Supplemental Digital Content is available in the text.
Abstract
Background:
Although the use of acellular dermal matrices (ADMs) in implant-based reconstruction increases, there is a lack of studies evaluating patient-reported outcome measures after this reconstruction method. We aim to evaluate the patient satisfaction after ADM-assisted implant-based breast reconstruction (IBBR) in 1 of the largest series of patients undergoing ADM-assisted IBBR.
Methods:
Patients with ADM-assisted IBBR were invited to fill out the BREAST-Q, a validated and standardized questionnaire to measure patient satisfaction after a breast reconstruction. A retrospective chart review was performed to identify patient and surgical characteristics.
Results:
In total, 208 patients (38.4%) responded and reported a mean satisfaction of 70.6 ± 20.2 with their breasts and 78.0 ± 20.5 with the outcome. An overall complication rate of 7.7% was noted, with 1.5% severe complications leading to hospital readmission (0.5%) and implant removal (0.5%). Patients with complications and unilateral reconstruction for oncological reasons reported overall less satisfaction rates compared with patients with bilateral, preventive surgery, and an uncomplicated postoperative course. Strongly related domains indicate the importance of patient satisfaction with their breasts and outcome on psychosocial and sexual functioning and satisfaction with information on satisfaction with breasts, outcome, and surgeon.
Conclusion:
There is an increased demand for patient-reported outcome measures in a changing practice to which the opinion of the patient assumes a larger role. With high satisfaction rates, ADM-assisted IBBR is a valuable reconstruction method, provided that complication rates remain low. Hence, it should only be performed in a selected group of women.
INTRODUCTION
In high-income countries, survival rates of breast cancer patients have increased to 80% or higher.1 Because incidence rates of breast cancer, especially in Western countries, are high and still rising, the number of breast cancer survivors is increasing rapidly. For this reason, focus of health care has shifted toward quality of life after cancer treatment. In most cases, breast surgery is required as part of cancer treatment, which entails either breast-conserving surgery or mastectomy. In women with an established high risk of breast cancer, mastectomy may also be performed prophylactically. In Western society, breast reconstruction has become an integral part of breast cancer treatment options. Breast reconstruction aims to approximate the “natural breast” as closely as possible with the ultimate goal to ameliorate the patients’ quality of life.2
There are multiple techniques for breast reconstruction, of which implant-based breast reconstruction (IBBR) is the most performed reconstruction method.3 In recent years, acellular dermal matrices (ADMs) are increasingly being used in IBBR to augment the subpectoral pocket and to allow immediate implantation of an implant or tissue expander.4 Supposed additional advantages are a better cosmetic outcome,4,5 and, in the long term, possible a reduced capsular contraction rate.6
Data regarding the safety of ADM use in IBBR vary widely, with complication rates ranging from below 5% to more than 50%.4,7–9 Recent results indicate that expertise with both the technique and the careful selection of eligible patients are important factors for optimal clinical outcomes.9,10 However, to assess to what extent the eventual goal of breast reconstructive surgery is reached, that is, to enhance the quality of life, measurement of patient-reported outcomes (PROs) is essential. Therefore, we aim to assess the satisfaction and quality of life of women who underwent ADM-assisted IBBR.
Previously, Salzberg et al.6,11 reported on the clinical outcomes in 1 of the largest series of patients treated with ADM-assisted breast reconstruction. The overall complication rate was 8.6%, and the cumulative incidence of capsular contraction was low (0.8%).8 In this study, we have evaluated the PROs of these women using the BREAST-Q, which is a validated tool developed specifically to assess satisfaction and quality of life after breast surgery.12
METHODS
Patients
All patients who underwent implant-based breast reconstruction (IBBR) in the senior surgeons practice between September 1988 and January 2016 were invited via e-mail to participate in the study. Patients’ follow-up consisted of an appointment every 3 months during the first year and then annually or if needed.
