Abstract
Conflict in specific family systems (e.g., interparental, parent-child) has been implicated in the development of a host of adjustment problems in adolescence, but little is known about the impact of family conflict involving multiple family systems. Furthermore, questions remain about the effects of family conflict on symptoms of specific disorders and adjustment problems and the processes mediating these effects. The present study prospectively examines the impact of family conflict and emotional security about the family system on adolescent symptoms of specific disorders and adjustment problems, including the development of symptoms of anxiety, depression, conduct problems, and peer problems. Security in the family system was examined as a mediator of these relations. Participants included 295 mother-father-adolescent families (149 girls) participating across three annual time points (grades 7–9). Including auto-regressive controls for initial levels of emotional insecurity and multiple adjustment problems (T1), higher-order emotional insecurity about the family system (T2) mediated relations between T1 family conflict and T3 peer problems, anxiety, and depressive symptoms. Further analyses supported specific patterns of emotional security/insecurity (i.e., security, disengagement, preoccupation) as mediators between family conflict and specific domains of adolescent adjustment. Family conflict was thus found to prospectively predict the development of symptoms of multiple specific adjustment problems, including symptoms of depression, anxiety, conduct problems, and peer problems, by elevating in in adolescent’s emotional insecurity about the family system. The clinical implications of these findings are considered.
Keywords: Adolescence, Anxiety, Depression, Conduct Problems, Peer Problems, Emotional Security, Family Conflict
Conflict in the family has long been linked with children’s risk for the development of adjustment problems (e.g., Cummings & Davies, 2010). However, research has focused on relations between conflicts in specific family systems, for example, interparental (e.g., Davies & Cummings, 1994) or parent-child hostility (e.g., Patterson, 1982), and children’s adjustment, rather than considering the implications of conflict in the family as a whole. Concerns with the role of conflict in the family have been compartmentalized, with investigators focusing only on specific family systems (e.g., interparental or parent-child), thereby limiting the conceptualization of family conflict as a risk factor, contributing to the development of isolated areas of study of family conflict (e.g., only interparental or parent-child conflict, respectively). However, conflict may be difficult to confine to one specific dyad and may involve multiple family members and systems (i.e., both parents and children). Additionally, past research has typically examined relations with relatively broad-band indicators of adjustment problems, that is, internalizing and/or externalizing problems, rather the prediction of specific symptoms or problems (e.g., depression, peer problems). Focusing on the prediction of the symptoms of specific disorders or problems increases the potential for application to child clinical psychology theory and practice.
Accordingly, the present paper advances a broader assessment of conflict (i.e., family conflict), and relations with symptoms of specific disorders or problems (i.e., depression, anxiety, conduct problems, peer problems). We endeavor to advance a more holistic, family-wide and process-oriented perspective on relations between family conflict and symptoms of specific disorders, utilizing Emotional Security Theory as an explanatory mechanism (EST, Davies & Cummings, 1994). EST postulates that children’s adjustment is influenced by the extent to which they feel secure in the family system. EST also provides well-articulated conceptual models and theory-based approaches to assessment concerning children’s regulatory processes and patterns in the face of threats to their security (Cummings & Davies, 2010). Research has demonstrated relations between youth adjustment and emotional insecurity about interparental conflict (Cummings & Davies, 2010) and parent-child attachment insecurity (DeKlyen & Greenberg, 2008). However, EST extends the study of emotional security beyond specific dyadic relationships and posits that youth’s emotional security is a significant goal in relation to multiple family relationships (Cummings & Davies, 1996). In previous research employing the Security in the Family System (SIFS) scales, Forman and Davies (2005) demonstrated in a community sample that children’s emotional security in the context of the family as a whole was predictive of child adjustment beyond the assessment of emotional security in the context of specific family relations. Accordingly, our hypothesis, which we will test in the context of a three-wave longitudinal design, is that emotional insecurity in the family system, will mediate relations between family conflict and youth’s symptoms of multiple specific disorders and problems, including depression, anxiety, and conduct and peer problems.
EST posits that maintaining a sense of protection, safety, and security is a primary goal for children and adolescents (Davies, Harold, Goeke-Morey, & Cummings, 2002). Supporting the assessment of a higher-order construct of emotional security, EST posits that organizations of youth’s emotional, behavioral, and cognitive responses reflect their responses to maintain this security but also may contribute to risk for adjustment problems over time if insecurity about family relations persists (Cummings, Schermerhorn, Davies, Goeke-Morey, & Cummings, 2006; Davies, Sturge-Apple, Boscoe, & Cummings, 2014). Emotional security in the family may increase the risk for youth maladjustment by increasing their emotional and behavioral dysregulation as well as engendering negative representations of family relationships (Cummings & Davies, 1996). Also, the process of preserving emotional security in the face of family conflict requires considerable expenditures of psychological and physical resources, limiting capacities to pursue developmental goals and increasing risk for exhibiting psychological maladjustment (Davies et al., 2002).
Secure base notions are at the foundation of both EST and attachment theory (Cummings & Davies, 2010; Waters & Cummings, 2000). These notions are extended to other family relations by EST, so that multiple family relationships are seen as pertinent to youth’s emotional insecurity, calling attention to the family as a whole in contributing to children’s emotional security. With regard to stage salient tasks of adolescence, a secure base allows for adolescents to strike a balance between the need to develop autonomy while maintaining relatedness in the family system (Allen & Antonishak, 2008). Notably, although many studies of secure base processes have focused on younger children, Cummings et al. (2006) reported in a longitudinal study of a community sample that emotional insecurity about interparental conflict was a stronger predictor of adjustment problems in adolescence than in earlier childhood, consistent with the notion that older children may be more aware of the threats posed to emotional security by family conflict (Cummings & Davies, 2010).
Problems in emotional and behavioral dyregulation have been linked both with insecure attachment (Esbjorn, Bender, Reinholdt-Dunne, Munck, & Ollendick, 2012) and insecurity about interparental conflict, including demonstrations of effects on emotional and behavioral responses linked prospectively to externalizing and internalizing symptoms (e.g., Davies et al., 2002; Harold, Shelton, Goeke-Morey & Cummings, 2004). Based on a meta-analysis of attachment studies primarily concerned with samples examined in infancy and early childhood, including both community and clinical samples, Groh and colleagues (Groh, Roisman, van IJzendoorn, Bakermans-Kranenburg, & Fearon, 2012) reported small but significant associations between attachment insecurity and internalizing problems, with avoidant patterns most closely linked with internalizing disorders. In another meta-analysis, Colonnesi et al. (2011) reported links from early childhood to adolescence between insecure attachment and anxiety.
Moreover, consistent with attachment theory and research, the psychological significance of identifying specific patterns of emotional insecurity as potential mediators of adjustment is also emphasized, including secure, disengaged, and preoccupied patterns (Davies & Forman, 2002; Forman & Davies, 2005). In regard to these specific patterns, secure adolescents are expected to be able to rely on their parents for safety, security, and protection, with secure appraisals reducing adjustment problems. On the other hand, Forman and Davies (2005) posited that disengaged patterns reflected emotional disengagement from social relations and a downplaying of the significance of the family, and found that this pattern was linked with increased risk for externalizing symptoms. By comparison, the preoccupied pattern, hypothesized as indicative of high levels of worrying and vigilance about stressful events in the family, was found to be associated with risk for the development of internalizing symptoms.
With regard to outcomes assessed in the present study, anxiety and depression share common etiologies (e.g., Hankin, Abramson, Miller & Haeffel, 2004), and are typically found to be co-morbid (see reviews in Gallerani, Garber, & Martin, 2010; Garber & Weersing, 2010). These relations are supported by an extensive literature including studies based on both community and clinical samples (Epkins & Heckler, 2011). However, although family discord has been linked with the etiology of adolescent depression (see meta-analysis by Kane & Garber, 2004), few prospective studies have been conducted; relations between family conflict and anxiety symptoms are little explored (Epkins & Heckler, 2011). According to EST (Davies et al, 2002) and attachment theory (Bowlby, 1973), threats to emotional insecurity activate emotional reactions of fear and anxiety in the service of the goal of acting to regain security, which, if persisting over time, may contribute to the risk for internalizing problems, including symptoms of anxiety. Cognitive reactions associated with potential loss and negative expectations and cognitive schema regarding future family functioning and stability may further contribute to the development of depressive symptoms (see also Cummings & Cicchetti, 1990). Common pathways from family conflict through emotional insecurity thus might be expected but many questions remain, including whether there are differences in the magnitude of these relations. Given the co-morbidity of these symptoms, simultaneous longitudinal tests of relations between family conflict, emotional security in the family system, and both symptoms of anxiety and depression are required to cogently evaluate patterns of influence (Hayward et al., 2008).
