Abstract
Cardiovascular disease is the leading cause of mortality in patients with chronic kidney disease. Endothelial cell injury and apoptosis may promote atherosclerosis and cardiovascular disease. The present study investigated the potential mechanisms of asymmetric dimethylarginine (ADMA)-induced apoptosis in human umbilical vein endothelial cells (HUVECs). It was demonstrated that ADMA decreased B-cell lymphoma-2 expression and increased cleaved-caspase-3 expression. Furthermore, terminal deoxynucleotidyl transferase (TdT)-mediated-digoxigenin-11-dUTP nick end labeling results indicated that ADMA induced apoptosis in HUVECs. These results suggest a potential mechanism of ADMA-induced endothelial cell injury. It was also verified that ADMA induced the expression of phosphorylated protein kinase RNA-like ER kinase, inositol requiring enzyme-1, C/EBP homologous protein and glucose-regulated protein, indicating activation of the endoplasmic reticulum (ER) stress response. Impaired function of sarco/endoplasmic reticulum calcium-ATPase (SERCA) is considered a major contributor to ER stress. It was demonstrated that ADMA induced a significant downregulation of SERCA3, however not SERCA2b. Overall, the results indicated that ADMA induced apoptosis in HUVECs, and that this effect was closely associated with induction of ER stress and decreased SERCA3 expression.
Keywords: ADMA, ER stress, apoptosis, SERCA
Introduction
The risk of death by cardiovascular disease (CVD) is greatly increased in chronic kidney disease (CKD). Besides the traditional risk factors, uremic toxins may be directly responsible for the pathogenesis of CVD in CKD. Asymmetric dimethylarginine (ADMA) is one of the most important uremic toxins that promote the progression of CKD (1). There is evidence of a strong association among atherosclerosis risk factors and ADMA levels (2–6). In previous reports, ADMA induced endothelial cell apoptosis (7,8), but the molecular biological mechanisms are not clear, yet. Endothelial cell injury and apoptosis can increase vascular permeability and enhance platelet activation and aggregation, thus promoting atherosclerosis and CVD.
Several recent studies proposed a role for endoplasmic reticulum (ER) stress in endothelial cell apoptosis and atherosclerosis. The ER facilitates protein folding and secretion. Impairment of normal ER function leads to an imbalance in protein homeostasis, accompanied by accumulation of misfolded proteins in the ER lumen, a condition referred to as ER stress. Activation of ER stress can ultimately return the ER to its normal physiological state. Three pathways activated during ER stress have been identified so far: Protein kinase RNA-like ER kinase (PERK), inositol requiring enzyme-1 (IRE1) and activating transcription factor 6 (ATF6). After activation of ER stress, improperly folded proteins undergo degradation, leading to expression of target genes including the ER chaperone, 78-kDa glucose-regulated protein (GRP78/BiP), and factors involved in degradation of unfolded proteins. The hypothesized purpose of ER stress is to promote cell survival by restoring ER function. However, prolonged activation of ER stress, an indication that the ER stress cannot be mitigated and homeostasis cannot be reestablished, correlates with cell death. Recently, PERK and IRE1 have been identified as factors involved in cell death (9,10).
The ER stress pathway can be evoked by abnormalities in calcium homeostasis. Calcium actively accumulates by sarco/endoplasmic reticulum calcium-ATPases (SERCAs) in the ER (11,12). Because the SERCA-dependent calcium transport is the only calcium uptake system in this organelle, regulation of SERCA function by the cell constitutes a key regulatory mechanism of calcium homeostasis in the ER. Impaired SERCA function is regarded as a major contributor to ER stress (13,14). The SERCA pump is encoded by a family of three genes, SERCA1, 2 and 3, which are highly conserved and located on different chromosomes (15). Expression of SERCA isoforms is cell-specific and developmentally regulated. SERCA3 has been consistently shown to be co-expressed with SERCA2b in differentiated human umbilical vein endothelial cells (HUVECs) (16,17).
In this study, we investigated whether ER stress is involved in ADMA-induced HUVEC apoptosis. We also explored whether the SERCA pathway is responsible for the ADMA-induced ER stress.
Materials and methods
Chemical reagents
ADMA was from Sigma-Aldrich (St. Louis, MO, USA). GRP78/BiP, IRE1 and cleaved caspase-3 antibodies were obtained from Cell Signaling Technology (Beverly, MA, USA). Bcl2, p-PERK, GAPDH and β-actin antibodies were purchased from Santa Cruz Biotechnology Inc. (Santa Cruz, CA, USA). SERCA2b and SERCA3 antibodies were purchased from Abcam Inc. (Cambridge, MA, USA). All other reagents, unless specially stated, were purchased from Sigma-Aldrich.
Cell culture
Primary HUVECs were from ScienCell Research Laboratories Inc. (Carlsbad, CA, USA). HUVECs were cultured in fibronectin-coated flasks using endothelial cell medium (ECM, Sciencell Inc.) with bullet kit additives (Sciencell Inc.) and 10% (v/v) fetal bovine serum (Sciencell Inc.). HUVECs used in the experiments were at passages 3–4.