We undertook the study in accordance with the Declaration of Helsinki, guidelines for Good Clinical Practice and in accordance with the STROBE statement.13
Surgical Technique
The surgical technique has been reported previously.8,14,15 Briefly, a retropectoral pocket was created, extending from the lateral border of the pectoralis major muscle to the second rib superiorly, to the sternum medially, and to the level of the contralateral inframammary fold inferiorly. After placement of the implant into the retropectoral pocket, the ADM was placed to provide implant coverage and protection by extending the pectoralis muscle over the inferior third of the implant. The ADM is sutured to the chest wall, the lateral mammary fold, the serratus fascia and to the inferior border of the pectoralis major muscle. Two suction drains are then placed retropectoral and in the subcutaneous space.
Outcomes
A retrospective chart review was performed to identify baseline characteristics including age, indication, final pathology, type of surgery, side of reconstruction, radiotherapy, complications, and interventions.
Patients were invited per e-mail to fill out the BREAST-Q reconstruction module.12 Patients who did not respond were sent a reminder up to 2 times.
The BREAST-Q reconstruction module is a validated and standardized questionnaire for evaluating the results after mastectomy and subsequent breast reconstruction. It contains 14 domains regarding satisfaction with breasts (Q1), visibility (Q2a) and sensation of rippling (Q2b), satisfaction with outcome (Q3), psychosocial well-being (Q4), sexual well-being (Q5), physical well-being: chest and upper body (Q6), physical well-being with abdomen and trunk (Q7), and satisfaction with abdomen (Q8, Q9), satisfaction with nipples (Q10), satisfaction with care regarding information (Q11), surgeon (Q12), the medical team (Q13), and office staff (Q14).
The domains Q7–Q10 are not applicable to this population, because only patients who underwent IBBR were included in this study.
Statistical Analyses
The QScore Scoring Software was used to convert the BREAST-Q scores ranging from 1 through 4 or 5 to a total score ranging from 0 to 100. A higher Q-Score indicates a higher patient satisfaction. Only scores of domains Q2a and Q2b are not converted; these scores range from 1 (very dissatisfied) to 4 (very satisfied).16
Differences between responding and nonresponding patients were assessed regarding age, follow-up, reason for surgery and side (prophylactic, therapeutic uni of bilateral), type of surgery, and complications with Student’s t test and chi-square tests. The correlation between the different domains of the BREAST-Q was assessed with a Spearman’s rho test. A univariate analysis was performed to assess differences in satisfaction related to age, follow-up, reason for surgery, type of surgery, and complications. For the univariate analyses, the continue variables age and follow-up time were dichotomized. The domain satisfaction with breasts (Q1), satisfaction with outcome (Q3), psychosocial well-being (Q4), physical well-being: chest and upper body (Q6), satisfaction with nipples (Q10), and satisfaction with care regarding information (Q11) were taken into account.
A multivariate analysis was performed on Q-scores that are related to at least 1 variable. Age and follow-up were used as continue variables in the multivariate model. Reason and side of surgery were defined as 1 variable, as most patients (95.2%) undergoing prophylactic surgery received a bilateral reconstruction. Age and follow-up were used as continuous variables in the multivariate model.
For the analyses, IBM SPSS statistics version 22 was used (IBM Corp. Released 2013. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp).
RESULTS
Response Rate
We invited 541 women to participate in the study (Fig. 1). The survey was returned by 208 patients (38.4%), of which 181 women filled out the survey completely and 27 women partially. All patients filled out the BREAST-Q 1 Satisfaction with breasts domain. The number of completed questionnaires for each domain are listed in Table 3.
Fig. 1.
