Abstract
Introduction
Post-transplant infections have been studied widely but data on comparisons of deceased donor liver transplants (DDLT) and living donor liver transplants (LDLT), type and timings of infections, and their relations to outcomes are not explored.
Material and methods
We analysed data from 612 participants of the Adult-to-Adult Living Donor Liver Transplantation Study (A2ALL), a retrospective data set of LDLT and DDLT. We compared the type and timing of the first post-transplant infection in relation to transplant outcomes between the two groups.
Results
Out of 611 patients, 24.5% experienced the first post-transplant infection, the majority of which were bacterial (35.3%), followed by fungal (11%) and viral infections (4.2%). There was no significant difference in the rate, type or timing of infection between LDLT and DDLT. Patients with late (> 1 year) first infection were 1.8 times more likely to die (95% CI: 1.12-2.98, p = 0.015) and 9 times more likely to have graft failures (95% CI: 3.26-24.8, p < 0.001). DDLT recipients who experienced bacterial infection had a significantly lower survival rate compared to LDLT recipients (p < 0.001).
Conclusions
Late infection is associated with lower survival in both DDLT and LDLT. Bacterial infection might be more detrimental for DDLT than LDLT. Late infection should be managed aggressively to improve outcomes.
Keywords: infection, mortality, liver transplantation, graft failure, A2ALL
Introduction
The prevalence of post-transplant infection has been reported from 41% to 56% in liver transplant recipients [1], with two-thirds being bacterial [2, 3]. It has been reported that 80% of recipients are found to have at least one infection during the first post-transplant year [4]. Opportunistic infections are generally absent during the first month after transplantation, since the full effect of immunosuppression is not yet present. Infections such as viraemia and candidaemia in this period are generally donor-derived or recipient-derived, or they are associated with technical complications of surgery [5]. Conversely, infectious complications during the late transplant period continue to impose a high clinical burden, with 85% occurring 6 months after transplantation [6]. These conflicting reviews on early and late post-transplant infections and their effect on outcomes in transplant recipients need further exploration to decrease post-transplant morbidity and mortality.
Moreover, immunologic and technical advances have improved infection control and post-transplant graft and patient survival, but improvements in immune monitoring and rejection management are required to increase the rates of re-transplantation success [7]. Re-transplant outcomes are poorly understood in liver transplants especially amongst patients receiving living donor transplants. It has been reported that re-transplantation outcomes after living donor liver transplants are not different from other re-transplant procedures despite the greater severity of illness in these patients [8].
The use of adult-to-adult living donor transplants (ALDLT) was first reported in the United States in 1998 [9]; it has now reached figures of over 1600 patients transplanted at 94 centres across the US [10]. We used data from the Adult-to-Adult Living Donor Liver Transplant Study (A2ALL), the largest North American experience of living donor liver transplants (LDLT) [11] to explore the timing and effect of first post-transplant infection on outcomes in living versus deceased donor transplants. Specific aims including the differences found between living versus deceased donor transplant recipients and early versus late post-transplant periods were focused on.
Material and methods
Study sample
The A2ALL consisted of both retrospective and prospective studies of LDLT. Legacy data from the A2ALL retrospective cohort are housed in the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) Data Repository [12, 13]. The current study was approved by the Institutional Review Board at Rhode Island Hospital and the approval submitted to NIDDK data repository for the acquisition of A2ALL data.
The A2ALL Study aimed to determine the survival benefit of ALDLT. Starting at the time a potential ALDLT recipient identified a potential donor (defined as the date of initial potential donor history and physical examination), survival of those who eventually received an ALDLT was compared with those who continued on the waiting list for a deceased donor liver transplant. Comparisons of ALDLT recipients to recipients of deceased donor liver transplants (DDLT) have been reported in several A2ALL publications [10, 11, 14]. For the purposes of the current study, data collected for the overall study objective were used to focus on details of infections and transplant and re-transplant outcomes of recipients of both LDLT and DDLT.
The A2ALL retrospective cohort comprised 819 adult patients. The A2ALL data for this study include 612 patients who had a potential living donor (207 patients did not have data on post-transplant infections and were excluded). Of these 612 potential recipients receiving LDLT or DDLT, 611 had follow-up data entered (1 patient had incomplete follow-up data and was excluded from the survival analysis).