Western blot analysis
Total protein was extracted from HUVECs with lysis buffer (50 mM Tris-HCl, pH 7.4, 150 mM NaCl, 1% Triton X-100, 1% sodium deoxycholate, 0.1% SDS and 1% PMSF). Protein concentration was determined using a BCA protein assay kit (Thermo Fisher Scientific, Waltham, MA, USA). Samples were mixed with an equal volume of 5´SDS loading buffer (125 mM Tris-HCl, 4% SDS, 100 mM DTT, 20% glycerol and 0.2% bromophenol blue) and heated at 99°C for 10 min. Subsequently, sample aliquots (20 µg protein each) were resolved on an 8–12% SDS-PAGE gel and the protein bands were electrophoretically transferred onto a nitrocellulose membrane (Amersham International plc., Cardiff, UK). Membranes were blocked with 5% nonfat milk in Tris-buffered saline (TBS) containing 0.1% Tween 20 (TBST) for 2.5 h at room temperature, followed by an overnight incubation with primary antibodies at 4°C. The membranes were then incubated with horseradish peroxidase-conjugated secondary antibodies for 1 h at room temperature, exposed to enhanced chemiluminescence (ECL) kit (Millipore Co., Bedford, MA, USA) and then to Kodak X-OMAT film (Eastman Kodak Inc., Rochester, NY, USA). Primary antibodies and dilutions were: anti-Bcl2 (1:1,000), anti-cleaved caspase-3 (1:1,000), anti-IRE1 (1:1,000), anti-p-PERK (1:1,000), anti-GPR78/BiP (1:1,000), anti-SERCA2b (1:500), anti-SERCA3 (1:500), anti-GAPDH (1:3,000) and anti-β-actin (1:5,000).
Terminal deoxynucleotidyl transferase (TdT)-mediated-digoxigenin-11-dUTP nick end labeling (TUNEL) assay
Apoptotic cells were evaluated by the TUNEL assay, using the In Situ Cell Death Detection kit (Roche Diagnostics, Mannheim, Germany) according to the manufacturer's recommendations. Briefly, cells were fixed with 4% paraformaldehyde for 60 min at room temperature. After washing with phosphate-buffered saline (PBS), the cells were permeabilized with 0.1% Triton X-100 for 2 min at 4°C, and then each sample was incubated with 45 µl of labeling solution plus 5 µl of enzyme solution at 37°C for 1 h. The cells were then washed three times with PBS. Cell nuclei were stained with 4′,6-diamidino-2-phenylindole (DAPI) for 15 min, and then washed with PBS for 5 min at room temperature. Finally, the cells were mounted onto coverslips. Cell images were acquired by fluorescence microscopy (Leica DM 4000B, Germany).
Measurement of SERCA activity
SERCA activity was measured based on Ca2+-dependent ATP hydrolysis and phosphate (Pi) release. HUVECs were incubated with various concentrations of ADMA for 24 h. They were then washed once with cold saline (0.9% NaCl in distilled water) and resuspended in saline. After sonication of samples for 5s, SERCA activity was measured with a Super Microscale Ca2+-ATPase Detection Kit (Nanjing Jiancheng Bioengineering Institute, Nanjing, China) according to the manufacturer's protocol.
Cytosolic Ca2+([Ca2+]cyt) measurements
Cytosolic calcium concentrations were measured using a LEICA TCS SP5 confocal microscope with the calcium-sensitive indicator Fluo-3 AM. Cells were incubated with loading buffer (10 mM HEPES, 0.5 mM Na2HPO4, 137 mM NaCl, 5 mM KCl, 1.3 mM CaCl2, 0.7 mM MgCl2 and 5 mM glucose, pH 7.4) containing 5 µM Fluo-3 AM (Molecular Probes, Eugene, OR, USA) and 0.02% pluronic acid (Molecular Probes) at 37°C for 45 min. The cells were then washed twice with loading buffer. Before measuring fluorescent signals, cells were washed in calcium-free medium to remove any dye nonspecifically associated with the cell surface, and then incubated for another 30 min to allow complete de-esterification of the intracellular AM esters. Changes in intracellular Ca2+ were then monitored by confocal fluorescence microscopy with emission and excitation at 520 and 485 nm, respectively.
Statistical analysis
Data are expressed as mean ± SE. Comparisons among experimental groups were made by one-way ANOVA. Differences in mean values were considered significant at P<0.05.
