Abstract
The NCCN Guidelines for Survivorship provide screening, evaluation, and treatment recommendations for common consequences of cancer and cancer treatment. They are intended to aid health care professionals who work with survivors of adult-onset cancer in the posttreatment period, including those in general oncology, specialty cancer survivor clinics, and primary care practices. Guidance is also provided to help promote physical activity, weight management, and proper immunizations in survivors. This article summarizes the NCCN Survivorship panel’s discussions for the 2016 update of the guidelines regarding the management of anxiety, depression, posttraumatic stress disorder–related symptoms, and emotional distress in survivors.
Overview
Nearly 14.5 million cancer survivors were alive in the United States in 2014, and these numbers are predicted to reach almost 19 million by 2024.1,2 Unfortunately, many of these survivors experience physical (eg, fatigue, pain, lymphedema, premature menopause, cognitive deficits, sexual dysfunction), psychological (eg, anxiety, depression, fear of recurrence), and psychosocial (eg, issues surrounding employment, finances, insurance) late and long-term effects of cancer and its treatment.3–22 These effects can be severe, debilitating, and sometimes permanent or life-threatening. Survivors may be discharged from the care of their oncologist or see the oncology team less frequently, resulting in feelings of isolation and worry or fear. Furthermore, their primary care physicians (PCPs), who may now be responsible for their care, often do not know how best to care for the specific concerns and needs of cancer survivors.23
The NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines) for Survivorship aid health care professionals who work with survivors of adult-onset cancers in the posttreatment period by providing screening, evaluation, and treatment recommendations for common consequences of cancer and cancer treatment. The guidelines are designed to provide a framework for the management of long-term and/or late effects of cancer and its treatment and for the coordination of care between the survivor’s health care providers to ensure that needs are appropriately addressed. They should be used as a supplement to the follow-up recommendations within the disease-specific guidelines (see NCCN Guidelines for Treatment of Cancer by Site, available at www.NCCN.org).
The 1.2016 version of the NCCN Guidelines for Survivorship focuses on several common issues of survivors: anxiety/depression/distress; anthracycline-induced cardiac toxicity; cognitive decline; fatigue; pain; female and male sexual dysfunction; sleep disorders; and the preventive health issues of immunizations and prevention of infections and healthy lifestyle behaviors. Additional topics will be addressed in subsequent updates.
2016 Updates to the NCCN Guidelines for Survivorship
During the update of the NCCN Guidelines for Survivorship this year, an emerging theme highlighted the fact that clinicians may not have the expertise needed to help survivors with the wide range of possible issues they may face. The panel therefore added the option for early referral to the appropriate specialist in many cases (eg, sexual dysfunction, sleep disorders). Thus, the algorithm for many of the survivorship topics now first includes information designed to increase clinician awareness of the issues, then includes appropriate screening questions or tools followed by the option for early referral to the appropriate specialist. In addition, the guidelines provide guidance for appropriate evaluation, treatment, and follow-up care at a level that can be appropriately performed by the oncologist, PCP, or specialist.
This paradigm was used in the redesign of the section on anxiety and depression in cancer survivors, as discussed herein. Additional issues discussed by the panel this year regarding the management of anxiety, depression, posttraumatic stress disorder (PTSD)–related symptoms, and distress in survivors are also described. Changes to the guidelines are indicated with blue font in the figures.
Anxiety, Depression, and Distress in Survivors
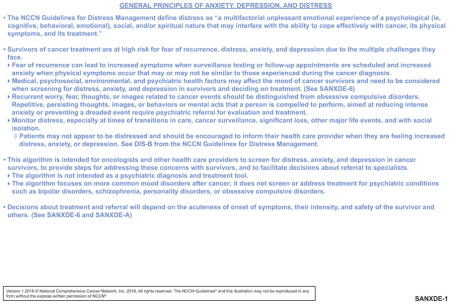
Cancer survivors are at especially high risk for anxiety, depression, and other forms of psychosocial distress because of the multiple stressors, vulnerabilities, and challenges they face. According to the NCCN Guidelines for Distress Management (available at www.NCCN.org), risk factors for psychosocial distress include cognitive impairment, severe comorbid illnesses, uncontrolled symptoms, communication barriers, or a history of psychiatric disorder, depression, or substance abuse. Social issues, such as living alone, having young children, being of younger age or female, and prior physical or sexual abuse, are also risk factors for psychosocial distress.