Outcome measures
The primary endpoints for this analysis were death, graft failure and re-transplant. The secondary endpoints included types and timings of first post-transplant infections. The relationship of the timing of infection to outcomes was split by early and late infections. Patients were divided into groups based on whether they had episodes of first post-transplant infection beyond 1 month after transplant or beyond 1 year after transplant such that:
early post-transplant infections occurred ≤ 30 days,
early-late post-transplant infections occurred > 30 days ≤ 1 year,
late post-transplant infections occurred > 1 year.
The relationship of type of infection to outcomes was split by bacterial, viral and fungal infections.
Statistical analysis
All analyses were carried out using SAS version 9.4 (The SAS Institute, Cary, NC). Each of the primary endpoints represented events occurring over time and so a combination of Kaplan-Meier estimated survival analysis and proportional hazards (Cox) regression was used. The Wilcoxon weighting of the χ2 test statistic, which reduces the influence of differences as the effective sample size decreases over time, was used when comparing estimated survival functions. All time-to-event outcomes were right-censored at 2 years, as effective sample sizes became prohibitively small (< 20) after this length of follow-up for most analyses. Proportional hazards regressions were constructed with both time-invariant and time-varying covariates, depending on the hypothesis being tested. For hypotheses containing more than one factor, fully factorial models were constructed including all higher order interactions. Non-significant interactions were removed in a backwards stepwise fashion, but the original main effect factors were left in each model. Alpha was conventionally set to 0.05. All model parameters (e.g. mean, hazard ratio) were presented with their 95% confidence intervals. Factors such as disease severity of recipients prior to transplant, type and quality of graft used, surgical and medical complications, and all other factors previously published in the A2ALL studies [15-20], were accounted for statistical interactions in our study. No significant interactions (p > 0.05) were found.
Results
Out of a total of 612 patients, 611 were included in the survival analyses (1 DDLT patient had incomplete data). The average age of the patients was 50.0 ± 10.7 years with 354 (57.8%) males and 258 (42.2%) females. The donors were either cadaveric (220; 35.9%) or living (392; 64.1%). The most common primary diagnosis was cirrhosis due to hepatitis C virus (18.5%). The baseline demographics, infections and outcomes overall and split by LDLT versus DDLT are displayed in Table 1. The demographics of LDLT versus DDLT were comparable except for the mean ages of the two groups where LDLT was 49.2 ± 11.0 years and DDLT was 51.4 ± 10.1 years (p = 0.013).
Table 1.
Demographics, infections and outcomes amongst the transplant recipients
| Characteristics | Overall (N = 612) | LDLT (n = 392) | DDLT (n = 220) |
|---|---|---|---|
| Age | 50.0 ± 10.7 | 49.2 ± 11.0 | 51.4 ± 10.1 |
| Gender | |||
| Male | 354 (57.8%) | 225 (57.4%) | 129 (58.6%) |
| Female | 258 (42.2%) | 167 (42.6%) | 91 (41.4%) |
| Infection type | |||
| Bacterial | 215 (35.1%) | 141 (36.0%) | 74 (33.6%) |
| Wound | 66 (10.8%) | 42 | 24 |
| Bile duct | 45 (7.4%) | 37 | 8 |
| Blood | 103 (16.8%) | 71 | 32 |
| Liver | 14 (2.3%) | 12 | 2 |
| Pulmonary | 59 (9.6%) | 36 | 23 |
| CNS | 2 (0.3%) | 2 | 0 |
| Urinary tract | 64 (10.5%) | 37 | 27 |
| Viral | 27 (4.2%) | 13 | 14 |
| Wound | 0 (0.0%) | 0 | 0 |
| Bile duct | 1 (0.2%) | 1 | 0 |
| Blood | 16 (2.6%) | 7 | 9 |
| Liver | 2 (0.3%) | 2 | 0 |
| Pulmonary | 7 (1.1%) | 2 | 5 |
| CNS | 2 (0.3%) | 2 | 0 |
| Urinary tract | 1 (0.2%) | 1 | 0 |
| Fungal | 63 (11.1%) | 37 | 26 |
| Wound | 12 (2.0%) | 9 | 3 |
| Bile duct | 2 (0.3%) | 2 | 0 |
| Blood | 19 (3.1%) | 11 | 8 |
| Liver | 6 (1.0%) | 6 | 0 |
| Pulmonary | 23 (3.8%) | 8 | 15 |
| CNS | 5 (0.8%) | 5 | 0 |
| Urinary tract | 21 (3.4%) | 7 | 14 |
| Re-transplants | 54 (8.8%) | 43 (11.0%) | 11 (5.0%) |
| Graft failures | 87 (14.2%) | 66 (16.8%) | 21 (9.5%) |
| Deaths | 158 (25.8%) | 104 (26.5%) | 53 (24.1%) |
LDLT – living donor liver transplant, DDLT – deceased donor liver transplant, CNS – central nervous system
During a median follow-up period of 2.3 years (interquartile range: 2.6 years), 54 (8.8%) patients underwent a re-transplant. There were 87 (14.2%) graft failures and 158 (25.8%) deaths (Table 1).
