The majority (approx. 80%) of infant acute lymphoblastic leukemia (ALL) cases are characterized by chromosomal rearrangements involving the Mixed Lineage Leukemia (MLL, or KMT2A) gene, which confer a poor prognosis: chances of event-free survival are 30–40% at best.1 We and others showed subclonal RAS mutations occur in 14–36% of MLL-rearranged ALL cases, depending on MLL-translocation subtype.2–4 RAS mutations diminish survival chances even further, with rapid occurrence of relapses and essentially no chance of survival.3 Recently, we found that MEK inhibitors effectively killed RAS-mutant infant ALL cells in vitro, with trametinib being the most potent compound tested.5 We therefore proposed that trametinib could be beneficial for MLL-rearranged infant ALL patients harboring additional RAS mutations. Here we report pre-clinical evaluation of trametinib in an RAS-mutant MLL-rearranged infant ALL mouse xenograft model.
Since trametinib was previously investigated in mouse models for other malignancies and was accepted for treatment of BRAF-mutant melanoma,6,7 we based our dosing regime on these studies, administering 5 mg/kg (low) or 30 mg/kg (high) trametinib 3 times per week through intraperitoneal injection in a toxicity assessment (n=3 mice per group). Within a week, 2 of 3 mice in the 30 mg/kg trametinib group died, while the final mouse was humanely euthanized due to weight loss. The vehicle and 5 mg/kg trametinib doses were tolerable for up to 28 days, without signs of discomfort or weight loss (Online Supplementary Figure S1A). One of the trametinib mice was smaller than its littermates, but there were no indications to exclude it from the study. Hematoxylin & eosin (HE) staining of tissue slices revealed that high trametinib dosing induced kidney damage, which was absent in the vehicle and low trametinib groups (Online Supplementary Figure S1B). Surprisingly, high-dose trametinib also resulted in enhanced abundance of myeloid cells in the spleen (Online Supplementary Figure S1C), which resembled splenic extramedullary hematopoiesis (EMH).8 Moreover, we observed hematopoietic cell depletion in bone marrows of mice that received low trametinib doses, while this did not occur in the vehicle-treated mice (Online Supplementary Figure S1D). Although bone marrow tissue for high-dose trametinib was unavailable, possibly high-dose trametinib induces more severe bone marrow depletion, evoking splenic EMH.
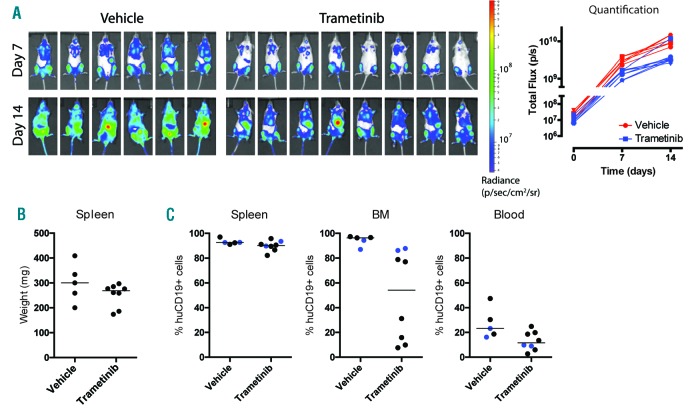
To assess the efficacy of trametinib in vivo, we transplanted NSG mice with the RAS-mutant MLL-rearranged infant ALL cell line KOPN8 (106 cells; tail-vein injection), previously transduced with a luciferase-reporter (from here on referred to as KOPN8-SLIEW). Subsequently, 1-week engraftment was assessed through intra-vital imaging. After randomization, vehicle or trametinib treatment (5 mg/kg, 3 times per week) commenced and leukemia progression was tracked by weekly intra-vital imaging. In both the vehicle- and trametinib-treated mice, systemic leukemia developed over a period of two weeks, although more severely in the vehicle mice, most evidently on day 14 (Figure 1A, left). Quantification of the intra-vital imaging revealed trametinib monotherapy delayed leukemia progression, but was insufficient to prevent leukemia out-growth (Figure 1A, right). The modest effect of trametinib on leukemia progression led us to investigate whether its mechanism of action was achieved at all in our model. Therefore, four hours before sacrificing the mice (day 17), 2 mice from the vehicle group and 2 mice from the trametinib group were randomly selected to receive a bolus injection of trametinib (5 mg/kg) for analysis of ERK activation in tissue samples later. Spleen, bone marrow and peripheral blood samples were extracted from all mice. As expected from the intra-vital imaging data, both treatment groups presented with splenomegaly, without a significant difference in spleen weight (Figure 1B and Online Supplementary Figure S2A). After processing the tissues, the presence of leukemic cells was analyzed using flow cytometry. (See Online Supplementary Figure S2B for example gating).
