Abstract
Background:
Overhead athletes are at a greater risk of developing scapular dyskinesis (SD). Although swimming is considered an overhead sport, information regarding SD in these athletes is scarce.
Purpose:
To determine the prevalence of SD in young, asymptomatic elite swimmers.
Study Design:
Cross-sectional study; Level of evidence, 3.
Methods:
A total of 661 asymptomatic elite swimmers were enrolled in this study (344 male, 317 female; mean age, 15.83 ± 2.20 years). Anthropometric characteristics, training routine, and stroke specialty were recorded. SD was assessed using a dynamic test consisting of an examination of the shoulder blades throughout synchronous forward flexion motion in the sagittal plane and was deemed to be either present or absent. Each movement was repeated 5 times. These evaluations were performed with athletes at rest, before any training or competition. Statistical analysis was performed.
Results:
SD was detected in 56 (8.5%) participants. Type I SD was the most common (46.5%); male participants were 2 times as likely to have SD as female participants (39 male, 17 female; P < .01). No correlation was found between the dominant limb and side affected (P = .258); rather, a correlation was found between the breathing side and side affected, in that swimmers with a preferred breathing side were more prone to develop SD in the opposite shoulder (P < .05). Swimmers involved in long-distance races were found to have a greater risk of developing SD (P = .01).
Conclusion:
SD may be an asymptomatic condition in elite young swimmers and is present in 8.5% of these athletes. Early diagnosis may be useful for asymptomatic athletes with SD and to avoid its possible evolution to a symptomatic condition.
Keywords: scapular dyskinesis, dyskinesis, scapula, overhead, athletes, shoulder, pain, swimming, swimmers, elite, young, asymptomatic, symptomatic
Normal scapular function is a key factor in overhead athletes. Scapular control allows for ideal positioning of the humerus related to the glenoid, transferring energy from the lower extremity to the distal upper one. Normal movement of the scapula consists of a combination of 3 movements: (1) upward/downward rotation around a horizontal axis perpendicular to the plane of the scapula, (2) internal/external rotation around a vertical axis through the plane of the scapula, and (3) anterior/posterior tilt around a horizontal axis in the plane of the scapula.12
Scapular dyskinesis (SD) is currently defined as an alteration of normal scapular kinematics.11,12,14 It can be caused by several factors: bone (thoracic kyphosis or clavicle diseases), joint (instability or arthrosis), nervous system (cervical radiculopathy or nerve palsy), soft tissue (tightness or stiffness of the pectoralis minor and posterior capsule), and muscular imbalance (between the upper trapezius and serratus anterior).14,16,17,19 SD has been reported as a common finding in athletes and is often associated with SICK scapula syndrome (scapular malposition, inferior medial border prominence, coracoid pain and malposition, and dyskinesis of scapular movement)2,8 and GIRD (glenohumeral internal rotation deficit).2 In 2016, Burn et al3 reported that SD is a common finding in elite athletes; in particular, it was significantly higher in overhead (61%) than in nonoverhead (33%) athletes.
Usually, swimming represents a competitive overheard sport; however, the current literature on the prevalence of SD in swimming is limited. Of only 3 studies, 2 have been performed in symptomatic cohorts,1,33 and 1 has been carried out in an asymptomatic group composed of only 78 athletes.19
The aims of our study were to determine the prevalence of SD in a large sample size of asymptomatic, young elite swimmers; investigate the possible extrinsic risk factors; and evaluate if SD may compromise performance.
Methods
Between 2014 and 2016, during the National Youth Swimming Championships (this competition involves athletes from 12 to 25 years old), 694 young elite swimmers were enrolled from a total of 1840. Recruitment was carried out by voluntary participation; for swimmers under 18 years old, parental consent was obtained.
Each participant was interviewed about his or her anthropometric characteristics (sex, height, weight, age, dominant limb, etc), swimming training routine (kilometers per day, kilometers per week, sessions per week, years of training, etc), swimming characteristics (stroke, distance, breathing side, etc), and level of competition (by calculating Fédération Internationale de Natation [FINA] points of their personal best in the 100-m freestyle in the short course and their personal best in the stroke-specific race in the long course).6 The FINA table of points allows comparisons of results among different swimming events. It assigns point values to swimming performances, with more points awarded for world-class performances and fewer points for slower performances.
