Abstract
Introduction:
One of the ovarian carcinogenesis theories was the presence of premalignant cells in the epithelium of the fallopian tube. Therefore, the prophylactic salpingectomy during benign gynecological surgery is now expected as the attempt to reduce the ovarian cancer incidence. We studied the effect of prophylactic bilateral salpingectomy (PBS) in reducing the ovarian cancer incidence.
Methods:
This evidence-based report resulted from critical appraisal of 5 articles. It is aimed to answer our clinical question, can bilateral prophylactic salpingectomy reduce the incidence of ovarian cancer among women underwent hysterectomy for benign condition or permanent contraception surgery? The search was conducted on the Cochrane Library®, PubMed®, and Embase® using keywords of “prophylactic salpingectomy,” and “ovarian cancer incidence.” Reference lists of relevant articles were searched for other possibly relevant articles.
Results:
Five studies were included in our appraisal. The incidence of ovarian cancer among women underwent prophylactic salpingectomy is lower compared to women who were not underwent any intervention (2.2% to 13% and 4.75% to 24.4%). The salpingectomy may reduce 29.2% to 64% of ovarian cancer incidence. No significant effect of PBS to ovarian function, quality of life, sexuality, surgery duration, and its cost-effective profile were also found throughout our literature study.
Conclusion:
PBS is suggested to be performed for women during benign gynecological surgery as a primary preventive strategy of ovarian cancer. PBS is a cost-effective procedure, risk-reducing for ovarian cancer and has no significant effect to the ovarian function.
Keywords: Ovarian cancer, prophylactic salpingectomy
Introduction
The global prevalence of ovarian cancer is 22.6/100.000 women. The 5-year survival rate ranges from approximately 30%–50%.[1] Ovarian cancer is one of lethal malignancies, approximately 14,000 deaths from the disease expected in the United States in 2013. Most cases are diagnosed at an advanced stage and no reliable methods to prevent the disease.[2] One of the ovarian carcinogenesis theories was the presence of premalignant cells in the epithelium of the fallopian tube. The precursor of most ovarian high-grade serous carcinomas and also low-grade serous tumors may originate in the fallopian tube.[3] This increase the gynecologists’ awareness regarding the role of fallopian tube in the development of epithelial ovarian cancer (EOC).[4]
Prophylactic bilateral salpingectomy (PBS) is expected to be associated with reductions in the risks of ovarian, fallopian tube, and breast carcinoma. However, a number of debatable issues, i.e., regarding the timing of the procedure, nononcologic morbidity, and the safety of menopausal hormonal therapy remain unresolved.[5] Therefore, the prophylactic salpingectomy is being studied by many authors to determine its effectivity in reducing the ovarian cancer.[6] In addition, The American Congress of Obstetricians and Gynecologists recommends the surgeon and patient should discuss the benefits of the removal of salpingectomy during a hysterectomy in women at population risk of ovarian cancer.[7] Other gynecological boards already declared the beneficial impact of PBS, however, no clear statement that PBS should be performed.[8] This critical review aims to study the risk-reducing potencies of PBS for ovarian cancer.
Case Illustration
Mrs. 41-year-old, P2A1, underwent a laparotomy total hysterectomy due to adenomyosis. She suffered from abnormal uterine bleeding and dysmenorrhea VAS 3 for 4 months before admission. She felt palpable mass on the lower abdomen and had history of hospitalization for blood transfusion due to anemia of blood loss (Hemoglobin level 6.8 g/dl). On ultrasound examination, we revealed enlarged and globular uterus, diffuse adenomyosis with the diameter of 52 mm. During hysterectomy, the Obstetrics and Gynecologist (OB-GYN) performed bilateral salpingectomy to reduce the risk of having ovarian cancer.
Clinical question
P (patients): Women underwent hysterectomy for benign condition or permanent contraception surgery
I (intervention): Bilateral prophylactic salpingectomy
C (comparison): No prophylactic salpingectomy
O (objective): Ovarian cancer incidence.
Among women underwent hysterectomy for benign condition or permanent contraception surgery, can bilateral prophylactic salpingectomy reduce the incidence of ovarian cancer?
Methods
Search strategy
We conducted the literature searching on July 27th, 2017 on the Cochrane Library®, Embase ® PubMed® with the combination of keywords of “prophylactic salpingectomy,” and “ovarian cancer.” Search focused on articles in clinical trial or case–control design. Reference lists of relevant articles were searched for other possibly relevant trials [Figure 1]. Studies without ovarian cancer incidence stated in the studies’ outcome were not included in this study.
Figure 1.