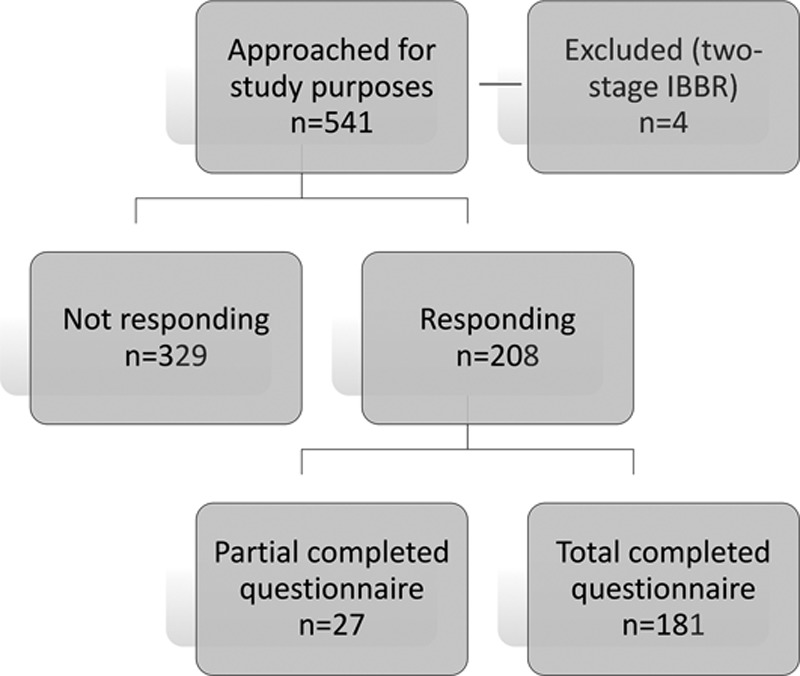
Inclusion of patients.
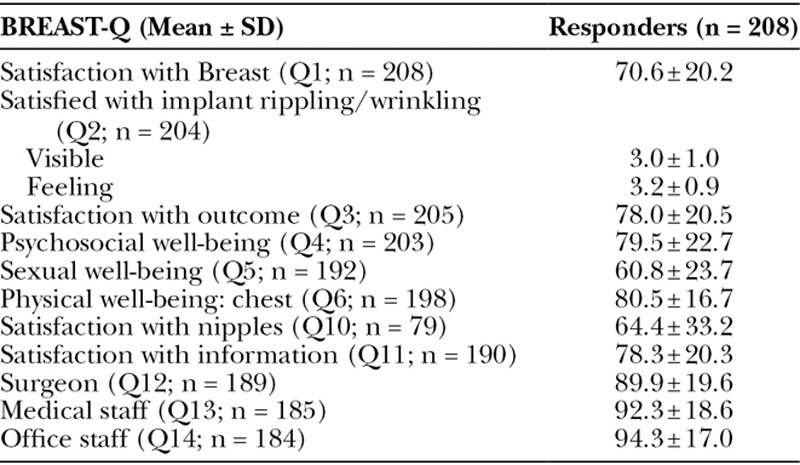
Table 3.
Details of Patients’ Responses on BREAST-Q
There were no statistical differences between women who did or did not respond regarding age, follow-up, reason for surgery, type of surgery, follow-up, and complications. There was a difference in type of reconstruction between responders and nonresponders; all responders underwent IBBR with an additional ADM, whereas 6.4% (n = 18) of the nonresponders received a reconstruction with an implant only (P = 0.008; Table 1).
Table 1.
Baseline Characteristics of Nonresponders, Responders, and All Patients (n = 541)
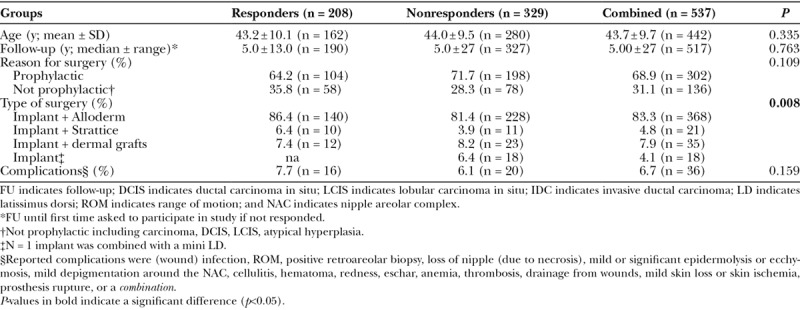
In 3 patients in the nonresponding group and 1 patient in the responding group, first expanders were placed and later replaced with definitive implants. These patients were excluded from the analyses.