Fear of recurrence, with persisting worry and distress sometimes reaching levels of clinical anxiety, is common in cancer survivors. This fear can increase at times of routine cancer surveillance testing or with physical symptoms that may or may not be related to the cancer diagnosis.11,24–27 Anxiety and/ or depression can also occur in survivors secondary to physical compromise, social isolation, or work and financial problems that result from cancer treatment.11,15,16,19,26 These challenges are underscored by the inevitable decreased medical and interpersonal support after completion of treatment and transition to the surveillance stage.28
Anxiety and depression affect up to 29% of survivors, with 1% to 19% of survivors reportedly meeting the criteria for PTSD.11,15,29–31 In addition, many survivors have less severe distress that might not lead to a clinical diagnosis of anxiety, depression, or PTSD but that can still have a negative impact on quality of life. Survivors with untreated, uncontrolled emotional distress are less likely to adhere to recommended surveillance and are less likely to engage in health-promoting activities, such as exercise and smoking cessation.32 Sometimes these individuals develop thoughts of ending their lives; the incidence of completed suicide among patients with cancer and survivors in the United States is approximately twice that of the general population.33–38
Possible Early Referral for Survivors With Anxiety, Depression, PTSD-Related Symptoms, and Distress
Reviewers from several NCCN Member Institutions indicated that the original anxiety and depression section of the guidelines was too complex, detailing evaluation and management that were beyond the scope of the typical oncologist or PCP. The extensive evaluation was viewed as a diagnostic evaluation better performed by a trained mental health provider.
Oncologists on the panel agreed that they do not feel comfortable diagnosing major psychiatric disorders, nor should oncologists or PCPs be doing so. However, the panel discussed the pervasiveness of psychosocial problems in survivors and the fact that many distressed survivors may not appear distressed. The panelists strongly believe that oncologists and PCPs need to know how to screen, when to screen, and to whom to refer when screening indicates a need for services. The panel therefore added information on the prevalence of and risk factors for distress in survivors (see SANXDE-1; page 717) and modified their recommendations to include the following general structure: screening, flagging those in need of referral, ensuring the safety of the survivor, and the option for early referral to mental health services (ie, psychiatrist, psychologist, advanced practice clinicians, and/or social worker) (see SANXDE-4 and SANXDE-6 as examples; pages 717 and 718). The panel’s intent is to provide information to facilitate decisions about referrals, and to take initial steps in providing care rather than to provide guidelines for psychiatric diagnoses. Instead of specifying the full diagnostic criteria for issues such as depression, anxiety, and PTSD, the panel listed the essential criteria for screening psychiatric diagnoses that are most common in survivors, and some key symptoms from the Diagnostic and Statistical Manual of Mental Disorders (Fifth Edition; DSM-V).39
The panel then discussed the fact that survivors with few or mild symptoms may be managed with oncology or primary care support and access to online, telephone-based, or community support resources, and may not require a referral to mental health services, and that in some places (eg, rural areas) there may not be sufficient mental health resources available to refer all survivors in need. It is important for oncology and PCPs to have awareness of the prevalence of anxiety, depression, and distress in survivors and guidance regarding initial steps in management. In addition, the panelists felt that guidance for the psychiatrists, psychologists, advanced practice clinicians, social workers, and/or licensed therapists who work with survivors was needed. The panel therefore retained the evaluation and management recommendations listed in the guidelines.