The most common type of infection encountered in the post-transplant period (median 2.3 years: IQ 2.6 years) was bacterial (35.3%) followed by fungal (11.1%) and viral (4.2%). The most common bacterial infections observed were bacterial blood infections (103/219, 47.0%). Pulmonary infections (23/63, 36.5%) formed the majority amongst those who experienced fungal infections while blood infections (16/27, 59.3%) were in preponderance amongst those who experienced viral infections. The rates of infection were similar between the two groups.
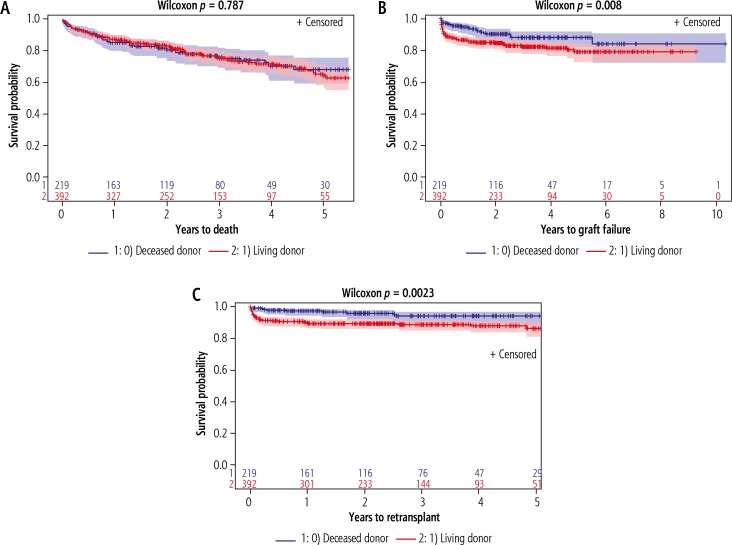
Figure 1 shows deaths, graft failures and re-transplants amongst LDLT versus DDLT patients. There was no significant difference in mortality rate between patients receiving LDLT and those receiving DDLT (p = 0.787) (Fig. 1A). Patients receiving DDLT had better rates of graft survival compared to LDLT (p = 0.008) (Fig. 1B). The rates of re-transplant free survival were better in DDLT than LDLT (p = 0.0023) (Fig. 1C).
Fig. 1.
