Abstract
Background
WeChat is a convenient and popular social medium, and it seems to be an appropriate platform for education and management of patients. This study sought to identify usefulness in clinical control of cough-variant asthma (CVA).
Material/Methods
A randomized controlled trial was conducted among 80 CVA patients. After being assigned to either the traditional group (TG) or the WeChat group (WG), they received the same inhalation therapy, but patients in WG received additional education and instruction via our public account on the WeChat application. Questionnaires on asthma and chronic cough, data on pulmonary function, blood-related items, follow-up adherence, and Emergency Department (ED) visits were collected at the initial visit and at 3 months.
Results
A total of 67 participants completed the trial for analysis. FEV1/predicted and FEV1/FVC were significantly increased in WG (p<0.001; p=0.012) after 3 months. PD20-FEV1 was increased in both groups compared with baseline, but more pronounced in WG (p=0.004). ACQ-7 scores were improved in both groups (p=0.024; p<0.001). Participants allocated to WG experienced a greater improvement in AQLQ and LCQ scores, and between-group differences were significant at 3 months (p=0.040; p=0.001). Furthermore, we observed decreases in blood eosinophil count and FeNO in WG (p=0.048; p=0.014), and WG presented better follow-up compliance (p=0.034).
Conclusions
Using WeChat as part of treatment and management of CVA can help patients learn about their disease and medications, as well as improve disease control and therapy outcomes.
MeSH Keywords: Asthma, Cellular Phone, Cough, Mobile Applications, Quality of Life, Respiratory Function Tests
Background
Cough-variant asthma (CVA), a subtype of bronchial asthma, is considered to be one of the most common causes of chronic cough among adults worldwide [1]. CVA differs from classic asthma, usually manifesting a symptom of only coughing without wheezing or dyspnea and particularly coughing at night. With less clinical manifestation and medical intervention, CVA patients are usually overlooked, and 30–40% of them will develop to classic asthma in the next few years [2]. Having the same pathobiologic basis, eosinophilic inflammation, and bronchial hyper-responsiveness as is involved in classic asthma, CVA patients are often administered inhaled corticosteroids (ICS) or a combination of inhaled corticosteroids and long-acting beta-agonists (ICS/LABA) to relieve the intractable cough [3,4]. To delay or control the progression of CVA to classic asthma is the first-line defense in prevention and treatment of bronchial asthma. However, poor long-term compliance of patients in follow-up results in poor prognosis of CVA.
With the rapid development of information technology, smartphones have been enthusiastically adopted by the general public. There have been several clinical studies conducted using smartphone applications (apps) for health management [5]. Among instant messaging apps, WeChat is a free, cross-platform app widely used for sending text, voice, video, and photos to friends and family [6]. After first being launched in January 2011, it gradually attracted nearly 846 million monthly active users by the third quarter of 2016 [7]. Conveniently, users can subscribe to public or official accounts on the WeChat platform to acquire selected news or information.
Health education has proven to be an effective approach to chronic disease prevention and treatment [8,9]. However, traditional health education for out-patients is often limited to clinics, usually leading to poor self-management and medication adherence. Thus, patients experience relatively lower treatment efficacy. To overcome this dilemma, we used WeChat public accounts as an educational and follow-up tool to educate and instruct CVA out-patients in this study, to determine if patients could benefit from this new method.
Material and Methods
Patients
We planned to enroll 100 patients for this study. All the patients were first physician-diagnosed with CVA according to accepted guidelines and had never used glucocorticoids before treatment. Owning a smartphone and having an active WeChat account were also necessary for participation. Exclusion criteria were: unable to communicate, illiterate, having cancer or serious cardiovascular disease, having cognitive impairment or serious psychiatric conditions, and being addicted to drugs.
Ethical approval
The study was approved by the Ethics Committee of the Second Affiliated Hospital of Zhejiang University and was registered in the Chinese Clinical Trial Registry at www.chictr.org (registration number: ChiCTR-INR-17011077). All participants informed verbally prior to obtaining written informed consent, and the study was conducted in accordance with the Helsinki Declaration and Good Clinical Practice guidelines.