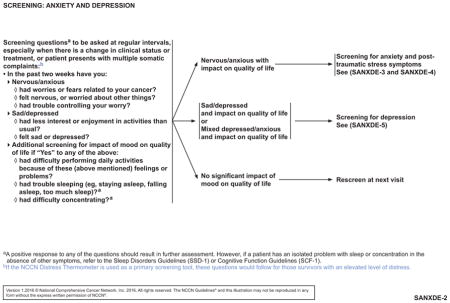
Screening
During the panel’s discussion regarding the appropriate initial screening for anxiety and depression in survivors, a panel member brought up the role of the NCCN Distress Thermometer (DT) in survivors. Several panel members noted that their institutions are using the DT to screen for distress in survivors at this time. The DT is embedded into many commercially available electronic health record (EHR) systems and is therefore used by many hospitals, clinics, and private practices.
The panel discussed the literature addressing the validity of the DT in cancer survivors. Studies generally do not support its use in a clinical survivorship setting because it lacks sufficient sensitivity and specificity in this population.40–46 For example, a study of 120 survivors of adult-onset cancer found that the DT had a sensitivity of 47.6% and 51.7%, using cutoff values of 5 and 4, respectively.44
The panel therefore recommended supplemental screening when the DT is used as an initial screening tool. They added a footnote indicating that survivors with an elevated level of distress by the DT should still be asked the initial screening questions provided by the panel (see SANXDE-2, page 718). These more specific questions allow the clinician to determine what particular issues are affecting the survivor and may identify more distressed or depressed survivors than the DT.
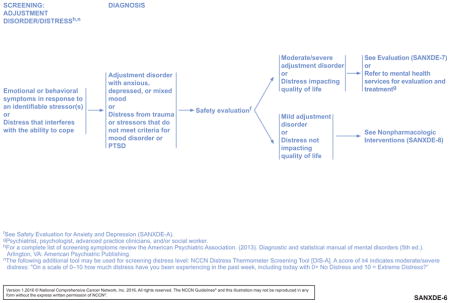
Distress/Adjustment Disorder
Reviewers from NCCN Member Institutions commented that the guidelines seemed mainly to address severe or extreme cases of anxiety and depression, but gave little guidance for cases of mild to moderate symptom burden, which are most common. Reviewers also suggested combining “mild adjustment disorder with depressed mood or with mixed depressed mood and anxiety” with “adjustment disorder with anxious mood,” noting that no clinical reasons justified their separation within the guidelines.
The panel agreed with these points. Panelists noted that many survivors may not have clinical diagnoses but still have symptoms that require further evaluation and intervention. Such survivors have what the NCCN Guidelines for Distress Management (available at www.NCCN.org) define as distress: “a multifactorial unpleasant emotional experience of a psychological (ie, cognitive, behavioral, emotional), social, and/or spiritual nature that may interfere with the ability to cope effectively with cancer, its physical symptoms, and its treatment.” Distress, often related to fear of recurrence, is common in survivors, and can negatively impact quality of life.11,24–27
The panel decided to restructure the guidelines to include a page for all survivors with symptoms who do not meet the diagnostic criteria for anxiety or depression and who do not have PTSD symptoms impacting quality of life (see SANXDE-6; page 720). This page addresses what the panel termed “adjustment disorder/distress.” To emphasize the importance of treating distress, the panel also changed the title of this section of the guideline to include the word “distress.”
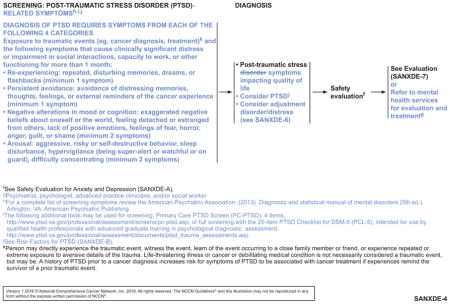
PTSD-Related Symptoms
A panel member asked the panel to discuss PTSD, noting that, as with distress, many survivors may not meet the full diagnostic criteria for PTSD but still have PTSD-related symptoms that need to be addressed. However, the way the guideline was originally written only allowed for patients to be treated if they had full PTSD. The panel discussed various studies showing that 17% to 38% of survivors have PTSD symptoms, whereas 1% to 19% meet the full criteria.11,29,31,47–50 In one longitudinal study, 12% of survivors reported that their PTSD symptoms resolved over 5 years, whereas 37% reported that their symptoms persisted or worsened during that time.30 Panel members also pointed out that PTSD symptoms in survivors can fluctuate over time, because of other events or other trauma occurring in the survivor’s life.