Characteristics of Responding Patients (n = 208)
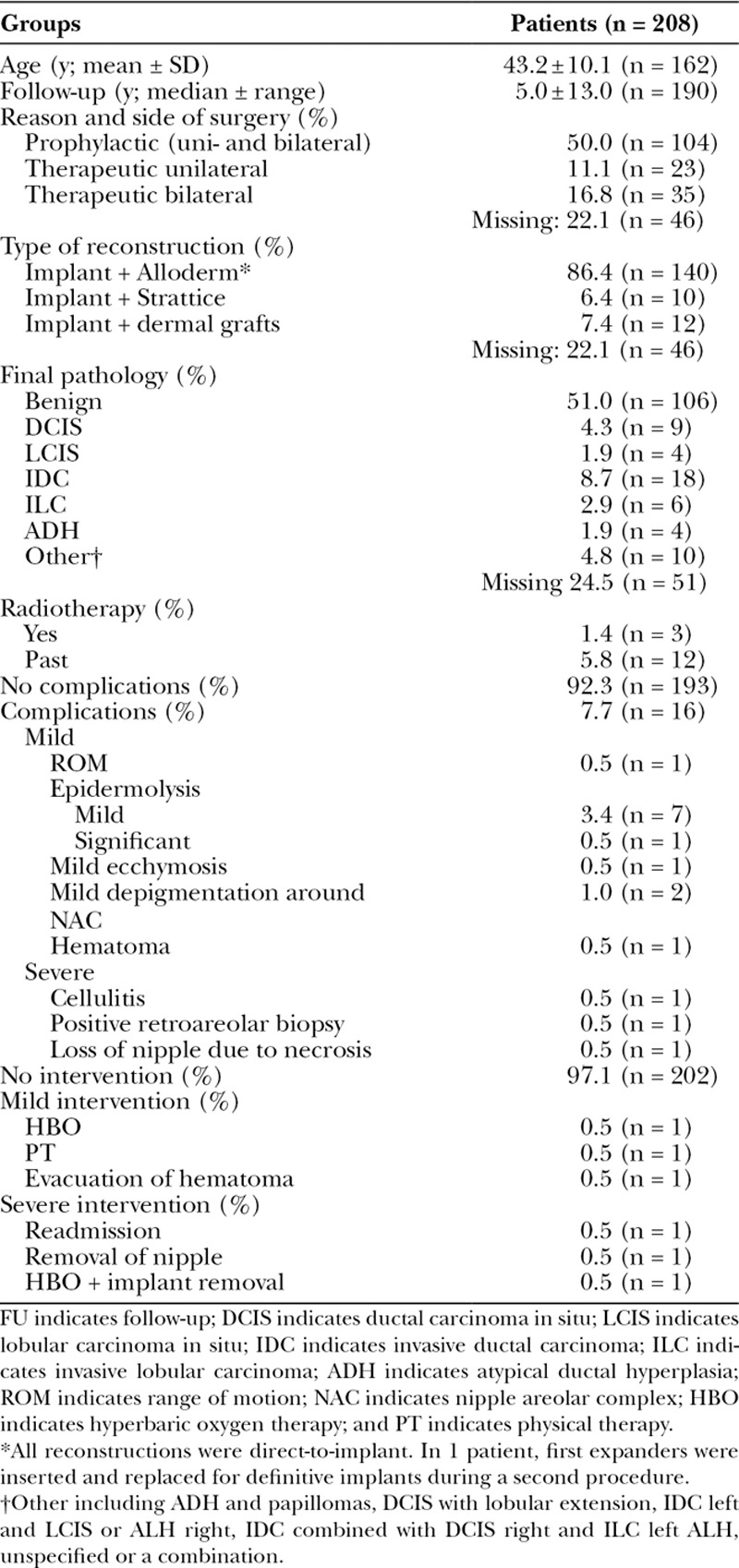
Patients were operated on between June 21, 2002, and January 7, 2016. The mean age was 43.2 (±10.1) years with a median follow-up of 5.0 (± 13.0) years. No patients were active smokers at the time of surgery. Reasons for surgery were prophylactic in 50.0% and comprised of reconstruction with an implant, mainly combined with ADM (Alloderm; 86.4%). All reconstructions were performed in 1 stage. An overall complication rate of 7.7% was noted, of which 1.5% were severe complications including cellulitis (0.5%), positive retroareolar biopsy (0.5%), and loss of nipple due to necrosis (0.5%).8,11 This led to hospital readmission (0.5%), removal of nipple (0.5%), or implant removal (0.5%; Table 2).
