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anthony LD, Burke RD, Nano FE. 1991. Growth of Francisella spp. in rodent macrophages. Infect Immun 59:3291–3296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fortier AH, Leiby DA, Narayanan RB, Asafoadjei E, Crawford RM, Nacy CA, Meltzer MS. 1995. Growth of Francisella tularensis LVS in macrophages: the acidic intracellular compartment provides essential iron required for growth. Infect Immun 63:1478–1483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lai XH, Golovliov I, Sjostedt A. 2001. Francisella tularensis induces cytopathogenicity and apoptosis in murine macrophages via a mechanism that requires intracellular bacterial multiplication. Infect Immun 69:4691–4694. doi: 10.1128/IAI.69.7.4691-4694.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shepard CC. 1959. Nonacid-fast bacteria and HeLa cells: their uptake and subsequent intracellular growth. J Bacteriol 77:701–714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sharma J, Mares CA, Li Q, Morris EG, Teale JM. 2011. Features of sepsis caused by pulmonary infection with Francisella tularensis type A strain. Microb Pathog 51:39–47. doi: 10.1016/j.micpath.2011.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McCrumb FR. 1961. Aerosol infection of man with Pasteurella tularensis. Bacteriol Rev 25:262–267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mares CA, Ojeda SS, Morris EG, Li Q, Teale JM. 2008. Initial delay in the immune response to Francisella tularensis is followed by hypercytokinemia characteristic of severe sepsis and correlating with upregulation and release of damage-associated molecular patterns. Infect Immun 76:3001–3010. doi: 10.1128/IAI.00215-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Conlan JW, Zhao X, Harris G, Shen H, Bolanowski M, Rietz C, Sjostedt A, Chen W. 2008. Molecular immunology of experimental primary tularemia in mice infected by respiratory or intradermal routes with type A Francisella tularensis. Mol Immunol 45:2962–2969. doi: 10.1016/j.molimm.2008.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Harris S. 1992. Japanese biological warfare research on humans: a case study of microbiology and ethics. Ann N Y Acad Sci 666:21–52. doi: 10.1111/j.1749-6632.1992.tb38021.x. [DOI] [PubMed] [Google Scholar]
- 11.Dennis DT, Inglesby TV, Henderson DA, Bartlett JG, Ascher MS, Eitzen E, Fine AD, Friedlander AM, Hauer J, Layton M, Lillibridge SR, McDade JE, Osterholm MT, O'Toole T, Parker G, Perl TM, Russell PK, Tonat K. 2001. Tularemia as a biological weapon: medical and public health management. JAMA 285:2763–2773. doi: 10.1001/jama.285.21.2763. [DOI] [PubMed] [Google Scholar]
- 12.Eigelsbach HT, Downs CM. 1961. Prophylactic effectiveness of live and killed tularemia vaccines. I. Production of vaccine and evaluation in the white mouse and guinea pig. J Immunol 87:415–425. [PubMed] [Google Scholar]
- 13.Tigertt WD. 1962. Soviet viable Pasteurella tularensis vaccines. A review of selected articles. Bacteriol Rev 26:354–373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kirimanjeswara GS, Golden JM, Bakshi CS, Metzger DW. 2007. Prophylactic and therapeutic use of antibodies for protection against respiratory infection with Francisella tularensis. J Immunol 179:532–539. doi: 10.4049/jimmunol.179.1.532. [DOI] [PubMed] [Google Scholar]
- 15.Fulop M, Mastroeni P, Green M, Titball RW. 2001. Role of antibody to lipopolysaccharide in protection against low- and high-virulence strains of Francisella tularensis. Vaccine 19:4465–4472. doi: 10.1016/S0264-410X(01)00189-X. [DOI] [PubMed] [Google Scholar]
