Summary:
Breast reconstruction that leaves no visible scars on the breast is possible for a subset of patients. This article reviews a cohort of 10 patients who underwent 14 autologous breast reconstructions. To achieve a reconstruction without visible breast scars, the mastectomy and autologous reconstruction are carried out through a periareolar incision. At the completion of the reconstruction, a small skin paddle is externalized through the mastectomy incision and in a subsequent stage entirely incorporated into a nipple areola reconstruction. Following completion of the breast and nipple areola reconstruction, a tattoo is performed that extends beyond the perimeter of the reconstructed areola and conceals all scars on the breast mound. The ideal candidate for this technique has a small or medium size breast, which is non- or minimally ptotic, and a donor site that can yield a flap larger than the volume of the native breast. In properly selected patients, this technique consistently yields high-quality results, which match or even surpass the aesthetics of the original breast.
INTRODUCTION
Scarless surgery has been an elusive goal in plastic surgery, but for a subset of patients breast reconstruction without visible scars is possible (Figure 1).1,2 Any time a full-thickness incision is made through the skin, a scar will inevitably result, but in many patients the scars can be positioned and concealed to yield a breast mound without visible scars at the completion of the breast reconstruction.3–7
Fig. 1.
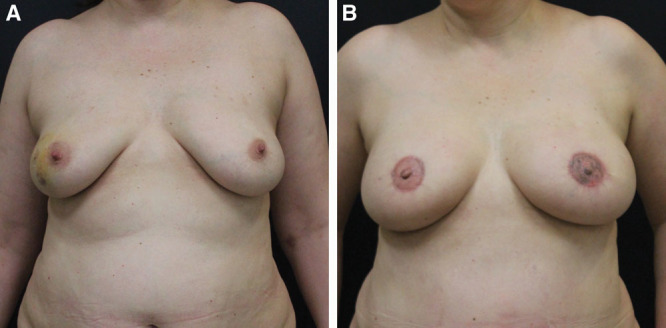
Pre- and postoperative patient photographs. A, Preoperative view of a patient who is indicated for a bilateral mastectomy. Breasts demonstrate minimal ptosis and moderate volume. The mastectomy weight in this case was 596 g on the left and 551 g on the right. B, Completed breast reconstruction following 2 surgical stages and nipple areola tattoo. The tattoo extends beyond the border of the areola resulting in no visible scars on the reconstructed breasts.
PATIENTS AND METHODS
This is review of 10 patients who underwent 14 autologous breast reconstructions by W.D. through a periareolar mastectomy incision between May 2016 and May 2017 (Table 1).
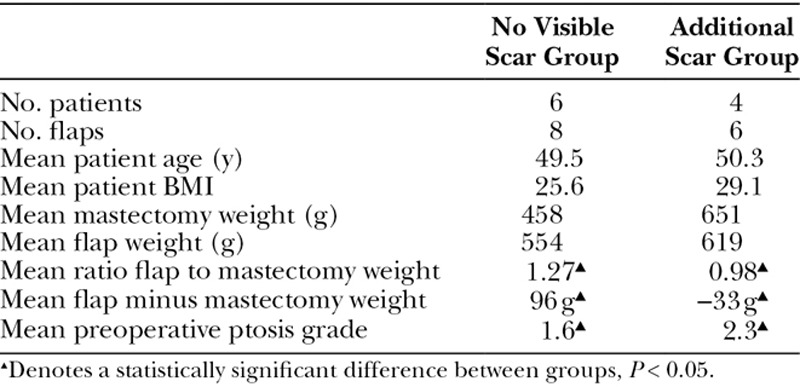
Table 1.
Breast Reconstruction Patient Data
All patients included in the study underwent a mastectomy through a circular incision, which encompassed the nipple, areola, and variable amounts of breast skin (Fig. 2A), and autologous breast reconstruction with deep inferior epigastric artery perforator (DIEP; n = 12), stacked DIEP (n = 1), or Profunda artery perforator (n = 1) flaps. In patients with a small areola, the incision was carried out as a concentric circle, which was marked beyond the border of the areola. In all cases, this resulted in an adequate opening through which the mastectomy, lymph node removal, recipient vessel dissection, microvascular anastomoses, flap placement, and inset were performed. The only step made more challenging by the small opening was the actual placement of the flap into the mastectomy pocket, which required additional retraction of the skin edges, continual visualization of the flap pedicle, and careful maneuvering.