Results
ADMA treatment of HUVECs induces apoptosis
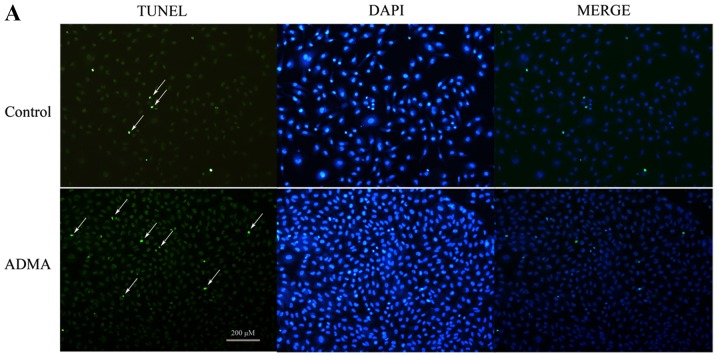
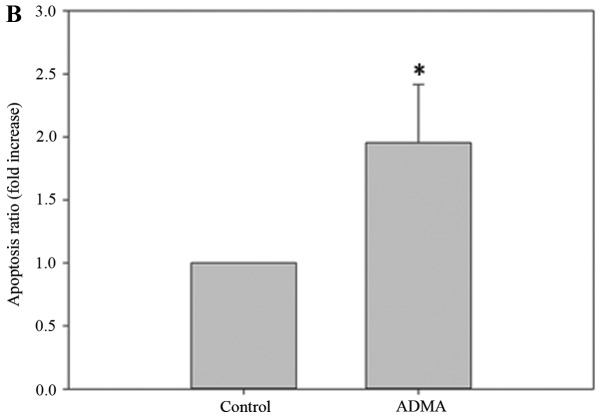
TUNEL staining was used to confirm apoptosis. As shown by TUNEL analysis (Fig. 1), HUVECs treated with 100 µM ADMA had a higher proportion of apoptotic cells than the control HUVECs. Bcl2, an apoptosis inhibitor, is a central modulator of intrinsic apoptosis. In HUVECs incubated with 100 µM ADMA for 0–48 h, Bcl2 was significantly downregulated (Fig. 2A and B). When HUVECs were incubated with various concentrations of ADMA (0–200 µM) for 24 h, the Bcl2 levels decreased in a dose-dependent manner (Fig. 2C and D). Furthermore, we analyzed the expression of cleaved caspase-3, a critical executioner of apoptosis. We found that ADMA increased cleaved caspase-3 expression in a time- and dose-dependent manner (Fig. 2E and F).
Figure 1.
ADMA induces apoptosis in HUVECs. Primary HUVECs were stimulated with 100 µM ADMA for 24 h. Apoptosis was measured by the TUNEL assay (green). DAPI (blue) was used to stain the nuclei of the cells. (A) Representative results out of three experiments. (B) Data of the mean ± SD of three independent experiments. *P<0.05 compared with control.
Figure 2.
ADMA suppresses Bcl2 and increased cleaved caspase-3 expression in HUVECs. (A-D) Cells were treated with the indicated concentration of ADMA (0–200 µM) for 24 h, or incubated with 100 µM ADMA for the indicated time periods. Bcl2 protein levels in cell extracts were analyzed by western blotting. Results are the mean ± SD (n=3). *P<0.05 compared with control. (E and F) Cells were treated with ADMA at the indicated dose (0–200 µM) and time period (0–48 h). Cell extracts were subjected to western blotting using antibodies against cleaved caspase-3.
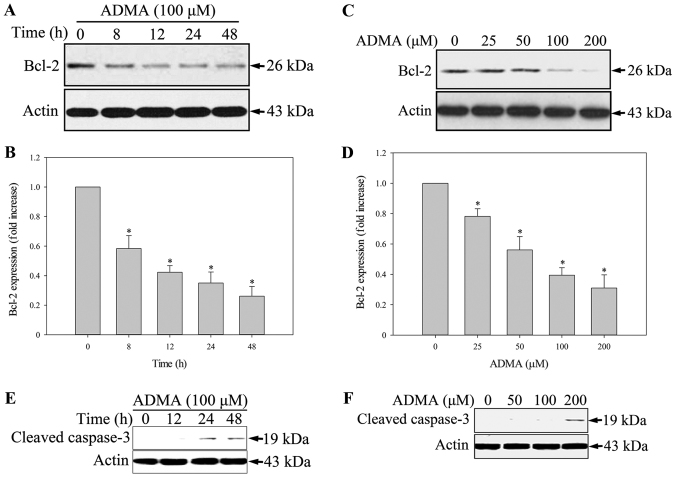
ER stress is involved in ADMA-induced HUVEC apoptosis
The ER stress pathway plays a role in apoptosis induction. Therefore, we investigated whether the ER stress pathway is involved in the ADMA-induced apoptosis in HUVECs. The levels of the ER stress-related protein, GPR78/BiP, and the apoptosis-related ER stress proteins, PERK and IRE1 (9,10), were analysed by western blot. As PERK activation requires phosphorylation, we examined the level of phosphorylated PERK (p-PERK). As expected, ADMA induced PERK phosphorylation, and increased GPR78/BiP and IRE1 expression in HUVECs in a time-dependent manner (Fig. 3A and B). Moreover, ADMA induced p-PERK, GPR78/BiP and IRE1 expression in a dose-dependent manner (Fig. 3C and D). These results indicated that ER stress was involved in ADMA-induced HUVEC apoptosis.
Figure 3.