Externalizing problems, including conduct problems, have been linked with interparental conflict in both clinical and community samples and with emotional security in both interparental (Cummings & Davies, 2010) and parent-child relationships (DeKlyen & Greenberg, 2008). In a meta-analysis, Fearon, Bakersman-Kranenburg, van IJzendoorn, Lapsley and Roisman (2010) reported that externalizing problems were linked with insecure patterns in infancy and early childhood, including disorganized patterns, with weaker effects for avoidance and resistance. They also reported that attachment insecurity was more strongly associated with externalizing than internalizing symptoms (see also Groh et al., 2012). Notably, links with externalizing problems mediated by emotional insecurity about interparental conflict are found (Cummings & Davies, 2010), with destructive interparental conflict linked with child aggression (e.g., Cummings, Goeke-Morey, & Papp, 2004). Although conduct problems are linked with interparental conflict, little is known about emotional insecurity as a mediating process for this specific type of symptoms (Cummings & Davies, 2010).
Social functioning in the peer domain is another dimension of adjustment in adolescence linked with interparental conflict (Cummings & Davies, 2010). Notably, differences are evident in the causes, correlates and consequences of peer problems compared to conduct problems, aggression and other externalizing problems. In studies of community samples, peer rejection and unpopularity are linked with externalizing problems whereas lack of peer acceptance, social isolation, and perceptions of social incompetence are associated with internalizing problems (Hymel, Rubin, Rowden, & LeMare, 1990; van Lier & Koot, 2010). With regard to emotional security, relations are found between early attachment security and the quality of later peer relations, especially in middle childhood and adolescence (Pallini, Baiocco, Schneider, Madigan, & Atkinson, 2014; Schneider, Atkinson, & Tardiff, 2001). Suggesting relations between peer problems and diminished security about the family system as a whole, in a study based on a community sample, Keelan, Schenk, McNally, and Fremouw (2014) reported that bullys, bully/ victims, and victims had lower scores on emotional security about the family based on the SIFS compared to control/normative families.
In summary, we hypothesize that T1 family conflict will be related to adolescents’ emotional insecurity about the family system at T2, and in turn adolescents’ emotional insecurity about the family system will be associated with the development of adolescents’ symptoms of mental health at T3. We expect that family conflict will predict both a higher-order or latent construct of emotional insecurity and also specific patterns of insecurity about the family system. We also hypothesize that higher-order emotional insecurity is related to risk for the development of all four specific symptoms examined in this study (e.g., depression, anxiety, conduct and peer problems). In terms of specific patterns of emotional insecurity, preoccupation is predicted to be especially related to symptoms of depression and anxiety whereas disengaged patterns are expected to increase the risk of conduct problems. Given the broad domain of peer problems and associations with both internalizing and externalizing problems, hypotheses regarding specific patterns of emotional insecurity are exploratory. The rigor of the theoretically-driven model test is increased by simultaneously testing relations with symptoms of mental health problems as outcomes, including autoregressive controls for initial levels (T1) of symptoms, and initial levels of emotional insecurity about the family system.
Method
Participants
Data for the current study are drawn from a dual-site, longitudinal project assessing family process and child adjustment during early adolescence. Participants included 295 mother-father-child families (146 boys, 149 girls, T1 M age = 13.10 years, SD = .53) who were recruited from communities in the Northeast and Midwest through flyers sent to local schools, churches, neighborhoods, and community events. One cohort of families (n = 210) was recruited when children were in kindergarten. Eligibility criteria required mother, father, and child participants to be cohabitating for a minimum of 3 years, the family have a child in kindergarten, and all participants to be English-proficient. The second cohort (n = 85) was recruited during early adolescence to match the age and grade of children in the original cohort. Data for the current study is drawn from the early adolescent years consisting of three annual time points (T1 Median grade = 7, T2 Median grade = 8, T3 Median grade = 9); both cohorts participated in all three time points. There were no differences in study variables between cohorts; however the adolescents in the original cohort were slightly younger (M = 13.03, SD = .53; F(1,252) = 7.50, p < .01) than the supplemental cohort (M = 13.23, SD = .52) at T1; thus, age was included as a covariate in analyses. Participants were representative of the communities from which they were drawn, reflecting mostly intact, middle-class families (92% intact, cohabitating families; intact family cohabitation with adolescent M = 11.9 years, SD = 3.3). At T1, 84.9% of couples were married and the majority of parents were the biological mother (92.8%) and father (79.2%) of the study child (remaining parents: 2.9% and 3.5% adoptive parent, 1.1% and 12.5% step-parent, 3.3% and 4.8% other family member or guardian for female and male caregivers, respectively). Of participants, 73.5% were White, 17.1% Black or African-American, 4.3% Hispanic, and 5.1% reported other or multiracial backgrounds. Of families participating at T1 (n = 280), 95.0% participated at T2 (n = 266; T2 child M age = 14.25 years, SD = .57). Additionally, of families participating at T2, 94.0% participated at T3 (n = 250; T3 child M age = 15.40 years, SD = .63). Seventy-nine percent of families participated in all three time points. Fifteen families of the original cohort were enrolled at either T2 or T3 after missing the T1 assessment. Families lost to attrition at either T2 or T3 did not differ from retained families on any of the study variables at T1 or demographic variables including, child gender, marital status, family income, or parent education.
Procedure
Mothers, fathers, and their adolescent child visited a laboratory setting designed to reflect a home living room environment for a 2.5 hour visit. Informed consent and assent were obtained prior to the start of each session and all study procedures were approved by the University’s institutional review board at each site. Parents were provided monetary compensation for their time and adolescents received a giftcard as compensation for their time.
Family Problem-Solving Task
Mothers, fathers, and adolescent children engaged in a seven-minute family problem-solving discussion task at T1. Families were instructed to discuss the topic they chose similar to how they would in their home, working toward a solution or resolution as a goal. Discussions were videotaped and later coded. The family problem-solving task was conducted consistent with other established procedures of triadic parent-child interaction tasks (Gordis, Margolin, & John, 2001; Lindahl & Malik, 1999).
Measures
Mother-, father-, and observer-reports of family conflict were utilized to construct a latent variable of family conflict. Adolescents completed assessments of family security and symptomology.
Family Conflict
Family conflict was assessed using observation and questionnaire assessments. The family problem-solving task was coded using the Negativity and Conflict subscale of the System for Coding Interactions and Family Functioning (SCIFF; Lindahl & Malik, 2000). Codes assessed the overall level of negativity and tension present at the family-level during the disagreement task. Observable levels of conflict and negativity were assessed from family members’ tone of voice, body language, and facial expressions, on a 5-point Likert scale from 1 (very low) to 5 (high). The SCIFF has good concurrent and constructive validity (Lindahl & Malik, 2001). A subset of 20% of videotaped interactions was coded by a separate trained coder to calculate reliability in the current sample. Reliability for the Negativity/Conflict scale was ICC = .81.
Family conflict was also measured using a revised version of the conflict scale of the Family Environment Scale (FES, nine items; Moos & Moos, 2002). Items reflected the degree to which family members engaged in various conflict tactics and included all members of the family. Parents rated items on four point Likert scales on a scale of 1 (very untrue), 2 (fairly untrue), 3 (fairly true), and 4 (very true). Sample items included “Family members sometimes hit each other” and “We fight a lot in our family”. Moos and Moos (2002) report good discriminant validity and test-retest reliability on the standard true-false version of the scale. Internal reliability was adequate in the current sample (mother-report α = .74; father-report α = .69).