Fig. 2.
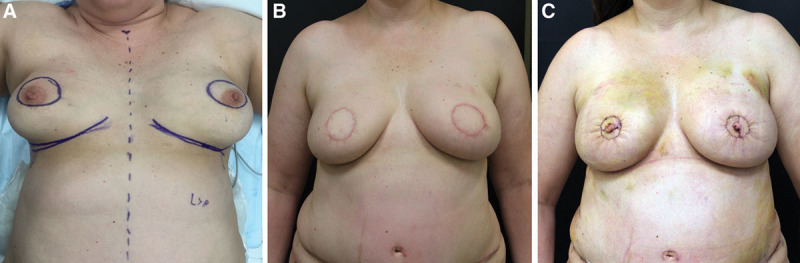
Preoperative and intermediate stage patient photographs. A, Preoperative view of a patient who is indicated for a bilateral mastectomy with markings for planned incisions. B, Following completion of the first stage of breast reconstruction with bilateral DIEP flaps. The flap weight in this case was 685 g on the left and 672 g on the right, which exceeds the mastectomy weights by approximately 100 g per breast. The mastectomy skin purse strings around a small skin paddle. C, Immediately following completion of breast reconstruction revision, fat grafting and nipple areola reconstruction. The mastectomy skin further purse strings around a 38 mm reconstructed areola. Mastectomy skin is initially pleated around the areola, which resolves over time.
Following completion of flap reperfusion, a 42-mm skin paddle was marked on the flap surface, and the remainder of the flap was deepithelialized. The mastectomy skin was then purse-stringed around this skin paddle (Fig. 2B). Second-stage revision surgery involved fat grafting, nipple reconstruction, and donor-site revisions. Nipple reconstruction was performed using the CV flap technique, and the skin paddle was further decreased to a 38-mm diameter (Fig. 2C). A nipple areola tattoo was performed, which overlapped the entire flap skin paddle and all scars resulting in a reconstruction without visible breast scars (Fig. 1B). A subgroup of patients required an adjustment of the mastectomy skin envelope necessitating the placement of an additional scar on the breast mount.
A two-tailed Student t test was used to compare data between patient who completed breast reconstruction without visible scars and those who required a second-stage revision resulting in an additional scar. A value of P < 0.05 was used to determine statistical significance.
RESULTS
Ten consecutively presenting patients who underwent 14 autologous breast reconstruction through a periareoral mastectomy incision were included in the study. In 8 of the 14 breast reconstructions (6 patients), no additional breast incisions were required to complete an aesthetic reconstruction. In 6 of the 14 breast reconstructions (4 patients), a decision was made to perform a second-stage revision that resulted in an additional vertical scar on the inferior midline of reconstructed breast, but produced a more aesthetic breast shape.
Mastectomy weight, flap weight, degree of ptosis, and BMI were recorded (Table 1). A statistically significant difference was observed when the ratio of flap weight to mastectomy weight, and the difference between flap weight and mastectomy weight was calculated for each breast. The mean ratio of flap weight to mastectomy weight was 1.27 (range, 0.88–1.52) in patients who successfully completed reconstruction without visible breast scars, and 0.98 (range, 0.82–1.1) in those who required a secondary surgery resulting in additional scars; this difference was statistically significant. The mean difference between the mastectomy weight and the weight of the flap that replaced it was 96 g (range, -64–150 g) in patients who successfully completed reconstruction without visible breast scars, and -32.5 g (range, -182–55 g) in those who required a secondary surgery resulting in additional scars; this difference was also statistically significant. All patients who successfully completed reconstruction without visible breast scars had either grade I or grade II ptosis (mean grade, 1.6), and the patients who required a secondary surgery resulting in additional scars had either grade II or grade III ptosis (mean grade, 2.3); this difference was statistically significant. The difference in BMI between groups was not statistically significant.