ADMA induces ER stress-associated cell death in HUVECs. Cells were incubated with 100 µM ADMA for the indicated time periods (A) or with the indicated ADMA concentration (0–200 µM) for 24 h (B). GPR78/BiP expression was analyzed by immunoblotting. (C) Cells were incubated with 100 µM ADMA for the indicated time periods. The protein levels of phosphorylated PERK and IRE1 were examined by immunoblotting. Actin was used as a loading control. (D) After preincubation with various ADMA concentrations (0–200 µM) for 24 h, proteins were extracted and analyzed for p-PERK and IRE1 by western blotting. Results are the mean ± SD (n=3). *P<0.05 compared with control.
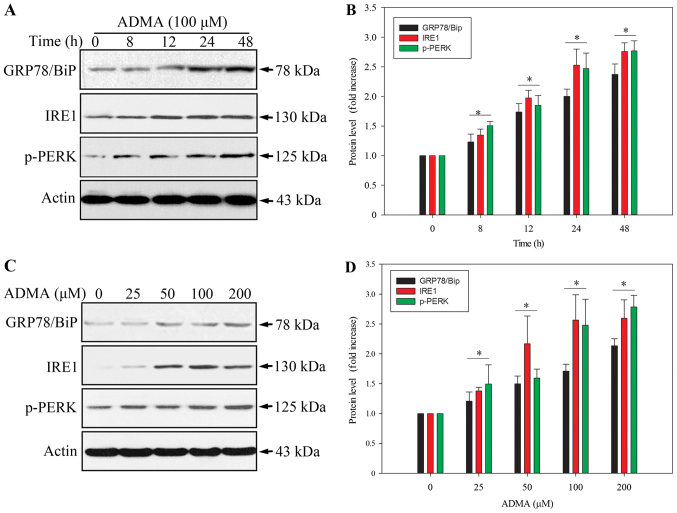
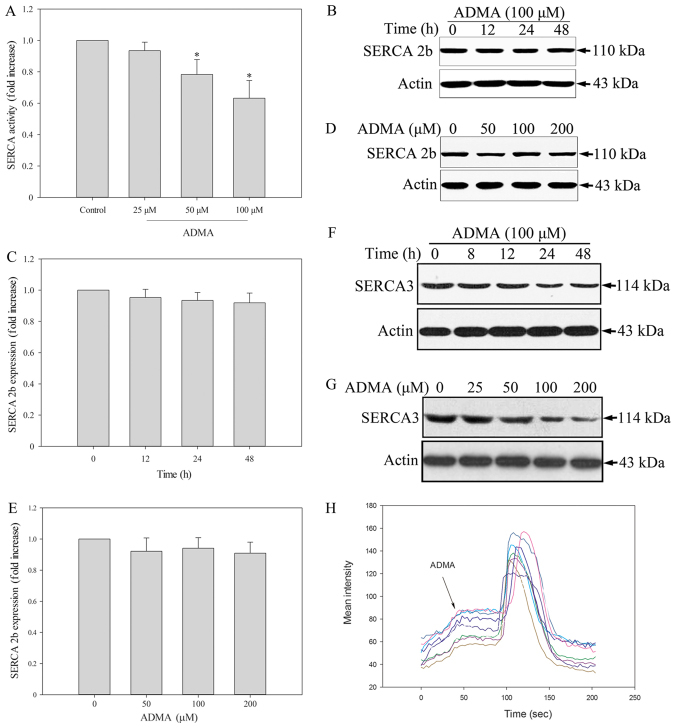
ADMA suppresses SERCA3 expression in HUVECs
A recent study supported an important role for ER calcium homeostasis in the development of apoptosis. Because SERCA is the only calcium pump in the ER, we further hypothesized that its inhibition may evoke ER stress. Thus, we tested whether SERCA is modulated by ADMA by measuring the Ca2+-ATPase activity. The results showed that ADMA (50–100 µM) significantly inhibited SERCA activity in HUVECs (Fig. 4A). Endothelial cells express two distinct isoforms, SERCA2b and SERCA3. It has been reported that in freshly isolated and early passage (P0-P1) HUVECs, SERCA3 was the dominant isoform. After further cell proliferation (P2-P4), there was a reduction in the expression of the SERCA3 isoform in HUVECs and a corresponding increase in SERCA2b (18). Therefore, we measured the levels of both HUVEC-associated SERCA isoforms by western blotting. We found that ADMA induced a slight, but not significant, decrease in SERCA2b protein expression (Fig. 4B-E). In contrast, ADMA induced a statistically significant downregulation of SERCA3 (Fig. 4F and G). This may be the mechanism of ADMA-induced ER stress and apoptosis in HUVECs. A decrease in SERCA expression leads to depletion of ER Ca2+ and increased cytosolic Ca2+ levels ([Ca2+]cyt). We therefore examined the [Ca2+]cyt levels in HUVECs. The change in the [Ca2+]cyt level was measured by confocal imagining using Fluo-3 dye in the presence of extracellular Ca2+. The change in fluorescence intensity after ADMA treatment was recorded, indicating the level of extracellular Ca2+. Fluorescence intensity measurements were made in every 3 sec. We found that ADMA treatment led to increased fluorescence intensity, which means that [Ca2+]cyt increased (Fig. 4H). Coloured lines represent every single cells. This may be the mechanism of ADMA-induced ER stress and apoptosis in HUVECs.