Study design
Eighty eligible CVA out-patients from August 2016 to June 2017 were enrolled and randomly assigned to 1 of 2 groups: the traditional group and the WeChat group (Figure 1). Each group received the same therapy: fixed-dose combination of inhaled corticosteroids (ICS) and long-acting β2-agonists (LABA). All participants in the study were only treated with budesonide/formoterol for 3 months. Data on demographic information, Asthma Control Questionnaire (ACQ), Asthma Quality of Life Questionnaire (AQLQ), Leicester Cough Questionnaire (LCQ), pulmonary function, fractional exhaled nitric oxide (FeNO), blood cell counts, total immunoglobulin E (IgE), follow-up adherence rate, and Emergency Department (ED) visits or hospitalization were collected at the initial visit (V0) and the end of the study (V1).
Figure 1.
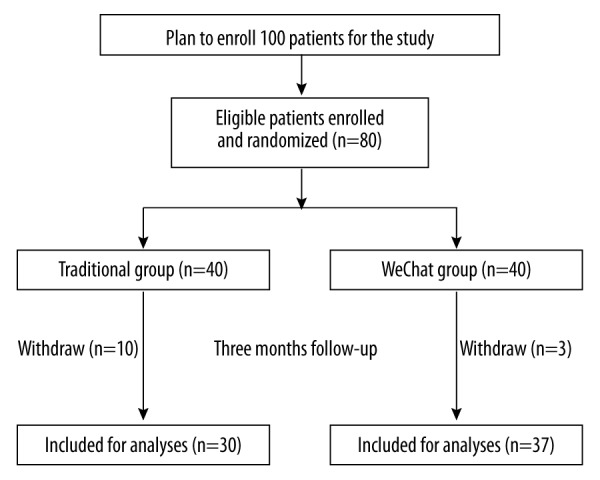
Flow of participants through the study.
Traditional group (TG)
Participants in this group received education on cough-variant asthma and usage of inhaler equipment by physicians or pharmacist at the initial visit. They were told to revisit the clinic after completing 3 months of treatment.
WeChat group (WG)
In addition to receiving traditional education as TG, participants in this group were invited to subscribe to the WeChat public account “Assistant of Respiratory Diseases” on their smartphone. On this public platform, participants can read educational articles about asthma and watch the online videos about various inhaler equipment for self-education. Conveniently, messages, voices, and videos can be left on the platform and be replied to by physicians within 48 hours. Messages are sent to patients to remind them to perform drug inhalation. A timer helped participants remember the time for drug usage every day and provided data about the next visit.
WeChat public account
Established in June 2016, “Assistant of Respiratory Diseases” was a public account in WeChat. It is a platform aiming to educate and communicate with patients who suffer from chronic airway diseases such as asthma, chronic obstructive pulmonary disease, and obstructive sleep apnea hypopnea syndrome. A subscriber can fill in the questionnaires online, and watch the instructional videos of inhaler equipment on this platform (Supplementary Figure 1). To avoid the influences of confounding factors, only participants who were invited can subscribe to the WeChat public account.
Statistical methods
Data analysis was conducted using SPSS, Version 19 (SPSS Inc., Chicago, IL, USA). The results for each variable are shown as mean ± standard deviation in the case of continuous variables, and as the number of cases per category and frequency of responses in the case of categorical variables. For the comparison of outcomes between baseline and 3 months, we used the paired t test. For the comparisons of categorical data, we used the chi-squared test. Pearson’s correlation test was used to examine the association between changes in ACQ and AQLQ. All statistical tests were two-sided and p values of 0.05 or less were considered to indicate statistical significance.
Results
A total of 80 participants met the inclusion criteria and were enrolled in the study, and then were randomized into 2 groups. Age ranged from 21 to 67 years old in all groups. After 3 months of follow-up, 67 participants completed the study and were analyzed (30 in the traditional group and 37 in the WeChat group) (Figure 1). All patients in the 2 groups had similar baseline characteristics, as shown in Table 1.
Table 1.
