Abstract
Colorectal cancer (CRC) is the third leading cause of cancer-associated mortality, and is a major health problem. Collagen type I α 1 (COL1A1) is a major component of collagen type I. Recently, it was reported to be overexpressed in a variety of tumor tissues and cells. However, the function of COL1A1 in CRC remains unclear. Herein, the present study demonstrated that COL1A1 was upregulated in CRC tissues and the paired lymph node tissues. Transwell assays showed that COL1A1 promoted CRC cell migration in vitro. Moreover, it was revealed that COL1A1 levels were correlated with those of WNT/planar cell polarity (PCP) signaling pathway genes; inhibition of COL1A1 decreased the expression levels of Ras-related C3 botulinum toxin substrate 1-GTP, phosphorylated-c-Jun N-terminal kinase, and RhoA-GTP, all of which are key genes in the WNT/PCP signaling pathway. These results may indicate the mechanisms underlying the oncogenic role of COL1A1 in CRC. In summary, the present data indicated that COL1A1 may serve as an oncoprotein, and that it may be used as a potential therapeutic target in CRC.
Keywords: colorectal cancer, COL1A1, WNT/PCP pathway, metastasis, bioinformatics analysis
Introduction
Colorectal cancer (CRC) is a common malignant tumor of the digestive system (1). In recent years, with changes in lifestyle and dietary structure, the incidence of CRC has increased annually. The symptoms of CRC are typically not obvious at the early stages, and tumors often have metastasized by the time the symptoms become noticeable. This is the main reason for the high mortality rate. Therefore, it is imperative to identify novel diagnostic markers, and to investigate the underlying mechanisms of metastasis in CRC.
Collagen type I α 1 (COL1A1) encodes the pro-α 1 chains of type I collagen, which has a triple helix composed of two α 1 chains and one α 2 chain (2). COL1A1 contains three conservative domains, namely a von Willebrand factor type C (vWFC) domain, a collagen triple-helix repeat and a fibrillar collagen C-terminal domain (COLF) (3). It was recently found that COL1A1 is associated with a variety of tumor types, and that the expression of COL1A1 was high in tumor tissues and cells (4–14). However, the function and mechanism of COL1A1 in CRC have not yet been reported. Therefore, in this study we aimed to detect the expression of COL1A1 in trios of tumor, normal and lymph node tissue samples, as well as to analyze the function and molecular mechanism of COL1A1 in the metastasis of CRC.
Materials and methods
Tissue microarrays and cell lines
Tissue chips, including 20 cases and 60 points, were purchased from Outdo Biotech (Shanghai, China). A total of 20 trios of CRC, adjacent normal, and lymph node tissues were included in the tissue microarrays. The CRC SW480 and SW620 cell lines used in this study were obtained from the ATCC and cultured in RPMI-1640 (HyClone; GE Healthcare Life Sciences, Logan, UT, USA) supplemented with 10% fetal bovine serum (FBS; Gibco; Thermo Fisher Scientific, Inc., Waltham, MA, USA) at 37°C and 5% CO2.
Immunohistochemistry (IHC)
The tissue microarrays were immunostained for COL1A1 as previously described (15). An antibody against COL1A1 was purchased from Abclone (Cambridge, MA, USA). The COL1A1 immunostaining score was calculated according to the percentage of positively stained tumor cells and the staining intensity. The percentage positivity was scored from 0 to 3, with 0 for <10%, 1 for 10–30%, 2 for 31–50%, and 3 for >50%. The staining intensity was scored from 0 to 3, with 0 for no staining, 1 for weakly stained, 2 for moderately stained, and 3 for strongly stained. Both the percentage positivity and the staining intensity were scored in a double-blinded manner. The total score for COL1A1 expression was calculated as the percentage positivity score × the staining intensity score, giving a value ranging from 0 to 9. COL1A1 expression was defined as either ‘low’ (score 0–4) or ‘high’ (score 5–9) (16).