Swimmers were sorted into different categories by sex, age (12-15, 16-19, ≥20 years ), years of training (1-4, 5-10, 11-15 years), body mass index (<18.49 [underweight], 18.50-24.99 [normal], ≥25.00 kg/m2 [overweight]), stroke (pure [if they perform only 1 stroke such as a crawl, backstroke, breaststroke, or butterfly], mixed [if they perform a medley or >1 stroke]), distance (sprint [50-100 m], mid-distance [200-400 m], long distance [800-1500 m]), and gesture (symmetrical [if they perform the butterfly or breaststroke], not symmetrical [if they perform the freestyle or backstroke], mixed [if they perform a medley or >1 stroke]).
Shoulder function was assessed by the Constant score, the short version of the Disabilities of the Arm, Shoulder and Hand (QuickDASH), and the sport module of the QuickDASH. Inclusion criteria were training at least 6 times per week, 12 hours of weekly training, no shoulder pain within the last 12 months, and no injury or surgery during the previous 12 months. Exclusion criteria were explicit and appreciable scoliosis, shoulder injuries, and shoulder pain or surgery during the previous 12 months.
Abnormal motion patterns in SD were detected by determining the position of the scapula with the patient’s arms at rest and then observing scapular motion in the sagittal plane. These patterns fall into 3 categories, characterized by the prominence of the inferomedial border of the scapula (type I), the entire medial border (type II), or the superomedial border (type III)17,34 (Figure 1) (see online Video Supplements 1-3). These alterations may play a part in shoulder dysfunction. Research has demonstrated that alterations of scapular motion are associated with shoulder injuries. Types I and II are commonly associated with labral lesions. Type III is associated with impingement and rotator cuff lesions.2,16 In the literature, normal scapular kinematics is defined as type IV.
Figure 1.
(A) Type I scapular dyskinesis. (B) Type II scapular dyskinesis. (C) Type III scapular dyskinesis.
All participants were evaluated at rest, before any physical effort, by the forward flexion test; through this test, scapular movement was evaluated by performing forward flexion, raising and lowering the arms concurrently in the sagittal plane, which is suggested as the preferred way to examine abnormalities in scapulohumeral rhythm.7 Five repetitions of each movement were conducted.
SD was assessed for the presence of winging or abnormal motion between the 2 sides. The presence of SD was first graded as “yes” or “no” and then assigned to 1 of 3 patterns.
The forward flexion test was recorded with a fixed camera, and 3 independent observers gave their judgment. SD was rated as “yes” if 2 of the 3 examiners graded it as present.
Intratester and intertester reliability of the dynamic clinical assessment method (yes/no method) were determined by calculating intraclass correlation coefficients. Interpretation of the κ statistic was performed as described by Landis and Koch.18 Agreement was considered excellent if κ fell between 0.81 and 1.00, high if κ was between 0.61 and 0.80, moderate if κ was 0.41 to 0.60, fair if κ was 0.21 to 0.40, and poor if κ was ≤0.20.18 The chi-square test and Mann-Whitney U test were conducted for statistical analysis, and P < .05 was used as the significance threshold.
Results
Of the 694 enrolled swimmers, 33 were excluded because 5 athletes had sustained shoulder injuries in the previous 12 months and 28 had appreciable scoliosis. Therefore, our study cohort was composed of 661 swimmers: 344 male (52%) and 317 female (48%).
Intratester and intertester reliability of the yes/no method (intratester κ = 0.84; intertester κ = 0.78) and the 4-type method (intratester κ = 0.78; intertester κ = 0.71) were high.