Baseline characteristics of patients with CVA.
| Patient characteristics | Traditional group (n=30) | WeChat group (n=37) | P |
|---|---|---|---|
| Anthropometric data | |||
| Gender (female/male) | 24/6 | 28/9 | 0.673 |
| Age, year; mean (SD) | 41.4 (12.0) | 39.1 (14.3) | 0.485 |
| BMI, kg/m2; mean (SD) | 22.3 (2.7) | 22.3 (3.4) | 0.932 |
| Education less than high school, n (%) | 24 (80.0) | 26 (70.3) | 0.363 |
| Duration of CVA, month; mean (SD) | 19.5 (36.0) | 20.4 (33.4) | 0.238 |
| Current smoker, n (%) | 3 (10.0) | 2 (5.4) | 0.477 |
| Current Second-hand smoker, n (%) | 16 (53.3) | 19 (61.3) | 0.872 |
| Atopic, n (%) | 12 (40.0) | 15 (40.5) | 0.964 |
| Allergic rhinitis | 11 | 14 | |
| Urticaria | 2 | 3 | |
| Allergic conjunctivitis | 0 | 1 | |
| Total-IgE, IU/ml; median (25th–75th) | 97.2 (38.0–324.8) | 87.3 (29.1–329.0) | 0.841 |
| FeNO, ppb; median (25th–75th) | 20 (12–31) | 22 (14–43) | 0.420 |
| Blood | |||
| Eosinophils,%; median (25th–75th) | 2.75 (1.33–3.85) | 2.60 (1.25–4.35) | 0.767 |
| Neutrophils,%; median (25th–75th) | 56.0 (50.4–63.2) | 55.6 (51.7–64.4) | 0.850 |
| Pulmonary function | |||
| FEV1/predicted,%; mean (SD) | 83.6 (8.6) | 82.2 (8.7) | 0.442 |
| FEV1/FVC,%; mean (SD) | 81.3 (7.5) | 79.2 (7.3) | 0.188 |
| PD20-FEV1, mg; median, mean (SD) | 0.80 (0.69) | 0.77 (0.65) | 0.865 |
| ACQ-7; mean (SD) | 2.04 (0.81) | 1.96 (0.56) | 0.972 |
| AQLQ; mean (SD) | 5.49 (0.59) | 5.43 (0.76) | 0.796 |
| LCQ; mean (SD) | 12.69 (2.14) | 12.69 (1.65) | 0.920 |
| Social; mean (SD) | 5.00 (1.01) | 4.92 (0.84) | 0.721 |
| Psychological; mean (SD) | 3.71 (0.89) | 3.63 (0.85) | 0.724 |
| Physiological; mean (SD) | 3.98 (0.96) | 4.14 (0.71) | 0.441 |
Data are presented as mean (SDs) unless otherwise stated. BMI – body mass index; FEV1 – forced expiratory volume in 1 second; PD20-FEV1 – the cumulative dose of methacholine provoking a 20 percent decline in FEV1; FVC – forced vital capacity; IgE – immunoglobulin E; FeNO – fractional exhaled nitric oxide; ppb – parts per billion; ACQ – Asthma Control Questionnaire; AQLQ – Asthma Quality of Life Questionnaire; LCQ – Leicester Cough Questionnaire.
Pulmonary function
All participants experienced an increased percentage of FEV1/predicted and FEV1/FVC (Table 2, Supplementary Figure 2), but WG (p<0.001; p=0.012) was more pronounced than TG (p=0.143; p=0.177). However, the intervention on FEV1/FVC had no difference between groups (p=0.654). At baseline, 49 patients were classified as having mild airway hyper-responsiveness (AHR) and 18 were classified as having moderate to severe AHR. At the V1, 2 patients (in TG) were not able to perform the bronchial provocation test because of chest distress and dizziness. After 3 months of treatment, the BHR was decreased in both groups, with an increase in PD20-FEV1 (TG: p=0.002; WG: p<0.001), and the p value of between-group difference was 0.004 (Figure 2). There were 11 patients with negative results after provocation test in TG and 24 patients in WG (p=0.022).
Table 2.
Mean changes in outcomes from the baseline (V0) to the end of the study (V1).