A) Deaths in recipients of Adult-to-Adult Living Donor Liver Transplantation Study (A2ALL) cohort: living donor liver transplants (LDLT) (n = 392) versus deceased donor liver transplants (DDLT) (n = 219). B) Graft failures in recipients of A2ALL cohort: LDLT (n = 392) versus DDLT (n = 219). C) Re-transplants in recipients of A2ALL cohort: LDLT (n = 392) versus DDLT (n = 219)
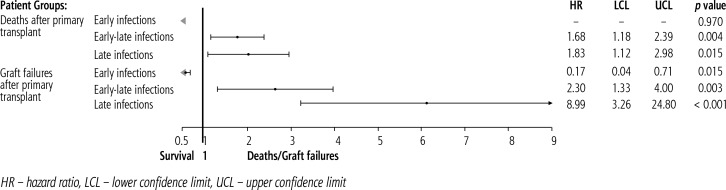
Patients with the first infection in the early-late period were 1.7 times more likely to die (p = 0.004) and 2.3 times more likely to have graft failures (p = 0.003) compared to those having an early first infection (Fig. 2). Patients with late first infection were similarly 1.8 times more likely to die (p = 0.015)) and 9 times more likely to have graft failures (p < 0.001) compared to patients with early first infection (Fig. 2).
Fig. 2.
Forest plot showing effect of early (≤ 30 days), early-late (> 30 days ≤ 1 year) and late infections (> 1 year) on post-transplant outcomes in Adult-to-Adult Living Donor Liver Transplantation Study (A2ALL) cohort: deaths/graft failures.
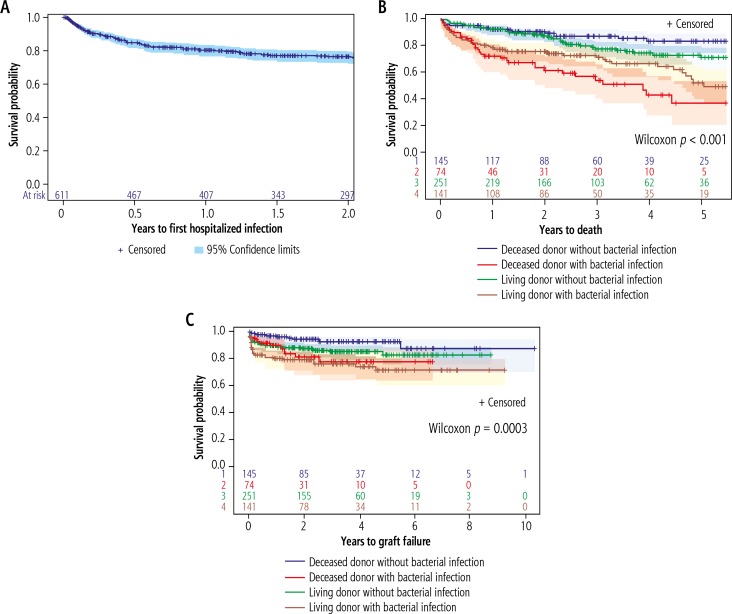
The occurrence of first post-transplant infection over the follow-up period in the whole group is shown in Figure 3A. 150 patients out of the total of 611 experienced first post-transplant infection, the majority of which were bacterial. Amongst the patients available for survival analyses, out of a total of 219 DDLT patients, 74 (33.8%) experienced a bacterial infection, while amongst the 392 LDLT patients, 141 (36.0%) experienced a bacterial infection. Figure 3B displays the overall survival of DDLT versus LDLT patients experiencing first post-transplant bacterial infection. LDLT patients seemed to have better survival rates after experiencing bacterial infections than DDLT (p < 0.001). The DDLT patients without bacterial infection had the highest overall survival rates, followed by LDLT without bacterial infection, followed by LDLT with bacterial infection and lastly DDLT with bacterial infection (Fig. 3B).
Fig. 3.
A) Years to first infection in recipients of Adult-to-Adult Living Donor Liver Transplantation Study (A2ALL) cohort: 150 patients had a first infection of some type. B) Deaths in patients with bacterial infections: living donor liver transplants (LDLT) (n = 392) versus deceased donor liver transplants (DDLT) (n = 219). C) Graft failures in patients with bacterial infections: LDLT (n = 392) versus DDLT (n = 219)
Figure 3C presents the Kaplan-Meier (KM) plots for graft survival amongst DDLT versus LDLT patients experiencing post-transplant bacterial infections. The effects of bacterial infection on graft survival rates were similar to the overall group, with highest rates of graft survival of DDLT without bacterial infection, followed by LDLT without bacterial infection, followed by DDLT with bacterial infection, and the lowest rates of graft survival of LDLT with bacterial infection (p = 0.0006).