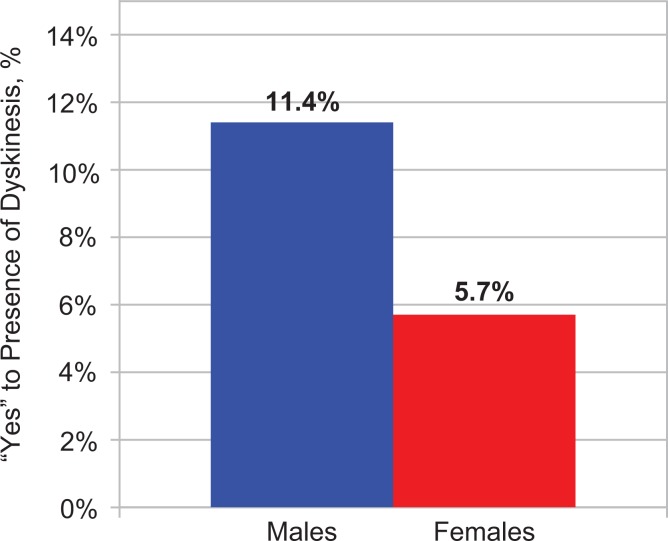
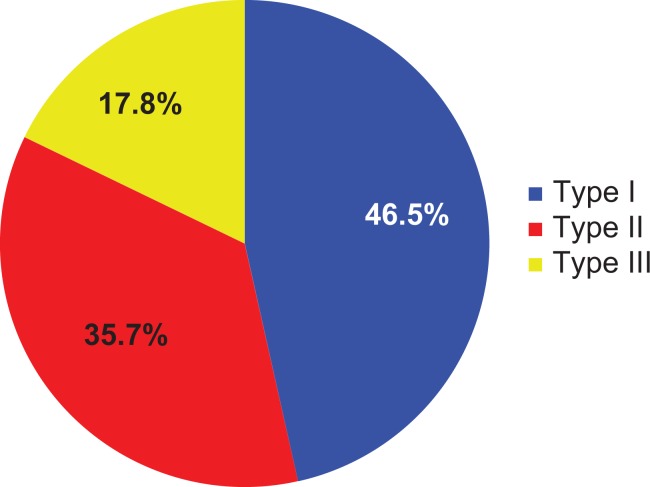
Tables 1, 2, and 3 show anthropometric data, age distribution according to sex, and swimming characteristics, respectively; Table 4 shows the swimming training routine of our athletes. SD was found in 56 participants (8.5%); baseline characteristics of the “yes” group are reported in Table 5. Figure 2 shows the sex distribution in the “yes” group. Male participants were found to be positive twice as much as female participants. Frequencies relative to SD types I, II, and III in the “yes” group are reported in Figure 3.
TABLE 1.
Anthropometric Data According to Sexa
| Female | Male | Total | |
|---|---|---|---|
| Age, y | 15.05 ± 1.94 | 16.56 ± 2.18 | 15.83 ± 2.20 |
| Weight, kg | 55.09 ± 6.25 | 69.09 ± 8.17 | 62.36 ± 10.11 |
| Height, m | 1.67 ± 0.06 | 1.79 ± 0.07 | 1.73 ± 0.09 |
| Body mass index, kg/m2 | 19.84 ± 1.65 | 21.48 ± 1.65 | 20.69 ± 1.84 |
| Hand dominance, % | |||
| Right | 89.0 | 89.5 | 89.3 |
| Left | 11.0 | 10.5 | 10.7 |
aValues are presented as mean ± standard deviation unless otherwise indicated.
TABLE 2.
Distribution of Ages According to Sexa
| Female | Male | Total | |
|---|---|---|---|
| 12-15 y | 205/661 (31.1) | 108/661 (16.3) | 313/661 (47.4) |
| 16-19 y | 105/661 (15.9) | 200/661 (30.2) | 305/661 (46.1) |
| ≥20 y | 7/661 (1.1) | 36/661 (5.4) | 43/661 (6.5) |
aValues are presented as n (%).
TABLE 3.
Swimming Characteristics According to Sexa
| Female | Male | Total | |
|---|---|---|---|
| Years of training | 5.79 ± 2.29 | 6.92 ± 2.71 | 6.38 ± 2.58 |
| Breathing side | |||
| Right | 53.6 | 67.8 | 61.0 |
| Left | 13.6 | 14.5 | 14.0 |
| Both | 32.8 | 17.7 | 25.0 |
| Distance | |||
| Sprint | 22.4 | 21.2 | 21.8 |
| Mid-distance | 57.4 | 60.8 | 59.1 |
| Long distance | 20.2 | 18.0 | 19.1 |
| Stroke | |||
| Pure | 49.5 | 53.8 | 51.8 |
| Mixed | 50.5 | 46.2 | 48.2 |
aValues are presented as mean ± standard deviation or as percentages.
TABLE 4.
Training Routinea
| Hours/day | 2.11 ± 0.35 |
| Sessions/day | 1.02 ± 0.15 |
| Sessions/week | 6.18 ± 0.66 |
| General, km/wk | 35.69 ± 6.65 |
| Stroke specific, km/wk | 10.50 ± 7.28 |
| Hand paddlesb/week | 3.07 ± 1.79 |
| Hand paddles, km/wk | 4.34 ± 3.89 |
| Drylandc, % | |
| Yes | 87.8 |
| No | 12.2 |
| Dryland/week, % | |
| 2 sessions | 52.2 |
| 3 sessions | 25.6 |
| Other | 22.2 |
aValues are presented as mean ± standard deviation unless otherwise indicated.
bTraining involving the use of hand paddles for technical support.
cLand-based strength and conditioning training for swimmers.