Figure 1.
RAS-mutant MLL-rearranged leukemia progression is tempered by trametinib. (A) Intra-vital imaging of KOPN8-SLIEW transplanted mice receiving either vehicle or trametinib treatment. (Left) Images were acquired on day 7 (top) and day 14 (bottom), and presented using the same luminescent scale (right). Quantification of intra-vital imaging data of each individual mouse from the vehicle and trametinib groups (red and blue, respectively), as measured on day 0 (pre-treatment), day 7 and day 14. Data are presented as photonic flux (i.e. the number of emitted photons per second). (B) Spleen weights of vehicle and trametinib mice. (C) Percentages of leukemic (huCD19+/MsCd45−/Ter119−) cells detected in spleen, bone marrow and peripheral blood (left, center and right, respectively). Data from mice that received a trametinib bolus are indicated as blue dots.
The majority of cells derived from either vehicle- or trametinib-treated spleens represented human leukemia cells (Figure 1C, left). However, the leukemic load in bone marrow aspirates was reduced to 10–30% in 4 of 8 trametinib-treated mice, while the remaining mice presented with leukemic bone marrows similar to the vehicle-treated group (80–95%) (Figure 1C, center). Additionally, we observed a reduction of leukemic cells in the peripheral blood of trametinib-treated mice compared to vehicle (12% and 23%, respectively), although this difference was not statistically significant (Figure 1C, right). The mice that received a trametinib bolus-injection (blue dots) were comparable to the non-bolus mice. The bimodal effect observed in bone marrow aspirates did not correlate with sex, total or spleen weight, leukemic cells in the peripheral blood or age (Online Supplementary Figure S2C).
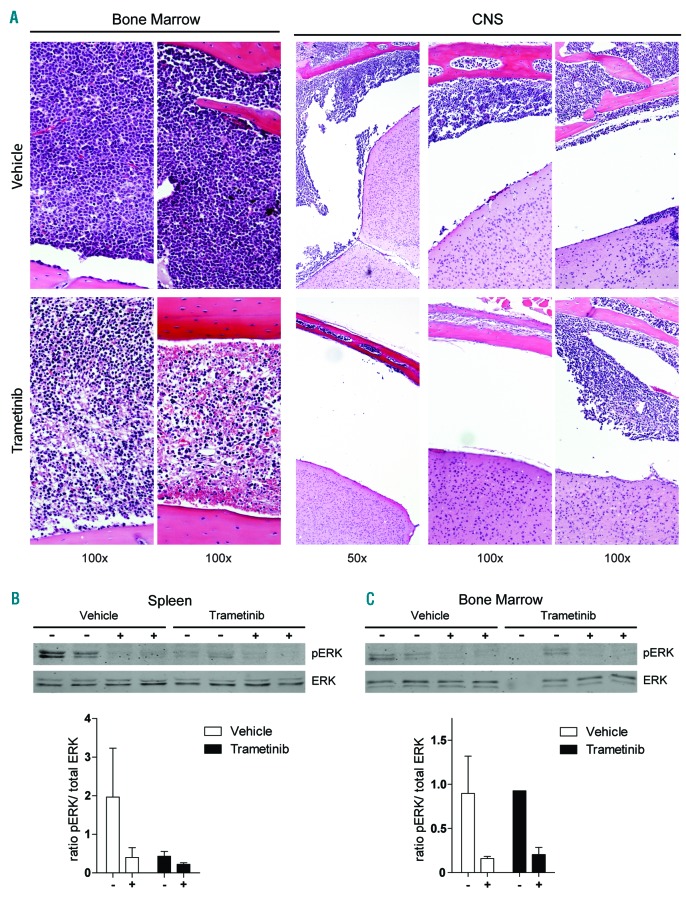
To further investigate leukemic cell distribution in the bone marrows of vehicle- and trametinib-treated mice, we performed HE staining on bone marrow tissue slices. Interestingly, in the vehicle bone marrows, we observed severe leukemic cell infiltration, whereas the selected bone marrows of trametinib-treated mice, with reduced leukemic load, actually showed hypocellularity (Figure 2A, left). Although these hypocellular bone marrows differ from healthy bone marrow, this is likely due to trametinib-induced leukemic cell death rather than toxicity, as suggested by the approval of trametinib for metastatic melanoma and recent clinical studies in other hematologic diseases.9
Figure 2.