Figure 4.
ADMA treatment leads to increased cytosolic concentrations of free Ca2+ through suppression of SERCA3. (A) HUVECs were stimulated with 0–100 µM ADMA for 24 h and SERCA activity in cell extracts was analyzed. (B-G) HUVECs were incubated with 100 µM ADMA for the indicated time periods or with various ADMA concentrations (0–200 µM) for 24 h. SERCA2 (B-E) and SERCA3 (F and G) levels were determined by immunoblotting. Results are the mean ± SD (n=3). *P<0.05 compared with control. (H) HUVECs were preloaded with Fluo-3 AM, and then stimulated with 75 µM ADMA. Serial Ca2+ images of Fluo-3 fluorescence were recorded at the indicated times (sec).
Discussion
CVD is the leading cause of death among CKD patients. There is an urgent need to characterize novel pathways and identify new therapeutic targets to control CVD progression. ADMA is a significant uremic toxin and its levels are elevated in CKD, even at the early stages. In a large cohort of subjects, those with higher ADMA levels had an increased risk of death attributed to cardiovascular disorders (19). Consistently, circulating ADMA levels have been shown to be independently associated with cardiovascular risk, death and incidence of CVD outcomes (5,6,20,21).
As an endogenous inhibitor of nitric oxide (NO) synthase, ADMA can reduce NO production. NO is a key factor maintaining vascular homeostasis. By reducing NO generation, ADMA can influence endothelial dysfunction (1). However, ADMA acts through mechanisms beyond its NO synthase inhibition. In previous reports, ADMA induced endothelial cell apoptosis (7,8). In our study, we also found that ADMA induced cleaved caspase-3 expression and decreased Bcl2 expression. These results demonstrated that endothelial cell apoptosis may contribute to ADMA-induced vascular injury.
ER stress results from the accumulation of misfolded proteins in the ER lumen. The likely purpose of ER stress is to help remove misfolded proteins and promote cell survival. However, prolonged ER stress triggers apoptosis. Among the three known ER stress sensors, PERK and IRE1 can trigger the cellular apoptosis program. Under normal conditions, BiP/GRP78 associates with and inactivates ER stress sensor proteins. Under stress conditions, GRP78/BiP dissociates from the ER sensor proteins, activating downstream signal transduction to rescue ER homeostasis. Increased GRP78/BiP levels in the ER compartment have been regarded as evidence for induction of ER stress. Several studies have strongly supported a central role for the ER stress response in the pathogenesis of endothelial dysfunction and CVD. Alleviating ER stress may thus represent a promising therapeutic approach for preventing or improving CVD. These studies led us to investigate whether ADMA induces ER stress in HUVECs. We confirmed that ADMA induced p-PERK, IRE1 and GRP78/BiP expression in a time- and dose-dependent manner, indicating activation of the ER stress response. We further explored the possible mechanisms involved in ADMA-induced ER stress.
High concentrations of Ca2+ in the ER lumen ([Ca2+]ER) are essential for normal ER folding capacity (13). SERCA, localized in the ER membrane, lowers [Ca2+]cyt by pumping Ca2+ from the cytosol into the ER. Inhibition of SERCA activity impaired ER Ca2+ homeostasis and caused prolonged ER stress (13,14). We therefore hypothesized that a disturbance in SERCA activity is the major cause of ADMA-induced ER stress in HUVECs. We found that ADMA inhibited the SERCA activity in HUVECs. The SERCA pump is coded by a family of three genes, SERCA1, 2 and 3, encoding the SERCA1, SERCA2 and SERCA3 isoforms, respectively. SERCA isoform expression is specific to cell type and developmental stages (15). While SERCA2b is a ubiquitous isoform expressed in muscle and non-muscle cells, the SERCA3 isoform is primarily expressed in non-muscle, especially endothelial, cells (16,17). Freshly isolated HUVECs contain only SERCA3 and no SERCA2b mRNA. These SERCA expression patterns change with increased cell proliferation. SERCA3 mRNA decreased, while that for SERCA2b increased, with increasing passages in culture. Because we used HUVECs at passages 3 and 4, we examined both SERCA2b and SERCA3 protein expression after ADMA stimulation. We found that ADMA slightly decreased SERCA2b expression, but more significantly reduced SERCA3 expression. This indicated that the ADMA-induced effects on SERCA were isoform-dependent. We also examined the changes in [Ca2+]cyt in HUVECs in response to ADMA. We used Fluo-3 to detect the calcium levels in the cytoplasm. We found that the fluorescence intensity greatly increased after addition of ADMA to the culture medium. This result indicated that the [Ca2+]cyt levels increased in HUVECs after ADMA stimulation.