TABLE 5.
Baseline Characteristics of Swimmers With Scapular Dyskinesis According to Sex and Agea
| Female | Male | Total | |
|---|---|---|---|
| Age, y | 14.53 ± 1.42 | 16.59 ± 2.22 | 15.96 ± 2.22 |
| Age group | |||
| 12-15 y | 14/205 (6.8) | 11/108 (10.2) | 25/313 (7.9) |
| 16-19 y | 3/105 (2.9) | 24/200 (12.0) | 27/305 (8.8) |
| ≥20 y | 0/7 (0.0) | 4/36 (11.1) | 4/43 (9.3) |
aValues are presented as mean ± standard deviation or as n (%).
Figure 2.
Distribution of sexes in the “yes” group. A significant difference was found (P = .006).
Figure 3.
Distribution of the 3 scapular dyskinesis types in the “yes” group.
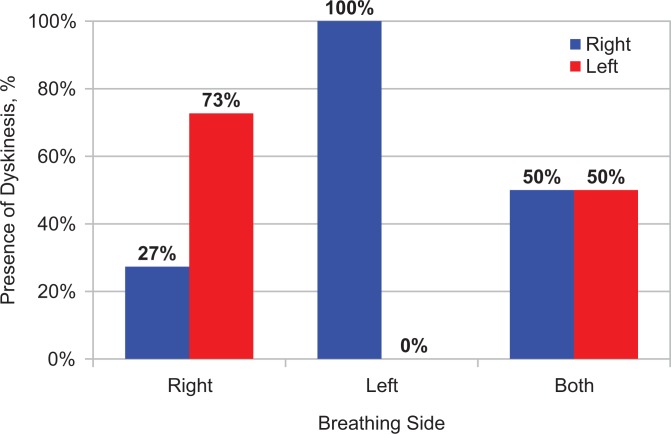
No significant prevalence was found between the presence of SD and age (P = .909). However, we observed a direct correlation between SD and years of training (P < .05); in general, swimmers who have swam for more than 4 years are twice as likely to develop SD than others. No significant statistical correlation was found comparing body mass index and the dynamic test (P = .198). SD was observed in 66.1% of athletes on the left side. No correlation was observed between hand dominance and the SD side (P = .258); instead, a correlation between the breathing side and SD side was found: SD was more commonly seen on the participant’s opposite shoulder compared to the breathing side (P < .05). SD was evenly distributed between shoulders in swimmers who breathed from both sides (Figure 4).
Figure 4.
Prevalence of scapular dyskinesis according to the breathing side and scapular dyskinesis side.
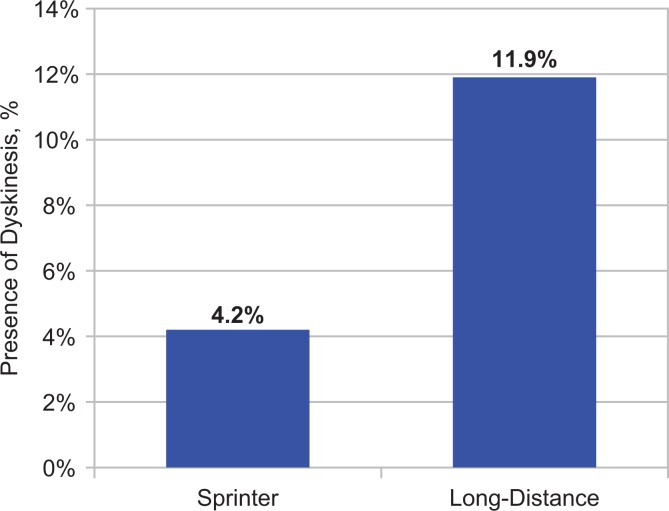
The prevalence of SD in swimmers with pure or mixed strokes was not significantly different (P = .515). For distance, SD was present in 4.2% of sprinters, 8.9% of mid-distance swimmers, and 11.9% of long-distance athletes. A significant difference (P = .01) in the presence of SD between sprinters and long-distance swimmers was detected (Figure 5). No significant difference was found between the prevalence of SD and gesture (P = .560).
Figure 5.
Distribution of scapular dyskinesis between sprinters and long-distance swimmers.