- 16.Roberts LM, Tuladhar S, Steele SP, Riebe KJ, Chen CJ, Cumming RI, Seay S, Frothingham R, Sempowski GD, Kawula TH, Frelinger JA. 2014. Identification of early interactions between Francisella and the host. Infect Immun 82:2504–2510. doi: 10.1128/iai.01654-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Golovliov I, Baranov V, Krocova Z, Kovarova H, Sjostedt A. 2003. An attenuated strain of the facultative intracellular bacterium Francisella tularensis can escape the phagosome of monocytic cells. Infect Immun 71:5940–5950. doi: 10.1128/IAI.71.10.5940-5950.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Clemens DL, Lee BY, Horwitz MA. 2004. Virulent and avirulent strains of Francisella tularensis prevent acidification and maturation of their phagosomes and escape into the cytoplasm in human macrophages. Infect Immun 72:3204–3217. doi: 10.1128/IAI.72.6.3204-3217.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bolger CE, Forestal CA, Italo JK, Benach JL, Furie MB. 2005. The live vaccine strain of Francisella tularensis replicates in human and murine macrophages but induces only the human cells to secrete proinflammatory cytokines. J Leukoc Biol 77:893–897. doi: 10.1189/jlb.1104637. [DOI] [PubMed] [Google Scholar]
- 20.Balagopal A, MacFarlane AS, Mohapatra N, Soni S, Gunn JS, Schlesinger LS. 2006. Characterization of the receptor-ligand pathways important for entry and survival of Francisella tularensis in human macrophages. Infect Immun 74:5114–5125. doi: 10.1128/IAI.00795-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Geier H, Celli J. 2011. Phagocytic receptors dictate phagosomal escape and intracellular proliferation of Francisella tularensis. Infect Immun 79:2204–2214. doi: 10.1128/IAI.01382-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Del Barrio L, Sahoo M, Lantier L, Reynolds JM, Ceballos-Olvera I, Re F. 2015. Production of anti-LPS IgM by B1a B cells depends on IL-1beta and is protective against lung infection with Francisella tularensis LVS. PLoS Pathog 11:e1004706. doi: 10.1371/journal.ppat.1004706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mara-Koosham G, Hutt JA, Lyons CR, Wu TH. 2011. Antibodies contribute to effective vaccination against respiratory infection by type A Francisella tularensis strains. Infect Immun 79:1770–1778. doi: 10.1128/IAI.00605-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Richard K, Mann BJ, Qin A, Barry EM, Ernst RK, Vogel SN. 2017. Monophosphoryl lipid A enhances efficacy of a Francisella tularensis LVS-catanionic nanoparticle subunit vaccine against F. tularensis Schu S4 challenge by augmenting both humoral and cellular immunity. Clin Vaccine Immunol 24:e00574016. doi: 10.1128/cvi.00574-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Misharin AV, Morales-Nebreda L, Mutlu GM, Budinger GR, Perlman H. 2013. Flow cytometric analysis of macrophages and dendritic cell subsets in the mouse lung. Am J Respir Cell Mol Biol 49:503–510. doi: 10.1165/rcmb.2013-0086MA. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Luster AD, Ravetch JV. 1987. Biochemical characterization of a gamma interferon-inducible cytokine (IP-10). J Exp Med 166:1084–1097. doi: 10.1084/jem.166.4.1084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Farber JM. 1997. Mig and IP-10: CXC chemokines that target lymphocytes. J Leukoc Biol 61:246–257. [PubMed] [Google Scholar]
- 28.Cole KE, Strick CA, Paradis TJ, Ogborne KT, Loetscher M, Gladue RP, Lin W, Boyd JG, Moser B, Wood DE, Sahagan BG, Neote K. 1998. Interferon-inducible T cell alpha chemoattractant (I-TAC): a novel non-ELR CXC chemokine with potent activity on activated T cells through selective high affinity binding to CXCR3. J Exp Med 187:2009–2021. doi: 10.1084/jem.187.12.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Metcalf D. 1985. The granulocyte-macrophage colony-stimulating factors. Science 229:16–22. doi: 10.1126/science.2990035. [DOI] [PubMed] [Google Scholar]