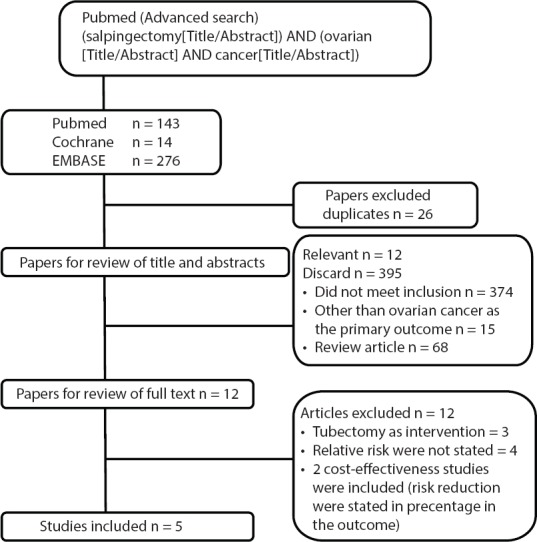
Searching flow
Selection
First selection was done by screening the study title and abstract [appendix Figure 1] for an overview of the selection of articles]. Five articles were available as full text and included in our analysis.
Critical appraisal
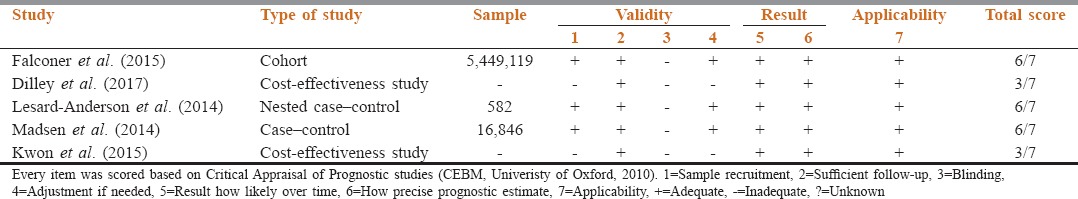
Appraisal of five studies including two cost-effectiveness studies and 3 population-based case–control studies, involving women underwent hysterectomy for benign condition or tubal sterilization were conducted finding at ovarian cancer incidence among they who underwent prophylactic salpingectomy and they who were not performed any intervention. The quality of study was evaluated using appraisal form developed by Center of Evidence-Based Medicine, University of Oxford, available from http://www.cebm.org.
Results
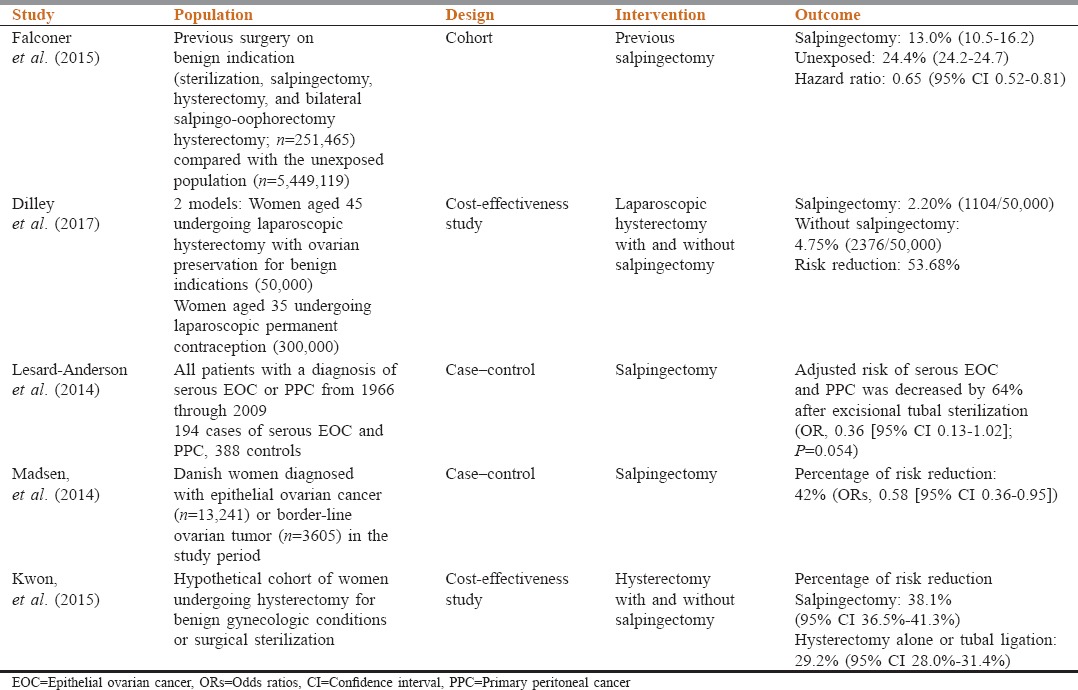
We included five studies in our appraisal. Two cost-effectiveness studies were included due to the statement of risk reduction percentage of ovarian cancer stated in the outcome of their studies [Table 1]. From two studies, the incidence of ovarian cancer among women underwent prophylactic or opportunistic salpingectomy was lower compared to they who were not underwent any intervention (2.2% to 13% and 4.75% to 24.4%). The salpingectomy might reduce 29.2% to 64% of ovarian cancer incidence.
