Abstract
Background
Patients with poor underlying prognosis experiencing surgical emergencies face challenging treatment decisions. The Best Case/Worst Case (BC/WC) framework has improved shared decision-making by surgeons, but it is unclear whether residents can be similarly trained. We evaluated senior general surgical residents’ acceptance of the BC/WC tool and their attitudes, confidence and actions before and after training.
Methods
Two-hour training included a didactic session, live demonstration, small-group practice and debriefing. We developed questionnaires to evaluate residents’ attitudes, confidence and actions at 3 time points: before the intervention, after the intervention and 6 months after the intervention. We used the Ottawa Decision Support Framework Acceptability questionnaire to evaluate acceptability and a structured observation form to evaluate performance.
Results
Eighteen (50%) of 36 invited residents participated. Most residents (83%) felt that a new communication tool would be useful. Almost all (94%) used BC/WC in practice. Residents found the tool acceptable and useful to enhance preference-sensitive communications. They felt that the training was valuable and that role play was its greatest strength but that these situations were challenging to simulate. Barriers to BC/WC use included time constraints and difficulty defining the best and worst cases precisely. Summative attitudes and confidence scores were not different before and after the intervention; however, actions scores were higher after the intervention (p = 0.04). Residents performed a median of 15 (interquartile range 13–17) of the 19 elements on the formative performance evaluation. Commonly missed items were narrating outcomes of palliative approaches, prompting deliberation and providing treatment recommendations.
Conclusion
Senior residents found the BC/WC tool to be acceptable and useful, and are amenable to training in this type of communication. After training, self-reported actions scores increased, and observed performance was accurate.
Abstract
Contexte
La prise de décisions relatives au traitement est difficile pour les patients qui ont un pronostic sous-jacent défavorable et qui envisagent une intervention chirurgicale d’urgence. Le cadre d’évaluation de la meilleure et de la pire issue possible (Best Case/Worst Case framework [BC/WC]) a amélioré la prise de décision partagée chez les chirurgiens, mais on ignore si les médecins résidents adopteraient aussi facilement une formation sur un tel cadre. Nous avons évalué à quel point les médecins résidents principaux en chirurgie générale étaient prêts à accepter le cadre BC/WC, ainsi que leur attitude, leur confiance et leurs actions avant et après une formation sur celui-ci.
Méthodes
La formation de 2 heures comprenait une présentation didactique, une démonstration pratique, une période d’essai en petits groupes et un débreffage. Nous avons créé un questionnaire évaluant l’attitude, la confiance et les actions des médecins résidents à 3 moments : avant la formation, immédiatement après celle-ci et 6 mois plus tard. Nous avons utilisé le questionnaire sur l’admissibilité du Modèle d’aide à la décision d’Ottawa pour évaluer le degré d’acceptation du cadre, et un formulaire d’observation structurée pour évaluer son application au travail.
Résultats
Des 36 médecins résidents invités, 18 (50 %) ont accepté de participer. La plupart d’entre eux (83 %) croyaient qu’un nouvel outil de communication leur serait utile. Presque tous (94 %) ont appliqué le cadre BC/WC dans leur travail. Ils l’ont trouvé acceptable, et considéraient qu’il permettait d’améliorer la communication tenant compte des préférences. Selon eux, la formation était utile, particulièrement les mises en situation, mais la nature des interactions se prêtait mal à la simulation. Interrogés sur les obstacles à l’application du cadre, ils ont cité les contraintes de temps et la difficulté de définir avec précision la meilleure et la pire issue. Les résultats sommatifs pour l’attitude et la confiance étaient similaires avant et après la formation; cependant, la note pour les actions était plus élevée après la formation qu’avant (p = 0,04). Pour l’évaluation formative du travail, la note médiane était de 15 (écart interquartile : 13 à 17), sur un total de 19 éléments. Parmi les éléments couramment oubliés, notons la description des issues des approches palliatives, l’incitation à la discussion et la formulation de recommandations de traitement.
Conclusion
Les médecins résidents considèrent le cadre BC/WC acceptable et utile, et seraient disposés à suivre une formation sur le type de communication qu’il prône. Après la formation, la note de l’auto-évaluation des actions a augmenté, une tendance aussi constatée à l’observation du travail.