The mean (± standard deviation) FINA scores in the 100-m freestyle in the short course in male swimmers with and without SD were 557.71 ± 130.68 and 579.75 ± 88.00 points, respectively, and in female swimmers they were 563.07 ± 100.00 and 593.98 ± 84.77 points, respectively. The mean FINA scores in the stroke-specific race in the long course in male swimmers with and without SD were 636.89 ± 122.17 and 651.46 ± 81.36 points, respectively, and in female swimmers they were 626.57 ± 118.33 and 641.71 ± 97.09 points, respectively. No statistical correlations were found between the FINA score and SD. Table 6 shows the mean values of the Constant score, QuickDASH, and sport module of the QuickDASH between swimmers with and without SD. No significant difference was detected.
TABLE 6.
Constant, QuickDASH, and Sport Module of QuickDASH Scores According to Sex and Presence of SDa
| Female | Male | |
|---|---|---|
| Constant (right) | ||
| SD | 97.21 ± 4.60 | 98.55 ± 3.00 |
| No SD | 96.90 ± 6.59 | 97.83 ± 3.78 |
| Constant (left) | ||
| SD | 98.76 ± 2.22 | 97.97 ± 3.19 |
| No SD | 97.24 ± 4.02 | 98.16 ± 3.37 |
| QuickDASH | ||
| SD | 9.46 ± 9.39 | 6.53 ± 8.65 |
| No SD | 8.55 ± 9.38 | 7.07 ± 8.04 |
| Sport module of QuickDASH | ||
| SD | 9.93 ± 13.08 | 6.73 ± 10.30 |
| No SD | 10.37 ± 14.40 | 10.54 ± 15.69 |
aValues are presented as mean ± standard deviation. QuickDASH, short version of the Disabilities of the Arm, Shoulder and Hand; SD, skapular dyskinesis.
Discussion
This is the first study on SD in a large group of young, asymptomatic elite swimmers. We found that SD, diagnosed by a validated dynamic test, was present in almost one-tenth of our young athletes. The literature lacks information regarding the prevalence of SD in the general population aged between 12 and 22 years. Uhl et al34 analyzed scapular functional asymmetry during shoulder flexion in a nonhomogeneous group composed of 35 patients with shoulder pain and 21 asymptomatic participants. They found that the prevalence of functional asymmetry was 71% for both groups. Based on these findings, we are not able to state if swimming at a high level of competition could be considered a risk or a protective factor for the development of SD. However, previous studies3,25 have demonstrated that athletes in volleyball,32 baseball,24,26 handball,4 and swimming19,33 have a double or triple risk of developing SD compared to those in nonoverhead sports.
In the literature, the prevalence of SD in swimmers varies from 9%1 to 57%.33 Unfortunately, these values come from nonhomogeneous groups that differ by number, age, and symptoms.
In 2011, Madsen et al,19 evaluating 78 asymptomatic swimmers, demonstrated that the prevalence of SD during a normal training session is high; it increased with more training and occurred early during the training session. Our study evaluated athletes at rest, before any physical effort and at the end of the season, to obtain a realistic prevalence of SD excluding the influence of fatigue.
Using the descriptive classification of SD introduced by Kibler et al,17 we observed that type I is the most frequent pattern in swimmers with SD. No previous studies have investigated the prevalence of SD patterns in the swimming population. Kawasaki et al,11 analyzing a cohort of 103 elite rugby players, found that types I, II, and III were present in 4.9%, 3.9%, and 22.2% of cases, respectively. It is plausible that different sport-specific gestures could be associated with a higher risk of developing a sport-specific SD pattern. Type I is related to insufficient lower trapezius and serratus anterior recruitment as well as excessive activation of the upper trapezius.12 This finding is supported by the observations of Pink et al27 and Scovazzo et al,30 who noted that the above-mentioned muscles, commonly altered in type I SD, are susceptible to functional changes during activity.