The viral and fungal infections were not explored over time due to low post-transplant occurrence of these infections.
Discussion
The A2ALL study reported significant superiority of LDLT graft survival rates over DDLT after the first 20 cases at each centre [10]. It also reported post-transplant complications to be more commonly biliary-related and hepatic artery thrombosis amongst LDLT recipients, while ascites, intra-abdominal bleeding, cardiac complications and pulmonary oedema were more common in DDLT recipients [14]. The current study based on 612 A2ALL participants receiving LDLT and DDLT demonstrates that early-late and late first infection after transplant is a significant predictor of poorer post-transplant outcomes in recipients of both living and deceased donors (Fig. 2) Furthermore, in this post-hoc analysis post-transplant bacterial infection was associated with poorer overall survival rates amongst DDLT recipients than LDLT (p < 0.001) (Fig. 3B).
The most common bacterial infections encountered by A2ALL patients were bloodstream infections (103/215). The preponderance of bacterial bloodstream infections (33.3%) amongst others has been reported before [7]. Identified risk factors for bloodstream infections after liver transplants include diabetes mellitus, hypoproteinaemia, catheterization, preoperative massive effusion or ascites, preoperative Staphylococcus aureus carriage, post-transplant haemodialysis, operative blood loss, reoperation, need for mechanical ventilation, and bile duct complications [21-24]. Many of these factors have been reported in the A2ALL group [14], supporting the previously reported findings. Fungal infections were also found comparative (11.1%) to previously reported findings of 5% to 42% [25, 26].
We report the timing of first post-transplant infection and its effects on outcomes in both LDLT and DDLT patients (Fig. 2). There was no significant difference between these effects in LDLT versus DDLT (p = 0.754), but we found that early-late first infection is associated with a 1.7 (p = 0.004) times higher mortality rate and 2.3 (p = 0.003) times higher graft failure rate than early first infection in the overall A2ALL group (including both LDLT and DDLT). On further exploration, we found that late first post-transplant infections had an even greater effect on outcomes (Fig. 2). Early, intermediate and late post-transplant infections have been described well in solid organ transplants [5], but data on the timing of post-transplant infection and its effects on outcomes are limited in liver transplants. It has been reported by Hamandi et al. that infectious complications in solid organ transplants require hospitalisation in 603 of 1414 readmissions at a rate of 0.43 episodes per 1000 transplant-days (95% CI: 0.40-0.47), with 85% occurring after 6 months following transplantation [6]. Conversely, Tu et al. report most post-DDLT infections (61.9%) occurring within the first week of transplant, and the 1- and 3-year survival rates without infection significantly increased compared with recipients with infection (p = 0.007) [27]. It is important to know the timings, rate and type of infections after LDLT and DDLT since these infections are not just a controllable risk factor for failure but there has also been a recent quest for markers such as neopterin, associating 1-year posttransplant infections with mortality [28].
Moreover, bacterial infections after liver transplant have also been reported to increase mortality, hospital stays and hence healthcare costs [29]. In this study, we report better overall survival rates of LDLT with post-transplant bacterial infection than DDLT with infection (p < 0.001). The graft survival rates of DDLT patients with post-transplant bacterial infections was however superior to LDLT with post-transplant bacterial infections (p = 0.0006). The reasons behind the overall survival benefit of LDLT with bacterial infection and the graft survival benefit of DDLT with bacterial infection remain uncertain due to interactions of infection and immunosuppression. Trevizol et al. identified nosocomial spread and inappropriate antibiotic use as reasons for a mortality rate of 46.7% in post-transplant recipients with Pseudomonas infections [7]. It is probable that improvement in these factors, development of sensitive microbiologic immunoassays and genomic and proteomic markers may provide the potential for individualized immunosuppression and prophylactic strategies [30, 31] in LDLT recipients, since there was a reported decrease in DDLT graft failures of 7.8% and 10.3% at 6 months and 1 year, respectively, but no appreciable change in LDLT graft failures in 2014 [32]. The suggested causes of this difference between DDLT and LDLT failures have been small numbers of LDLT performed between 2008 and 2014 and the consistent increase in the severity of liver disease [32]. These numbers could be increased by upgrading standards of care for LDLT recipients such as infection control along with a dynamic assessment of immune status.