No flaps were lost; complications were limited to minor wound healing delay along incisions, which occurred in 4 patients and healed without intervention, and 1 breast hematoma that occurred on postoperative day 7 and required return to the operating room.
DISCUSSION
Patients who successfully completed reconstruction without visible breast scars on average had a flap that was 27% larger, or nearly 100 g more massive than the mastectomy tissue that it replaced. Additionally, they had either no ptosis or only a low degree of ptosis. The patients had a relatively low BMI, averaging 25.6, although reconstruction without visible breast scars was successfully completed in a patient with a BMI as high as 31.5. Although reconstruction without visible breast scars can be successfully performed in unilateral breast reconstruction cases, bilateral reconstruction will yield the greatest degree of symmetry. Whenever a DIEP or a Profunda Artery Perforator flap is utilized, a scar in the flap donor site is unavoidable.
Breast reconstruction with this technique is not compatible with nipple-sparing mastectomy. Patients who are candidates for nipple-sparing mastectomy must weigh the aesthetic benefits of having a natural nipple against the disadvantage of having a visible scar on the breast mound. An interesting subset of patients are those who require removal of the nipple and areola on 1 side but are candidates for nipple-sparing mastectomy on the contralateral side. In those cases, a greater aesthetic result may be achieved by planning a symmetric bilateral reconstruction without visible breast scars, at the cost of sacrificing a natural nipple areola on 1 side.
CONCLUSIONS
Breast reconstruction that leaves no visible scars on the breast is possible for a subset of patients. The ideal candidate has breasts that are non- or minimally ptotic, and a donor site that can yield a flap larger than or equal to the volume of the native breast. Preoperative factors such as a small breast size and low BMI did not yield statistical significance in predicting successful completion of a reconstruction without visible breast scars but make the operation technically easier to perform. Careful patient selection is essential to the success of a reconstruction without visible breast scars. The technique described consistently yields high-quality results, which match or even surpass the aesthetics of the original breast.
Footnotes
Disclosure: The author has no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.Ho OA, Lin YL, Huang JJ, et al. Contralateral augmentation with a transmidline scarless technique during unilateral breast reconstruction using implants. Plast Reconstr Surg Glob Open. 2017;5:e1298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Huang JJ, Chao LF, Wu CW, et al. Simultaneous scarless contralateral breast augmentation during unilateral breast reconstruction using bilateral differentially split DIEP flaps. Plast Reconstr Surg. 2011;128:593e–604e.. [DOI] [PubMed] [Google Scholar]
- 3.de Runz A, Boccara D, Bekara F, et al. Outcome of 122 delayed breast reconstruction following post-mastectomy radiotherapy: the scarless latissimus dorsi flap with tissue expansion technique. Ann Chir Plast Esthet. 2017;62:23–30.. [DOI] [PubMed] [Google Scholar]
- 4.Lee MA, Miteff KG. The scarless latissimus dorsi flap provides effective lower pole prosthetic coverage in breast reconstruction. Plast Reconstr Surg Glob Open. 2014;2:e147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Elliott LF, Ghazi BH, Otterburn DM. The scarless latissimus dorsi flap for full muscle coverage in device-based immediate breast reconstruction: an autologous alternative to acellular dermal matrix. Plast Reconstr Surg. 2011;128:71–79.. [DOI] [PubMed] [Google Scholar]
- 6.Cahan AC, Palaia DA, Rosenberg M, et al. The aesthetic mastectomy utilizing a non-nipple-sparing portal approach. Ann Plast Surg. 2011;66:424–428.. [DOI] [PubMed] [Google Scholar]
- 7.Hidalgo DA. Aesthetic refinement in breast reconstruction: complete skin-sparing mastectomy with autogenous tissue transfer. Plast Reconstr Surg. 1998;102:63–70.; discussion 71. [DOI] [PubMed] [Google Scholar]