The sex-related prevalence of SD in swimmers has been investigated only by Bak and Faunø.1 Their study was performed on 49 painful shoulders in 36 athletes and failed to find any correlation between the sexes. In our study, the prevalence of SD was significantly higher (double) in male swimmers. This finding, extrapolated from the entire examined population, was determined by the marked exuberance of male swimmers with SD who were skeletally mature (≥16 years old), in which the prevalence of SD was found to be 8 times more frequent than in the female participants. However, no differences between the sexes were found in athletes under 16 years old. To try to explain these data, we formulated 2 different hypotheses: (1) Uncorrected technical errors might influence the swimming gesture, leading to the development of functional asymmetry through the years. The prevalence of SD might be higher in male participants because they might be exposed to technical errors for a longer period, because of a longer career, than female participants. This hypothesis is supported by our observation that SD is significantly different with years of training. (2) Considering that SD is mainly caused by muscle imbalance,19 it is plausible that the greater amount of training in male athletes, which is usually reached at the end of puberty when the muscle mass is similar to that of the adult swimmer, leads to functional asymmetry and muscular fatigue that usually do not appear in prepubertal athletes.
In our population, distance specialization was a significant factor in determining SD: long-distance swimmers developed SD 3 times more frequently than sprinters. This finding may be because of the different training volumes that the 2 types of swimmers have during the season.28,29 Technical errors in the gesture appear to not have a significant impact ; in fact, 2 studies by McCabe et al20,21 found no biomechanical differences between long-distance athletes and sprinters regarding the stroke pattern when swimming at the same pace.
Prior studies on tennis,5,25 baseball,2,12,13 handball,4 and volleyball32 athletes have demonstrated that SD is more likely to develop on the dominant side. In our group, hand dominance was not correlated with SD. All the above-mentioned sports are also considered asymmetric disciplines. Swimming is defined as a symmetric activity, but actually, this assumption might not be completely true for swimmers with a preferred breathing side. No study has investigated the prevalence of SD between the breathing side and SD side in swimmers. We found a strong statistical difference between the breathing side and SD side: swimmers with a preferred breathing side were more prone to develop SD in the opposite shoulder. McCabe et al,22 analyzing the breathing cycle, found that swimmers spent 14% longer in the pull phase, 16% less time in the push phase, and 6% less in the depth of hand path in the ipsilateral shoulder compared to when the swimmer does not breathe. Considering the nonbreathing side, it might be possible that it is exposed to constant and increased functional stress during the entire push phase, leading to functional asymmetry over time. The scapula on the nonbreathing side may be internally rotated when the swimmer rolls up to the breathing side, resulting in functional dyskinesis from repetitive use.
No correlation was found between the presence of SD and stroke (pure or mixed) or gesture (symmetrical or not symmetrical). This finding was not unexpected; in fact, as demonstrated by the literature29,31,35 and confirmed by our investigation, swimmers spent more than 70% of their training time only on the freestyle stroke as general training, even when specializing in the breaststroke, backstroke, or butterfly, making it almost impossible to classify them in strict categories based on specialization.
Finally, no previous study has investigated possible correlation between SD and the competition level according to the FINA score. In our analysis, no correlation was found. These findings may be explained by the fact that our athletes with SD were asymptomatic. No difference in shoulder functional scores were detected between swimmers with and without SD. Hickey et al9 demonstrated in a systematic review and meta-analysis that asymptomatic athletes with SD have an increased risk of future shoulder pain by 43%. Therefore, further studies with a longitudinal follow-up are needed to determine whether the presence of SD predisposes one to developing shoulder symptoms or whether SD is just a functional adaptation that helps the athlete have a more efficient stroke.
This study has several limitations: (1) The method used for detecting SD: The yes/no method resulted in 78% sensitivity but 38% specificity. The sensitivity of the 4-type method varied across the types of scapular patterns, ranging from 20% to 54%, and the specificity ranged from 67% to 94%.34 However, these methods are the most used and reproducible to detect SD.10,14–16,23 (2) The selection method: The voluntary participation of 694 swimmers from a total of 1840 could result in either overestimating or underestimating the prevalence of SD. (3) Only asymptomatic swimmers were recruited in this study, and this suggests that no comparison with symptomatic swimmers could be possible to determine if there is a significant difference between these 2 groups. (4) This study considered only extrinsic factors as possible causes of SD in swimmers. Further studies are needed to detect and discuss the impact of intrinsic factors (such as hyperlaxity, GIRD, etc) in swimmers concerning SD. (5) This is an observational and cross-sectional study. No longitudinal follow-up was performed. Further studies are needed to observe swimmers longitudinally over time to see if athletes with SD develop shoulder symptoms and to set up a rehabilitation protocol.
Conclusion
SD may be an asymptomatic condition in elite young swimmers; it was present in 8.5% of our cohort, and it did not seem to affect performance. Type I was the most common pattern; male athletes were twice as susceptible as female athletes to have SD. We also found that SD was correlated with the breathing side and with long-distance specialization.