Patients with poor underlying prognosis who experience a surgical emergency face challenging treatment decisions. With an aging population, this situation is not uncommon in frail older patients with multimorbidity. Although efforts have been made to promote the use of advance directives, many patients have not previously considered what their preferences might be in the setting of a surgical emergency.1 Some may assume that surgical emergencies have a “fix,” but this is not often the case, and many patients receive nonbeneficial interventions.2,3 In these cases, treatment decisions are challenging, as consideration must be given to remaining life expectancy, underlying health status and a shifted risk–benefit balance.4 Furthermore, these patients may place higher importance on outcomes such as functional independence, symptom control, quality of life and avoiding prolonged recovery.5–7 These situations are characterized by uncertainty, a high level of risk and decision-making that is preference sensitive.8
Surgeons usually lack training in preference-sensitive communication skills to provide decisional support in situations that require complex weighing of desirable and undesirable outcomes.9 There is considerable variability in how these discussions go, and surgeons and trainees report challenges with perioperative communication.10 Often, surgeons frame discussions within the structure of informed consent, which emphasizes the risks of operative intervention and the likelihood of death without surgery.11 This approach does not convey information in relation to a patients’ values or about what it may be like to experience undesirable outcomes and how these may affect quality of life, need for additional treatment and functional status.12 In addition, options may be framed as a choice between certain death with a nonoperative palliative approach versus a surgical intervention carrying high risk for death and complications; within this framework, many patients hope that they are within the group that survives surgical intervention.13 In focusing solely on high-risk surgery as an attempt to avoid certain death, the patient’s overall prognosis and the impact of nonbeneficial interventions are not adequately addressed.14,15
Work has been done recently to elucidate the unique and growing communication needs among surgeons, older patients and their families during a surgical emergency. Cooper and colleagues16 identified pitfalls in communication that lead to nonbeneficial emergency surgery, and an interdisciplinary expert panel provided recommendations to overcome this.17 The Best Case/Worst Case (BC/WC) framework is a decision support tool developed to improve communication between surgeons and patients with poor underlying prognosis experiencing life-threatening surgical emergencies.13,15 This framework has been used to change how practising surgeons structure discussions for high-risk surgical decisions and to promote shared decision-making.11,18 Several programs have been developed to educate surgical residents on geriatric topics, yet none specifically addresses the issue of communication about surgical emergencies in patients with poor underlying prognosis.19–23 Although BC/WC was taught successfully to practising surgeons, it is unclear for several reasons whether surgical trainees would be amenable to training of this kind. For instance, trainees may feel that this type of communication and decision-making should be conducted by faculty surgeons, that this situation does not require specific communication skills or that specific training is not necessary in addition to existing communication training in medical education. Therefore, we aimed to evaluate senior general surgical residents’ rating of the acceptability and usefulness of training using BC/WC and to evaluate their attitudes, confidence and actions before and after training.
Methods
Study design and population
We conducted a self-controlled time-series study at a large university-based general surgery residency training program. All senior general surgery residents in years 3, 4 or 5 of a 5-year training program at the University of Toronto were invited to participate. At the University of Toronto, senior general surgery residents have weekly scheduled teaching half-days; 1 session was used for the intervention and 1 was used for evaluation. All participants provided written informed consent. The University of Toronto Research Ethics Board approved this research.
Best Case/Worst Case framework
The BC/WC framework is a decision-support tool developed by the University of Wisconsin research group to improve communication between surgeons and patients facing high-risk surgical decisions.9,13,15,18 A graphic and detailed description of the tool is available in the initial publications.11,18 The framework is based on a foundation of shared decision-making that is useful in situations in which uncertainty surrounds outcomes and the best choice requires an understanding of the patient’s values.24 The tool aims to help surgeons provide information about treatment options in a way that contextualizes surgical decisions into a larger personal framework for patients. It provides a framework to present treatment options, discuss possible outcomes, including those that are more likely, express uncertainty, promote dialogue and deliberation in the context of life-threatening illness, and enable patients to express preferences for relevant outcomes. We selected the BC/WC framework for our study because, unlike most decision aids, it offers the advantage of flexibility for decision-making in the emergency setting and strives to convey the broader clinical picture of various treatment options and potential outcomes rather than simply enumerating separate risks and benefits.25
Intervention
For this study, we adapted the BC/WC framework. The 2-hour training intervention included a didactic session, a live demonstration, small-group practice and debriefing. The didactic session involved a 15-minute predesigned lecture by faculty covering the unique decisional challenge presented by patients with poor underlying prognosis facing a new life-threatening surgical emergency, the burden of unwanted and nonbeneficial care, and a case presentation with narrative examples. This was followed by a 10-minute live role-play demonstration by 2 faculty members. The remaining training consisted of small-group practice through case-based role-play facilitated by trained instructors. For this, residents clustered into groups of 2–3 and used predesigned case prompts to practise using BC/WC. Residents were provided with pocket cards with the BC/WC visual aid. Residents used observation forms, also developed by the developers of the BC/WC tool, to check each other’s performance during this practice. Trained instructors observed and facilitated this session. Finally, there was a 15-minute large-group debriefing to discuss the use of BC/WC. Residents were encouraged to do more practice at home before their formative performance evaluation and to use the tool clinically once their evaluation was completed.
Outcome measures
We used multiple outcome measures collected at 3 time points: before the intervention, after the intervention and 6 months after the intervention.
Formative performance evaluation was conducted 2 weeks after the training intervention. This included a standardized case and observation by a trained instructor using a 19-point structured observation form developed for this purpose. After this, residents were given formative feedback about their performance.
We used the Ottawa Decision Support Framework Acceptability questionnaire to evaluate the acceptability of BC/WC by residents after the intervention.26 This 15-question instrument is designed to elicit a tool’s acceptability to practitioners. The questionnaire was administered after the intervention and at 6 months.