Ei et al. further reported that the rate of bacterial infection is much lower in the early enteral nutrition (EEN) group than in the total parenteral nutrition (TPN) group in LDLT patients [33]. It might be plausible to improve EEN in LDLT recipients to reduce bacterial infections and hence increase LDLT survival. Bacterial infections in general and bacteraemia in particular have been reported to be the major causes of post-transplant mortality [34-37]. Our findings of LDLT having higher survival rates with bacterial infections than DDLT highlight the importance of timely treatment and effective empirical therapy for potential bacterial pathogens in LDLT. These patients if monitored closely and evaluated by expert clinicians could become the answer to the scarcity of DDLT donations.
Re-transplant outcomes in DDLT versus LDLT were similar to the overall group. DDLT patients had higher re-transplant free survival rates than LDLT (p = 0.0023). Re-transplant has been a controversial topic because of decreased survival [8]. Studies have indicated that re-transplant candidates do not disadvantage primary transplant candidates on the waitlists, yet do experience waitlist mortality [38]. This means that risks such as post-primary-transplant bacterial infections need to be explored further for better LDLT outcomes. Articles have previously explored other factors in re-transplant failures and postulated surgical complexities and missed optimal timings as causes of mortality [39].
Conclusions
LDLT patients seem to fare better with post-transplant bacterial infections than DDLT, and hence strict monitoring of these patients can help solve the problem of the scarcity of DDLT donors by improving outcomes in LDLT. Appropriate treatment of post-transplant bacterial infections could potentially increase the availability of transplant opportunities for patients facing this scarcity of organs.
Disclosure
Authors report no conflict of interest.
References
- 1.Antunes M, Teixeira A, Fortuna P, et al. Infections after liver transplantation: a retrospective, single-center study. Transplant Proc. 2015;47:1019–1024. doi: 10.1016/j.transproceed.2015.03.009. [DOI] [PubMed] [Google Scholar]
- 2.Steinberg JP, Del Rio C. Other gram-negative bacilli. In: Mandell GL, Bennet JE, Dolin R, editors. Mandell’s Principles and Practice of Infectious Diseases. 7 ed. Philadelphia: Elsevier; 2000. pp. 2459–2474. [Google Scholar]
- 3.Bonomo RA, Szabo D. Mechanisms of multidrug resistance in Acinetobacter species and Pseudomonas aeruginosa. Clin Infect Dis. 2006;43:S49–S56. doi: 10.1086/504477. [DOI] [PubMed] [Google Scholar]
- 4.Kawecki D, Chmura A, Pacholczyk M, et al. Bacterial infections in the early period after liver transplantation: etiological agents and their susceptibility. Med Sci Monit. 2009;15:628–637. [PubMed] [Google Scholar]
- 5.Fishman JA. Infection in solid-organ transplant recipients. N Engl J Med. 2007;20:2601–2614. doi: 10.1056/NEJMra064928. [DOI] [PubMed] [Google Scholar]
- 6.Hamandi B, Husain S, Grootendorst P, et al. Clinical and microbiological epidemiology of early and late infectious complications among solid-organ transplant recipients requiring hospitalization. Transpl Int. 2016;29:1029–1038. doi: 10.1111/tri.12808. [DOI] [PubMed] [Google Scholar]
- 7.Trevizol AP, David AI, Yamashita ET, et al. Intestinal and multivisceral retransplantation results: literature review. Transplant Proc. 2013;45:1133–1136. doi: 10.1016/j.transproceed.2013.03.007. [DOI] [PubMed] [Google Scholar]
- 8.Bittermann T, Shaked A, Goldberg DS. When living donor liver allografts fail: exploring the outcomes of retransplantation using deceased donors. Am J Transplant. 2017;17:1097–1102. doi: 10.1111/ajt.14037. [DOI] [PubMed] [Google Scholar]
- 9.Wachs ME, Bak TE, Karrer FM, et al. Adult living donor liver transplantation using a right hepatic lobe. Transplantation. 1998;66:1313–1316. doi: 10.1097/00007890-199811270-00008. [DOI] [PubMed] [Google Scholar]
- 10.Olthoff KM, Merion RM, Ghobrial RM, et al. A2ALL Study Group Outcomes of 385 adult-to-adult living donor liver transplant recipients: a report from the A2ALL Consortium. Ann Surg. 2005;242:314–325. doi: 10.1097/01.sla.0000179646.37145.ef. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Olthoff KM, Abecassis MM, Emond JC, et al. A2ALL Study Group Outcomes of adult living donor liver transplantation: comparison of the Adult-to-adult Living Donor Liver Transplantation Cohort Study and the national experience. Liver Transpl. 2011;17:789–797. doi: 10.1002/lt.22288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Adult Living Donor Liver Transplantation (A2ALL) Available at: https://www.niddkrepository.org/studies/a2all/Accessed on: February 10, 2017.
