Abstract
Background:
Incidental gallbladder carcinoma (IGBC) is rare cancer diagnosed during or after cholecystectomy done for benign gallbladder disease. The concern whether routine histopathological examination is needed for all cholecystectomy specimens still remains debatable.
Materials and Methods:
Twenty patients diagnosed with IGBC over a period of 2 years were retrospectively reviewed. Clinical details including clinical presentation, preoperative ultrasound (USG) findings, and macroscopic features were retrieved. Diagnosis of IGBC was confirmed on microscopic examination, and staging was done using the tumor node metastasis staging system.
Results:
Of the 4800 cholecystectomy specimens retrieved, diagnosis of IGBC was rendered in twenty cases (0.41%). Mean patient age was 50.65 years with a female preponderance. Preoperative USG detected an increase in wall thickness in six cases (30%) in contrast to gross examination which revealed the same in 55% (11/20) cases. Mucosal ulceration was observed in two cases (10%) of IGBC and seven cases (35%) did not reveal any preoperative or macroscopic findings suggestive of malignancy. Associated cholelithiasis was observed in 14 cases. Final diagnosis of IGBC was made on histomorphological assessment with tumor cells infiltrating the lamina propria in three cases (pT1b), muscularis propria in 15 cases (pT1b), and serosa in the remaining 2 cases (pT2).
Conclusion:
IGBC is a clinical masquerader which often evades the eye of a radiologist and comes as pathological surprise. Histopathological examination of cholecystectomy specimens remains the gold standard for the detection of this occult, yet notorious malignancy and assessment of the depth of invasion in IGBC guide further management.
Keywords: Histopathology, incidental gallbladder carcinoma, radiology
Introduction
Gallbladder carcinoma (GBC) ranks fifth among the gastrointestinal carcinomas and is the most common cancer of the biliary tract.[1] According to the Indian cancer registry data, incidence of GBC is 0.8%–1%. While New Delhi and Bhopal are the leading states, lowest incidence is seen in Chennai.[2] Risk factors include cholelithiasis, calcified gallbladder wall, adenomatous polyp, obesity, estrogen, choledochal cyst, and chemical carcinogens.[3] Of these, gallstones are a well-established risk factor associated with the development of GBCs in 75%–90% of cases.[4] Incidental gallbladder carcinoma (IGBC) is defined as GBC diagnosed histopathologically after cholecystectomy done for benign gallbladder disease. It is also known as occult/in apparent/missed GBCs.[2] Most of these patients do not have a radiological or intraoperative suspicion for malignancy.[5,6]
The concern whether routine histopathological examination is needed for all cholecystectomy specimens done for benign gallbladder diseases is still debatable. The Royal College of Pathologists suggests a histopathological examination of all cholecystectomy specimens as IGBC can be easily missed out.[7] However, few authors are of the view that histopathology is not needed for all surgically resected benign gallbladders as the incidence of IGBC is low and many of the cases present at an early stage with simple cholecystectomy being the optimal treatment.[5,8] The present study highlights the clinicopathological features including clinical features, preoperative imaging, and postoperative gross examination in patients of IGBC. We further analyze the need for histopathological evaluation in surgically resected gallbladders.
Materials and Methods
The archives of Department of Histopathology were retrospectively reviewed from July 2014 to June 2016. Of the 29,482 cases received, cholecystectomy specimens with a clinical diagnosis of benign gallbladder disease were included in the study. Both laparoscopic and open cholecystectomy specimens were included in the study. The excised specimen was fixed in 10% neutral buffered formalin and sent for histopathological examination. Gallbladder wall more than 3 mm was considered to be thickened. Diagnosis of IGBC was confirmed on hematoxylin- and eosin-stained, formalin-fixed, paraffin-embedded sections, and staging was done using the International Union Against Cancer (Union for International Cancer Control) tumor node metastasis (TNM) staging system. The medical records and clinical details of diagnosed cases of IGBC including demographic data, clinical presentation, preoperative imaging findings on computed tomography (CT) and/or ultrasound (USG), and macroscopic features were then retrospectively reviewed.