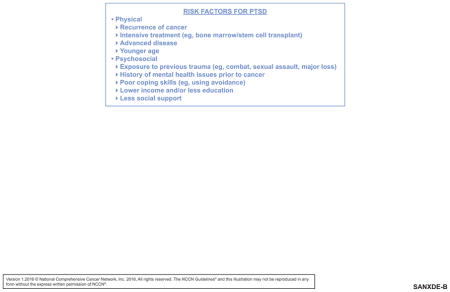
The panel decided to expand the section on PTSD, changing it to “PTSD-related symptoms” to emphasize the fact that survivors may not meet the full diagnostic criteria for PTSD but still have symptoms deserving of treatment (see SANXDE-4, page 719). The panel included an extensive list of PTSD criteria, so that clinicians can be aware when a survivor might have PTSD. The panel also decided to add a list of risk factors for PTSD, so that clinicians are alert to the disease-related and other physical and psychosocial factors that can play a role in the disorder (see SANXDE-B, page 721). In addition, the guidelines now allow for further evaluation, referral, and treatment for survivors with PTSD-related symptoms impacting quality of life, even if the full PTSD diagnostic criteria are not met.
Conclusions
The diagnosis and treatment of cancer can have a vast and persistent impact on the survivor’s health, physical, and mental states; health behaviors; professional and personal identity; sexuality; and financial standing. Clinicians providing survivorship care can improve the lives of the survivors by understanding this impact; conducting screening for physical, psychological, and psychosocial effects; and providing appropriate referrals, treatment, and/or follow-up. As the number of survivors continues to grow, clinician awareness about these critical issues becomes increasingly important. In particular, clinicians who work with cancer survivors need to be aware that distress is prevalent in the survivor population and may not be evident in an individual survivor without appropriate screening. Distressed survivors may not meet criteria for a full clinical psychiatric diagnosis, but can still benefit from interventions to improve quality of life. Clinicians can refer distressed survivors to an appropriate mental health professional or can perform evaluation and treatment as their expertise and resources allow.
NCCN Categories of Evidence and Consensus.
Category 1
Based upon high-level evidence, there is uniform NCCN consensus that the intervention is appropriate.
Category 2A
Based upon lower-level evidence, there is uniform NCCN consensus that the intervention is appropriate.
Category 2B
Based upon lower-level evidence, there is NCCN consensus that the intervention is appropriate.
Category 3
Based upon any level of evidence, there is major NCCN disagreement that the intervention is appropriate.
Acknowledgments
This activity is supported by educational grants from AstraZeneca, Bayer Healthcare Pharmaceuticals Inc., Bristol-Myers Squibb, Clovis Oncology, Foundation Medicine, Genentech, Novartis Oncology, Otsuka America Pharmaceutical, Inc., Seattle Genetics, Inc., and Takeda Oncology; support provided by Actelion Pharmaceuticals US, Inc.; and by an independent educational grant from Astellas and Medivation, Inc.
Footnotes
Please Note
The NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) are a statement of consensus of the authors regarding their views of currently accepted approaches to treatment. The NCCN Guidelines® Insights highlight important changes to the NCCN Guidelines® recommendations from previous versions. Colored markings in the algorithm show changes and the discussion aims to further the understanding of these changes by summarizing salient portions of the NCCN Guideline Panel discussion, including the literature reviewed.