Construction of COL1A1-knockdown cell lines and transfection
The siRNA used to inhibit COL1A1 expression was purchased from GenePharma (Shanghai, China). The nucleotide sequence of the siRNA against COL1A1 was TTGGTGTTGTGCGATGACGTG. Cells were transfected with siRNA oligonucleotides and plasmids using Lipofectamine® 2000 (Invitrogen Thermo Fisher Scientific, Inc.).
RNA extraction and reverse transcription-quantitative PCR (RT-qPCR)
Total RNA was extracted from tissues or cells using TRIzol® reagent (Takara Biotechnology Co., Ltd., Dalian, China), according to the manufacturer's instructions. The reverse transcription of RNA to cDNA was performed with a reverse transcription kit (Takara). RT-qPCR analyses were conducted using SYBR-Green® (Takara) in triplicate. Results were normalized to the expression of GAPDH (17). The primer sequences used for RT-qPCR were as follows: COL1A1 forward, 5′-GAGGGCCAAGACGAAGACATC-3′, and reverse, 5′-CAGATCACGTCATCGCACAAC-3′; GAPDH forward, 5′-GACTCATGACCACAGTCCATGC-3′, and reverse, 5′-AGAGGCAGGGATGATGTTCTG-3′.
Transwell assay
The migration of transfected CRC cells was determined as previously described (18).
Western blot assay
Proteins were extracted using lysis buffer, and quantified using a Bicinchoninic Acid (BCA) Protein Quantification kit (KeyGen Biotech Co., Ltd., Nanjing, China). Protein lysates were separated via 10% SDS-PAGE and transferred onto a PVDF membrane (Roche, Basel, Switzerland). Subsequently, the membrane was incubated with the specific primary antibodies, followed by the appropriate second antibody. The bands were visualized using a Pierce ECL Western Blotting Substrate (Thermo Fisher Scientific, Inc.). Antibodies against COL1A1, p-JNK and MMP9 were purchased from Abclone. Antibodies against Rac1-GTP and RhoA-GTP were purchased from NewEast Biosciences (Malvern, PA, USA).
Statistical analysis
Data was analyzed by SPSS 20.0 Statistical software. Western blot bands were quantified by Image J 1.45 software. Quantitative data was plotted by Graphpad prism 5 software and presented as the mean ± SD of at least 3 independent experiments. The differences between independent experimental groups were tested by using a two-tailed paired Student's t-test. Differences were considered significant if P<0.05: *P<0.05; **P<0.01; ***P<0.001.
Results
COL1A1 is upregulated in CRC and metastatic lymph node tissues
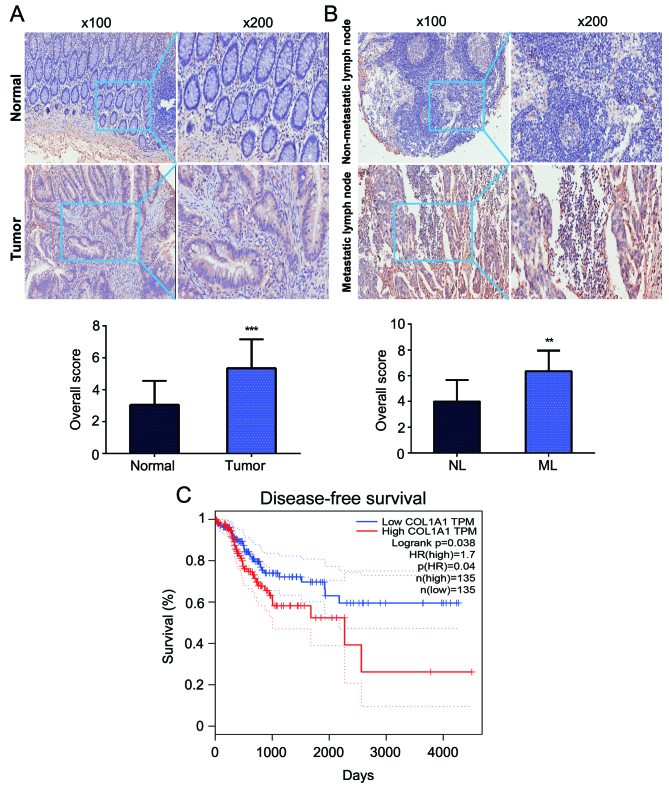
To investigate the role of COL1A1 in CRC tumorigenesis, the expression levels of COL1A1 protein were detected in trios of CRC tissues, adjacent normal counterparts and paired lymph node tissues from 20 patients using IHC analysis. We observed that COL1A1 protein expression was increased in CRC tumor tissues compared with in the adjacent normal mucosae (P<0.001) (Fig. 1A). Furthermore, COL1A1 protein expression in metastatic lymph node tissues was higher than that in non-metastatic lymph node tissues (P<0.01) (Fig. 1B). We further evaluated the prognostic role of COL1A1 in CRC. The data from TCGA showed that the disease-free survival (DFS) of patients with higher COL1A1 expression had worse outcomes than did patients with lower COL1A1 expression (Fig. 1C) (19).