Security in the Family System
Adolescents completed the SIFS at T1 and T2 (22 items; Forman & Davies, 2005), assessing specific scales of secure, disengaged, and preoccupied appraisals about the family. Adolescents reported on a 5-point Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree). Sample items for the seven-item security subscale included “I’m glad to be a part of my family because there are more good things about it than bad things” and “When I think about the problems in my family, I feel that things will work out in the end”. Sample items for the eight-item preoccupied subscale included “I feel like something could go very wrong in my family at any time” and “When something I don’t like happens in my family, I think about it over and over again.” Sample items for the seven-item disengaged subscale included “When something bad happens in my family, I wish I could live with a different family” and “I don’t care what goes on in my family.” Forman and Davies (2005) report good internal consistency, test-retest reliability, and discriminant validity of the three subscales. Internal reliability in the current sample were preoccupation: T1 α = .83, T2 α = .90; security: T1 α = .85, T2 α = .83; and disengagement subscale: T1 α = .84, T2 α = .89.
Adolescent Depressive Symptoms
Adolescents completed the 20-item Center for Epidemiologic Studies Depression scale (CES-D; Radloff, 1977) assessing depressive symptomatology over a one-week period at T1 and T3. Sample items include “I felt lonely” and “I was bothered by things that usually don’t bother me”. Adolescents rated how frequently they experienced each item over the last week on a 4-point Likert scale ranging from 1 (rarely or none of the time; less than one day) to 4 (most or all of the time; five to seven days). The CES-D is suitable for assessing depression in adolescence (Radloff, 1991; Roberts, Andrews, Lewinsohn, & Hops, 1990) and had adequate internal reliability in the current sample (T1 α = .87; T3 α = .89). Scores of 16 or higher reflect clinical levels of depression in adult samples (Radloff & Teri, 1986), with 18.4% (T1) and 23.4% (T3) of adolescents scoring in this range.
Adolescent Anxiety Symptoms
Adolescents completed the 28-item Revised Children’s Manifest Anxiety Scale (RCMAS; Reynolds & Richmond, 1978). Sample items included “I worry a lot of the time” and “it is hard for me to get to sleep at night.” The RCMAS has good construct validity and adequate reliability (Reynolds, 1980; Reynolds & Paget, 1983) and good internal reliability for the current sample (T1 α = .87; T3 α = .86). Scores of 19 or greater reflect clinical levels of anxiety (Stellard, Velleman, Langsford, & Baldwin, 2001), with 8.3% (T1) and 5.2% (T3) of adolescents scoring in this range.
Adolescent Peer and Conduct Problems
Adolescents completed the five-item peer problems and the five-item conduct problems subscales of the Strengths and Difficulties Questionnaire at T1 and T3 (SDQ; Goodman, 1997). The peer problem subscale assesses difficulties with same age peers and social relationships. Sample items include “other children or young people pick on me” and “I am usually on my own.” The conduct problem subscale assesses delinquent behaviors and sample items include “I fight a lot” and “I get very angry and often lose my temper.” Adolescents responded to items on a three-point Likert scale (“not true”, “somewhat true”, and “certainly true”). Internal reliabilities in the current sample were low (peer problems: T1 α = .44, T3 α = .52; conduct problems: T1 α = .64, T3 α = .64). Low reliabilities of these scales have been consistently found (Nunnally & Bernstein, 1994); particularly for the peer and conduct problems subscales (Bourdon et al., 2005; McCrory & Layte, 2012; Muris et al., 2003). Scale construction of the original SDQ focused on the creation of subscales that maximize clinical significance, resulting in heightened predictive validity while reducing the internal consistency of the SDQ scales. Consistent with the goal of optimizing predictive validity, Goodman and Scott (1999) reported the SDQ scales were more highly correlated with interview-based ratings of clinical symptoms than the Child Behavior Checklist. Additionally they found that the SDQ discriminated between high risk and low risk samples in support of criterion validity.
Results
Descriptive statistics and correlations among study variables are displayed in Table 1. T1 symptoms were significantly correlated with T3 symptoms of disorders and maladjustment, indicating moderate stability. Additionally, symptoms were significantly correlated across adjustment problems within time points. There were no gender differences in depressive or anxious symptoms at T1 F(1,254) = 3.68, ns; F(1,239) = 2.24, ns, respectively. At T3, girls reported higher depressive (M = 12.29, SD = 9.67) and anxious (M = 9.76, SD = 5.72) symptoms compared to boys (M = 9.69, SD = 8.68; M = 7.35, SD = 5.14, respectively), F(1,230) = 4.65, p < .05; F(1,227) = 11.15, p < .001, respectively. Additionally no gender differences were found in adolescents’ peer or conduct problems at T1 F(1,267) = 1.43, ns; F(1,262) = 1.72, ns or T3 F(1,238) = 2.04, ns; F(1,237) = 2.85, ns. Given the differences in depressive and anxiety symptoms, child gender was examined as a moderator in subsequent analyses. Family income was correlated with many of the study variables (see Table 1), thus it was included as a covariate in subsequent analyses.
Table 1.
Correlations and Descriptive Statistics
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. T1 MR Family Conflict | -- | ||||||||||||||||||
| 2. T1 FR Family Conflict | .37** | -- | |||||||||||||||||
| 3. T1 OR Family Conflict | .22** | .14* | -- | ||||||||||||||||
| 4. T1 Preoccupation | .12* | .11 | .15* | -- | |||||||||||||||
| 5. T1 Security | −.25** | −.28** | −.20** | −.26** | -- | ||||||||||||||
| 6. T1 Disengagement | .22** | .20 | .22** | .68** | −.53** | -- | |||||||||||||
| 7. T2 Preoccupation | .19** | .11 | .15* | .54** | −.39** | .53** | -- | ||||||||||||
| 8. T2 Security | −.16* | −.11 | −.18* | −.14* | .53** | −.31** | −.34** | -- | |||||||||||
| 9. T2 Disengagement | .17* | .15* | .24** | .41** | −.47** | .62** | .75** | −.53** | -- | ||||||||||
| 10. T1 Depressive Sx. | .09 | .20** | .12 | .46** | −.49** | .56** | .44** | −.20** | .42** | -- | |||||||||
| 11. T1 Anxious Sx. | .07 | .12 | .03 | .52** | −.33** | .50** | .42** | −.21** | .35** | .60** | -- | ||||||||
| 12. T1 Peer Problems | .05 | .16* | .14* | .19* | −.43** | .25** | .20** | −.29** | .30** | .45** | .36** | -- | |||||||
| 13. T1 Conduct Problems | .21** | .28** | .24** | .30** | −.48** | .42** | .37** | −.29** | .47** | .41** | .37** | .47** | -- | ||||||
| 14. T3 Depressive Sx. | .11 | .01 | .01 | .29** | −.30** | .36** | .35** | −.35** | .36** | .34** | .42** | .11 | .10 | -- | |||||
| 15. T3 Anxious Sx. | .05 | .05 | −.07 | .26** | −.22** | .36** | .44** | −.20** | .35** | .32** | .47** | .17* | .18** | .67** | -- | ||||
| 16. T3 Peer Problems | .06 | .08 | .14* | .17* | −.32** | .19** | .26** | −.38** | .30** | .25** | .37** | .37** | .28** | .38** | .32** | -- | |||
| 17. T3 Conduct Problems | .14* | .07 | .32** | .33** | −.26** | .33** | .33** | −.39** | .47** | .22** | .19** | .13 | .37** | .39** | .27** | .27** | -- | ||
| 18. Child Age | .00 | −.06 | −.07 | .09 | −.08 | .15* | .02 | −.03 | .04 | .12 | .13 | .11 | .06 | .13 | .16** | .01 | .01 | -- | |
| 19. Family Income | −.06 | −.04 | −.24** | −.24** | .23** | −.11 | −.40** | .25** | −.30** | −.13 | −.13 | −.14 | −.20** | −.13 | −.08 | −.18* | −.22** | −.03 | -- |
|
| |||||||||||||||||||
| M | 17.96 | 17.77 | 2.35 | 17.84 | 29.24 | 13.25 | 17.58 | 29.26 | 13.47 | 10.31 | 8.33 | 1.43 | 1.82 | 11.06 | 8.61 | 1.58 | 1.82 | 15.40 | -- |
| SD | 4.10 | 3.96 | 1.43 | 6.23 | 5.24 | 5.43 | 6.78 | 4.80 | 5.66 | 8.64 | 5.90 | 1.51 | 1.83 | 9.29 | 5.57 | 1.60 | 1.75 | .63 | -- |
Note.
p < .05,
p < .01.