Table 2.
Baseline Characteristics of Included Patients (n = 209)
Patient-reported Outcomes Measured with the BREAST-Q
The mean satisfaction with breast and outcome measured with the BREAST-Q was 70.6 ± 20.2 and 78.0 ± 20.5, respectively. On psychosocial well-being, an average score of 79.5 ± 22.7 was reported, on sexual well-being 60.8 ± 23.7, and on physical well-being with chest 80.5 ± 16.7. Satisfaction with nipples was moderate, with a mean score of 64.4 ± 33.2.
Patients were in general satisfied with the information (mean score, 78.3 ± 20.3), their surgeon (89.9 ± 19.6), medical staff (92.3 ± 18.6), and office staff (94.3 ± 17.0; Table 3).
Correlation BREAST-Q Domains
Psychosocial well-being (Q4) and sexual well-being (Q5) were related strongly (r = 0.752, P < 0.001). Satisfaction with breasts (Q1) showed strong relationships (r ≥ 0.704) with satisfaction with outcome (Q3), psychosocial well-being (Q4), and sexual well-being (Q5; P < 0.001). Also, visibility (Q2a) and sensation (Q2b) of rippling (r = 0.733) and satisfaction with outcome (Q3) and psychosocial well-being (Q4) were correlated (r = 0.687; P < 0.001). At length, satisfaction with care regarding information (Q11) was correlated to satisfaction with breasts (Q1, r = 0.652), satisfaction with outcome (Q3, r = 0.668), and satisfaction with the surgeon (Q12, r = 0.654; see table, Supplemental Digital Content 1, which displays Spearman’s correlation between BREAST-Q modules, http://links.lww.com/PRSGO/A676).
Influence of Age, Complications, Reason for Surgery, and Side of Reconstruction
In the univariate model, younger patients were more satisfied with the outcome (Q3 mean, 81.5 ± 18.5) and with the information of care provided (Q11, 82.2 ± 16.9) compared with older patients (Q3, 73.0 ± 21.9, P = 0.001; Q11, 74.5 ± 22.5, P = 0.010). A shorter follow-up resulted in a lower physical well-being (Q6, 76.1 ± 17.2, P = 0.001).
Patients with a mastectomy for therapeutical reasons and a unilateral reconstruction were in general less satisfied with the outcome (Q3, 69.5 ± 21.4, P = 0.045), psychosocial well-being (Q4, 70.0 ± 24.3, P = 0.027) and with their nipples (Q10, 44.9 ± 27.0, P = 0.011). At length, patients with a complication were significantly less satisfied with the outcome (Q3 mean, 62.6 ± 22.0), their psychosocial well-being (Q4 mean, 68.7 ± 27.5), and with the information provided (Q11 mean, 66.4 ± 25.8) compared with patients with an uncomplicated course [Q3 men, 79.3 ± 19.9, P = 0.002; Q4 mean, 80.5 ± 21.0, P = 0.037; Q11 mean, 79.2 ± 19.4, P = 0.027; see table, Supplemental Digital Content 2, which displays influence of age, follow-up, reason for surgery and side of reconstruction, and complications on PROs (univariate model), http://links.lww.com/PRSGO/A677].
In the multivariate model, patients with a shorter follow-up (< 5 years) reported less physical well-being [Q6, 7.6 (2.1, 13.1) P = 0.007]. Patients with a mastectomy for therapeutical reasons and a unilateral reconstruction were less satisfied with their psychosocial well-being [Q4, -12.7 (-22.7 to 2.6) P = 0.014] and their nipples [Q10, -26.2 (-45.6, -6.9) P = 0.009] compared with patients undergoing a preventive mastectomy. Patients with a complication reported less satisfaction with the outcome [Q3, -14.2 (24.8, -3.6) P = 0.009] and with the information provided [Q11, -12.1 (-23.7, -0.6) P = 0.040; see table, Supplemental Digital Content 3, which displays the influence of age, follow-up, reason for surgery and side of reconstruction, and complications on PROs (multivariate model), http://links.lww.com/PRSGO/A678).