These NCCN Guidelines Insights do not represent the full NCCN Guidelines; further, the National Comprehensive Cancer Network® (NCCN®) makes no representation or warranties of any kind regarding the content, use, or application of the NCCN Guidelines and NCCN Guidelines Insights and disclaims any responsibility for their applications or use in any way.
The full and most current version of these NCCN Guidelines are available at NCCN.org.
Disclosure of Relevant Financial Relationships
Individuals Who Provided Content Development and/or Authorship Assistance:
Crystal S. Denlinger, MD, Panel Chair, has disclosed that she is a scientific advisor for Eli Lilly and Company and Merrimack Pharmaceuticals.
Jennifer A. Ligibel, MD, Panel Vice Chair, has disclosed that she has received a product donation from Fitbit for a research study.
Madhuri Are, MD, Panel Member, has disclosed that she has no relevant financial relationships.
Grace H. Ku, MD, Panel Member, has disclosed that she has no relevant financial relationships.
Elizabeth Kvale, MD, Panel Member, has disclosed that she is a consult for Aspire Healthcare.
Mary S. McCabe, RN, BS, MA, Panel Member, has disclosed that she has no relevant financial relationships.
Mary Ann Morgan, PhD, FNP-BC, Panel Member, has disclosed that she is on the speakers’ bureau for Genentech.
Electra D. Paskett, PhD, Panel Member, has disclosed that she has equity interest/stock options from Pfizer Inc, and receives grant/research support from Merck & Co., Inc.
Jeffrey Peppercorn, MD, MPH, Panel Member, has disclosed that he has equity interest/stock options and receives salary from GlaxoSmith-Kline, and receives grant/research support from Pfizer Inc.
Kathryn J. Ruddy, MD, MPH, Panel Member, has disclosed that she has no relevant financial relationships.
Tara Sanft, MD, Panel Member, has disclosed that she has no relevant financial relationships.
Karen L. Syrjala, PhD, Panel Member, has disclosed that she has no relevant financial relationships.
Nicole R. McMillian, MS, Guidelines Coordinator, NCCN, has disclosed that she has no relevant financial relationships.
Deborah A. Freedman-Cass, PhD, Oncology Scientist/Senior Medical Writer, NCCN, has disclosed that she has no relevant financial relationships.
References
- 1.Cancer survivors—United States, 2007. MMWR Morb Mortal Wkly Rep. 2011;60:269–272. [PubMed] [Google Scholar]
- 2.DeSantis CE, Lin CC, Mariotto AB, et al. Cancer treatment and survivorship statistics, 2014. CA Cancer J Clin. 2014;64:252–271. doi: 10.3322/caac.21235. [DOI] [PubMed] [Google Scholar]
- 3.Beckjord EB, Reynolds KA, van Londen GJ, et al. Population-level trends in posttreatment cancer survivors’ concerns and associated receipt of care: results from the 2006 and 2010 LIVESTRONG surveys. J Psychosoc Oncol. 2014;32:125–151. doi: 10.1080/07347332.2013.874004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Weaver KE, Forsythe LP, Reeve BB, et al. Mental and physical health-related quality of life among U.S. cancer survivors: population estimates from the 2010 National Health Interview Survey. Cancer Epidemiol Biomarkers Prev. 2012;21:2108–2117. doi: 10.1158/1055-9965.EPI-12-0740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stein KD, Syrjala KL, Andrykowski MA. Physical and psychological long-term and late effects of cancer. Cancer. 2008;112:2577–2592. doi: 10.1002/cncr.23448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Valdivieso M, Kujawa AM, Jones T, Baker LH. Cancer survivors in the United States: a review of the literature and a call to action. Int J Med Sci. 2012;9:163–173. doi: 10.7150/ijms.3827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Park SY, Bae DS, Nam JH, et al. Quality of life and sexual problems in disease-free survivors of cervical cancer compared with the general population. Cancer. 2007;110:2716–2725. doi: 10.1002/cncr.23094. [DOI] [PubMed] [Google Scholar]