Sx = Symptoms. MR = Mother-report. FR = Father-report. OR = Observer-report.
Higher-order Emotional Insecurity in the Family System as a Mediator
Consistent with the emphasis of emotional security theory on emotional security as a higher-order construct (Cummings & Davies, 2010), a model was fit using the structural equation modeling framework (SEM) to investigate a latent variable of emotional security in the family system (T2) as a mediator in the relation between family conflict (T1) and depressive and anxiety symptoms and peer and conduct problems (T3). SEM analyses were conducted using Analysis of Moment Structure software (AMOS, v. 18.0.0; Arbuckle, 1995–2009). AMOS utilizes full-information maximum likelihood estimation to account for missing data. A latent variable of family conflict at T1 was created using mother and father report of family conflict on the FES and observer ratings of family conflict and negativity during the family problem-solving task. Latent variables for emotional security at T1 and T2 were created using adolescent-report of the preoccupied, secure, and disengaged security subscales.
The SEM mediation model included family income and child age as covariates. Autoregressive controls at T1 were included for emotional security and adolescent symptoms. T1 controls were included to account for correlations among all study variables at the start of the study. Residual errors were allowed to correlate across time among the security subscales. Given the similarity in measurement scales, residual errors were allowed to correlate for mother- and father-report of family conflict. Residual errors among symptoms at T3 were also allowed to correlate.
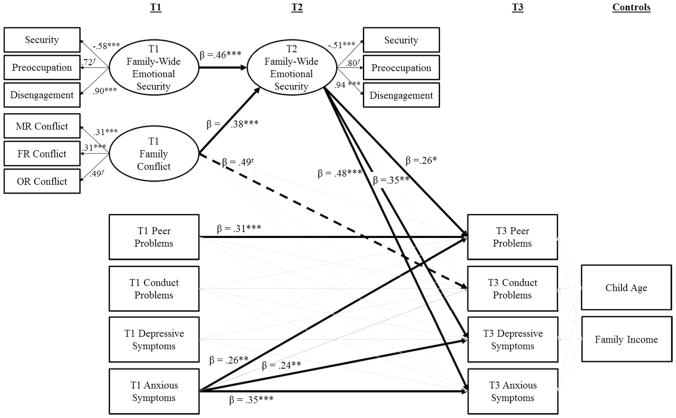
The model provided adequate fit to the data (χ2(90)= 232.06, p < .001; χ2/df = 2.58; RMSEA = .07; CFI = .91; T3 depressive symptoms R2 = .24, T3 anxious symptoms R2 = .34, T3 peer problems R2 = .25, T3 conduct problems R2 = .35). Results for significant pathways are depicted in Figure 1. Family conflict at T1 predicted emotional insecurity at T2 (β = .38, p < .001), in turn, emotional insecurity at T2 predicted peer problems (β = .26, p < .05) and depressive (β = .35, p < .01) and anxious (β = .48, p < .001) symptoms at T3. Emotional security in the family system was moderately stable across the one-year period (β = .46, p < .001). Adolescent anxiety symptoms were a significant predictor of depressive (β = .24, p < .01) and anxiety symptoms (β = .35, p < .001) and peer problems (β = .26, p < .01) two years later. No significant effects were found for conduct problems; however, there was a trend for the direct effect of family conflict on greater conduct problems (β = .49, p < .10) and a trend for emotional security on conduct problems (β = .20, p = .11). Tests of the indirect effects were also examined (Tofighi & MacKinnon, 2011); bootstrapped confidence intervals are reported for the unstandardized parameter estimates of the indirect effect. Proportion of the maximum indirect effect, as a measure of the effects size for the indirect effect, are reported in accordance with the guidelines outlined in Preacher and Kelley (2011). A significant indirect effect was found, suggesting the relation between family conflict and adolescent depressive symptoms was mediated by emotional insecurity in the family system (indirect effect: 1.76, 95% CI: .37, 3.67; K2 = .13). Similarly, a significant indirect effect of family conflict on anxiety symptoms through emotional insecurity was found (indirect effect: 1.43, 95% CI: .44, 2.75; K2 = .15). Lastly, there was a significant indirect effect for peer problems such that emotional insecurity mediated the relation between family conflict and peer problems (indirect effect: .22, 95% CI: .01, .52; K2 = .09).
Figure 1.
Model examining adolescent latent family-wide emotional insecurity as a mediator between family conflict and adolescent symptoms of adjustment problems.
Note. Correlations not depicted in Figure. Figure depicts standardized regression coefficients for significant pathways only. Dashed line indicates statistical trend. MR = Mother-Report. FR = Father-Report. OR = Observer-Report. f= fixed factor loading. tp < .10. *p < .05. **p < .01. ***p < .001. χ2(90) = 232.06, p < .001. CFI = .91, RMSEA = .07. Peer Problems R2=.25, Conduct Problems R2=.35, Depressive Symptoms R2=.24, Anxiety Symptoms R2=.34.
Child Gender as a Moderator
To examine if child gender moderated the mediational pathways, multi-group comparisons were conducted. Gender differences were examined in a reduced model examining T2 emotional security as a mediator between T1 family conflict and T3 depressive and anxious symptoms without the inclusion of the autoregressive controls and covariates. Prior to the multi-group analyses, support for measurement invariance in the factor loadings was found. Models in which the structural pathways were constrained to be equal across groups did not fit the data significantly worse than a model in which these pathways were free to vary (pathways constrained model: χ2 (170.90) = 96.67, χ2 difference = 12.01, Δdf = 9, ns) suggesting no child gender differences in the mediation model. Pathways of this reduced model were similar to pathways in the larger model.
Specific Scales of Emotional Insecurity as Mediators
To examine the role of individual subtypes of emotional security, additional analyses were conducted examining adolescents appraisals of security, preoccupation, and disengagement in the family system at T2 as mediators between T1 family conflict and adolescents’ T3 mental health symptoms. Separate models were conducted examining 1) anxiety and depressive symptoms and 2) peer and conduct problems as outcomes. Similar to the above analyses, a latent variable of family conflict was used and family income and child age were included as covariates. Autoregressive controls for T1 security subtypes and T1 symptoms were included.
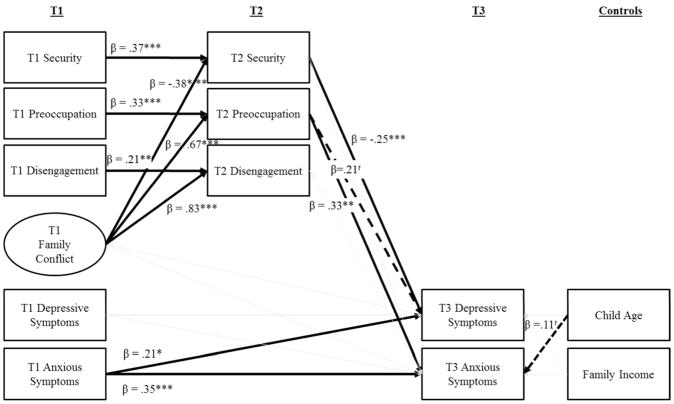
Anxiety and Depressive Symptoms
The model provided adequate fit to the data (χ2(50)= 100.67, p < .001; χ2/df = 2.01; RMSEA = .06; CFI = .96; T3 depressive symptoms R2 = .28, T3 anxious symptoms R2 = .31). Results for significant pathways are depicted in Figure 2. Family conflict at T1 predicted all three subtypes of emotional security at T2 including appraisals of security, (β = −.38, p < .001), preoccupation (β = .67, p < .001), and disengagement (β = .83, p < .001). In turn, lower security appraisals at T2 predicted increased depressive symptoms (β = −.25, p < .001) whereas higher preoccupation predicted higher anxious symptoms (β = .33, p < .01). Tests of the indirect effects supported these two mediation pathways. Higher conflict was predictive of higher depressive symptoms through lower security appraisals (indirect effect: 2.38, 95% CI: .64, 4.73; K2 = .10). Higher conflict was associated with higher anxiety through increased preoccupied appraisals (indirect effect: 3.18, 95% CI: .78, 6.37; K2 = .21).