Figure 1.
Expression levels of COL1A1 protein are increased in CRC metastatic lymph node tissues. (A) Representative COL1A1 staining in CRC tissues and adjacent normal tissues. ***P<0.001. (B) Representative COL1A1 staining in metastatic and in non-metastatic lymph node tissues. **P<0.01. (C) DFS analysis based on COL1A1 expression. The log-rank test was used to test the significance of the survival analysis. CRC, colorectal cancer; COL1A1, collagen type I α 1; DFS, disease-free survival.
Knockdown of COL1A1 inhibits CRC cell migration in vitro
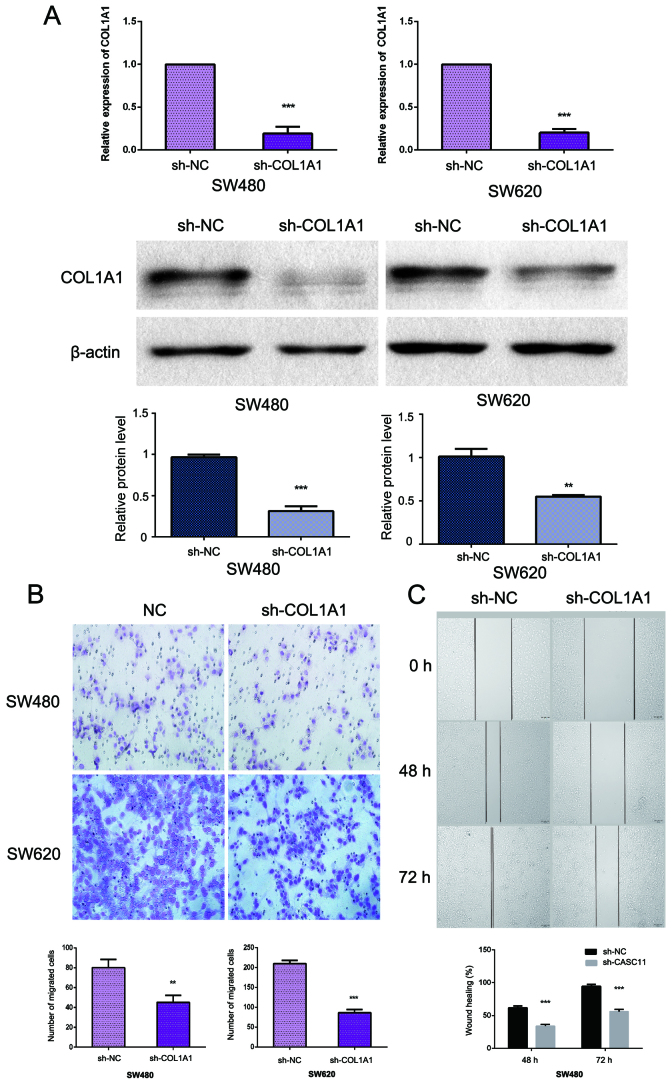
As COL1A1 expression appeared to be associated with metastasis, we evaluated the role of COL1A1 in cell migration. We knocked down COL1A1 using siCOL1A1 in SW480 and SW620 cells (Fig. 2A). Transwell and wound healing assays were used to determine cell motility; the results revealed that the suppression of COL1A1 could attenuate the migration capabilities of SW480 and SW620 cells when compared with cells transfected with a control vector (Fig. 2B and C).