Our results are consistent with other studies reporting that ADMA induced the ER stress response in many different cell types, such as mesangial cells, adipocytes, macrophages, glomerular endothelial cells and lung epithelial cells (22–27). These results implicated ER stress as the common pathway through which ADMA contributes to a variety of human diseases, including CKD, diabetes mellitus and liver disease. Thus, inhibition of ER stress and related pathways may be effective as a wide range treatment. However, there are a few limitations in our study. First, the SERCA isoforms expressed in HUVECs are influenced by the number of passages. Additionally, after 5 or 6 passages the cell phenotype changes to another phenotype, such as fibroblasts. Therefore, in this study we used cells from passages 3 and 4, which may be the main reason behind the finding that ADMA only obviously inhibited SERCA3, as it is the main isoform in the these passages. Hence, this in vitro expreiement is limited by the cell culture. Thus, futher in vivo experiments are required, to elucidate which isoforms are the main ones responsible for ADMA-induced ER stress in vascular cells. Moreover, in the normal population, the plasma level of ADMA is 0.92–0.11 µM (28,29). However, the plasma levels of ADMA are increased in some diseases, such as CKD, diabetes, cardiovascular disease and hypertension (30–32). Hemodialysis patients with atherosclerosis show significantly higher ADMA levels of up to 7.31 µM (33). However, when we performed experiments to study the toxicity mechanisms of ADMA in vitro, much larger doses (0–200 µM) than the pathological concentrations in clinical patients were required (22,25,34). Therefore, wheher ADMA inhibits SERCA3 expression and induces ER stress during long-term ADMA accumulation in the human body still need to be explored in future in vivo studies.
In conclusion, we think that ADMA-induced ER stress and apoptosis are closely related to the decrease in SERCA3 expression.
In this study, we found that ADMA induced ER stress, decreased Bcl2 expression and ultimately induced apoptosis in HUVECs. In addition, ADMA decreased SERCA3 activity and expression. Together, our results indicated that ADMA induced growth suppression and apoptosis in HUVECs, effects that are related to activation of ER stress and inhibition of SERCA3 expression. Developing therapies that directly target the defective endogenous SERCA enzyme to correct Ca2+ imbalances in the ER may constitute a novel approach for treating ADMA-induced vascular injury.
Acknowledgements
The authors would like to thank the BeiJing Talents Fund (no. 2016000021469G223) for financial support.
References
- 1.Vallance P, Leone A, Calver A, Collier J, Moncada S. Accumulation of an endogenous inhibitor of nitric oxide synthesis in chronic renal failure. Lancet. 1992;339:572–575. doi: 10.1016/0140-6736(92)90865-Z. [DOI] [PubMed] [Google Scholar]
- 2.Konya H, Miuchi M, Satani K, Matsutani S, Yano Y, Tsunoda T, Ikawa T, Matsuo T, Ochi F, Kusunoki Y, et al. Asymmetric dimethylarginine, a biomarker of cardiovascular complications in diabetes mellitus. World J Exp Med. 2015;5:110–119. doi: 10.5493/wjem.v5.i2.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Böger RH, Maas R, Schulze F, Schwedhelm E. Asymmetric dimethylarginine (ADMA) as a prospective marker of cardiovascular disease and mortality-an update on patient populations with a wide range of cardiovascular risk. Pharmacol Res. 2009;60:481–487. doi: 10.1016/j.phrs.2009.07.001. [DOI] [PubMed] [Google Scholar]
- 4.Landim MB, Filho A Casella, Chagas AC. Asymmetric dimethylarginine (ADMA) and endothelial dysfunction: Implications for atherogenesis. Clinics. 2009;64:471–478. doi: 10.1590/S1807-59322009000500015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schnabel R, Blankenberg S, Lubos E, Lackner KJ, Rupprecht HJ, Espinola-Klein C, Jachmann N, Post F, Peetz D, Bickel C, et al. Asymmetric dimethylarginine and the risk of cardiovascular events and death in patients with coronary artery disease: Results from the AtheroGene Study. Circ Res. 2005;97:e53–e59. doi: 10.1161/01.RES.0000181286.44222.61. [DOI] [PubMed] [Google Scholar]