Figure 2.
Model examining adolescent individual family-wide emotional insecurity indicators as mediators between family conflict and adolescent depressive and anxious symptoms.
Note. Correlations and measurement model not depicted in Figure. Figure depicts standardized regression coefficients for significant pathways only. Dashed line indicates statistical trend. t p < .10. *p < .05. **p < .01. ***p < .001. χ2(50) = 100.67, p < .001. CFI = .96, RMSEA = .06. Depressive Symptoms R2=.28, Anxiety Symptoms R2=.31.
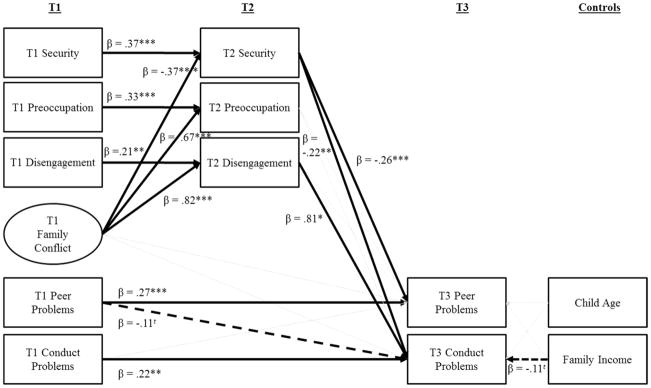
Peer and Conduct Problems
The model provided adequate fit to the data (χ2(50)= 105.25, p < .001; χ2/df = 2.11; RMSEA = .06; CFI = .95; T3 peer problems R2 = .23, T3 conduct problems R2 = .33). Results for significant pathways are depicted in Figure 3. Family conflict at T1 predicted all three subtypes of emotional security at T2 including appraisals of security (β = −.37, p < .001), preoccupation (β = .67, p < .001), and disengagement (β = .82, p < .001). In turn, lower security appraisals at T2 predicted both increased peer (β = −.26, p < .001) and conduct problems (β = −.22, p < .001) at T3. Tests of the indirect effects supported three mediation pathways. Higher conflict, through lower security appraisals, was predictive of greater peer (indirect effect: .42, 95% CI: .12, .83; K2 = .10) and conduct problems (indirect effect: .39, 95% CI: .09, .81; K2 = .08). Higher conflict was associated with higher conduct problems through increased disengaged appraisals (indirect effect: 3.21, 95% CI: .03, 7.68; K2 = .61).
Figure 3.
Model examining adolescent individual family-wide emotional insecurity indicators as mediators between family conflict and adolescent peer and conduct problems.
Note. Correlations and measurement model not depicted in Figure. Figure depicts standardized regression coefficients for significant pathways only. Dashed line indicates statistical trend. t p < .10. *p < .05. ** p < .01. ***p < .001. χ2(50) = 105.25, p < .001. CFI = .95, RMSEA = .06. Peer Problems R2=.23, Conduct Problems R2=.33.
Discussion
In this study, family conflict was related to the development of several adolescent mental health symptoms including, anxiety, depression, conduct problems, and peer problems over the course of early adolescence. Including auto-regressive controls for initial levels of emotional insecurity and multiple adjustment problems, emotional security about the family system measured as a higher-order construct and as specific patterns of emotional security/insecurity, respectively, mediated relations between family conflict and multiple specific mental health symptoms. Formal tests of the significance of indirect effects further supported conclusions.
EST (Cummings & Davies, 2010) has advanced empirical studies supporting a higher-order construct of emotional security/insecurity as reflecting a multiplicity of responses in the service of emotional security and thus providing a measure of an underlying dimension of emotional security/insecurity. Attachment research also provides theory and evidence to support measurement of a higher-order construct of emotional security in addition to specific patterns of emotional security/insecurity (Cummings, 1990; Fraley & Spieker, 2003). Emotional security about the family system measured as a higher-order construct was found in the present study to mediate relations between family conflict and symptoms of anxiety, depression, and peer problems. Employing a higher-order construct of emotional security, reflecting a relatively broad array of insecure/secure behaviors within the family context, thus allowed for the identification of adolescents at risk for a host of developmental difficulties. This conceptualization of emotional security thus provides a conceptually parsimonious and statistically sophisticated model for a dimension of processes underlying youth’s risk for later mental health problems in the face of family discord.
Consistent with Forman and Davies (2005) and with approaches to investigate patterns of emotional security in the family based on attachment theory, additional tests indicated that specific patterns of security/insecurity mediated relations with symptoms of specific disorders and problems. Notably, insecurity characterized by preoccupation was related to symptoms of anxiety whereas insecurity characterized by disengagement was associated with conduct problems. Preoccupation may be adaptive in the face of heightened family discord by increasing vigilance toward further threatening events. However, in the long-run increased worry and preoccupation may promote anxious behaviors in broader settings beyond the family unit. On the other hand, disengaged or dismissing strategies allow adolescents to manage family discord by distancing or diminishing the importance of the family. Contrary to the long-term effects of preoccupation, disengagement may promote problems with social rule violations and deviance outside the family environment. Secure patterns also mediated relations between family conflict and adolescent mental health; heightened security was linked with reduced symptoms of depression, conduct problems, and peer problems. These results thus provide support for the notion that secure appraisals may serve as a protective factor fostering resilience in the face of family conflict. Children’s confidence in the family as a safe haven and predictable environment may diminish the effects of discord on their mental health across many domains of functioning. Although relations between insecurity and heightened risk for youth adjustment problems in the face of family discord are causes for concern, it is also important to keep in mind that youth’s sense of security about the family is a highly positive response process, consistently linked with reduced negative and elevated positive responding in both the short- and long-term (Cummings & Davies, 2010).
This study builds on past work examining mediating processes concerning adolescents’ specific symptoms of psychopathology (Compas, Connor-Smith, Saltzman, Thomsen, & Wadsworth, 2001) by contributing information about specific mediating processes (Garber, 2006) and specific mechanisms at play within the family context (Grant et al., 2003). Building on research on the role of security in the mother-child relationship in youth adjustment (Abela et al., 2005; Brumariu & Kerns, 2008, 2010a, 2010b), the present study provides support for the significance of insecure response strategies in the family system for etiological models of symptoms of specific disorders and adjustment problems (Essau, 2004). Moreover, notions of insecure response strategies, that is, patterns of emotional insecurity in the family system, reflected an extension of parallel insecure strategies in the context of parent-child attachment (DeKlyen & Greenberg, 2008).
Interpersonal stress (Carter & Garber, 2011; Krackow & Rudolph, 2008; Pine, Cohen, Johnson & Brooks, 2002), psychosocial adversity (Foster, Webster, Weissman et al., 2008), and the emotional climate in the family (Nomura et al., 2002) have been related to adolescents’ symptoms of disorders. Complementing this research, family conflict is conceptualized as an index of the emotional climate of the family and adolescents’ reactions to family conflict are conceptualized as coping processes (Cummings & Cummings, 1988). These coping responses serve to regain or maintain a secure base within the family when coping with threatening interpersonal stress and adversity (Waters & Cummings, 2000).