| Outcomes | Traditional group (n=30) | WeChat group (n=37) | P value between-group difference | ||||||
|---|---|---|---|---|---|---|---|---|---|
| V0 | V1 | Mean (95% CI) within-group difference | P value | V0 | V1 | Mean (95% CI) within-group difference | P value | ||
| Total-IgE (IU/ml) | 191.2 (112.8, 324.8) | 209.2 (115.1, 303.4) | −7.15 (−24.3, 10.0) | 0.923 | 248.4 (117.0, 379.8) | 189.4 (96.5, 282.3) | −59.0 (−130.8, 12.7) | 0.627 | 0. 200 |
| FeNO (ppb) | 24.9 (18.4, 31.5) | 20. 7 (16.3, 25.2) | −4.2 (−7.9, −0.64) | 0.539 | 28.1 (22.4, 33.7) | 17.5 (14.6, 20.5) | −10.5 (−14.5, −6.5) | 0.014 | 0.033 |
| Blood (%) | |||||||||
| Eosinophils | 3.08 (2.19, 3.97) | 2.61 (1.96, 3.25) | −0.47 (−0.99, 0.04) | 0.668 | 3.35 (2.48, 4.23) | 2.20 (1.65, 2.74) | −1.16 (−1.90, −0.14) | 0.048 | 0.183 |
| Neutrophils | 57.1 (54.0, 60.2) | 57.5 (55.8, 59.3) | 0.47 (−2.4, 3.4) | 0.929 | 56.2 (53.3, 59.1) | 58.8 (56.3, 61.2) | 2.6 (0.27, 4.8) | 0.134 | 0.484 |
| Pulmonary function (%) | |||||||||
| FEV1/predicted | 83.64 (80.43, 86.86) | 87.88 (84.14, 91.63) | 4.24 (−0.08, 8.56) | 0.143 | 82.23 (79.32, 85.15) | 93.50 (90.70, 96.31) | 11.27 (8.01, 14.53) | <0.001 | 0.023 |
| FEV1/FVC | 81.25 (78.51, 83.99) | 84.47 (80.82, 88.12) | 3.17 (0.47, 5.89) | 0.177 | 79.20 (76.77, 81.62) | 83.95 (81.12, 86.78) | 4.76 (2.21, 7.30) | 0.012 | 0.654 |
| ACQ-7 | 2.06 (1.76, 2.35) | 1.60 (1.39, 1.81) | −0.46 (−0.69, −0.23) | 0.024 | 2.04 (1.82, 2.25) | 1.38 (1.23, 1.52) | −0.66 (−0.87, −0.45) | <0.001 | 0.145 |
| AQLQ | 5.49 (5.27, 5.71) | 5.70 (5.53, 5.88) | 0.21 (−0.01, 0.43) | 0.128 | 5.43 (5.18, 5.69) | 6.04 (5.92, 6.16) | 0.60 (0.38, 0.83) | <0.001 | 0.040 |
| LCQ (total) | 12.69 (11.89, 13.49) | 13.51 (12.82, 14.20) | 0.82 (0.45, 1.19) | 0.117 | 12.69 (12.14, 13.24) | 14.43 (13.98, 14.88) | 1.74 (1.29, 2.19) | <0.001 | 0.001 |
| Social | 5.00 (4.62, 5.38) | 5.34 (4.81, 5.48) | 0.14 (−0.09, 0.38) | 0.661 | 4.92 (4.64, 5.20) | 5.33 (5.10, 5.57) | 0.41 (0.20, 0.63) | 0.297 | 0.050 |
| Psychological | 3.71 (3.39, 4.04) | 4.25 (3.97, 4.53) | 0.54 (0.30, 0.79) | 0.006 | 3.63 (3.34, 3.91) | 4.63 (4.35, 4.92) | 1.00 (0.68, 1.33) | <0.001 | 0.044 |
| Physiological | 3.98 (3.63, 4.34) | 4.12 (3.82, 4.41) | 0.13 (−0.08, 0.35) | 0.871 | 4.14 (3.90, 4.38) | 4.47 (4.28, 4.65) | 0.32 (0.16, 0.48) | 0.053 | 0.096 |
Data are presented as mean (95% CI) unless otherwise stated.
Figure 2.
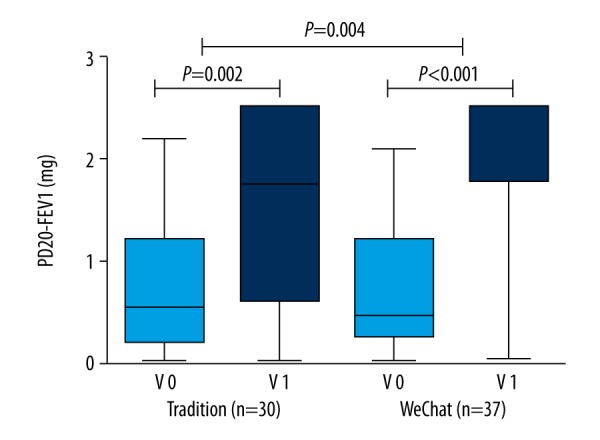
Change of PD20-FEV1 in 2 groups.