Table 1.
Critical appraisal summary based on five published studies
Dilley et al. calculated the cost saving and ovarian cancer incidence among two population models: (1) 50,000 women aged 45 undergoing laparoscopic hysterectomy and (2) 300,000 women aged undergoing laparoscopic permanent contraception. The incidence of ovarian cancer at the age of 65 of these populations was, respectively, 2.20% (1104/50,000) among they who underwent prophylactic salpingectomy and 4.75% (2376/50,000) among they who not underwent PBS. Ovarian cancer rates were estimated based on lifetime population risk of ovarian cancer of 1.3%, and risk reduction data from a large population-based cohort conducted by Falconer et al.[9] They stated that opportunistic salpingectomy may save $23.9 million in health-care budget.[10]
Kwon et al. predicted that salpingectomy would reduce ovarian cancer risk by 38.1% (95% confidence interval [CI] 36.5-41.3%) and 29.2% (95% CI 28.0-31.4%) compared with hysterectomy alone or tubal ligation, respectively.[11] In addition, they also stated that salpingectomy with hysterectomy was less costly than hysterectomy alone or with bilateral salpingo-oophorectomy.[11]
In their population-based cohort study, Falconer et al. was clearly stated that salpingectomy might reduce ovarian cancer risk in the general population. The risk for ovarian cancer among women underwent salpingectomy was significantly lower compared with the unexposed population (hazard ratio [HR] = 0.65, 95% CI = 0.52–0.81).
In addition, bilateral salpingectomy was better than the unilateral procedure to prevent the incidence of ovarian cancer (HR = 0.35, 95% CI = 0.17–0.73, and 0.71, 95% CI = 0.56–0.91, respectively).[9]
Lessard-Anderson et al. studied the effects of excisional tubal sterilization on the risk of serous EOC or primary peritoneal cancer (PPC). Excisional tubal sterilization, i.e., complete salpingectomy, partial salpingectomy, and distal fimbriectomy was statistically lower the risk of serous EOC and PPC by 64% after (odds ratio [OR], 0.36 [95% CI, 0.13-1.02]; P = 0.054) compared with those without sterilization or with nonexcisional tubal sterilization. Tubal sterilization reduces the risk of EOC and PPC by 41%.[12]
Madsen et al. conducted the Denish nationwide register-based case–control study during 1982-2011. They found that bilateral salpingectomy reduced EOC risk by 42% (OR 0.58). Tubal ligation reduced overall EOC risk (OR 0.87), the strongest risk reductions associated with endometrioid cancer (OR 0.66) and EOC of “other” histology (OR 0.60). Interval 0.43–0.83).[13] All studies was summarized in Table 2.
Table 2.
Study characteristics
Discussion
Ovarian cancer incidence after prophylactic salpingectomy
The incidence of ovarian cancer among was, respectively, 2.2% to 13% and 4.75% to 24.4% among they who underwent prophylactic salpingectomy and they who were not underwent any intervention. The risk-reducing capability of prophylactic salpingectomy in our study was similar with latest meta-analysis performed by Yoon et al. They revealed the risk of incidence of ovarian cancer was lower 49% among the patients who underwent bilateral salpingectomy compared to the controls (OR: 0.51, 95% CI 0.35-0.75).[14] In our study, PBS may reduce 29.2% to 64% of ovarian cancer incidence. Three cohort studies appraised in our study had better appraisal score due to its clearly-stated sample recruitment, duration of follow-up, and risk-reducing parameters.