- 30.Moser B, Clark-Lewis I, Zwahlen R, Baggiolini M. 1990. Neutrophil-activating properties of the melanoma growth-stimulatory activity. J Exp Med 171:1797–1802. doi: 10.1084/jem.171.5.1797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schumacher C, Clark-Lewis I, Baggiolini M, Moser B. 1992. High- and low-affinity binding of GRO alpha and neutrophil-activating peptide 2 to interleukin 8 receptors on human neutrophils. Proc Natl Acad Sci U S A 89:10542–10546. doi: 10.1073/pnas.89.21.10542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yoshimura T, Robinson EA, Tanaka S, Appella E, Kuratsu J, Leonard EJ. 1989. Purification and amino acid analysis of two human glioma-derived monocyte chemoattractants. J Exp Med 169:1449–1459. doi: 10.1084/jem.169.4.1449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Carr MW, Roth SJ, Luther E, Rose SS, Springer TA. 1994. Monocyte chemoattractant protein 1 acts as a T-lymphocyte chemoattractant. Proc Natl Acad Sci U S A 91:3652–3656. doi: 10.1073/pnas.91.9.3652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Maghazachi AA, Al-Aoukaty A, Schall TJ. 1996. CC chemokines induce the generation of killer cells from CD56+ cells. Eur J Immunol 26:315–319. doi: 10.1002/eji.1830260207. [DOI] [PubMed] [Google Scholar]
- 35.Legler DF, Loetscher M, Roos RS, Clark-Lewis I, Baggiolini M, Moser B. 1998. B cell-attracting chemokine 1, a human CXC chemokine expressed in lymphoid tissues, selectively attracts B lymphocytes via BLR1/CXCR5. J Exp Med 187:655–660. doi: 10.1084/jem.187.4.655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wu TH, Hutt JA, Garrison KA, Berliba LS, Zhou Y, Lyons CR. 2005. Intranasal vaccination induces protective immunity against intranasal infection with virulent Francisella tularensis biovar A. Infect Immun 73:2644–2654. doi: 10.1128/IAI.73.5.2644-2654.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Malik M, Bakshi CS, McCabe K, Catlett SV, Shah A, Singh R, Jackson PL, Gaggar A, Metzger DW, Melendez JA, Blalock JE, Sellati TJ. 2007. Matrix metalloproteinase 9 activity enhances host susceptibility to pulmonary infection with type A and B strains of Francisella tularensis. J Immunol 178:1013–1020. doi: 10.4049/jimmunol.178.2.1013. [DOI] [PubMed] [Google Scholar]
- 38.Kirimanjeswara GS, Olmos S, Bakshi CS, Metzger DW. 2008. Humoral and cell-mediated immunity to the intracellular pathogen Francisella tularensis. Immunol Rev 225:244–255. doi: 10.1111/j.1600-065X.2008.00689.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nakamura T, Abu-Dahab R, Menger MD, Schafer U, Vollmar B, Wada H, Lehr CM, Schafers HJ. 2005. Depletion of alveolar macrophages by clodronate-liposomes aggravates ischemia-reperfusion injury of the lung. J Heart Lung Transplant 24:38–45. doi: 10.1016/j.healun.2003.10.007. [DOI] [PubMed] [Google Scholar]
- 40.Hand WL, Cantey JR. 1974. Antibacterial mechanisms of the lower respiratory tract. I. Immunoglobulin synthesis and secretion. J Clin Invest 53:354–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Murphy BR, Nelson DL, Wright PF, Tierney EL, Phelan MA, Chanock RM. 1982. Secretory and systemic immunological response in children infected with live attenuated influenza A virus vaccines. Infect Immun 36:1102–1108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Burlington DB, Clements ML, Meiklejohn G, Phelan M, Murphy BR. 1983. Hemagglutinin-specific antibody responses in immunoglobulin G, A, and M isotypes as measured by enzyme-linked immunosorbent assay after primary or secondary infection of humans with influenza A virus. Infect Immun 41:540–545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ito R, Ozaki YA, Yoshikawa T, Hasegawa H, Sato Y, Suzuki Y, Inoue R, Morishima T, Kondo N, Sata T, Kurata T, Tamura S. 2003. Roles of anti-hemagglutinin IgA and IgG antibodies in different sites of the respiratory tract of vaccinated mice in preventing lethal influenza pneumonia. Vaccine 21:2362–2371. doi: 10.1016/S0264-410X(03)00078-1. [DOI] [PubMed] [Google Scholar]
- 44.Huber VC, Lynch JM, Bucher DJ, Le J, Metzger DW. 2001. Fc receptor-mediated phagocytosis makes a significant contribution to clearance of influenza virus infections. J Immunol 166:7381–7388. doi: 10.4049/jimmunol.166.12.7381. [DOI] [PubMed] [Google Scholar]
- 45.Wiertsema SP, Veenhoven RH, Walraven V, Uiterwaal CS, Schilder AG, Rijkers GT, Sanders EA. 2006. Pneumococcal vaccine efficacy for mucosal pneumococcal infections depends on Fcgamma receptor IIa polymorphism. Vaccine 24:792–797. doi: 10.1016/j.vaccine.2005.08.029. [DOI] [PubMed] [Google Scholar]