Supplementary Material
Acknowledgment
The authors express deep gratitude to their national swimming federation, Federazione Italiana Nuoto, for its technical assistance and support. All coaches and participants in this study are gratefully acknowledged. Lastly, they express special gratitude to their technical team, Matteo Zaccarin, Jacopo Ciccani, Maddalena Preziosi Standoli, Francesco Fabi, Emanuele Rosati, Marcello Piergentili, and Walter Bolognani, for their assistance with data collection.
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.
Ethical approval for this study was waived by Sapienza University of Rome.
A Video Supplement for this article is available at http://journals.sagepub.com/doi/suppl/10.1177/2325967117750814
References
- 1. Bak K, Faunø P. Clinical findings in competitive swimmers with shoulder pain. Am J Sports Med. 1997;25:254–260. [DOI] [PubMed] [Google Scholar]
- 2. Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: spectrum of pathology. Part III: the SICK scapula, scapular dyskinesis, the kinetic chain, and rehabilitation. Arthroscopy. 2003;19:641–661. [DOI] [PubMed] [Google Scholar]
- 3. Burn MB, McCulloch PC, Lintner DM, Liberman SR, Harris JD. Prevalence of scapular dyskinesis in overhead and nonoverhead athletes: a systematic review. Orthop J Sports Med. 2016;4:2325967115627608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Clarsen B, Bahr R, Andersson SH, Munk R, Myklebust G. Reduced glenohumeral rotation, external rotation weakness and scapular dyskinesis are risk factors for shoulder injuries among elite male handball players: a prospective cohort study. Br J Sports Med. 2014;48:1327–1333. [DOI] [PubMed] [Google Scholar]
- 5. Cools AM, Johansson FR, Cambier DC, Velde AV, Palmans T, Witvrouw EE. Descriptive profile of scapulothoracic position, strength and flexibility variables in adolescent elite tennis players. Br J Sports Med. 2010;44:678–684. [DOI] [PubMed] [Google Scholar]
- 6. Fédération Internationale de Natation. FINA points. Available at: http://www.fina.org/content/fina-points. Accessed January 2017.
- 7. Giphart JE, Brunkhorst JP, Horn NH, Shelburne KB, Torry MR, Millett PJ. Effect of plane of arm elevation on glenohumeral kinematics: a normative biplane fluoroscopy study. J Bone Joint Surg Am. 2013;95:238–245. [DOI] [PubMed] [Google Scholar]
- 8. Gumina S, Carbone S, Postacchini F. Scapular dyskinesis and SICK scapula syndrome in patients with chronic type III acromioclavicular dislocation. Arthroscopy. 2009;25:40–45. [DOI] [PubMed] [Google Scholar]
- 9. Hickey D, Solvig V, Cavalheri V, Harrold M, Mckenna L. Scapular dyskinesis increases the risk of future shoulder pain by 43% in asymptomatic athletes: a systematic review and meta-analysis. Br J Sports Med. 2018;52:102–110. [DOI] [PubMed] [Google Scholar]
- 10. Huang TS, Huang HY, Wang TG, Tsai YS, Lin JJ. Comprehensive classification test of scapular dyskinesis: a reliability study. Man Ther. 2015;20:427–432. [DOI] [PubMed] [Google Scholar]
- 11. Kawasaki T, Yamakawa J, Kaketa T, Kobayashi H, Kaneko K. Does scapular dyskinesis affect top rugby players during a game season? J Shoulder Elbow Surg. 2012;21:709–714. [DOI] [PubMed] [Google Scholar]
- 12. Kibler BW, Sciascia A, Wilkes T. Scapular dyskinesis and its relation to shoulder injury. J Am Acad Orthop Surg. 2012;20:364–372. [DOI] [PubMed] [Google Scholar]
- 13. Kibler WB. The role of the scapula in athletic shoulder function. Am J Sports Med. 1998;26:325–337. [DOI] [PubMed] [Google Scholar]
- 14. Kibler WB, Kuhn JE, Wilk K, et al. The disabled throwing shoulder: spectrum of pathology. 10-year update. Arthroscopy. 2013;29:141–161.e26. [DOI] [PubMed] [Google Scholar]
- 15. Kibler WB, Ludewig PM, McClure PW, et al. Clinical implications of scapular dyskinesis in shoulder injury: the 2013 consensus statement from the ‘Scapular Summit’. Br J Sports Med. 2013;47:877–885. [DOI] [PubMed] [Google Scholar]