Youth’s risk for adjustment problems may be specifically associated with forms of conflict that undermine or foster security in the family system. For example, the impact of interparental conflict has been found to have negative or positive consequences depending on whether the conflict behaviors are destructive or constructive, respectively (Cummings & Davies, 2010). The study of the role of constructive as well as destructive family conflict in child well-being and adjustment is an important direction for future research and help to elucidate the development of secure appraisals. Relations between family conflict, emotional insecurity in the family system, and adjustment outcomes were not significantly different for boys and girls, consistent with findings from research on interparental conflict, emotional insecurity, and child adjustment (Cummings & Davies, 2010) suggesting that conflict is a distressing concern for children and regardless of gender, children employ the similar types of coping mechanisms.
Multiple risk models are essential towards fully understanding the etiology of symptoms of specific disorders or problems, including notions of cumulative risk models (Epkins & Heckler, 2011; Garber & Weersing, 2010). The present findings add to the evidence regarding certain specific classes of risk and protective factors, that is, family conflict and adolescents’ emotional insecurity/security in the family system. Future research should strive to incorporate the present constructs into broader models of risk and protective factors, including temperament, negative affectivity, genetic, and other environmental influences (Clark, 2005; Clark & Watson, 1991; also see De Bolle & De Fruyt, 2010).
Anxiety and depression have been found to be co-morbid (Garber & Weersing, 2010). Consistent with past research (Bittner et al., 2004; Gallerani et al., 2010), the present study found that earlier anxiety symptoms were implicated in the development of later depressive symptoms (see Figure 1). Although a significant pathway was not identified in the final model tests between early and later depression symptoms (see Figure 1), a significant zero-order correlation was found between early and later depressive symptoms (see Table 1). The present findings are thus more indicative of the relative size of the relations between earlier anxiety symptoms and later depressive symptoms than a lack of relationship between early and later depression symptoms.
The present study is not without limitations. Families were drawn from a community sample and although sub-clinical symptoms contribute to understanding of the emergence of clinical disorders (Garber, 2006), these relations may not generalize to clinical samples of distressed families. Additionally, the study relied on adolescents’ self-report measures of symptoms; the use of clinical diagnostic tools is an important direction for future research. Specific patterns of emotional security were identified in the development of symptoms of conduct problems, including negative relations with security and positive relations with disengagement, highlighting the role of security processes in the development of these symptoms. Consistent with past work based on EST, higher-order assessments of emotional insecurity were related to multiple adjustment problems. However, the overall latent construct of emotional insecurity was not related to changes in conduct problems. We are unsure why this link was not found, especially since specific facets of emotional insecurity (i.e., low security, high disengagement) did mediate the prediction of conduct problems. One possibility is that this non-finding reflected that the latent construct for emotional insecurity included indicators (i.e., preoccupied) more closely linked with other dimensions of adjustment problems (e.g., anxiety symptoms), thereby diminishing the unique associations with conduct problems. Notably, other relations were only indicated based on the higher-order construct of emotional insecurity, indicating again the value of scoring for higher-order and specific facets of emotional insecurity (Cummings & Davies, 2010).
Finally, with regard to implications for clinical practice, the importance for understanding the etiology of specific symptoms of disorders and problems associated with adolescents’ emotional insecurity/security and family discord was underscored (Kraaij et al., 2003; Sander & McCarty, 2005). Both parents should be made aware of the potentially negative implications of family conflict and the impact on youths’ appraisals of safety and security. Promotion of safety and security has been identified across multiple contexts as an essential element of intervention or prevention efforts for youth exposed to threatening environments (Hobfoll et al., 2007). Both underlying dimensions of security/ insecurity in the family system and specific patterns of responding in the service of regaining or maintaining security may be relevant to consider in prevention and intervention for adolescents in context of family discord. Parents may be able to reduce children’s risk for mental health problems by influencing or altering patterns of family negative emotional expression and conflict resolution. The present study further illuminates family factors and response processes affecting adolescents’ risk for symptoms of specific disorders. The findings suggest psychological interventions geared toward improving conflict resolution in the family and emotional security in the family system hold promise for reducing multiple mental health symptoms of psychopathology in adolescents.
Acknowledgments
This research was supported by grant R01 MH57318 from the National Institute of Mental Health awarded to Patrick T. Davies and E. Mark Cummings. Support was provided to Kalsea J. Koss by a National Institute of Mental Health training grant (T32 MH015755, PI: Dante Cicchetti) during the preparation of this article. The authors are grateful to the families who participated in this project and the staff and students who assisted on various stages of the project at the University of Notre Dame and the University of Rochester, in particular to Jana Lam for her assistance with the observational coding.
Contributor Information
E. Mark Cummings, University of Notre Dame.
Kalsea J. Koss, Institute of Child Development, University of Minnesota
Patrick T. Davies, University of Rochester
References
- Abela JRZ, Hankin BL, Haigh EAP, Adams P, Vinokuroff T, Trayhern L. Interpersonal vulnerability to depression in high-risk children: The role of insecure attachment and reassurance seeking. Journal of Clinical Child and Adolescent Psychology. 2005;34:182–192. doi: 10.1207/s15374424jccp3401_17. [DOI] [PubMed] [Google Scholar]
- Allen JP, Antonishak J. Understanding adolescent peer influences: Beyond the dark side. In: Prinstein MJ, Dodge KS, editors. Peer Influence Among Youth. New York: Guilford Press; 2008. [Google Scholar]
- Arbuckle JL. AMOS version 18.0.0 [Computer software] 1995–2009. [Google Scholar]
- Bittner A, Goodwin RD, Wittchen H, Beesdo K, Höfler M, Lieb R. What characteristics of primary anxiety disorders predict subsequent major depressive disorder? Journal of Clinical Psychiatry. 2004;65:618–626. doi: 10.4088/JCP.v65n0505. [DOI] [PubMed] [Google Scholar]
- Bourdon KH, Goodman R, Rae DS, Simpson G, Koretz DS. The strengths and difficulties questionnaire: US normative data and psychometric properties. Journal of the American Academy of Child and Adolescent Psychiatry. 2005;44:557–564. doi: 10.1097/01.chi.0000159157.57075.c8. [DOI] [PubMed] [Google Scholar]
- Bowlby J. Attachment and loss, Vol. 2: Separation. New York, NY: Basic Books; 1973. [Google Scholar]
- Brumariu LE, Kerns KA. Mother-child attachment and social anxiety symptoms in middle childhood. Journal of Applied Developmental Psychology. 2008;29:393–402. doi: 10.1016/j.appdev.2008.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brumariu LE, Kerns KA. Mother–child attachment patterns and different types of anxiety symptoms: Is there specificity of relations? Child Psychiatry and Human Development. 2010a;41:663–674. doi: 10.1007/s10578-010-0195-0. [DOI] [PubMed] [Google Scholar]