DISCUSSION
In this study, we assessed PROs in women who underwent ADM-assisted IBBR. In general, women were satisfied with the result of their breast reconstruction, with a satisfaction ranging from 60.8 ± 23.7 to 94.3 ± 17.0 in the various domains. Satisfaction was negatively influenced by the occurrence of a complication. Patients who were treated prophylactically and underwent bilateral reconstruction were most satisfied with the results.
Recently, normative baseline values for the BREAST-Q were obtained by Mundy et al.17 by inviting the Army of Women to fill out the different preoperative BREAST-Q’s. As no preoperative questionnaires were filled out in our study, it is most appropriate to compare our data with their results. Women in the present study are more satisfied with their breasts (mean difference, 12.6 ± 1.5, P < 0.001), and score higher on psychosocial well-being (8.5 ± 1.7, P < 0.001) and sexual well-being (4.8 ± 1.8, P = 0.01). The normative values for physical well-being are higher in the cohort by Mundy et al.17 (-12.5 ± 1.2, P < 0.001).
Previous studies reported high satisfaction rates after direct-to-implant ADM-assisted breast reconstruction in 2 articles concerning 118 and 63 patients using the BREAST-Q.18,19 However, the actual numbers cannot be compared with our data, because they did not use the scoring conversion method as provided by the developers of the questionnaire.18,19 In general, it has been found that autologous breast reconstruction leads to a higher satisfaction rates compared with other reconstructions methods.17,20–22 Pusic et al.22 conducted a large Mastectomy Reconstruction Outcomes Consortium study, a 5-year, prospective, multicenter study including 1,632 patients to compare satisfaction and quality of life 1 year after immediate reconstruction within and between autologous and IBBR. Only patients with breast cancer diagnosis were included, which hampers legitimate comparison with our results.22 To our knowledge, no meta-analysis of the current literature is yet available comparing the PROs after different reconstruction methods, which is necessary to properly compare outcomes and draw any conclusions.
Of course, satisfaction is affected by more factors than the reconstruction method. Immediate reconstruction after a mastectomy for cancer treatment is a known risk factor for lower overall patient satisfaction, compared with risk-reducing treatment.23 Because prophylactic treatment is usually bilateral, while therapeutic treatment can be both, the separate effect of these factors (therapeutic/prophylactic and bi/unilateral treatment) cannot easily be distinguished. As almost half of the patients (49.8%) underwent a prophylactic mastectomy, this contributes to the high satisfaction rate reported in this study.
In this study, satisfaction was lower in patients who underwent unilateral therapeutic treatment. It is recommendable to discuss a preventive contralateral mastectomy with patients scheduled for a unilateral mastectomy.
The occurrence of complications can negatively influence a patients’ satisfaction,20 which was confirmed by our findings. In this cohort, the overall complication rate was low (7.7%). All patients in this cohort were nonsmokers, and the majority of patients received a prophylactic mastectomy, which may contribute to the low complication rate. Furthermore, the operating surgeon is highly experienced with ADM-assisted IBBR, which also contributes to a lower complication rate.10,24 Previous studies, however, have shown a high variance in complication rate with this technique, ranging from only 5% up till 50%.4,7–9 It can be expected that patient-reported satisfaction rates vary analogously; however, this has not been clearly established.
The domains satisfaction with breasts, satisfaction with outcome, psychosocial well-being, and sexual well-being are most strongly interrelated (r ≥ 0.665, P < 0.001). This underscores the importance of a womens’ breast for her psychosocial and sexual functioning. Furthermore, satisfaction with information is strongly correlated to satisfaction with breasts, outcome, and the surgeon, which indicates the importance of adequate information.