Trametinib impinges on niche distribution of RAS-mutant MLL-rearranged ALL cells and reduces ERK phosphorylation in vivo. (A) Hematoxylin & eosin (HE) stained bone marrow slides from 2 vehicle (top left) and 2 trametinib (bottom left) treated mice. HE stained slices from the skull of 3 vehicle-treated (top right) and 3 trametinib-treated (bottom right) mice. (B) (top) pERK and total ERK levels were analyzed by western blot in MACS-enriched spleen isolates from vehicle or trametinib mice. Bolus trametinib injection samples are indicated by ‘+’. (Bottom) The pERK/total ERK ratio as quantified from the western blot. (C) (Top) pERK and total ERK levels determined by western blot of MACS-enriched bone marrow aspirates. Samples from mice that received a bolus trametinib injection are indicated by ‘+’. (Bottom) The pERK/total ERK ratio as quantified from the western blot. Quantification data are presented as mean+Standard Deviation.
Since RAS mutations in MLL-rearranged infant ALL have been implicated with enhanced central nervous system (CNS) infiltration,10 we investigated fixated skull sections for presence of leukemic cells. Interestingly, trametinib substantially reduced leukemia infiltration into the leptomeningeal space in 2 of 3 trametinib-treated mice, whereas all vehicle mice presented with cell invasion (Figure 2A, right).
We electrophoretically resolved protein lysates of spleen and bone marrow samples and investigated ERK dephosphorylation as marker of trametinib efficacy. Interestingly, vehicle non-bolus spleen samples had evident ERK phosphorylation (pERK), while the vehicle mice that received a bolus presented with markedly lower pERK signal (Figure 2B, top). Moreover, trametinib inhibited ERK phosphorylation in all spleen isolates, both by successive trametinib injections (black bars), as well as a single bolus injection in vehicle group mice (white bars), as was confirmed by quantifying the relative pERK signal of these blots (Figure 2B, bottom). Additionally, the bone marrow samples of bolus and non-bolus mice (before purification by magnetic-activated cell sorting; MACS) contained comparable percentages of leukemic cells (Online Supplementary Figure S3A). Interestingly, the vehicle bone marrow samples showed a similar ERK phosphorylation pattern to the spleen samples, with the trametinib bolus lowering the pERK level (Figure 2C, top), while in the trametinib group, the bolus injection was also accompanied by reduced ERK phosphorylation. Quantifying the blots revealed that in non-bolus bone marrows there was little difference between the vehicle and trametinib groups, though a bolus of trametinib effectively diminished ERK phosphorylation (Figure 2C, bottom). Hence, successive trametinib treatment did not result in maintained pERK reduction, as observed in the spleen, but bolus trametinib injections transiently decreased pERK levels in the bone marrow.
Although MEK inhibition previously proved effective in RAS-mutant BCP-ALL xenograft model, trametinib could not substantially inhibit leukemia progression in our MLL-rearranged infant ALL model.11 However, trametinib treatment did impinge on engraftment localization, specifically bone marrow and brain infiltration of RAS-mutant MLL-rearranged ALL cells. The difference in efficacy of MEK inhibition between RAS-mutant MLL-rearranged ALL and BCP-ALL might be explained by differences in cytogenetic subtype and associated outcome.
Interestingly, Prieto et al. showed that in mouse xenografts of human MLL-rearranged ALL cell line SEM, ectopic expression of KRASG12V significantly promoted CNS infiltration, which together with our data suggests MEK inhibition might diminish CNS involvement.10 Furthermore, MEK inhibitor selumetinib significantly reduced CNS infiltration in a pediatric RAS-mutant BCP-ALL xenograft model.11
Spleen-derived leukemic cells from the trametinib group showed sustained reduced pERK levels, whereas a bolus trametinib injection could also reduce pERK in the vehicle group. Furthermore, we observed bone marrow hypocellularity in 4 of 8 mice after trametinib treatment, while ERK phosphorylation was reduced after a trametinib bolus in the mice with highly leukemic bone marrows. Possibly trametinib clearance reduces its effect or alternate signaling mechanisms restore pERK, and our dosing frequency is too low to induce sustained inhibition of ERK phosphorylation. Although more frequent dosing might improve efficacy, there is a risk for toxicity. However, other studies in patient-derived solid tumor xenografts have used daily oral dosing regimes (0.3–3 mg/kg), and while we chose intraperitoneal administration to better control trametinib levels, these protracted studies for some models resulted in better efficacy than we observed.
Survival chances for MLL-rearranged infant ALL patients carrying RAS mutations are close to zero.3 Since trametinib reduces ERK phosphorylation, a key downstream effect of mutant RAS, this implies that trametinib treatment could revert the effect of RAS mutations in MLL-rearranged ALL, inducing a response to standard therapy that more resembles RAS-wild-type MLL-rearranged ALL. Moreover, glucocorticoid resistance remains a detrimental feature of MLL-rearranged infant ALL, and is associated with RAS mutations.1,3,12,13 Previously, we and others have shown that MEK inhibitors trametinib, selumetinib and MEK162 could sensitize ALL to glucocorticoids.5,14,15 This suggests that combination therapy of trametinib with glucocorticoids could be beneficial.