Clinical asthma control and asthma quality of life
According to ACQ-7 at baseline, 17 patients were classified as having partially controlled asthma (score 0.75–1.5) and others were classified as having uncontrolled asthma (score>1.5). Both groups presented improvements in asthma control (TG: p=0.024; WG: p<0.001) at 3 months, but WG did not show better control than TG (p=0.145) (Table 2, Supplementary Figure 2). Within-group difference of WG (p<0.001) and between-group differences (p=0.040) were observed in AQLQ total score. There was no significant linear relationship between the improvement in ACQ and AQLQ in TG group (r=−0.254, p=0.478); however, it had a significant linear relationship in the WG group (r=−0.518, p=0.022).
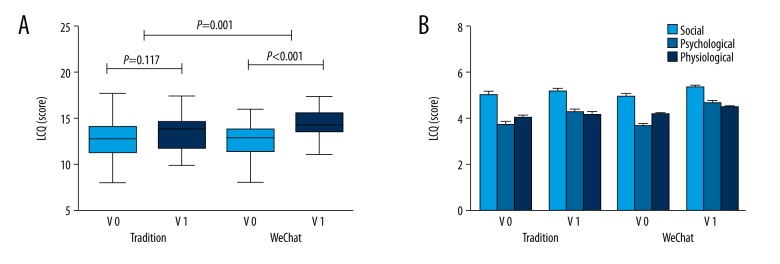
Leicester cough questionnaire
After 3-months follow-up, the TG group and WG group both presented increased scores in LCQ, but compared with baseline, the WG group (p<0.001) showed a better improvement than in the TG group (p=0.117). Between-group differences were observed in LCQ total score (p=0.050) (Table 2, Figure 3). Psychological score in LCQ was increased significantly in both groups (TG: p=0.006; WG: p<0.001) and the WG group manifested a remarkable increase in social and psychological scores of the LCQ (p=0.044; p=0.050).
Figure 3.
Effects of WeChat intervention on (A): LCQ; (B) Social, psychological and physiological scores of LCQ.
Blood cell counts
Eosinophils count was decreased in WG (p=0.048); however, no significant difference in decrease in eosinophils was observed between groups (p=0.183). WeChat applied follow-up had no influence on fluctuating neutrophil count (Table 2, Supplementary Figure 2).
Total-IgE and FeNO
The TG and WG demonstrated similar baseline levels of total-IgE and FeNO. However, the intervention did not induce a significant change in total-IgE for either TG (p=0.923) or WG (p=0.627) (Table 2, Supplementary Figure 2). FeNO was decreased in WG (p=0.014), and the differences between groups were significant (p=0.033).
Follow-up adherence and ED visits (or hospitalization)
The follow-up adherence rates were 75% and 92.5%, respectively, which were significantly different between the 2 groups (p=0.034). More CVA patients who received the WeChat educational intervention came back for the follow-up visit than those receiving traditional education intervention (Figure 4). Details of reasons for patient withdraw are shown in Supplementary Table 1. There was 1 patient who once visited the Emergency Department (ED) and 2 patients needed hospitalization for control of asthma in TG, and 2 patients in WG visited the ED for uncontrollable cough. However, the incidence of ED visits or hospitalization did not differ significantly between the 2 groups (p=0.510, Figure 4). Medication adherence was good in both groups (p>0.05) (data not shown).
Figure 4.
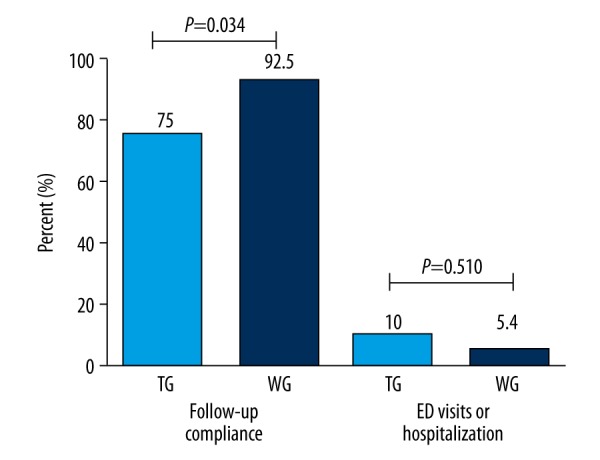
Follow-up adherence and ED visits (or hospitalization) in 2 groups.