- 8.Paskett ED, Dean JA, Oliveri JM, Harrop JP. Cancer-related lymphedema risk factors, diagnosis, treatment, and impact: a review. J Clin Oncol. 2012;30:3726–3733. doi: 10.1200/JCO.2012.41.8574. [DOI] [PubMed] [Google Scholar]
- 9.Ruddy KJ, Partridge AH. Fertility (male and female) and menopause. J Clin Oncol. 2012;30:3705–3711. doi: 10.1200/JCO.2012.42.1966. [DOI] [PubMed] [Google Scholar]
- 10.Boyes AW, Girgis A, D’Este C, Zucca AC. Prevalence and correlates of cancer survivors’ supportive care needs 6 months after diagnosis: a population-based cross-sectional study. BMC Cancer. 2012;12:150. doi: 10.1186/1471-2407-12-150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hodgkinson K, Butow P, Fuchs A, et al. Long-term survival from gynecologic cancer: psychosocial outcomes, supportive care needs and positive outcomes. Gynecol Oncol. 2007;104:381–389. doi: 10.1016/j.ygyno.2006.08.036. [DOI] [PubMed] [Google Scholar]
- 12.Koch L, Jansen L, Brenner H, Arndt V. Fear of recurrence and disease progression in long-term (>/= 5 years) cancer survivors--a systematic review of quantitative studies. Psychooncology. 2013;22:1–11. doi: 10.1002/pon.3022. [DOI] [PubMed] [Google Scholar]
- 13.Savard J, Ivers H. The evolution of fear of cancer recurrence during the cancer care trajectory and its relationship with cancer characteristics. J Psychosom Res. 2013;74:354–360. doi: 10.1016/j.jpsychores.2012.12.013. [DOI] [PubMed] [Google Scholar]
- 14.Thewes B, Butow P, Bell ML, et al. Fear of cancer recurrence in young women with a history of early-stage breast cancer: a cross-sectional study of prevalence and association with health behaviours. Support Care Cancer. 2012;20:2651–2659. doi: 10.1007/s00520-011-1371-x. [DOI] [PubMed] [Google Scholar]
- 15.Bellizzi KM, Miller MF, Arora NK, Rowland JH. Positive and negative life changes experienced by survivors of non-Hodgkin’s lymphoma. Ann Behav Med. 2007;34:188–199. doi: 10.1007/BF02872673. [DOI] [PubMed] [Google Scholar]
- 16.Hoffman KE, McCarthy EP, Recklitis CJ, Ng AK. Psychological distress in long-term survivors of adult-onset cancer: results from a national survey. Arch Intern Med. 2009;169:1274–1281. doi: 10.1001/archinternmed.2009.179. [DOI] [PubMed] [Google Scholar]
- 17.Bradley CJ. Financial hardship: a consequence of survivorship? J Clin Oncol. 2012;30:1579–1580. doi: 10.1200/JCO.2011.40.7247. [DOI] [PubMed] [Google Scholar]
- 18.McGrath PD, Hartigan B, Holewa H, Skarparis M. Returning to work after treatment for haematological cancer: findings from Australia. Support Care Cancer. 2012;20:1957–1964. doi: 10.1007/s00520-011-1298-2. [DOI] [PubMed] [Google Scholar]
- 19.Mitchell AJ, Ferguson DW, Gill J, et al. Depression and anxiety in long-term cancer survivors compared with spouses and healthy controls: a systematic review and meta-analysis. Lancet Oncol. 2013;14:721–732. doi: 10.1016/S1470-2045(13)70244-4. [DOI] [PubMed] [Google Scholar]
- 20.Mols F, Aaronson NK, Vingerhoets AJ, et al. Quality of life among long-term non-Hodgkin lymphoma survivors: a population-based study. Cancer. 2007;109:1659–1667. doi: 10.1002/cncr.22581. [DOI] [PubMed] [Google Scholar]