Results
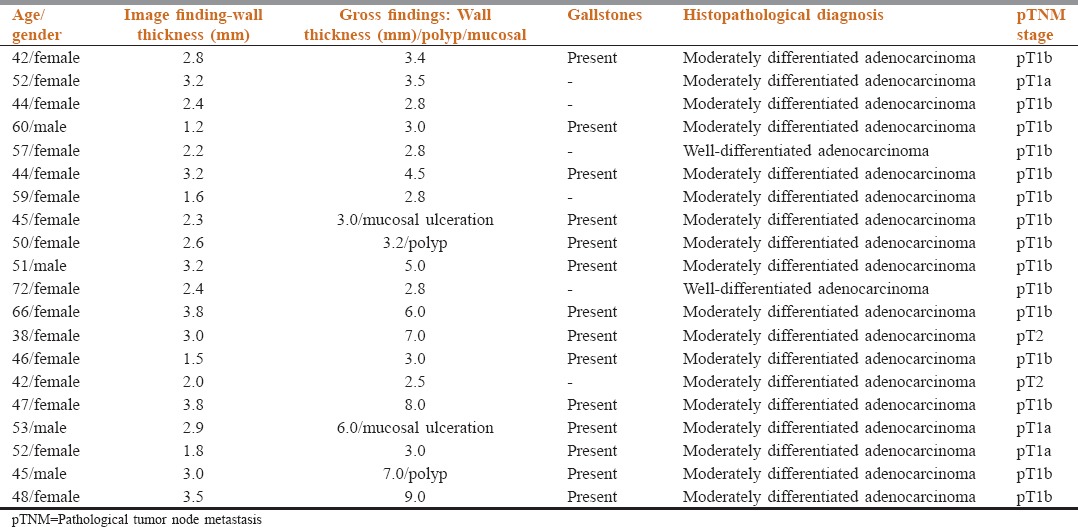
Out of 29,482 cases received in the department over a period of 2 years, 4800 cholecystectomy specimens without any preoperative suspicion of malignancy were found. The mean patient age at the time of surgery was 40.2 years (range 20–74 years). There were 1440 (30%) males and 3360 (70%) females with a female:male ratio of 2.3. Most common presenting symptom was pain in the right hypochondriac region seen in 89% of the patients followed by nausea and vomiting (6%) and epigastric pain (3%). Chronic calculous cholecystitis was the most frequent disease seen in 3765 patients (78.43%) followed by chronic acalculous cholecystitis in 960 patients (20%), xanthogranulomatous cholecystitis in 40 (0.83%), mucocele in 10 (0.20%), adenomyomatosis in 04 (0.08%), and a single case of cholesterol polyp. There were twenty cases (0.41%) diagnosed as IGBC. These cases were further studied based on preoperative imaging findings, macroscopic findings, and pathological TNM staging as shown in Table 1. It was observed that out of the twenty cases of IGBC, 80% (16/20) were females while 20% (4/20) were males. The age group affected was 38–72 years (mean – 50.65 years). Preoperative USG detected an increase in wall thickness in 6 cases (30%). No intraluminal mass lesion was detected in any of the cases. Gross inspection of the majority specimens revealed thickening of gallbladder wall in 55% (11/20) cases followed by mucosal ulceration in two cases (10%). Seven cases (35%) did not show any preoperative or macroscopic findings suggestive of malignancy. Majority of the cases of IGBC (14/20) were associated with gallstones. On microscopic examination, all cases showed features of adenocarcinoma, in which tumor cells were arranged in glands and papillae. Tumor cells were round to cuboidal with moderate eosinophilic cytoplasm and a central pleomorphic vesicular nucleus with 1–2 nucleoli. Mitosis including atypical forms was seen. Lymphovascular invasion and perineural invasion were seen in 14 cases and 2 cases, respectively. Tumor cells were seen infiltrating the lamina propria in 3 cases (pT1b), muscularis propria in 15 cases (pT1b), and serosa in the remaining 2 cases (pT2).
Table 1.