Discussion
Many patients present at clinics complain of chronic and persistent cough. Due to lack of accurate diagnosis of CVA, most of these patients received improper treatment and developed repeat cough-related symptoms or even progressed to typical asthma. Given the role of WeChat in patient follow-up education, our aim was to enhance the management and treatment effect of CVA patients. Furthermore, we explored an innovative management mode in order to provide a better approach for long-term management of chronic airway diseases. In this study, a WeChat public account was used as a platform for education and management of CVA patients, and during 3 months of treatment it showed unique advantages over the traditional treatment.
In clinical practice, inhalation therapy plays a critical role in the treatment of asthma. Incorrect use of inhalers may increase risk of uncontrolled asthma states, unwanted adverse effects, and higher treatment costs [10]. Unfortunately, the condition of incorrect inhaler technique has not been improved over the past 40 years, and the overall prevalence of correct inhaler technique was only 31% on average [11]. During drug inhalation, the technique and dosage/frequency of medications are the cornerstones of successful treatment. In this study, instructional video clips of 3 commonly used ICS/LABA inhalers – salmeterol xinafoate/fluticasone propionate (Seretide®), budesonide/formoterol (Symbicort Turbuhaler®) and beclomethasone dipropionate/formoterol fumarate (Foster®) – were provided to patients on the WeChat platform (Supplementary Figure 1, patients were only treated with budesonide/formoterol in this study). An auto-reminder message was sent to each patient’s smartphone individually for the time of drug usage every day, so as to guarantee accurate inhaled doses. According to a former report, instructions must be repeated at least 3 times to achieve effective inhalation skills [12]. However, at clinics, the usage of inhalers was demonstrated to each patient only once by physicians or pharmacists. This is clearly insufficient, and this traditional education is usually received by patients with poor self-management. Insufficient therapeutic effects then usually lead to exacerbation or destabilization of asthma. Thus, mastering the correct inhaler use skill and taking correct doses are the premise of asthma therapy. WeChat platform subscribers could watch the standard instructive videos repeatedly for self-education and inhale their drugs on time by getting reminders. It is more convenient and efficient for both patients and doctors.
In our study, some clinical and symptomatic questionnaire items showed significant improvements in WG compared with traditional management of patient education. The WeChat group had better asthma-related scores (ACQ, AQLQ, and LCQ) and a pronounced FeNO level decline compared to the traditional group. This may show that participants in WG benefited from instruction by WeChat platform interaction. A decline of fractional nitric oxide concentration in exhaled breath (FeNO) was observed in WG (p=0.010). FeNO is a simple and safe method of measuring eosinophilic airway inflammation, and CVA patients with high FeNO levels tend to have more cough-related symptoms [13,14]. This may mean that participants could achieve better recovery from use of the WeChat platform assistant in both asthma-related symptoms and airway inflammation. Follow-up adherence increased in WG, which may be why more patients in WG mastered correct inhaler use skills, as reported previously [12]. The WeChat public, account as an asthma therapy supervisor and reminder, contributed to a better follow-up adherence for WG. WeChat-based health education services had positive effects on therapy outcomes. In our study, cough symptoms and pulmonary function were improved after ICS/LABA therapy, especially for patients using WeChat, and psychological conditions also improved. Mental disorders are associated with poorly controlled asthma, and CVA patients are on average more depressed and anxious than classic asthma patients [2]. Hence, with the help of our WeChat platform, CVA patients could learn more about the disease itself. Moreover, it will gradually strengthen their confidence when confronted with illness. With this benign psychological stimulation, patients obtained more benefits from the whole treatment.