- 13.About the National Institute of Diabetes and Digestive and Kidney Diseases Available at: https://www.niddk.nih.gov/about-niddk/Pages/default.aspx. Accessed on: June 4, 2017.
- 14.Samstein B, Smith AR, Freise CE, et al. Complications and Their Resolution in Recipients of Deceased and Living Donor Liver Transplants: Findings From the A2ALL Cohort Study. Am J Transplant. 2016;16:594–602. doi: 10.1111/ajt.13479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Baker TB, Zimmerman MA, Goodrich NP, et al. Biliary Reconstructive techniques and associated anatomic variants in adult living donor liver transplants: The A2ALL experience. Liver Transpl. 2017;23:1519–1530. doi: 10.1002/lt.24872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Emond JC, Goodrich NP, Pomposelli JJ, et al. Hepatic Hemodynamics and Portal Flow Modulation: The A2ALL Experience. Transplantation. 2017;101:2375–2384. doi: 10.1097/TP.0000000000001823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Levitsky J, Goldberg D, Smith AR, et al. Acute Rejection Increases Risk of Graft Failure and Death in Recent Liver Transplant Recipients. Clin Gastroenterol Hepatol. 2017;15:584–593. doi: 10.1016/j.cgh.2016.07.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pomposelli JJ, Goodrich NP, Emond JC, et al. Patterns of Early Allograft Dysfunction in Adult Live Donor Liver Transplantation: The A2ALL Experience. Transplantation. 2016;100:1490–1499. doi: 10.1097/TP.0000000000001240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Olthoff KM, Emond JC, Shearon TH, et al. Liver regeneration after living donor transplantation: adult-to-adult living donor liver transplantation cohort study. Liver Transpl. 2015;21:79–88. doi: 10.1002/lt.23966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Freise CE, Gillespie BW, Koffron AJ, et al. A2ALL Study Group Recipient morbidity after living and deceased donor liver transplantation: findings from the A2ALL Retrospective Cohort Study. Am J Transplant. 2008;8:2569–2579. doi: 10.1111/j.1600-6143.2008.02440.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kim SI, Kim YJ, Jun YH, et al. Epidemiology and risk factors for bacteremia in 144 consecutive living-donor liver transplant recipients. Yonsei Med J. 2009;50:112–121. doi: 10.3349/ymj.2009.50.1.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hashimoto M, Sugawara Y, Tamura S, et al. Bloodstream infection after living donor liver transplantation. Scandinavian J Infect Dis. 2008;40:509–516. doi: 10.1080/00365540701824116. [DOI] [PubMed] [Google Scholar]
- 23.Bert F, Larroque B, Paugam Burtz C, et al. Microbial epidemiology and outcome of bloodstream infections in liver transplant recipients: an analysis of 259 episodes. Liver Transpl. 2010;16:393–401. doi: 10.1002/lt.21991. [DOI] [PubMed] [Google Scholar]
- 24.Shi SH, Kong HS, Xu J, et al. Multidrug resistant gram-negative bacilli as predominant bacteremic pathogens in liver transplant recipients. Transplant Infect Dis. 2009;11:405–412. doi: 10.1111/j.1399-3062.2009.00421.x. [DOI] [PubMed] [Google Scholar]
- 25.Pappas PG, Alexander BD, Andes DR, et al. Invasive fungal infections among organ transplant recipients: results of the Transplant-Associated Infection Surveillance Network (TRANSNET) Clin Infect Dis. 2010;50:1101–1111. doi: 10.1086/651262. [DOI] [PubMed] [Google Scholar]