- 46.van oud Alblas AB, van Furth R. 1979. Origin, kinetics, and characteristics of pulmonary macrophages in the normal steady state. J Exp Med 149:1504–1518. doi: 10.1084/jem.149.6.1504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Green GM, Kass EH. 1964. The role of the alveolar macrophage in the clearance of bacteria from the lung. J Exp Med 119:167–176. doi: 10.1084/jem.119.1.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bosio CM, Dow SW. 2005. Francisella tularensis induces aberrant activation of pulmonary dendritic cells. J Immunol 175:6792–6801. doi: 10.4049/jimmunol.175.10.6792. [DOI] [PubMed] [Google Scholar]
- 49.Bosio CM, Bielefeldt-Ohmann H, Belisle JT. 2007. Active suppression of the pulmonary immune response by Francisella tularensis Schu4. J Immunol 178:4538–4547. doi: 10.4049/jimmunol.178.7.4538. [DOI] [PubMed] [Google Scholar]
- 50.Chase JC, Celli J, Bosio CM. 2009. Direct and indirect impairment of human dendritic cell function by virulent Francisella tularensis Schu S4. Infect Immun 77:180–195. doi: 10.1128/IAI.00879-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Steiner DJ, Furuya Y, Jordan MB, Metzger DW. 2017. Protective role for macrophages in respiratory Francisella tularensis infection. Infect Immun 85:e00064-. doi: 10.1128/iai.00064-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Skyberg JA, Rollins MF, Samuel JW, Sutherland MD, Belisle JT, Pascual DW. 2013. Interleukin-17 protects against the Francisella tularensis live vaccine strain but not against a virulent F. tularensis type A strain. Infect Immun 81:3099–3105. doi: 10.1128/IAI.00203-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kingry LC, Troyer RM, Marlenee NL, Bielefeldt-Ohmann H, Bowen RA, Schenkel AR, Dow SW, Slayden RA. 2011. Genetic identification of unique immunological responses in mice infected with virulent and attenuated Francisella tularensis. Microbes Infect 13:261–275. doi: 10.1016/j.micinf.2010.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Forestal CA, Malik M, Catlett SV, Savitt AG, Benach JL, Sellati TJ, Furie MB. 2007. Francisella tularensis has a significant extracellular phase in infected mice. J Infect Dis 196:134–137. doi: 10.1086/518611. [DOI] [PubMed] [Google Scholar]
- 55.Yu JJ, Raulie EK, Murthy AK, Guentzel MN, Klose KE, Arulanandam BP. 2008. The presence of infectious extracellular Francisella tularensis subsp. novicida in murine plasma after pulmonary challenge. Eur J Clin Microbiol Infect Dis 27:323–325. doi: 10.1007/s10096-007-0434-x. [DOI] [PubMed] [Google Scholar]
- 56.Mircescu MM, Lipuma L, van Rooijen N, Pamer EG, Hohl TM. 2009. Essential role for neutrophils but not alveolar macrophages at early time points following Aspergillus fumigatus infection. J Infect Dis 200:647–656. doi: 10.1086/600380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Beck-Schimmer B, Schwendener R, Pasch T, Reyes L, Booy C, Schimmer RC. 2005. Alveolar macrophages regulate neutrophil recruitment in endotoxin-induced lung injury. Respir Res 6:61. doi: 10.1186/1465-9921-6-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lofgren S, Tarnvik A, Bloom GD, Sjoberg W. 1983. Phagocytosis and killing of Francisella tularensis by human polymorphonuclear leukocytes. Infect Immun 39:715–720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lofgren S, Tarnvik A, Carlsson J. 1980. Demonstration of opsonizing antibodies to Francisella tularensis by leukocyte chemiluminescence. Infect Immun 29:329–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.McCaffrey RL, Allen LA. 2006. Francisella tularensis LVS evades killing by human neutrophils via inhibition of the respiratory burst and phagosome escape. J Leukoc Biol 80:1224–1230. doi: 10.1189/jlb.0406287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sjostedt A, Conlan JW, North RJ. 1994. Neutrophils are critical for host defense against primary infection with the facultative intracellular bacterium Francisella tularensis in mice and participate in defense against reinfection. Infect Immun 62:2779–2783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Conlan JW, KuoLee R, Shen H, Webb A. 2002. Different host defences are required to protect mice from primary systemic vs pulmonary infection with the facultative intracellular bacterial pathogen, Francisella tularensis LVS. Microb Pathog 32:127–134. doi: 10.1006/mpat.2001.0489. [DOI] [PubMed] [Google Scholar]