Figure 2.
COL1A1 promotes CRC cell migration in vitro. (A) RT-qPCR and western blot analyses were used to assess COL1A1 mRNA and protein levels following transfection of the siCOL1A1 plasmid. **P<0.01; ***P<0.001. (B) Migration capacity was determined via Transwell assays. The bar chart represents the mean numbers of migrated cells ± SD from 5 different fields. **P<0.01; ***P<0.001. (C) Wound-healing assays were used to determine the migratory ability of siCOL1A1cells. The bar chart represents the wound width (%) at 24 or 48 h, divided by the width at 0 h. Date are presented as the mean ± SD of 3 independent experiments. ***P<0.001. CRC, colorectal cancer; COL1A1, collagen type I α 1.
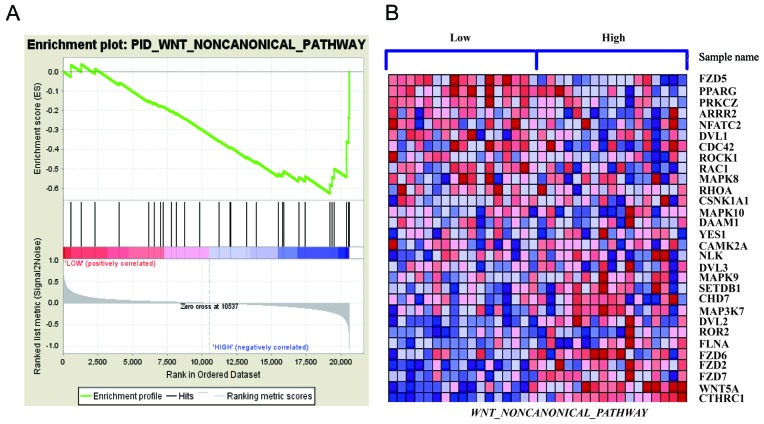
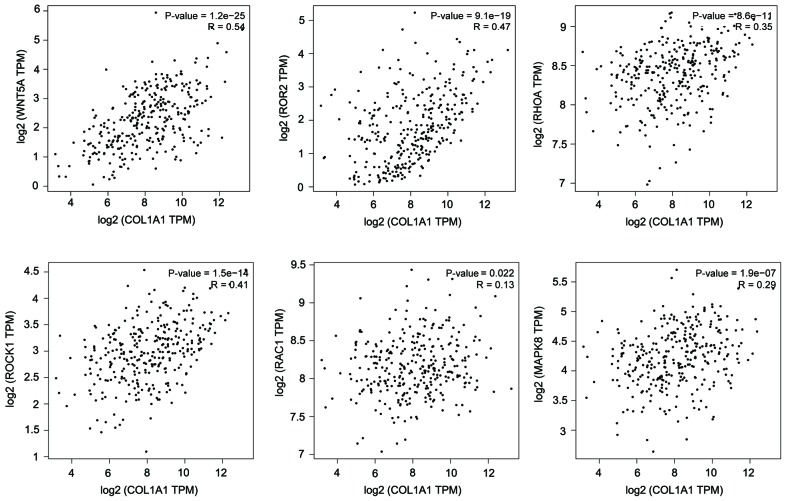
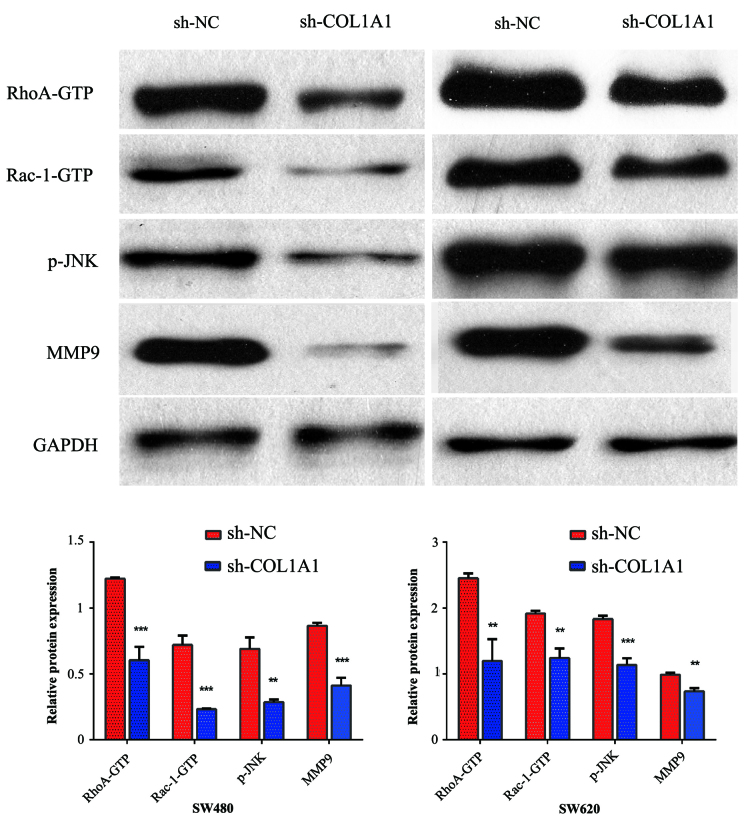
COL1A1 promotes WNT/planar cell polarity (PCP) pathway activation
Through gene set enrichment analysis (GSEA), we analyzed the GSE32323 data and observed that the WNT/PCP signaling pathway was correlated with COL1A1 expression (Fig. 3) (20,21). The results from the TCGA data analysis also showed that COL1A1is correlated with key genes in the WNT/PCP pathway. The results were calculated using the online web service GEPIA (http://gepia.cancer-pku.cn/index.html) (Fig. 4) (19). We hypothesized that COL1A1 could modulate Wnt/PCP signaling. To test the hypothesis that COL1A1 serves an important role in activating WNT/PCP signaling, we