- 21.Short PF, Vargo MM. Responding to employment concerns of cancer survivors. J Clin Oncol. 2006;24:5138–5141. doi: 10.1200/JCO.2006.06.6316. [DOI] [PubMed] [Google Scholar]
- 22.Syrjala K, Yi J. Overview of psychosocial issues in the adult cancer survivor. In: Ganz P, Dizon D, editors. UpToDate. Waltham, MA: Wolters Kluwer Health; 2014. [Google Scholar]
- 23.Nekhlyudov L, Aziz N, Lerro CC, Virgo KS. Oncologists’ and primary care providers’ awareness of late effects of cancer treatment: Implications for survivorship care [abstract] J Clin Oncol. 2012;30(Suppl) Abstract 6008. [Google Scholar]
- 24.Mehnert A, Koch U, Sundermann C, Dinkel A. Predictors of fear of recurrence in patients one year after cancer rehabilitation: a prospective study. Acta Oncol. 2013;52:1102–1109. doi: 10.3109/0284186X.2013.765063. [DOI] [PubMed] [Google Scholar]
- 25.Ploos van Amstel FK, van den Berg SW, van Laarhoven HW, et al. Distress screening remains important during follow-up after primary breast cancer treatment. Support Care Cancer. 2013;21:2107–2115. doi: 10.1007/s00520-013-1764-0. [DOI] [PubMed] [Google Scholar]
- 26.Roerink SH, de Ridder M, Prins J, et al. High level of distress in long-term survivors of thyroid carcinoma: results of rapid screening using the distress thermometer. Acta Oncol. 2013;52:128–137. doi: 10.3109/0284186X.2012.723822. [DOI] [PubMed] [Google Scholar]
- 27.Harrison SE, Watson EK, Ward AM, et al. Primary health and supportive care needs of long-term cancer survivors: a questionnaire survey. J Clin Oncol. 2011;29:2091–2098. doi: 10.1200/JCO.2010.32.5167. [DOI] [PubMed] [Google Scholar]
- 28.Stanton AL. What happens now? Psychosocial care for cancer survivors after medical treatment completion. J Clin Oncol. 2012;30:1215–1220. doi: 10.1200/JCO.2011.39.7406. [DOI] [PubMed] [Google Scholar]
- 29.Smith SK, Zimmerman S, Williams CS, et al. Post-traumatic stress outcomes in non-Hodgkin’s lymphoma survivors. J Clin Oncol. 2008;26:934–941. doi: 10.1200/JCO.2007.12.3414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Smith SK, Zimmerman S, Williams CS, et al. Post-traumatic stress symptoms in long-term non-Hodgkin’s lymphoma survivors: does time heal? J Clin Oncol. 2011;29:4526–4533. doi: 10.1200/JCO.2011.37.2631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wiener L, Battles H, Bernstein D, et al. Persistent psychological distress in long-term survivors of pediatric sarcoma: the experience at a single institution. Psychooncology. 2006;15:898–910. doi: 10.1002/pon.1024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Carmack CL, Basen-Engquist K, Gritz ER. Survivors at higher risk for adverse late outcomes due to psychosocial and behavioral risk factors. Cancer Epidemiol Biomarkers Prev. 2011;20:2068–2077. doi: 10.1158/1055-9965.EPI-11-0627. [DOI] [PubMed] [Google Scholar]
- 33.Kendal W. Suicide and cancer: a gender-comparative study. Ann Oncol. 2007;18:381–387. doi: 10.1093/annonc/mdl385. [DOI] [PubMed] [Google Scholar]
- 34.Miller M, Mogun H, Azrael D, et al. Cancer and the risk of suicide in older Americans. J Clin Oncol. 2008;26:4720–4724. doi: 10.1200/JCO.2007.14.3990. [DOI] [PubMed] [Google Scholar]
- 35.Misono S, Weiss NS, Fann JR, et al. Incidence of suicide in persons with cancer. J Clin Oncol. 2008;26:4731–4738. doi: 10.1200/JCO.2007.13.8941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Recklitis CJ, Diller LR, Li X, et al. Suicide ideation in adult survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. J Clin Oncol. 2010;28:655–661. doi: 10.1200/JCO.2009.22.8635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Recklitis CJ, Zhou ES, Zwemer EK, et al. Suicidal ideation in prostate cancer survivors: understanding the role of physical and psychological health outcomes. Cancer. 2014;120:3393–3400. doi: 10.1002/cncr.28880. [DOI] [PubMed] [Google Scholar]