- 63.Lilius EM, Marnila P. 1992. Photon emission of phagocytes in relation to stress and disease. Experientia 48:1082–1091. doi: 10.1007/BF01947995. [DOI] [PubMed] [Google Scholar]
- 64.Periasamy S, Avram D, McCabe A, MacNamara KC, Sellati TJ, Harton JA. 2016. An immature myeloid/myeloid-suppressor cell response associated with necrotizing inflammation mediates lethal pulmonary tularemia. PLoS Pathog 12:e1005517. doi: 10.1371/journal.ppat.1005517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Clemens DL, Horwitz MA. 2007. Uptake and intracellular fate of Francisella tularensis in human macrophages. Ann N Y Acad Sci 1105:160–186. [DOI] [PubMed] [Google Scholar]
- 66.Thepen T, Van Rooijen N, Kraal G.. 1989. Alveolar macrophage elimination in vivo is associated with an increase in pulmonary immune response in mice. J Exp Med 170:499–509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Knapp S, Leemans JC, Florquin S, Branger J, Maris NA, Pater J, van Rooijen N, van der Poll T. 2003. Alveolar macrophages have a protective antiinflammatory role during murine pneumococcal pneumonia. Am J Respir Crit Care Med 167:171–179. [DOI] [PubMed] [Google Scholar]
- 68.Bang BR, Chun E, Shim EJ, Lee HS, Lee SY, Cho SH, Min KU, Kim YY, Park HW. 2011. Alveolar macrophages modulate allergic inflammation in a murine model of asthma. Exp Mol Med 43:275–280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Balhara J, Gounni AS. 2012. The alveolar macrophages in asthma: a double-edged sword. Mucosal Immunol 5:605. [DOI] [PubMed] [Google Scholar]
- 70.Khalil N, Bereznay O, Sporn M, Greenberg AH. 1989. Macrophage production of transforming growth factor beta and fibroblast collagen synthesis in chronic pulmonary inflammation. J Exp Med 170:727–737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Vignola AM, Chanez P, Chiappara G, Merendino A, Zinnanti E, Bousquet J, Bellia V, Bonsignore G. 1996. Release of transforming growth factor-beta (TGF-beta) and fibronectin by alveolar macrophages in airway diseases. Clin Exp Immunol 106:114–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Letterio JJ, Roberts AB. 1998. Regulation of immune responses by TGF-beta. Annu Rev Immunol 16:137–161. [DOI] [PubMed] [Google Scholar]
- 73.Brandes ME, Mai UE, Ohura K, Wahl SM. 1991. Type I transforming growth factor-beta receptors on neutrophils mediate chemotaxis to transforming growth factor-beta. J Immunol 147:1600–1606. [PubMed] [Google Scholar]
- 74.De Rose V, Trentin L, Crivellari MT, Cipriani A, Gialdroni G, Pozzi E, Folco G, Semenzato G. 1997. Release of prostaglandin E2 and leukotriene B4 by alveolar macrophages from patients with sarcoidosis. Thorax 52:76–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Wiemer AJ, Hegde S, Gumperz JE, Huttenlocher A. 2011. A live imaging cell motility screen identifies PGE2 as a T cell stop signal antagonist. J Immunol 187:3663–3670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Kalinski P. 2012. Regulation of immune responses by prostaglandin E2. J Immunol 188:21–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Shishikura K, Horiuchi T, Sakata N, Trinh DA, Shirakawa R, Kimura T, Asada Y, Horiuchi H. 2016. Prostaglandin E2 inhibits neutrophil extracellular trap formation through production of cyclic AMP. Br J Pharmacol 173:319–331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.National Research Council. 2011. Guide for the care and use of laboratory animals, 8th ed National Academies Press, Washington, DC. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.