detected the expression of key mediators in the WNT/PCP pathway, including Rac1-GTP, p-JNK, RhoA-GTP, and the target gene MMP9, all of which are important contributors to tumor cell migration and invasion. We found that the inhibition of COL1A1 decreased the expression of Rac1-GTP, p-JNK, RhoA-GTP and MMP9 (Fig. 5).
Figure 3.
Analysis of WNT/PCP pathway-related gene enrichment in CRC with high COL1A1 expression. (A) GSEA results showing ‘WNT non-canonical pathway’ signatures enriched in COL1A1 high expression tissue samples. (B) GSEA-generated heat map for highly enriched genes in COL1A1 high-expression samples vs. COL1A1 low-expression samples. PCP, planar cell polarity; GSEA, gene set enrichment analysis; CRC, colorectal cancer; COL1A1, collagen type I α 1.
Figure 4.
Pearson's correlation analysis of COL1A1 and WNT/PCP pathway-related genes. We used the services provided by the website GEPIA (http://gepia.cancer-pku.cn/index.html) to examine the correlations between WNT5A, ROR2, RHOA, ROCK1, RAC1, MAPK9 and COL1A1. COL1A1, collagen type I α 1.
Figure 5.
Western blotting was performed to detect Rac1-GTP, p-JNK, RhoA-GTP and MMP9 expression following COL1A1 knockdown. The expression levels of Rac1-GTP, p-JNK, RhoA-GTP and MMP9 in SW480 and SW620 cells were detected by western blotting, following the knockdown of COL1A1. GAPDH served as the loading control. Data are presented as the mean ± SD of triplicate samples. **P<0.01; ***P<0.001.