- Brumariu LE, Kerns KA. Parent-child attachment and internalizing symptoms in childhood and adolescence: A review of empirical findings and future directions. Development and Psychopathology. 2010b;22:177–203. doi: 10.1017/S0954579409990344. [DOI] [PubMed] [Google Scholar]
- Carter JS, Garber J. Predictors of the first onset of a major depressive episode and changes in depressive symptoms across adolescence: Stress and negative cognitions. Journal of Abnormal Psychology. 2011;120:779–796. doi: 10.1037/a0025441. [DOI] [PubMed] [Google Scholar]
- Clark LA. Temperament as a unifying basis for personality and psychopathology. Journal of Abnormal Psychology. 2005;114:505–521. doi: 10.1037/0021-843X.114.4.505. [DOI] [PubMed] [Google Scholar]
- Clark LA, Watson D. Tripartite model of anxiety and depression: Psychometric evidence and taxonomic implications. Journal of Abnormal Psychology. 1991;100:316–336. doi: 10.1037/0021-843X.100.3.316. [DOI] [PubMed] [Google Scholar]
- Colonnesi C, Draijer EM, Stams GJJM, Van der Bruggen CO, Bogels SM, Noom MJ. The relation between insecure attachment and child anxiety: A meta-analytic review. Journal of Child and Analytic Psychology. 2011;40:630–645. doi: 10.1080/15374416.2011.581623. [DOI] [PubMed] [Google Scholar]
- Compas BE, Connor-Smith J, Saltzman H, Thomsen AH, Wadsworth ME. Coping with stress during childhood and adolescence: Problems, progress, and potential in theory and research. Psychological Bulletin. 2001;127:87–127. doi: 10.1037/0033-2909.127.1.87. [DOI] [PubMed] [Google Scholar]
- Cummings EM. Classification of attachment on a continuum of felt-security: Illustrations from the study of children of depressed parents. In: Greenberg M, Cicchetti D, Cummings EM, editors. Attachment in the preschool years: Theory, research, and intervention. Chicago and London: The University of Chicago Press; 1990. pp. 311–338. [Google Scholar]
- Cummings EM, Cicchetti D. Towards a transactional model of relations between attachment and depression. In: Greenberg M, Cicchetti D, Cummings EM, editors. Attachment in the preschool years: Theory, research, and intervention. Chicago and London: The University of Chicago Press; 1990. pp. 339–372. [Google Scholar]
- Cummings EM, Cummings JS. A process-oriented approach to children’s coping with adults’ angry behavior. Developmental Review. 1988;3:296–321. doi: 10.1016/0273-2297(88)90008-1. [DOI] [Google Scholar]
- Cummings EM, Davies PT. Emotional security as a regulatory process in normal development and the development of psychopathology. Development and Psychopathology. 1996;8:123–139. doi: 10.1017/S0954579400007008. [DOI] [Google Scholar]
- Cummings EM, Davies PT. Marital conflict and children: An emotional security perspective. New York and London: The Guilford Press; 2010. [Google Scholar]
- Cummings EM, Goeke-Morey MC, Papp LM. Everyday marital conflict and child aggression. Journal of Abnormal Child Psychology. 2004;32:191–202. doi: 10.1023/B:JACP.0000019770.13216.be. [DOI] [PubMed] [Google Scholar]
- Cummings EM, Schermerhorn AC, Davies PT, Goeke-Morey MC, Cummings JS. Interparental discord and child adjustment: Prospective investigations of emotional security as an explanatory mechanism. Child Development. 2006;77:132–152. doi: 10.1111/j.1467-8624.2006.00861.x. [DOI] [PubMed] [Google Scholar]
- Davies PT, Cummings EM. Marital conflict and child adjustment: An emotional security hypothesis. Psychological Bulletin. 1994;116:387–411. doi: 10.1037/0033-2909.116.3.387. [DOI] [PubMed] [Google Scholar]
- Davies PT, Forman EM. Children’s patterns of preserving emotional security in the interparental subsystem. Child Development. 2002;73:1880–1903. doi: 10.1111/1467-8624.t01-1-00512. [DOI] [PubMed] [Google Scholar]
- Davies PT, Harold GT, Goeke-Morey MC, Cummings EM. Children’s emotional security and interparental conflict. Monographs of the Society for Research on Child Development. 2002:67. [PubMed] [Google Scholar]
- Davies PT, Sturge-Apple M, Boscoe SM, Cummings EM. The legacy of early insecurity histories in shaping adolescent adaptation to interparental conflict. Child Development. 2014;85:338–354. doi: 10.1111/cdev.12119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Bolle M, De Fruyt F. The tripartite model in childhood and adolescence: Future directions for developmental research. Child Development Perspectives. 2010;4:174–180. doi: 10.1111/j.1750-8606.2010.00136.x. [DOI] [Google Scholar]
- DeKlyen M, Greenberg MT. Attachment and psychopathology in childhood. In: Cassidy J, Shaver PR, editors. Handbook of attachment: Theory, research, and clinical applications. New York, NY: Guilford Press; 2008. pp. 637–665. [Google Scholar]
- Epkins CC, Heckler DR. Integrating etiological models of social anxiety and depression in youth: Evidence for a cumulative interpersonal risk model. Clinical Child and Family Psychology Review. 2011;14:329–376. doi: 10.1007/s10567-011-0101-8. [DOI] [PubMed] [Google Scholar]
- Essau CA. The association between family factors and depressive disorders in adolescents. Journal of Youth and Adolescence. 2004;33:365–372. doi: 10.1023/B:JOYO.0000037630.01098.d4. [DOI] [Google Scholar]
- Esbjorn BH, Bender PK, Reinholdt-Dunne ML, Munck LA, Ollendick TH. The development of anxiety disorders: considering the contributions of attachment and emotion regulation. Clinical Child and Family Psychology Review. 2012;15:129–143. doi: 10.1007/s10567-011-0105-4. [DOI] [PubMed] [Google Scholar]
- Fearon RP, Bakersman-Kranenburg MJ, van Ijzendoorn MH, Lapsley AM, Roisman GI. The significance of insecure attachment and disorganization in the development of children’s externalizing behavior: A meta-analytic study. Child Development. 2010;81:435–456. doi: 10.1111/j.1467-8624.2009.01405.x. [DOI] [PubMed] [Google Scholar]
- Forman EM, Davies PT. Assessing children’s appraisals of security in the family system: The development of the security in the family system (SIFS) scales. Journal of Child Psychology and Psychiatry. 2005;46:900–916. doi: 10.1111/j.1469-7610.2004.00385.x. [DOI] [PubMed] [Google Scholar]
- Foster CE, Webster MC, Weissman MM, Pilowsky DJ, Wickramaratne PJ, Rush AJ, … King CA. Course and severity of maternal depression: Associations with family functioning and child adjustment. Journal of Youth and Adolescence. 2008;37:906–916. doi: 10.1007/s10964-007-9216-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fraley RC, Spieker SJ. Are infant attachment patterns continuously or categorically distributed? A taxometric analysis of Strange Situation behavior. Developmental Psychology. 2003;39:387–404. doi: 10.1037/0012-1649.39.3.387. [DOI] [PubMed] [Google Scholar]
- Gallerani CM, Garber J, Martin NC. The temporal relation between depression and comorbid psychopathology in adolescents at varied risk for depression. Journal of Child Psychology and Psychiatry. 2010;51:242–249. doi: 10.1111/j.1469-7610.2009.02155.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garber J. Depression in children and adolescents: Linking risk research and prevention. American Journal of Preventive Medicine. 2006;31:S104–S125. doi: 10.1016/j.amepre.2006.07.007. [DOI] [PubMed] [Google Scholar]
- Garber J, Weersing VR. Comorbidity of anxiety and depression in youth: Implications for treatment and prevention. Clinical Psychology: Science and Practice. 2010;17:293–306. doi: 10.1111/j.1468-2850.2010.01221.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman R. The strengths and difficulties questionnaire: A research note. Journal of Child Psychology and Psychiatry. 1997;38:581–586. doi: 10.1111/j.1469-7610.1997.tb01545.x. [DOI] [PubMed] [Google Scholar]
- Goodman R, Scott S. Comparing the strengths and difficulties questionnaire and the child behavior checklist: Is small beautiful? Journal of Abnormal Psychology. 1999;27:17–24. doi: 10.1023/A:1022658222914. [DOI] [PubMed] [Google Scholar]
- Gordis EB, Margolin G, John RS. Parents’ hostility in dyadic marital and triadic family settings and children’s behavior problems. Journal of Consulting and Clinical Psychology. 2001;69:727–734. doi: 10.1037/0022-006X.69.4.727. [DOI] [PubMed] [Google Scholar]