There are several questionnaires available to evaluate patient-reported outcome measures (PROMs), but they are mainly self-made and not validated.25 The BREAST-Q is a questionnaire validated to measure PROs after breast surgery.12 There are 5 separate modules available, and the postmastectomy reconstruction module is increasingly used in studies reporting on breast reconstructive surgery.26 PROMs are necessary to improve health care and are important to avoid observer bias.26,27 Although more studies focus on PROMs, they are not integrated in most health care systems. As stated by Black27, PROMs should become part of daily care. It is important that at least future studies will take PROMs into account, and preferably all use the same questionnaire. Only with comparable outcomes, we will be able to compare the results of future studies with each other.26
Limitations
This study is limited by its retrospective design and consequently contains missing data. No preoperative questionnaires were administered; therefore, the difference in patient satisfaction before and after the surgery could not be assessed. In this study, 208 patients (38.4%) responded to the invitation, and only the more recently treated patients responded. Although the groups were comparable regarding most baseline characteristics, there still might have been a bias regarding the patients who did or did not respond. This also concerns the type of reconstruction, because all patients receiving an implant only did not respond to the questionnaire. Dissatisfaction might be 1 of the reasons that the patients did not respond to the survey, and this can diminish the validity of the data. In this cohort, 1 patient in the responding group and 3 patients in the nonresponding group received 2-stage IBBR. It is inherent in the reconstruction process that in selected cases an expander should be placed first, due to the worries about the mastectomy skin flap quality. To maintain clarity, these patients were excluded in the study.
At length, there are others factors that might affect the patient satisfaction and could not be assessed in this study due to missing data. These factors include implant size and whether the mastectomy was nipple sparing or not. Future studies could focus on these factors.
CONCLUSIONS
This is 1 of the first studies of a large cohort evaluating patient satisfaction after ADM-assisted IBBR reporting with long-term follow-up. This procedure is associated with comparable or even higher satisfaction rates compared with other reconstruction methods. ADM-assisted IBBR is a valuable option for breast reconstruction, provided that complication rates remain low. Hence, it should only be selected and performed in a group of women who meet the criteria for the procedure.
Supplementary Material
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
Supplemental digital content is available for this article. Clickable URL citations appear in the text.
REFERENCES
- 1.Ginsburg O, Bray F, Coleman MP, et al. The global burden of women’s cancers: a grand challenge in global health. Lancet. 2017;389:847–860.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.D’Souza N, Darmanin G, Fedorowicz Z. Immediate versus delayed reconstruction following surgery for breast cancer. Cochrane Database Syst Rev. 2011;CD008674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.American Society of Plastic Surgeons. Plastic surgery statistics report 2016. Available at http://www.PlasticSurgery.org. Accessed August 18, 2017.
- 4.Potter S, Browning D, Savović J, et al. Systematic review and critical appraisal of the impact of acellular dermal matrix use on the outcomes of implant-based breast reconstruction. Br J Surg. 2015;102:1010–1025.. [DOI] [PubMed] [Google Scholar]
- 5.Macadam SA, Lennox PA. Acellular dermal matrices: use in reconstructive and aesthetic breast surgery. Can J Plast Surg. 2012;20:75–89.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Salzberg CA, Ashikari AY, Berry C, et al. Acellular dermal matrix-assisted direct-to-implant breast reconstruction and capsular contracture: a 13-year experience. Plast Reconstr Surg. 2016;138:329–337.. [DOI] [PubMed] [Google Scholar]
- 7.Kim SY, Bang SI. Impact of acellular dermal matrix (ADM) use under mastectomy flap necrosis on perioperative outcomes of prosthetic breast reconstruction. Aesthetic Plast Surg. 2017;41:275–281.. [DOI] [PubMed] [Google Scholar]
- 8.Hunsicker LM, Ashikari AY, Berry C, et al. Short-term complications associated with acellular dermal matrix-assisted direct-to-implant breast reconstruction. Ann Plast Surg. 2017;78:35–40.. [DOI] [PubMed] [Google Scholar]
- 9.Dikmans RE, Negenborn VL, Bouman MB, et al. Two-stage implant-based breast reconstruction compared with immediate one-stage implant-based breast reconstruction augmented with an acellular dermal matrix: an open-label, phase 4, multicentre, randomised, controlled trial. Lancet Oncol. 2017;18:251–258.. [DOI] [PubMed] [Google Scholar]
- 10.Mullender MG, Dikmans REG, Negenborn VL, et al. Results from the BRIOS randomised trial—authors’ reply. Lancet Oncol. 2017;18:e191. [DOI] [PubMed] [Google Scholar]
- 11.Salzberg CA, Dunavant C, Nocera N. Immediate breast reconstruction using porcine acellular dermal matrix (Strattice™): long-term outcomes and complications. J Plast Reconstr Aesthet Surg. 2013;66:323–328.. [DOI] [PubMed] [Google Scholar]
- 12.Pusic AL, Klassen AF, Scott AM, et al. Development of a new patient-reported outcome measure for breast surgery: the BREAST-Q. Plast Reconstr Surg. 2009;124:345–353.. [DOI] [PubMed] [Google Scholar]
- 13.von Elm E, Altman DG, Egger M, et al. ; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370:1453–1457.. [DOI] [PubMed] [Google Scholar]
- 14.Salzberg CA, Ashikari AY, Koch RM, et al. An 8-year experience of direct-to-implant immediate breast reconstruction using human acellular dermal matrix (AlloDerm). Plast Reconstr Surg. 2011;127:514–524.. [DOI] [PubMed] [Google Scholar]
- 15.Salzberg CA. Nonexpansive immediate breast reconstruction using human acellular tissue matrix graft (AlloDerm). Ann Plast Surg. 2006;57:1–5.. [DOI] [PubMed] [Google Scholar]
- 16.DiLaura A, Stefan C, Pusic AL. QScore scoring software. Available at https://webcore.mskcc.org/breastq/scoring.html. Accessed March 14, 2017.