Discussion
Metastasis remains the major cause of death in patients with CRC, though the critical molecular mechanisms underlying tumor metastasis are poorly understood. Prior studies have shown that COL1A1 is upregulated in CRC tissues vs. normal tissues (22). COL1A1 is a major component of collagen type I. The available reports regarding COL1A1 have mainly focused on osteogenesis, osteoporosis and bone diseases (23). Recently, many studies have shown COL1A1 to be associated with a variety of tumor types, and that the expression of COL1A1 is increased in tumor tissues and cells (4–14). However, little is known about the function and mechanism of COL1A1 in CRC. In this study, we investigated COL1A1 expression in CRC tumor tissues, adjacent normal counterparts and paired lymph node tissues, and explored its function and underlying mechanism in CRC. Compared with the normal tissues, the expression of COL1A1 was increased in CRC tumor tissues and paired lymph node tissues. Moreover, COL1A1 upregulation in patients with CRC indicated poorer outcomes and DFS. These results indicated that COL1A1functions as an oncogene in CRC progression and is associated with metastasis.
To further ascertain the roles of COL1A1 in CRC, we determined the migration ability of cells with reducedCOL1A1 expression. The results showed that the suppression of COL1A1 decreased the migratory ability of CRC cells; therefore, COL1A1 appears to exert an oncogenic effect, promoting migration in CRC.
The mechanism of COL1A1 in promoting CRC migration is still uncertain. Through GSEA, we found that the WNT/PCP signaling pathway was enriched when COL1A1 was expressed at higher levels. Moreover, COL1A1 expression was correlated with key genes in the WNT/PCP pathway. We further determined that COL1A1 could regulate Rac1-GTP, p-JNK, and RhoA-GTP expression. These findings suggest that COL1A1 may activate the WNT/PCP signaling pathway. The Wnt signaling pathway consists of three branches: The canonical Wnt/β-catenin signaling pathway, which activates gene transcription through β-catenin nuclear localization; the Wnt/PCP pathway, which regulates cytoskeletal rearrangements through the activation of JNK by the small G protein; and the Wnt/Ca2+ pathway, which affects cell adhesion and related gene expression by releasing intracellular Ca2+. Among these, the Wnt/PCP pathway is evolutionarily conserved, and carries signals from cell-surface Frizzled and ROR2/RYK co-receptors to the nucleus via Rho GTPases and JNK, processes that are essential for cell migration (24). Rho GTPases (e.g., Rac1 and RhoA) and JNK are involved in cell morphology, adhesion and metastasis. JNK can rearrange the actin cytoskeleton, thereby regulating the planar polarity of the cell to promote invasion and metastasis of the tumor. JNK can also increase the secretion of MMPs in CRC cells to promote their metastasis (25–27). Therefore, we speculated that COL1A1 may promote CRC cell migration through the WNT/PCP pathway.
In summary, our results indicated that COL1A1 promotes tumor metastasis, and that its inhibition may suppress CRC cell migration. In addition, the role of COL1A1 in CRC metastasis seems to be associated with the regulation of the WNT/PCP pathway. Our findings also indicated that COL1A1 may be a promising therapeutic target for CRC.
Acknowledgements
The present study was supported by funding from the Xinxiang Medical College (grant nos. XYBSKYZZ201632 and 2014ZD109), Higher Education Institutions of Henan Province, China (no. 17A310023), the National Natural Science Foundation of China (no. 81702891), Taihang Young Scholar Foundation of Xinxiang Medical University, Doctoral Scientific Research Foundation of Xinxiang Medical University (no. 505079).