- Grant KE, Compas BE, Stuhlmacher AF, Thurm AE, McMahon SD, Halpert JA. Stressors and child and adolescent psychopathology: Moving from markers to mechanisms of risk. Psychological Bulletin. 2003;129:447–466. doi: 10.1037/0033-2909.129.3.447. [DOI] [PubMed] [Google Scholar]
- Groh AM, Roisman GI, van IJzendoorn MH, Bakermans-Kranenburg MJ, Fearon RP. The significance of insecure and disorganized attachment for children’s internalizing symptoms: a meta-analytic study. Child Development. 2012;83:591–610. doi: 10.1111/j.1467-8624.2011.01711.x. [DOI] [PubMed] [Google Scholar]
- Hankin BL, Abramson LY, Miller N, Haeffel GJ. Cognitive vulnerability-stress theories of depression: Examining affective specificity in the prediction of depression versus anxiety in three prospective studies. Cognitive Therapy and Research. 2004;28:309–345. doi: 10.1023/B:COTR.0000031805.60529.0d. [DOI] [Google Scholar]
- Harold GT, Shelton KH, Goeke-Morey MC, Cummings EM. Marital conflict, child emotional security about family relationships and child adjustment. Social Development. 2004;13:350–376. doi: 10.1111/j.1467-9507.2004.00272.x. [DOI] [Google Scholar]
- Hayward C, Wilson KA, Lagle K, Kraemer HC, Killen JD, Taylor CB. The developmental psychopathology of social anxiety in adolescents. Depression and Anxiety. 2008;25:200–206. doi: 10.1002/da.20289. [DOI] [PubMed] [Google Scholar]
- Hobfoll SE, Hall BJ, Canetti-Nisim D, Galea S, Johnson RJ, Palmieri PA. Refining our understanding of traumatic growth in the face of terrorism: Moving from meaning cognitions to doing what is meaningful. Applied Psychology: An International Review. 2007;56:345–366. doi: 10.1111/j.1464-0597.2007.00292.x. [DOI] [Google Scholar]
- Hymel S, Rubin KH, Rowden L, LeMare L. Children’s peer relationships: longitudinal prediction of internalizing and externalizing problems from middle to late childhood. Child Development. 1990;61:2004–2021. [Google Scholar]
- Kane P, Garber J. The relations among depression in fathers, children’s psychopathology, and father-child conflict: A meta-analysis. Clinical Psychology Review. 2004;24:339–360. doi: 10.1016/j.cpr.2004.03.004. [DOI] [PubMed] [Google Scholar]
- Keelan CM, Schenk AM, McNally MR, Fremouw WJ. The interpersonal worlds of bullies: parents, peers, and partners. Journal of Interpersonal Violence. 2014;29:1339–1353. doi: 10.1177/0886260513506278. [DOI] [PubMed] [Google Scholar]
- Kraaij V, Garnefski N, de Wilde EJ, Dijkstra A, Gebhardt W, Maes S, ter Doest L. Negative life events and depressive symptoms in late adolescence: Bonding and cognitive coping as vulnerability factors? Journal of Youth and Adolescence. 2003;32:185–193. doi: 10.1023/A:1022543419747. [DOI] [Google Scholar]
- Krackow E, Rudolph KD. Life stress and the accuracy of cognitive appraisals in depressed youth. Journal of Clinical Child and Adolescent Psychology. 2008;37:376–385. doi: 10.1080/15374410801955797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindahl KM, Malik NM. Marital conflict, family processes, and boys’ externalizing behavior in Hispanic American and European American families. Journal of Clinical Child Psychology. 1999;28:12–24. doi: 10.1207/s15374424jccp2801_2. [DOI] [PubMed] [Google Scholar]
- Lindahl KM, Malik NM. System for coding interactions and family functioning (SCIFF) University of Miami; Miami, FL: 2000. Unpublished manual. [Google Scholar]
- Lindahl KM, Malik NM. The System for Coding Interactions and Family Functioning. In: Kerig PK, Lindahl KM, editors. Family observational coding systems: Resources for systemic research. Philadelphia, PA: Brunner/Mazel; 2001. pp. 75–90. [Google Scholar]
- McCrory C, Layte R. Testing competing models of the Strengths and Difficulties Questionnaire’s (SDQ’s) factor structure for the parent-informant instrument. Personality and Individual Differences. 2012;52:882–887. doi: 10.1016/j.paid.2012.02.011. [DOI] [Google Scholar]
- Moos RH, Moos BS. Family Environment Scale manual. 3. Palo Alto, CA: Mind Garden; 2002. [Google Scholar]
- Muris P, Meesters C, van den Berg F. The Strengths and Difficulties Questionnaire (SDQ) – further evidence for its reliability and validity in a community sample of Dutch children and adolescents. European Child and Adolescent Psychiatry. 2003;12:1–8. doi: 10.1007/s00787-003-0298-2. [DOI] [PubMed] [Google Scholar]
- Nomura Y, Wickramaratne PJ, Warner V, Mufson L, Weissman MM. Family discord, parental depression and psychopathology in offspring: Ten-year follow-up. Journal of the American Academy of Child & Adolescent Psychiatry. 2002;41:402–409. doi: 10.1097/00004583-200204000-00012. [DOI] [PubMed] [Google Scholar]
- Nunnally JC, Bernstein IH. Psychometric theory. 3. New York: McGraw-Hill; 1994. [Google Scholar]
- Pallini S, Baiocco R, Schneider BH, Madigan S, Atkinson L. Early child-parent attachment and peer relations: a meta-analysis of recent research. Journal of Family Psychology. 2014;28(1):118–123. doi: 10.1037/a0035736. [DOI] [PubMed] [Google Scholar]
- Patterson . Coercive Family Processes. Eugene, Oregon: Castalia; 1982. [Google Scholar]
- Pine DS, Cohen P, Johnson JG, Brook JS. Adolescent life events as predictors of adult depression. Journal of Affective Disorders. 2002;68:49–57. doi: 10.1016/S0165-0327(00)00331-1. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Kelley K. Effect sizes for mediation models: Quantitative strategies for communicating indirect effects. Psychological Methods. 2011;16:93–115. doi: 10.1037/a0022658. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- Radloff LS. The use of the center for epidemiologic studies of depression scale in adolescents and young adults. Journal of Youth and Adolescence. 1991;20:149–166. doi: 10.1007/BF01537606. [DOI] [PubMed] [Google Scholar]
- Radloff LS, Teri L. 6/Use of the center for epidemiological studies-depression scale with older adults. Clinical Gerontologist. 1986;5:119–136. doi: 10.1300/J018v05n01_06. [DOI] [Google Scholar]
- Reynolds CR. Concurrent validity of what I think and feel: The revised children’s manifest anxiety scale. Journal of Consulting and Clinical Psychology. 1980;48:774–775. doi: 10.1037/0022-006X.48.6.774. [DOI] [PubMed] [Google Scholar]
- Reynolds CR, Paget KD. National normative and reliability data for the revised children’s manifest anxiety scale. School Psychology Review. 1983;12:324–336. [Google Scholar]
- Reynolds CR, Richmond BO. What I think and feel: A revised measure of children’s manifest anxiety. Journal of Abnormal Child Psychology. 1978;6:271–280. doi: 10.1007/bf00919131. [DOI] [PubMed] [Google Scholar]
- Roberts RE, Andrews JA, Lewinsohn PM, Hops H. Assessment of depression in adolescents using the center for epidemiologic studies depression scale. Psychological Assessment: A Journal of Consulting and Clinical Psychology. 1990;2:122–128. doi: 10.1037/1040-3590.2.2.122. [DOI] [Google Scholar]
- Sander JB, McCarty CA. Youth depression in the family context: Familial risk factors and models of treatment. Clinical Child and Family Psychology Review. 2005;8:203–219. doi: 10.1007/s10567-005-6666-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider BH, Atkinson L, Tardif C. Child-parent attachment and children’s peer relations: a quantative review. Developmental Psychology. 2001;37(1):86–100. [PubMed] [Google Scholar]
- Stellard P, Velleman R, Langsford J, Baldwin S. Coping and psychological distress in children involved in road traffic accidents. British Journal of Clinical Psychology. 2001;40:197–208. doi: 10.1348/014466501163643. [DOI] [PubMed] [Google Scholar]
- Tofighi D, MacKinnon DP. RMediation: An R package for mediation analysis confidence intervals. Behavior Research Methods. 2011;43:692–700. doi: 10.3758/s13428-011-0076-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Lier PA, Koot HM. Developmental cascades of peer relations and symptoms of externalizing and internalizing problems from kindergarten to fourth-grade elementary school. Development and Psychopathology. 2010;22:569–582. doi: 10.1017/S09545794100000283. [DOI] [PubMed] [Google Scholar]
- Waters E, Cummings EM. A secure base from which to explore close relationships. Child Development. 2000;71:164–172. doi: 10.1111/1467-8624.00130. [DOI] [PubMed] [Google Scholar]