- 17.Mundy LR, Homa K, Klassen AF, et al. Breast cancer and reconstruction: normative data for interpreting the BREAST-Q. Plast Reconstr Surg. 2017;139:1046e–1055e.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Headon H, Kasem A, Manson A, et al. Clinical outcome and patient satisfaction with the use of bovine-derived acellular dermal matrix (SurgiMend™) in implant based immediate reconstruction following skin sparing mastectomy: a prospective observational study in a single centre. Surg Oncol. 2016;25:104–110.. [DOI] [PubMed] [Google Scholar]
- 19.El Hage Chehade H, Headon H, Wazir U, et al. Nipple-sparing mastectomy using a hemi-periareolar incision with or without minimal medial-lateral extensions; clinical outcome and patient satisfaction: a single centre prospective observational study. Am J Surg. 2017;213:1116–1124.. [DOI] [PubMed] [Google Scholar]
- 20.Liu C, Zhuang Y, Momeni A, et al. Quality of life and patient satisfaction after microsurgical abdominal flap versus staged expander/implant breast reconstruction: a critical study of unilateral immediate breast reconstruction using patient-reported outcomes instrument BREAST-Q. Breast Cancer Res Treat. 2014;146:117–126.. [DOI] [PubMed] [Google Scholar]
- 21.Cohen WA, Mundy LR, Ballard TN, et al. The BREAST-Q in surgical research: a review of the literature 2009-2015. J Plast Reconstr Aesthet Surg. 2016;69:149–162.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pusic AL, Matros E, Fine N, et al. Patient-reported outcomes 1 year after immediate breast reconstruction: results of the mastectomy reconstruction outcomes consortium study. J Clin Oncol. 2017;35:2499–2506.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Howard MA, Sisco M, Yao K, et al. Patient satisfaction with nipple-sparing mastectomy: a prospective study of patient reported outcomes using the BREAST-Q. J Surg Oncol. 2016;114:416–422.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Colwell AS, Damjanovic B, Zahedi B, et al. Retrospective review of 331 consecutive immediate single-stage implant reconstructions with acellular dermal matrix: indications, complications, trends, and costs. Plast Reconstr Surg. 2011;128:1170–1178.. [DOI] [PubMed] [Google Scholar]
- 25.Pusic AL, Chen CM, Cano S, et al. Measuring quality of life in cosmetic and reconstructive breast surgery: a systematic review of patient-reported outcomes instruments. Plast Reconstr Surg. 2007;120:823–837.; discussion 838. [DOI] [PubMed] [Google Scholar]
- 26.Javid SH, Lawrence SO, Lavallee DC. Prioritizing patient-reported outcomes in breast cancer surgery quality improvement. Breast J. 2017;23:127–137.. [DOI] [PubMed] [Google Scholar]
- 27.Black N. Patient reported outcome measures could help transform healthcare. BMJ. 2013;346:f167. [DOI] [PubMed] [Google Scholar]