- 26.Husain S, Tollemar J, Dominguez EA, et al. Changes in the spectrum and risk factors for invasive candidiasis in liver transplant recipients: prospective, multicenter, case-controlled study. Transplantation. 2003;75:2023–2029. doi: 10.1097/01.TP.0000065178.93741.72. [DOI] [PubMed] [Google Scholar]
- 27.Tu Z, Xiang P, Xu X, et al. DCD liver transplant infection: experience from a single centre in China. Int J Clin Pract. 2016;70(Suppl 185):3–10. doi: 10.1111/ijcp.12810. [DOI] [PubMed] [Google Scholar]
- 28.Oweira H, Lahdou I, Daniel V, et al. Early post-transplant neopterin associated with one year survival and bacteremia in liver transplant recipients. Hum Immunol. 2016;77:115–120. doi: 10.1016/j.humimm.2015.11.003. [DOI] [PubMed] [Google Scholar]
- 29.Trifan A, Stoica O, Stanciu C, et al. Clostridium difficile infection in patients with liver disease: a review. Eur J Clin Microbiol Infect Dis. 2015;34:2313–2324. doi: 10.1007/s10096-015-2501-z. [DOI] [PubMed] [Google Scholar]
- 30.Jenner RG, Young RA. Insights into host responses against pathogens from transcriptional profiling. Nat Rev Microbiol. 2005;3:281–294. doi: 10.1038/nrmicro1126. [DOI] [PubMed] [Google Scholar]
- 31.Wang D, Coscoy L, Zylberberg M, et al. Microarray-based detection and genotyping of viral pathogens. Proc Natl Acad Sci. 2002;99:15687–15692. doi: 10.1073/pnas.242579699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kim WR, Lake JR, Smith JM, et al. OPTN/SRTR 2015 Annual Data Report: Liver. Am J Transplant. 2017;17:174–251. doi: 10.1111/ajt.14126. [DOI] [PubMed] [Google Scholar]
- 33.Ei S, Shinoda M, Itano O, et al. Effects of Addition of Early Enteral Nutritional Support During the Postoperative Phase in Patients after Living-Donor Liver Transplantation. Ann Transplant. 2015;20:357–365. doi: 10.12659/AOT.893421. [DOI] [PubMed] [Google Scholar]
- 34.Patel G, Huprikar S. Infectious complications after orthotopic liver transplantation. Semin Respir Crit Care Med. 2012;33:111–124. doi: 10.1055/s-0032-1301739. [DOI] [PubMed] [Google Scholar]
- 35.Singh N, Paterson DL, Gayowski T, et al. Predicting bacteremia and bacteremic mortality in liver transplant recipients. Liver Transpl. 2000;6:54–61. doi: 10.1002/lt.500060112. [DOI] [PubMed] [Google Scholar]
- 36.Iida T, Kaido T, Yagi S, et al. Posttransplant bacteremia in adult living donor liver transplant recipients. Liver Transpl. 2010;16:1379–1385. doi: 10.1002/lt.22165. [DOI] [PubMed] [Google Scholar]
- 37.Ikegami T, Shirabe K, Matono R, et al. Etiologies, risk factors, and outcomes of bacterial pneumonia after living donor liver transplantation. Liver Transpl. 2012;18:1060–1068. doi: 10.1002/lt.23483. [DOI] [PubMed] [Google Scholar]
- 38.Kim HJ, Larson JJ, Lim YS, et al. Impact of MELD on waitlist outcome of retransplant candidates. Am J Transpl. 2010;10:2652–2657. doi: 10.1111/j.1600-6143.2010.03315.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hwang S, Ahn CS, Kim KH, et al. Liver retransplantation for adult recipients. Korean J Hepatobiliary Pancreat Surg. 2013;17:1–7. doi: 10.14701/kjhbps.2013.17.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]