It has been reported that a combination of long-acting β2-adrenergic agonist (LABA) and corticosteroid had potent effects in relieving symptoms of CVA [15]. Current guidelines state that the principles for CVA treatment are identical to those for classic asthma: a combination of low-dose ICS and bronchodilators, along with short-term oral glucocorticoid if necessary. In our study, all the participants received the same dose of budesonide/formoterol, but the findings of this study should be interpreted in light of its possible limitations. First, the study was conducted at a single center and the sample size was limited. Second, it is suggested that the fundamental pathophysiological characteristics of CVA are identical to those of classic asthma [16,17]; therefore, further research is needed on whether CVA should be divided into different phenotypes such as classic asthma. Third, airway inflammation is a major factor in the pathogenesis of asthma, and asthma control was associated with fluctuations in sputum eosinophil counts [18,19]. Thus, induced sputum cells count may be a more specific and sensitive index. Forth, although guidelines in different countries state that the CVA treatment should last for at least 8 weeks initially, no exact treatment duration was recommended. In our study, 3 months of ICS/LABA was administrated. A long-term and large-sample study is needed to elucidate its safety, and to verify whether the prolonged anti-inflammatory effect can actually prevent the development of CVA.
Conclusions
Our study shows that using WeChat in treatment and management of CVA can help patients learn more about their disease and medications, thus improving disease control and therapy outcomes. New functions of this platform need to be developed for elaborate and dynamic management of more chronic airway diseases. Further studies with large sample sizes and long-term follow-up are required to confirm this new disease management method.
Supplementary Files
Display of “Assistant of Respiratory Diseases” WeChat public account on smartphone. (A) Profile of the WeChat public account. (B–D) Platform of “Assistant of Respiratory Diseases” WeChat public account (Including 3 parts: 1. Practical tools: Questionnaires or tests related to asthma; 2. Inhaler equipment: videos of inhaler equipment for respiratory diseases; 3. Home of patients: articles on asthmatic education)
Effects of WeChat intervention on (A) Total-IgE, (B) FeNO, Blood cell counts: (C) Neutrophils; (D) Eosinophils, Pulmonary function: (E) FEV1/predicted; (F) FEV1/FVC. (G) ACQ-7 and (H) AQLQ in CVA Patients.
Supplementary Table 1.
Detail of patients withdraw.
| Reasons | Traditional group (n=10) | WeChat group (n=3) |
|---|---|---|
| Pregnant | 2 | 0 |
| Death (car accident) | 1 | 0 |
| Unable to finish bronchial provocation test | 2 | 0 |
| Unable to attend | 2 | 1 |
| Diagnosed with cancer | 0 | 1 |
| Lost contact | 1 | 1 |
| Reason not given | 2 | 0 |
Acknowledgments
None.
Footnotes
Source of support: Departmental sources
Conflict of interest
None.
References
- 1.Pratter MR. Overview of common causes of chronic cough: ACCP evidence-based clinical practice guidelines. Chest. 2006;129:59S–62S. doi: 10.1378/chest.129.1_suppl.59S. [DOI] [PubMed] [Google Scholar]
- 2.Saito N, Itoga M, Tamaki M, et al. Cough variant asthma patients are more depressed and anxious than classic asthma patients. J Psychosom Res. 2015;79:18–26. doi: 10.1016/j.jpsychores.2015.03.011. [DOI] [PubMed] [Google Scholar]
- 3.Dicpinigaitis PV. Chronic cough due to asthma: ACCP evidence-based clinical practice guidelines. Chest. 2006;129:75S–79S. doi: 10.1378/chest.129.1_suppl.75S. [DOI] [PubMed] [Google Scholar]
- 4.Kohno S, Ishida T, Uchida Y, et al. The Japanese Respiratory Society guidelines for management of cough. Respirology. 2006;11(Suppl 4):S135–86. doi: 10.1111/j.1440-1843.2006.00920_1.x. [DOI] [PubMed] [Google Scholar]
- 5.Zapata BC, Fernandez-Aleman JL, Idri A, Toval A. Empirical studies on usability of mHealth apps: A systematic literature review. J Med Syst. 2015;39:1. doi: 10.1007/s10916-014-0182-2. [DOI] [PubMed] [Google Scholar]
- 6.WeChat Wikipedia. 2011. [Accessed: 21 Sep 2011]. https://en.wikipedia.org/wiki/WeChat.