Clinicopathological characteristics of incidental gallbladder carcinomas
Discussion
Incidental GBCs are defined as carcinomas of gallbladder diagnosed during or after cholecystectomy done for benign diseases of gallbladder. The incidence of IGBC is reported to be 0.2%–2.1%.[4,9,10,11] In our study, it was found to be 0.41%. It was more commonly seen in females and in the elderly age group which was in concordance with the previous literature.[12,13] Cholelithiasis is a well-known risk factor for gallbladder cancers.[5,12,13,14] We found the presence of gallstones in 70% of IGBCs. Waghmare and Kamat reported a higher (85%) association of gallstones with IGBC.[5] Difference in rate of incidence of gallbladder stones and GBC among various studies might be due to different ethnic groups, race, and religion. Further, gallstones cause mucosal irritation and chronic inflammation setting a stage for the development of dysplasia and subsequently carcinoma. This transformation requires many years to occur, most cases of GBC are seen in the elderly.[12,15]
Various studies in the past concluded that preoperative imaging and/or macroscopic examination is abnormal in cases of invasive carcinoma and thereby recommended a selective policy rather than a routine histopathological examination of cholecystectomy specimens.[15,16] However, in our study, a total of 14 cases of IGBC were misdiagnosed as benign lesions on USG. Of these, USG detected wall thickening in only 6 cases of IGBC in comparison to 11 cases on gross examination. Further 9 cases revealed normal preoperative imaging studies and did not show any abnormality on gross examination. Thus, preoperative USG was not useful in raising a high degree of clinical suspicion of malignancy. Similarly, gross examination did not reveal significant findings in all cases of IGBC in our study. In a study conducted at the Johns Hopkins Hospital, preoperative radiology failed to pick up 50% of gallbladder tumors.[4] Further, since IGBC is known to be early stage cancers (pT1a and pT1b), many authors propose simple cholecystectomy for the treatment of these lesions.[2,17] However, in contrast, our study revealed two cases of IGBC at pT2. For Tis and pT1a tumors, simple cholecystectomy is sufficient with 5-year survival rate being almost 100%. However, for pT1b tumors, beyond radical re-resection is recommended. For pT2 tumors, the 5-year survival rate improves from 20% to 70% if simple cholecystectomy is followed by radical cholecystectomy after the diagnosis of IGBC.[2] Therefore, histopathology should be done for all surgically resected gallbladders as it is the only tool which can detect IGBC accurately which improves patient's survival as compared to GBC.
The Royal College of Pathologists suggests a histopathological examination of all cholecystectomy specimens as normal gross morphological features may be misleading.[7] However, few authors have observed pre- and intra-operative features to be useful in raising suspicion for malignancy. They are of the view that selective histological examination should be carried out on the cholecystectomy specimens received with clinically benign diagnosis.[6,8,16,18,19] The present study highlights the fact that it is difficult to suspect malignancy in all the specimens based on imaging or macroscopic features. It is important to assess the depth of invasion in IGBC as surgery depends on the staging.[2]
Conclusion
To conclude, gallbladder cancers are one of the common tumors of gastrointestinal tracts and are known to have a poor prognosis. Incidence of IGBC is low and is usually early stage cancers with a better 5-year survival rate as compared to GBC. Radiology and macroscopic findings usually fail to raise suspicion of malignancy (IGBC) in cholecystectomy specimens. Thus, histopathological examination of cholecystectomy specimens is the gold standard for the detection of occult malignancy. In a developing country where resources are limited, selective sampling of resected gallbladders can be cost-effective. However, as GBC has a poor prognosis and tends to have rapid progression selective sampling is not justifiable in cholecystectomy specimens. Therefore, the authors strongly recommend histological assessment of all cholecystectomy specimens regardless of the radiological diagnosis or macroscopic findings.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Solan MJ, Jackson BT. Carcinoma of the gall-bladder. A clinical appraisal and review of 57 cases. Br J Surg. 1971;58:593–7. doi: 10.1002/bjs.1800580814. [DOI] [PubMed] [Google Scholar]