- 6.Lu TM, Ding YA, Charng MJ, Lin SJ. Asymmetrical dimethylarginine: A novel risk factor for coronary artery disease. Clin Cardiol. 2003;26:458–464. doi: 10.1002/clc.4960261006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li J, Zhang Z, Lv L, Qiao H, Chen X, Zou C. (−)-epigallocatechin gallate inhibits asymmetric dimethylarginine-induced injury in human brain microvascular endothelial cells. Neurochem Res. 2016;41:1868–1876. doi: 10.1007/s11064-016-1898-9. [DOI] [PubMed] [Google Scholar]
- 8.Ma J, Zhao S, Gao G, Chang H, Ma P, Jin B. probucol protects against asymmetric dimethylarginine-induced apoptosis in the cultured human brain microvascular endothelial cells. J Mol Neurosci. 2015;57:546–553. doi: 10.1007/s12031-015-0635-1. [DOI] [PubMed] [Google Scholar]
- 9.Walter P, Ron D. The unfolded protein response: From stress pathway to homeostatic regulation. Science. 2011;334:1081–1086. doi: 10.1126/science.1209038. [DOI] [PubMed] [Google Scholar]
- 10.Woehlbier U, Hetz C. Modulating stress responses by the UPRosome: a matter of life and death. Trends in Biochem Sci. 2011;36:329–337. doi: 10.1016/j.tibs.2011.03.001. [DOI] [PubMed] [Google Scholar]
- 11.Zarain-Herzberg A, Garcia-Rivas G, Estrada-Aviles R. Regulation of SERCA pumps expression in diabetes. Cell Calcium. 2014;56:302–310. doi: 10.1016/j.ceca.2014.09.005. [DOI] [PubMed] [Google Scholar]
- 12.Brini M, Cali T, Ottolini D, Carafoli E. The plasma membrane calcium pump in health and disease. FEBS J. 2013;280:5385–5397. doi: 10.1111/febs.12193. [DOI] [PubMed] [Google Scholar]
- 13.Fu S, Yang L, Li P, Hofmann O, Dicker L, Hide W, Lin X, Watkins SM, Ivanov AR, Hotamisligil GS. Aberrant lipid metabolism disrupts calcium homeostasis causing liver endoplasmic reticulum stress in obesity. Nature. 2011;473:528–531. doi: 10.1038/nature09968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Li W, Ouyang Z, Zhang Q, Wang L, Shen Y, Wu X, Gu Y, Shu Y, Yu B, Wu X, et al. SBF-1 exerts strong anticervical cancer effect through inducing endoplasmic reticulum stress-associated cell death via targeting sarco/endoplasmic reticulum Ca(2+)-ATPase 2. Cell Death Dis. 2014;5:e1581. doi: 10.1038/cddis.2014.538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Periasamy M, Kalyanasundaram A. SERCA pump isoforms: Their role in calcium transport and disease. Muscle Nerve. 2007;35:430–442. doi: 10.1002/mus.20745. [DOI] [PubMed] [Google Scholar]
- 16.Lipskaia L, Keuylian Z, Blirando K, Mougenot N, Jacquet A, Rouxel C, Sghairi H, Elaib Z, Blaise R, Adnot S, et al. Expression of sarco (endo) plasmic reticulum calcium ATPase (SERCA) system in normal mouse cardiovascular tissues, heart failure and atherosclerosis. Biochim Biophys Acta. 2014;1843:2705–2718. doi: 10.1016/j.bbamcr.2014.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mountian I, Manolopoulos VG, De SH, Parys JB, Missiaen L, Wuytack F. Expression patterns of sarco/endoplasmic reticulum Ca(2+)-ATPase and inositol 1,4,5-trisphosphate receptor isoforms in vascular endothelial cells. Cell Calcium. 1999;25:371–380. doi: 10.1054/ceca.1999.0034. [DOI] [PubMed] [Google Scholar]
- 18.Anger M, Samuel JL, Marotte F, Wuytack F, Rappaport L, Lompré AM. In situ mRNA distribution of sarco (endo)plasmic reticulum Ca (2+)-ATPase isoforms during ontogeny in the rat. J Mol Cell Cardiol. 1994;26:1–550. doi: 10.1006/jmcc.1994.1064. [DOI] [PubMed] [Google Scholar]
- 19.Valkonen VP, Päivä H, Salonen JT, Lakka TA, Lehtimäki T, Laakso J, Laaksonen R. Risk of acute coronary events and serum concentration of asymmetrical dimethylarginine. Lancet. 2001;358:2127–2128. doi: 10.1016/S0140-6736(01)07184-7. [DOI] [PubMed] [Google Scholar]
- 20.Nicholls SJ, Wang Z, Koeth R, Levison B, DelFraino B, Dzavik V, Griffith OW, Hathaway D, Panza JA, Nissen SE, et al. Metabolic profiling of arginine and nitric oxide pathways predicts hemodynamic abnormalities and mortality in patients with cardiogenic shock after acute myocardial infarction. Circulation. 2007;116:2315–2324. doi: 10.1161/CIRCULATIONAHA.107.693986. [DOI] [PubMed] [Google Scholar]