References
- 1.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2017. CA Cancer J Clin. 2017;67:7–30. doi: 10.3322/caac.21387. [DOI] [PubMed] [Google Scholar]
- 2.Maasalu K, Nikopensius T, Kõks S, Nõukas M, Kals M, Prans E, Zhytnik L, Metspalu A, Märtson A. Whole-exome sequencing identifies de novo mutation in the COL1A1 gene to underlie the severe osteogenesis imperfecta. Hum Genomics. 2015;9:6. doi: 10.1186/s40246-015-0028-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Simon MP, Maire G, Pedeutour F. COL1A1 (collagen, type I, alpha 1) Atlas Genet Cytogenet Oncol Haematol. 2001;5:78–82. [Google Scholar]
- 4.Tian ZQ, Li ZH, Wen SW, Zhang YF, Li Y, Cheng JG, Wang GY. Identification of commonly dysregulated genes in non-small-cell lung cancer by integrated analysis of microarray data and qRT-PCR validation. Lung. 2015;193:583–592. doi: 10.1007/s00408-015-9726-6. [DOI] [PubMed] [Google Scholar]
- 5.Li J, Ding Y, Li A. Identification of COL1A1 and COL1A2 as candidate prognostic factors in gastric cancer. World J Surg Oncol. 2016;14:297. doi: 10.1186/s12957-016-1056-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Song Y, Kim SH, Kim KM, Choi EK, Kim J, Seo HR. Activated hepatic stellate cells play pivotal roles in hepatocellular carcinoma cell chemoresistance and migration in multicellular tumor spheroids. Sci Rep. 2016;6:36750. doi: 10.1038/srep36750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhang H, Liu B, Xu XF, Jiang TT, Zhang XQ, Shi YL, Chen Y, Liu F, Gu J, Zhu LJ, Wu N. Pathophysiology of chronic pancreatitis induced by dibutyltin dichloride joint ethanol in mice. World J Gastroenterol. 2016;22:2960–2970. doi: 10.3748/wjg.v22.i10.2960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Boguslawska J, Kedzierska H, Poplawski P, Rybicka B, Tanski Z, Piekielko-Witkowska A. Expression of genes involved in cellular adhesion and extracellular matrix remodeling correlates with poor survival of patients with renal cancer. J Urol. 2016;195:1892–1902. doi: 10.1016/j.juro.2015.11.050. [DOI] [PubMed] [Google Scholar]
- 9.Willis CM, Klüppel M. Chondroitin sulfate-E is a negative regulator of a pro-tumorigenic Wnt/beta-catenin-Collagen 1 axis in breast cancer cells. PLoS One. 2014;9:e103966. doi: 10.1371/journal.pone.0103966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brooks M, Mo Q, Krasnow R, Ho PL, Lee YC, Xiao J, Kurtova A, Lerner S, Godoy G, Jian W, et al. Positive association of collagen type I with non-muscle invasive bladder cancer progression. Oncotarget. 2016;7:82609–82619. doi: 10.18632/oncotarget.12089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hurst R, Elliott RM, Goldson AJ, Fairweather-Tait SJ. Se-methylselenocysteine alters collagen gene and protein expression in human prostate cells. Cancer Lett. 2008;269:117–126. doi: 10.1016/j.canlet.2008.04.025. [DOI] [PubMed] [Google Scholar]
- 12.Poplawski P, Rybicka B, Boguslawska J, Rodzik K, Visser TJ, Nauman A, Piekielko-Witkowska A. Induction of type 1 iodothyronine deiodinase expression inhibits proliferation and migration of renal cancer cells. Mol Cell Endocrinol. 2017;442:58–67. doi: 10.1016/j.mce.2016.12.004. [DOI] [PubMed] [Google Scholar]
- 13.Yu PN, Yan MD, Lai HC, Huang RL, Chou YC, Lin WC, Yeh LT, Lin YW. Downregulation of miR-29 contributes to cisplatin resistance of ovarian cancer cells. Int J Cancer. 2014;134:542–551. doi: 10.1002/ijc.28399. [DOI] [PubMed] [Google Scholar]