In conclusion, though trametinib monotherapy was unable to systemically inhibit RAS-mutant MLL-rearranged ALL in vivo, bone marrow leukemic burden was reduced in half of the mice, and trametinib effectively reduced ERK phosphorylation in leukemic cells from bone marrows and spleens. This illustrates the potential value of MEK inhibitors through reduction of CNS infiltration and possible potentiation of glucocorticoid sensitivity.
Supplementary Material
Footnotes
Information on authorship, contributions, and financial & other disclosures was provided by the authors and is available with the online version of this article at www.haematologica.org.
References
- 1.Pieters R, Schrappe M, De Lorenzo P, et al. A treatment protocol for infants younger than 1 year with acute lymphoblastic leukaemia (Interfant-99): an observational study and a multicentre randomised trial. Lancet. 2007;370(9583):240–250. [DOI] [PubMed] [Google Scholar]
- 2.Andersson AK, Ma J, Wang J, et al. The landscape of somatic mutations in infant MLL-rearranged acute lymphoblastic leukemias. Nat Genet. 2015;47(4):330–337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Driessen EM, van Roon EH, Spijkers-Hagelstein JA, et al. Frequencies and prognostic impact of RAS mutations in MLL-rearranged acute lymphoblastic leukemia in infants. Haematologica. 2013;98(6):937–944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Emerenciano M, Barbosa Tda C, de Almeida Lopes B, Meyer C, Marschalek R, Pombo-de-Oliveira MS. Subclonality and prenatal origin of RAS mutations in KMT2A (MLL)-rearranged infant acute lymphoblastic leukaemia. Br J Haematol. 2015;170(2):268–271. [DOI] [PubMed] [Google Scholar]
- 5.Kerstjens M, Driessen EM, Willekes M, et al. MEK inhibition is a promising therapeutic strategy for MLL-rearranged infant acute lymphoblastic leukemia patients carrying RAS mutations. Oncotarget. 2016;8(9):14835–14846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Walters DM, Lindberg JM, Adair SJ, et al. Inhibition of the growth of patient-derived pancreatic cancer xenografts with the MEK inhibitor trametinib is augmented by combined treatment with the epidermal growth factor receptor/HER2 inhibitor lapatinib. Neoplasia. 2013;15(2):143–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Menzies AM, Long GV. Dabrafenib and trametinib, alone and in combination for BRAF-mutant metastatic melanoma. Clin Cancer Res. 2014;20(8):2035–2043. [DOI] [PubMed] [Google Scholar]
- 8.National-Toxicology-Program. Spleen - Extramedullary Hematopoiesis. 2015. [Available from: https://ntp.niehs.nih.gov/nnl/immune/spleen/exmh/spleen-extramedullary-hematopoiesis-pdf_508.pdf]
- 9.Nordmann TM, Juengling FD, Recher M, et al. Trametinib after disease reactivation under dabrafenib in Erdheim-Chester disease with both BRAF and KRAS mutations. Blood. 2017;129(7):879–882. [DOI] [PubMed] [Google Scholar]
- 10.Prieto C, Stam RW, Agraz-Doblas A, et al. Activated KRAS Cooperates with MLL-AF4 to Promote Extramedullary Engraftment and Migration of Cord Blood CD34+ HSPC But Is Insufficient to Initiate Leukemia. Cancer Res. 2016;76(8):2478–2489. [DOI] [PubMed] [Google Scholar]
- 11.Irving J, Matheson E, Minto L, et al. Ras pathway mutations are prevalent in relapsed childhood acute lymphoblastic leukemia and confer sensitivity to MEK inhibition. Blood. 2014;124(23):3420–3430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pieters R, den Boer ML, Durian M, et al. Relation between age, immunophenotype and in vitro drug resistance in 395 children with acute lymphoblastic leukemia–implications for treatment of infants. Leukemia. 1998;12(9):1344–1348. [DOI] [PubMed] [Google Scholar]
- 13.Dordelmann M, Reiter A, Borkhardt A, et al. Prednisone response is the strongest predictor of treatment outcome in infant acute lymphoblastic leukemia. Blood. 1999;94(4):1209–1217. [PubMed] [Google Scholar]
- 14.Rambal AA, Panaguiton ZL, Kramer L, Grant S, Harada H. MEK inhibitors potentiate dexamethasone lethality in acute lymphoblastic leukemia cells through the pro-apoptotic molecule BIM. Leukemia. 2009;23(10):1744–1754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Polak A, Kiliszek P, Sewastianik T, et al. MEK Inhibition Sensitizes Precursor B-Cell Acute Lymphoblastic Leukemia (B-ALL) Cells to Dexamethasone through Modulation of mTOR Activity and Stimulation of Autophagy. PLoS One. 2016;11(5):e0155893. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.