- 21.Tousoulis D, Bouras G, Antoniades C, Marinou K, Papageorgiou N, Miliou A, Hatzis G, Stefanadi E, Tsioufis C, Stefanadis C. Methionine-induced homocysteinemia impairs endothelial function in hypertensives: The role of asymmetrical dimethylarginine and antioxidant vitamins. Am J Hypertens. 2011;24:936–942. doi: 10.1038/ajh.2011.65. [DOI] [PubMed] [Google Scholar]
- 22.Park MJ, Oh KS, Nho JH, Kim GY, Kim DI. Asymmetric dimethylarginine (ADMA) treatment induces apoptosis in cultured rat mesangial cells via endoplasmic reticulum stress activation. Cell Biol Int. 2016;40:662–670. doi: 10.1002/cbin.10602. [DOI] [PubMed] [Google Scholar]
- 23.Hong D, Gao HC, Wang X, Li LF, Li CC, Luo Y, Wang KK, Bai YP, Zhang GG. Asymmetric dimethylarginine triggers macrophage apoptosis via the endoplasmic reticulum stress pathway. Mol Cell Biochem. 2015;398:31–38. doi: 10.1007/s11010-014-2202-4. [DOI] [PubMed] [Google Scholar]
- 24.Leng YP, Qiu N, Fang WJ, Zhang M, He ZM, Xiong Y. Involvement of increased endogenous asymmetric dimethylarginine in the hepatic endoplasmic reticulum stress of type 2 diabetic rats. PLoS One. 2014;9:e97125. doi: 10.1371/journal.pone.0097125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Guo W, Ding J, Zhang A, Dai W, Liu S, Diao Z, Wang L, Han X, Liu W. The inhibitory effect of quercetin on asymmetric dimethylarginine-induced apoptosis is mediated by the endoplasmic reticulum stress pathway in glomerular endothelial cells. Int J Mol Sci. 2014;15:484–503. doi: 10.3390/ijms15010484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhou QG, Zhou M, Hou FF, Peng X. Asymmetrical dimethylarginine triggers lipolysis and inflammatory response via induction of endoplasmic reticulum stress in cultured adipocytes. Am J Physiol Endocrinol Metab. 2009;296:E869–E878. doi: 10.1152/ajpendo.91011.2008. [DOI] [PubMed] [Google Scholar]
- 27.Lim SK, Choi H, Park MJ, Kim DI, Kim JC, Kim GY, Jeong SY, Rodionov RN, Han HJ, Yoon KC, Park SH. The ER stress-mediated decrease in DDAH1 expression is involved in formaldehyde-induced apoptosis in lung epithelial cells. Food Chem Toxicol. 2013;62:763–769. doi: 10.1016/j.fct.2013.10.014. [DOI] [PubMed] [Google Scholar]
- 28.Lundman P, Eriksson MJ, Stühlinger M, Cooke JP, Hamsten A, Tornvall P. Mild-to-moderate hypertriglyceridemia in young men is associated with endothelial dysfunction and increased plasma concentrations of asymmetric dimethylarginine. J Am Coll Cardiol. 2001;38:111–116. doi: 10.1016/S0735-1097(01)01318-3. [DOI] [PubMed] [Google Scholar]
- 29.Surdacki A, Nowicki M, Sandmann J, Tsikas D, Boeger RH, Bode-Boeger SM, Kruszelnicka-Kwiatkowska O, Kokot F, Dubiel JS, Froelich JC. Reduced urinary excretion of nitric oxide metabolites and increased plasma levels of asymmetric dimethylarginine in men with essential hypertension. J Cardiovasc Pharmacol. 1999;33:652–658. doi: 10.1097/00005344-199904000-00020. [DOI] [PubMed] [Google Scholar]
- 30.Alpoim PN, Sousa LP, Mota AP, Rios DR, Dusse LM. Asymmetric dimethylarginine (ADMA) in cardiovascular and renal disease. Clin Chim Acta. 2015;440:1–39. doi: 10.1016/j.cca.2014.11.002. [DOI] [PubMed] [Google Scholar]
- 31.Tousoulis D, Georgakis MK, Oikonomou E, Papageorgiou N, Zaromitidou M, Latsios G, Papaioannou S, Siasos G. Asymmetric dimethylarginine: Clinical significance and novel therapeutic approaches. Curr Med Chem. 2015;22:2871–2901. doi: 10.2174/0929867322666150625095046. [DOI] [PubMed] [Google Scholar]
- 32.Santilli F, Liani R, Di Fulvio P, Formoso G, Simeone P, Tripaldi R, Ueland T, Aukrust P, Davì G. Increased circulating resistin is associated with insulin resistance, oxidative stress and platelet activation in type 2 diabetes mellitus. Thromb Haemost. 2016;116:1089–1099. doi: 10.1160/TH16-06-0471. [DOI] [PubMed] [Google Scholar]
- 33.Kielstein JT, Böger RH, Bode-Böger SM, Schäffer J, Barbey M, Koch KM, Frölich JC. Asymmetric dimethylarginine plasma concentrations differ in patients with end-stage renal disease: Relationship to treatment method and atherosclerotic disease. J Am Soc Nephrol. 1999;10:594–600. doi: 10.1681/ASN.V103594. [DOI] [PubMed] [Google Scholar]
- 34.Wang LY, Zhang DL, Zheng JF, Zhang Y, Zhang QD, Liu WH. Apelin-13 passes through the ADMA-damaged endothelial barrier and acts on vascular smooth muscle cells. Peptides. 2011;32:2436–2443. doi: 10.1016/j.peptides.2011.10.001. [DOI] [PubMed] [Google Scholar]