- 14.Balbous A, Cortes U, Guilloteau K, Villalva C, Flamant S, Gaillard A, Milin S, Wager M, Sorel N, Guilhot J, et al. A mesenchymal glioma stem cell profile is related to clinical outcome. Oncogenesis. 2014;3:e91. doi: 10.1038/oncsis.2014.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yuan L, Zhou C, Lu Y, Hong M, Zhang Z, Zhang Z, Chang Y, Zhang C, Li X. IFN-γ-mediated IRF1/miR-29b feedback loop suppresses colorectal cancer cell growth and metastasis by repressing IGF1. Cancer Lett. 2015;359:136–147. doi: 10.1016/j.canlet.2015.01.003. [DOI] [PubMed] [Google Scholar]
- 16.Gu Y, Wang Q, Guo K, Qin W, Liao W, Wang S, Ding Y, Lin J. TUSC3 promotes colorectal cancer progression and epithelial-mesenchymal transition (EMT) through WNT/β-catenin and MAPK signalling. J Pathol. 2016;239:60–71. doi: 10.1002/path.4697. [DOI] [PubMed] [Google Scholar]
- 17.Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) method. Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 18.Zhou C, Liu G, Wang L, Lu Y, Yuan L, Zheng L, Chen F, Peng F, Li X. MiR-339-5p regulates the growth, colony formation and metastasis of colorectal cancer cells by targeting PRL-1. PLoS One. 2013;8:e63142. doi: 10.1371/journal.pone.0063142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tang Z, Li C, Kang B, Gao G, Li C, Zhang Z. GEPIA: A web server for cancer and normal gene expression profiling and interactive analyses. Nucleic Acids Res. 2017 Apr 12; doi: 10.1093/nar/gkx247. (Epub ahead of print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mootha VK, Lindgren CM, Eriksson KF, Subramanian A, Sihag S, Lehar J, Puigserver P, Carlsson E, Ridderstråle M, Laurila E, et al. PGC-1alpha-responsive genes involved in oxidative phosphorylation are coordinately downregulated in human diabetes. Nat Genet. 2003;34:267–273. doi: 10.1038/ng1180. [DOI] [PubMed] [Google Scholar]
- 21.Subramanian A, Tamayo P, Mootha VK, Mukherjee S, Ebert BL, Gillette MA, Paulovich A, Pomeroy SL, Golub TR, Lander ES, Mesirov JP. Gene set enrichment analysis: A knowledge-based approach for interpreting genome-wide expression profiles; Proc Natl Acad Sci USA; 2005; pp. 15545–15550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zou X, Feng B, Dong T, Yan G, Tan B, Shen H, Huang A, Zhang X, Zhang M, Yang P, et al. Up-regulation of type I collagen during tumorigenesis of colorectal cancer revealed by quantitative proteomic analysis. J Proteomics. 2013;94:473–485. doi: 10.1016/j.jprot.2013.10.020. [DOI] [PubMed] [Google Scholar]
- 23.Byers PH, Pyott SM. Recessively inherited forms of osteogenesis imperfecta. Annu Rev Genet. 2012;46:475–497. doi: 10.1146/annurev-genet-110711-155608. [DOI] [PubMed] [Google Scholar]
- 24.Pan Y, Guo X, Yang Z, Chen S, Lei Y, Lin M, Wang L, Feng C, Ke Z. AEG-1 activates Wnt/PCP signaling to promote metastasis in tongue squamous cell carcinoma. Oncotarget. 2016;7:2093–2104. doi: 10.18632/oncotarget.6573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zeke A, Misheva M, Reményi A, Bogoyevitch MA. JNK signaling: Regulation and functions based on complex protein-protein partnerships. Microbiol Mol Biol Rev. 2016;80:793–835. doi: 10.1128/MMBR.00043-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Monin MB, Krause P, Stelling R, Bocuk D, Niebert S, Klemm F, Pukrop T, Koenig S. The anthelmintic niclosamide inhibits colorectal cancer cell lines via modulation of the canonical and noncanonical Wnt signaling pathway. J Surg Res. 2016;203:193–205. doi: 10.1016/j.jss.2016.03.051. [DOI] [PubMed] [Google Scholar]
- 27.Zhang Y, Lin L, Jin Y, Lin Y, Cao Y, Zheng C. Overexpression of WNT5B promotes COLO 205 cell migration and invasion through the JNK signaling pathway. Oncol Rep. 2016;36:23–30. doi: 10.3892/or.2016.4772. [DOI] [PubMed] [Google Scholar]