- 16. Kibler WB, Sciascia A. Current concepts: scapular dyskinesis. Br J Sports Med. 2010;44:300–305. [DOI] [PubMed] [Google Scholar]
- 17. Kibler WB, Uhl TL, Maddux JW, Brooks PV, Zeller B, McMullen J. Qualitative clinical evaluation of scapular dysfunction: a reliability study. J Shoulder Elbow Surg. 2002;11:550–556. [DOI] [PubMed] [Google Scholar]
- 18. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159. [PubMed] [Google Scholar]
- 19. Madsen PH, Bak K, Jensen S, Welter U. Training induces scapular dyskinesis in pain-free competitive swimmers: a reliability and observational study. Clin J Sport Med. 2011;21:109–113. [DOI] [PubMed] [Google Scholar]
- 20. McCabe CB, Psycharakis S, Sanders R. Kinematic differences between front crawl sprint and distance swimmers at sprint pace. J Sports Sci. 2011;29:115–123. [DOI] [PubMed] [Google Scholar]
- 21. McCabe CB, Sanders RH. Kinematic differences between front crawl sprint and distance swimmers at a distance pace. J Sports Sci. 2012;30:601–608. [DOI] [PubMed] [Google Scholar]
- 22. McCabe CB, Sanders RH, Psycharakis SG. Upper limb kinematic differences between breathing and non-breathing conditions in front crawl sprint swimming. J Biomech. 2015;48:3995–4001. [DOI] [PubMed] [Google Scholar]
- 23. McClure P, Tate AR, Kareha S, Irwin D, Zlupko E. A clinical method for identifying scapular dyskinesis, part 1: reliability. J Athl Train. 2009;44:160–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Myers JB, Laudner KG, Pasquale MR, Bradley JP, Lephart SM. Scapular position and orientation in throwing athletes. Am J Sports Med. 2005;33:263–271. [DOI] [PubMed] [Google Scholar]
- 25. Oyama S, Myers JB, Wassinger CA, Ricci RD, Lephart SM. Asymmetric resting scapular posture in healthy overhead athletes. J Athl Train. 2008;43:565–570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Park JY, Hwang JT, Kim KM, Makkar D, Moon SG, Han KJ. How to assess scapular dyskinesis precisely: 3-dimensional wing computer tomography. A new diagnostic modality. J Shoulder Elbow Surg. 2013;22:1084–1091. [DOI] [PubMed] [Google Scholar]
- 27. Pink M, Perry J, Browne A, Scovazzo ML, Kerrigan J. The normal shoulder during freestyle swimming. Am J Sports Med. 1991;19:569–576. [DOI] [PubMed] [Google Scholar]
- 28. Pink MM, Tibone JE. The painful shoulder in the swimming athlete. Orthop Clin North Am. 2000;31:247–261. [DOI] [PubMed] [Google Scholar]
- 29. Richardson AB, Jobe FW, Collins HR. The shoulder in competitive swimming. Am J Sports Med. 1979;8:159–163. [DOI] [PubMed] [Google Scholar]
- 30. Scovazzo ML, Browne A, Pink M, Jobe FW, Kerrigan J. The painful shoulder during freestyle swimming. Am J Sports Med. 1991;19:577–582. [DOI] [PubMed] [Google Scholar]
- 31. Sein ML, Walton J, Linklater J, et al. Shoulder pain in elite swimmers: primarily due to swim-volume-induced supraspinatus tendinopathy. Br J Sports Med. 2010;44:105–113. [DOI] [PubMed] [Google Scholar]
- 32. Struyf F, Nijs J, Meeus M, et al. Does scapular positioning predict shoulder pain in recreational overhead athletes? Int J Sports Med. 2013;35:75–82. [DOI] [PubMed] [Google Scholar]
- 33. Tate A, Turner GN, Knab SE, Jorgensen C, Strittmatter A, Michener LA. Risk factors associated with shoulder pain and disability across the lifespan of competitive swimmers. J Athl Train. 2012;47:149–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Uhl TL, Kibler WB, Gecewich B, Tripp BL. Evaluation of clinical assessment methods for scapular dyskinesis. Arthroscopy. 2009;25:1240–1248. [DOI] [PubMed] [Google Scholar]
- 35. Wolf BR, Ebinger AE, Lawler MP, Britton CL. Injury patterns in Division I collegiate swimming. Am J Sports Med. 2009;37:2037–2042. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.