Opportunistic salpingectomy at the time of pelvic surgery for a benign condition develops as an option for primary prevention of high-grade serous cancer. It was based on the theory suggests that precursor lesions of high-grade serous cancer originate in the fallopian tube. The presumed precursor tubal lesion, localized at the fimbrial end of the fallopian tubes, is termed the serous tubal intraepithelial carcinoma.[8]
Other impact of prophylactic salpingectomy
Prophylactic salpingectomy probably has low effect to the ovarian function after surgery. It was proven by insignificant change anti-Mullerian Hormone levels three months after hysterectomy of and there were reported morbidities related to the procedure.[2] Findley et al., in their pilot randomized controlled trial revealed similar finding that PBS did not have any short-term negative effects on ovarian reserve.[15] The latest study conducted by Venturella et al. revealed that follicle-stimulating hormone, anti-Mullerian hormone, 3-dimensional antral follicle count, vascular index, flow index, and vascular flow index did not show different profile up to 35 years after surgery after prophylactic salpingectomy compared to the control group.[16]
Antosh et al. stated that PBS increases operating time by 11 min and blood loss by 6 ml.[17] However, it did not increase the complication rate of surgeries.[18] In Italia, PBS is already well-known among the Italian OBGYNs as the attempt to reduce ovarian cancer incidence.[19] In Austria, PBS is now widely performed during benign gynecologic surgery and cesarean section.[20] We need further research to know the knowledge and practice among OBGYNs regarding this issue. Among low-risk women undergoing pelvic surgery, PBS is a cost-effective strategy for decreasing ovarian cancer risk.[10] PBS also did not affect either on the general quality of life or sexuality.[21]
We suggest that removal of the fallopian tubes is an effective attempt to reduce the ovarian cancer risk in the general population. This was similar with the latest meta-analysis. Therefore, PBS should be considered for women who require hysterectomy with benign indications or sterilization procedures.[14] Due to its beneficiary effect, the patients should be counseled about the risks and benefits of both procedures based on the current available evidence.[22]
Conclusion
PBS is suggested to be performed for women during benign gynecological surgery as a primary preventive strategy of ovarian cancer. PBS is a cost-effective procedure that has risk-reducing profile has no significant effect to the ovarian function.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, et al. Cancer incidence and mortality worldwide: Sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136:E359–86. doi: 10.1002/ijc.29210. [DOI] [PubMed] [Google Scholar]
- 2.Tanner EJ, Long KC, Visvanathan K, Fader AN. Prophylactic salpingectomy in premenopausal women at low risk for ovarian cancer: Risk-reducing or risky? Fertil Steril. 2013;100:1530–1. doi: 10.1016/j.fertnstert.2013.09.039. [DOI] [PubMed] [Google Scholar]
- 3.Vang R, Shih IeM, Kurman RJ. Fallopian tube precursors of ovarian low- and high-grade serous neoplasms. Histopathology. 2013;62:44–58. doi: 10.1111/his.12046. [DOI] [PubMed] [Google Scholar]
- 4.Pölcher M, Hauptmann S, Fotopoulou C, Schmalfeldt B, Meinhold-Heerlein I, Mustea A, et al. Opportunistic salpingectomies for the prevention of a high-grade serous carcinoma: A statement by the Kommission Ovar of the AGO. Arch Gynecol Obstet. 2015;292:231–4. doi: 10.1007/s00404-015-3697-y. [DOI] [PubMed] [Google Scholar]
- 5.Greene MH, Mai PL, Schwartz PE. Does bilateral salpingectomy with ovarian retention warrant consideration as a temporary bridge to risk-reducing bilateral oophorectomy in BRCA1/2 mutation carriers. Am J Obstet Gynecol. 2011;204:19.e1–6. doi: 10.1016/j.ajog.2010.05.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Oliver Perez MR, Magriñá J, García AT, Jiménez Lopez JS. Prophylactic salpingectomy and prophylactic salpingoophorectomy for adnexal high-grade serous epithelial carcinoma: A reappraisal. Surg Oncol. 2015;24:335–44. doi: 10.1016/j.suronc.2015.09.008. [DOI] [PubMed] [Google Scholar]
- 7.Salpingectomy for ovarian cancer prevention. Committee Opinion No. 620. American College of Obstetricians and Gynecologists. Obstet Gynecol. 2015;125:279–81. doi: 10.1097/01.AOG.0000459871.88564.09. [DOI] [PubMed] [Google Scholar]