- 2.Rathanaswamy S, Misra S, Kumar V, Chintamani N, Pogal J, Agarwal A, et al. Incidentally detected gallbladder cancer – The controversies and algorithmic approach to management. Indian J Surg. 2012;74:248–54. doi: 10.1007/s12262-012-0592-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ghimire P, Yogi N, Shrestha BB. Incidence of incidental carcinoma gall bladder in cases of routine cholecystectomy. Kathmandu Univ Med J (KUMJ) 2011;9:3–6. doi: 10.3126/kumj.v9i2.6278. [DOI] [PubMed] [Google Scholar]
- 4.Shih SP, Schulick RD, Cameron JL, Lillemoe KD, Pitt HA, Choti MA, et al. Gallbladder cancer: The role of laparoscopy and radical resection. Ann Surg. 2007;245:893–901. doi: 10.1097/SLA.0b013e31806beec2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Waghmare RS, Kamat RN. Incidental gall bladder carcinoma in patients undergoing cholecystectomy: A report of 7 cases. J Assoc Physicians India. 2014;62:793–6. [PubMed] [Google Scholar]
- 6.Mittal R, Jesudason MR, Nayak S. Selective histopathology in cholecystectomy for gallstone disease. Indian J Gastroenterol. 2010;29:211. doi: 10.1007/s12664-010-0056-6. [DOI] [PubMed] [Google Scholar]
- 7.2nd ed. London, UK: Royal College of Pathologists; 2005. Royal College of Pathologists. Histopathology and Cytopathology of Limited or No Clinical Value, in Report of Working Group of the Royal College of Pathologists. [Google Scholar]
- 8.Darmas B, Mahmud S, Abbas A, Baker AL. Is there any justification for the routine histological examination of straightforward cholecystectomy specimens? Ann R Coll Surg Engl. 2007;89:238–41. doi: 10.1308/003588407X168361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jemal A, Siegel R, Ward E, Murray T, Xu J, Smigal C, et al. Cancer statistics, 2006. CA Cancer J Clin. 2006;56:106–30. doi: 10.3322/canjclin.56.2.106. [DOI] [PubMed] [Google Scholar]
- 10.Butte JM, Matsuo K, Gönen M, D’Angelica MI, Waugh E, Allen PJ, et al. Gallbladder cancer: Differences in presentation, surgical treatment, and survival in patients treated at centers in three countries. J Am Coll Surg. 2011;212:50–61. doi: 10.1016/j.jamcollsurg.2010.09.009. [DOI] [PubMed] [Google Scholar]
- 11.Zhang WJ, Xu GF, Zou XP, Wang WB, Yu JC, Wu GZ, et al. Incidental gallbladder carcinoma diagnosed during or after laparoscopic cholecystectomy. World J Surg. 2009;33:2651–6. doi: 10.1007/s00268-009-0218-9. [DOI] [PubMed] [Google Scholar]
- 12.Ahn Y, Park CS, Hwang S, Jang HJ, Choi KM, Lee SG. Incidental gallbladder cancer after routine cholecystectomy: When should we suspect it preoperatively and what are predictors of patient survival? Ann Surg Treat Res. 2016;90:131–8. doi: 10.4174/astr.2016.90.3.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Munshi S, Pal S, Ray D, Sarkar N, Chowdhury D. Incidental gallbladder carcinoma in patients undergoing cholecystectomy for cholelithiasis; a clinicopathological study. J Surg Arts. 2015;8:41–7. [Google Scholar]
- 14.Genc V, Kirimker EO, Akyol C, Koccay AT, Korabork A, Tuzuner A, et al. Incidental gall bladder cancer diagnosed during or after laproscopic cholecystectomy in members of the Turkish population with gall stone disease. Turk J Gastroenterol. 2011;22:513–6. doi: 10.4318/tjg.2011.0250. [DOI] [PubMed] [Google Scholar]
- 15.Talreja V, Ali A, Khawaja R, Rani K, Samnani SS, Farid FN. Surgically resected gall bladder: Is histopathology needed for all? Surg Res Pract 2016. 2016 doi: 10.1155/2016/9319147. 9319147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dix FP, Bruce IA, Krypcyzk A, Ravi S. A selective approach to histopathology of the gallbladder is justifiable. Surgeon. 2003;1:233–5. doi: 10.1016/s1479-666x(03)80023-9. [DOI] [PubMed] [Google Scholar]
- 17.Kallianpur AA, Gupta N, Vinod N, Rakesh G, Samra SS, Goyal S. Management of incidentally detected gallbladder carcinomas in a high prevalence area of gallbladder cancer. Trop Gastroenterol. 2014;35:39–43. [PubMed] [Google Scholar]
- 18.Bazoua G, Hamza N, Lazim T. Do we need histology for a normal-looking gallbladder? Surgeon. 2003;1:233–5. doi: 10.1007/s00534-007-1225-6. [DOI] [PubMed] [Google Scholar]
- 19.Bisgaard T, Hansen BF, Lassen AH, Rosenberg J. Histological examination of the gallbladder after cholecystectomy. Ugeskr Laeger. 2001;163:5025–8. [PubMed] [Google Scholar]