- 7.Number of monthly active WeChat users from 2nd quarter 2010 to 3rd quarter 2016 (in millions) [Accessed: 15 February 2017]. https://www.statista.com/statistics/255778/number-of-active-wechat-messenger-accounts/
- 8.Gautam A, Bhatta DN, Aryal UR. Diabetes-related health knowledge, attitude and practice among diabetic patients in Nepal. BMC Endocr Disord. 2015;15:25. doi: 10.1186/s12902-015-0021-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rana AK, Kabir ZN, Lundborg CS, Wahlin A. Health education improves both arthritis-related illness and self-rated health: An intervention study among older people in rural Bangladesh. Public Health. 2010;124:705–12. doi: 10.1016/j.puhe.2010.07.005. [DOI] [PubMed] [Google Scholar]
- 10.Apikoglu-Rabus S, Yesilyaprak G, Izzettin FV. Drug-related problems and pharmacist interventions in a cohort of patients with asthma and chronic obstructive pulmonary disease. Respir Med. 2016;120:109–15. doi: 10.1016/j.rmed.2016.10.006. [DOI] [PubMed] [Google Scholar]
- 11.Levy ML, Dekhuijzen P, Barnes PJ, et al. Inhaler technique: Facts and fantasies. A view from the Aerosol Drug Management Improvement Team (ADMIT) NPJ Prim Care Respir Med. 2016;26:16028. doi: 10.1038/npjpcrm.2016.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Takaku Y, Kurashima K, Ohta C, et al. How many instructions are required to correct inhalation errors in patients with asthma and chronic obstructive pulmonary disease? Respir Med. 2017;123:110–15. doi: 10.1016/j.rmed.2016.12.012. [DOI] [PubMed] [Google Scholar]
- 13.Dweik RA, Boggs PB, Erzurum SC, et al. An official ATS clinical practice guideline: interpretation of exhaled nitric oxide levels (FENO) for clinical applications. Am J Respir Crit Care Med. 2011;184:602–15. doi: 10.1164/rccm.9120-11ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tang W, Zhou J, Miao L, Shi G. Clinical features in patients of cough variant asthma with normal and high level of exhaled fractional nitric oxide. Clin Respir J. 2016 doi: 10.1111/crj.12568. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 15.Lai K. Chinese National Guidelines on Diagnosis and Management of Cough: consensus and controversy. J Thorac Dis. 2014;6:S683–88. doi: 10.3978/j.issn.2072-1439.2014.10.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liu M, Liu K, Zhu N, et al. Inflammatory mediators in induced sputum and airway hyperresponsiveness in cough variant asthma during long-term inhaled corticosteroid treatment. Mediators Inflamm. 2012;2012:403868. doi: 10.1155/2012/403868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Matsuoka H, Niimi A, Matsumoto H, et al. Inflammatory subtypes in cough-variant asthma: Association with maintenance doses of inhaled corticosteroids. Chest. 2010;138:1418–25. doi: 10.1378/chest.10-0132. [DOI] [PubMed] [Google Scholar]
- 18.Twaddell SH, Gibson PG, Carty K, et al. Assessment of airway inflammation in children with acute asthma using induced sputum. Eur Respir J. 1996;9:2104–8. doi: 10.1183/09031936.96.09102104. [DOI] [PubMed] [Google Scholar]
- 19.Demarche SF, Schleich FN, Paulus VA, et al. A longitudinal study in daily practice. J Allergy Clin Immunol Pract. 2017;5(5):1335–43.e5. doi: 10.1016/j.jaip.2017.01.026. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Display of “Assistant of Respiratory Diseases” WeChat public account on smartphone. (A) Profile of the WeChat public account. (B–D) Platform of “Assistant of Respiratory Diseases” WeChat public account (Including 3 parts: 1. Practical tools: Questionnaires or tests related to asthma; 2. Inhaler equipment: videos of inhaler equipment for respiratory diseases; 3. Home of patients: articles on asthmatic education)
Effects of WeChat intervention on (A) Total-IgE, (B) FeNO, Blood cell counts: (C) Neutrophils; (D) Eosinophils, Pulmonary function: (E) FEV1/predicted; (F) FEV1/FVC. (G) ACQ-7 and (H) AQLQ in CVA Patients.
Supplementary Table 1.
Detail of patients withdraw.
| Reasons | Traditional group (n=10) | WeChat group (n=3) |
|---|---|---|
| Pregnant | 2 | 0 |
| Death (car accident) | 1 | 0 |
| Unable to finish bronchial provocation test | 2 | 0 |
| Unable to attend | 2 | 1 |
| Diagnosed with cancer | 0 | 1 |
| Lost contact | 1 | 1 |
| Reason not given | 2 | 0 |