- 8.Ziętek A, Bogusiewicz M, Szumiło J, Rechberger T. Opportunistic salpingectomy for prevention of sporadic ovarian cancer – A jump from basic science to clinical practice? Ginekol Pol. 2016;87:467–72. doi: 10.5603/GP.2016.0027. [DOI] [PubMed] [Google Scholar]
- 9.Falconer H, Yin L, Grönberg H, Altman D. Ovarian cancer risk after salpingectomy: A nationwide population-based study. J Natl Cancer Inst. 2015;107:pii: dju410. doi: 10.1093/jnci/dju410. [DOI] [PubMed] [Google Scholar]
- 10.Dilley SE, Havrilesky LJ, Bakkum-Gamez J, Cohn DE, Michael Straughn J, Jr, Caughey AB, et al. Cost-effectiveness of opportunistic salpingectomy for ovarian cancer prevention. Gynecol Oncol. 2017;146:373–9. doi: 10.1016/j.ygyno.2017.05.034. [DOI] [PubMed] [Google Scholar]
- 11.Kwon JS, McAlpine JN, Hanley GE, Finlayson SJ, Cohen T, Miller DM, et al. Costs and benefits of opportunistic salpingectomy as an ovarian cancer prevention strategy. Obstet Gynecol. 2015;125:338–45. doi: 10.1097/AOG.0000000000000630. [DOI] [PubMed] [Google Scholar]
- 12.Lessard-Anderson CR, Handlogten KS, Molitor RJ, Dowdy SC, Cliby WA, Weaver AL, et al. Effect of tubal sterilization technique on risk of serous epithelial ovarian and primary peritoneal carcinoma. Gynecol Oncol. 2014;135:423–7. doi: 10.1016/j.ygyno.2014.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Madsen C, Baandrup L, Dehlendorff C, Kjaer SK. Tubal ligation and salpingectomy and the risk of epithelial ovarian cancer and borderline ovarian tumors: A nationwide case-control study. Acta Obstet Gynecol Scand. 2015;94:86–94. doi: 10.1111/aogs.12516. [DOI] [PubMed] [Google Scholar]
- 14.Yoon SH, Kim SN, Shim SH, Kang SB, Lee SJ. Bilateral salpingectomy can reduce the risk of ovarian cancer in the general population: A meta-analysis. Eur J Cancer. 2016;55:38–46. doi: 10.1016/j.ejca.2015.12.003. [DOI] [PubMed] [Google Scholar]
- 15.Findley AD, Siedhoff MT, Hobbs KA, Steege JF, Carey ET, McCall CA, et al. Short-term effects of salpingectomy during laparoscopic hysterectomy on ovarian reserve: a pilot randomized controlled trial. Fertil Steril. 2013;100:1704–8. doi: 10.1016/j.fertnstert.2013.07.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Venturella R, Lico D, Borelli M, Imbrogno MG, Cevenini G, Zupi E, et al. 3 to 5 Years later: Long-term effects of prophylactic bilateral salpingectomy on ovarian function. J Minim Invasive Gynecol. 2017;24:145–50. doi: 10.1016/j.jmig.2016.08.833. [DOI] [PubMed] [Google Scholar]
- 17.Antosh DD, High R, Brown HW, Oliphant SS, Abed H, Philip N, et al. Feasibility of prophylactic salpingectomy during vaginal hysterectomy. Am J Obstet Gynecol. 2017;217:605.e1–0000. doi: 10.1016/j.ajog.2017.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vorwergk J, Radosa MP, Nicolaus K, Baus N, Jimenez Cruz J, Rengsberger M, et al. Prophylactic bilateral salpingectomy (PBS) to reduce ovarian cancer risk incorporated in standard premenopausal hysterectomy: Complications and re-operation rate. J Cancer Res Clin Oncol. 2014;140:859–65. doi: 10.1007/s00432-014-1622-6. [DOI] [PubMed] [Google Scholar]
- 19.Venturella R, Rocca M, Lico D, Trapasso S, Di Cello A, Gizzo S, et al. Prophylactic bilateral salpingectomy for the prevention of ovarian cancers: What is happening in Italy? Eur J Cancer Prev. 2016;25:410–5. doi: 10.1097/CEJ.0000000000000191. [DOI] [PubMed] [Google Scholar]
- 20.Potz FL, Tomasch G, Polterauer S, Laky R, Marth C, Tamussino K, et al. Incidental (Prophylactic) salpingectomy at benign gynecologic surgery and cesarean section: A Survey of practice in Austria. Geburtshilfe Frauenheilkd. 2016;76:1325–9. doi: 10.1055/s-0042-116493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Skorupska KA, Miotła P, Kubik-Komar A, Rechberger E, Adamiak-Godlewska A, Rechberger T, et al. Are there any differences in quality of life and sexual functions after various types of hysterectomy - does prophylactic salpingectomy matter? Ginekol Pol. 2016;87:26–31. doi: 10.17772/gp/60554. [DOI] [PubMed] [Google Scholar]
- 22.Ely LK, Truong M. The role of opportunistic bilateral salpingectomy vs. tubal occlusion or ligation for ovarian cancer prophylaxis. J Minim Invasive Gynecol. 2017;24:371–8. doi: 10.1016/j.jmig.2017.01.001. [DOI] [PubMed] [Google Scholar]