- 38.Walker J, Waters RA, Murray G, et al. Better off dead: suicidal thoughts in cancer patients. J Clin Oncol. 2008;26:4725–4730. doi: 10.1200/JCO.2007.11.8844. [DOI] [PubMed] [Google Scholar]
- 39.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5. Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- 40.Boyes A, D’Este C, Carey M, et al. How does the Distress Thermometer compare to the Hospital Anxiety and Depression Scale for detecting possible cases of psychological morbidity among cancer survivors? Support Care Cancer. 2013;21:119–127. doi: 10.1007/s00520-012-1499-3. [DOI] [PubMed] [Google Scholar]
- 41.Craike MJ, Livingston PM, Warne C. Sensitivity and specificity of the Distress Impact Thermometer for the detection of psychological distress among CRC survivors. J Psychosoc Oncol. 2011;29:231–241. doi: 10.1080/07347332.2011.563347. [DOI] [PubMed] [Google Scholar]
- 42.Hong JS, Tian J. Sensitivity and specificity of the Distress Thermometer in screening for distress in long-term nasopharyngeal cancer survivors. Curr Oncol. 2013;20:e570–576. doi: 10.3747/co.20.1617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Livingston PM, Craike MJ, White VM, et al. A nurse-assisted screening and referral program for depression among survivors of colorectal cancer: feasibility study. Med J Aust. 2010;193:S83–87. doi: 10.5694/j.1326-5377.2010.tb03935.x. [DOI] [PubMed] [Google Scholar]
- 44.Merport A, Bober SL, Grose A, Recklitis CJ. Can the distress thermometer (DT) identify significant psychological distress in long-term cancer survivors? A comparison with the Brief Symptom Inventory-18 (BSI-18) Support Care Cancer. 2012;20:195–198. doi: 10.1007/s00520-011-1269-7. [DOI] [PubMed] [Google Scholar]
- 45.Recklitis CJ, Licht I, Ford J, et al. Screening adult survivors of childhood cancer with the distress thermometer: a comparison with the SCL-90-R. Psychooncology. 2007;16:1046–1049. doi: 10.1002/pon.1212. [DOI] [PubMed] [Google Scholar]
- 46.Recklitis CJ, Blackmon JE, Chang G. Screening young adult cancer survivors for distress with the Distress Thermometer: Comparisons with a structured clinical diagnostic interview. Cancer. 2016;122:296–303. doi: 10.1002/cncr.29736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Abbey G, Thompson SB, Hickish T, Heathcote D. A meta-analysis of prevalence rates and moderating factors for cancer-related post-traumatic stress disorder. Psychooncology. 2015;24:371–381. doi: 10.1002/pon.3654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Custers JA, Gielissen MF, Janssen SH, et al. Fear of cancer recurrence in colorectal cancer survivors. Support Care Cancer. 2016;24:555–562. doi: 10.1007/s00520-015-2808-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ford JS, Chou JF, Sklar CA, et al. Psychosocial outcomes in adult survivors of retinoblastoma. J Clin Oncol. 2015;33:3608–3614. doi: 10.1200/JCO.2014.60.5733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Varela VS, Ng A, Mauch P, Recklitis CJ. Posttraumatic stress disorder (PTSD) in survivors of Hodgkin’s lymphoma: prevalence of PTSD and partial PTSD compared with sibling controls. Psychooncology. 2013;22:434–440. doi: 10.1002/pon.2109. [DOI] [PMC free article] [PubMed] [Google Scholar]