Last, we developed a questionnaire for this study to evaluate the residents’ attitudes, confidence and actions using standard methods for survey research.27,28 To create the questionnaire, we generated items within the domains of attitudes, confidence and actions related to communication with patients with poor underlying prognosis facing a life-threatening surgical emergency. Item generation was continued to achieve sampling to redundancy within each domain with the use of a table of specifications, which was then used to eliminate items to create the shortest possible questionnaire without important omissions. Each item was then pre-tested by 3 reviewers to ensure clarity of wording. The full questionnaire was then pilot tested by 6 reviewers to evaluate flow, timing, meaning and comprehensibility. Sensibility testing by 3 reviewers with content expertise was conducted to evaluate face validity and content validity ensuring pertinence, accuracy and completeness of scope. The final questionnaire contained Likert-type questions within each domain, and other Likert-type and open-ended questions were included to evaluate attitudes about BC/WC and the training intervention (Appendix 1, available at canjsurg.ca/011317-a1). The questionnaire was administered before the intervention, after the intervention and at 6 months.
Statistical analysis
The responses to the Ottawa Decision Support Framework Acceptability questionnaire were calculated as percentages for agree, neutral and disagree, and displayed graphically. We summed the scores on the 7-point Likert-type questions within each of the attitudes, confidence and actions domains and used equal weighting to create summative 21-point scales within each domain at each of the 3 time points (before the intervention, after the intervention and at 6 mo). We used the Friedman test for repeated measures to test for change between the 3 time points. Scores on individual Likert-type questions regarding BC/WC and the training intervention were calculated as percentages for agree, neutral and disagree. We analyzed open-ended questions using simple methods to identify themes and ideas that were summarized narratively. We analyzed quantitative data using SAS software, version 9.4 (SAS Institute). Two-sided p values of less than 0.05 were considered to indicate statistical significance.
Results
Eighteen (50%) of the 36 invited residents participated. On the formative performance evaluation, residents performed a median of 15 (79%) (interquartile range 13–17) of the 19 elements on the structured observation form. The 2 best-performed elements, performed by all residents, were presenting 2 explicit treatment options and avoiding medical jargon. Four elements were performed by less than 60% of residents. The 2 most commonly missed elements were making a recommendation at the end of the encounter, and encouraging deliberation after describing the treatment options and possible outcomes. Residents also were challenged by describing the worst case for the palliative treatment option and providing narrative stories for the possible outcomes of a palliative approach.
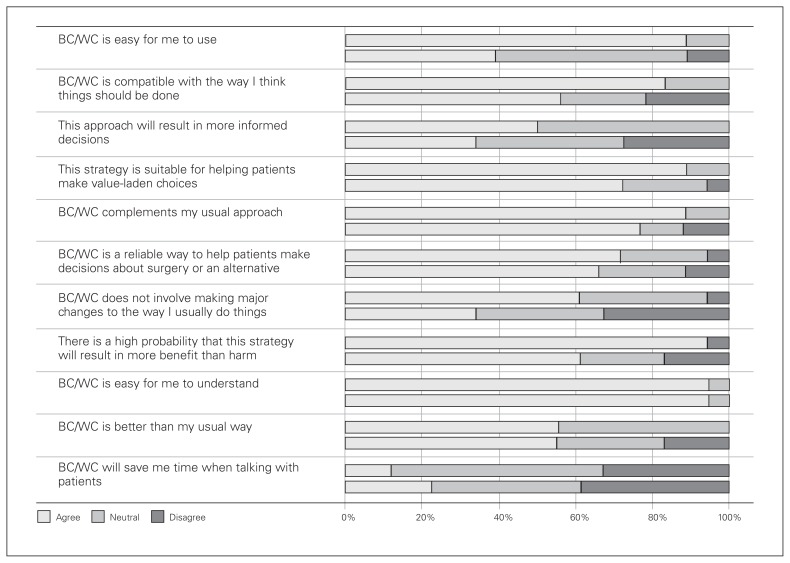
Results of the Ottawa Decision Support Framework Acceptability questionnaire after the intervention and at 6 months are displayed in Fig. 1. After the intervention, 84% of residents felt that BC/WC was compatible with the way they thought things should be done, but, on follow-up, only 56% agreed. A total of 70% felt BC/WC was a reliable way to help patients decide about surgery or an alternative. At both time points, almost all residents (95%) found BC/WC easy to understand. Just over half (55%) felt BC/WC was better than their usual way.
Fig. 1.
Responses to the Ottawa Decision Support Framework questionnaire. For each question, the upper bar is the posttraining response before using the tool clinically, and the lower bar is the 6-month follow-up response.
Before the intervention, most residents (89%) agreed that they see patients at high risk presenting with life-threatening surgical conditions. Likewise, most (83%) agreed that a new communication tool to support discussion would be useful. After the intervention, most residents agreed that the intervention was useful (89%) and that it had increased their knowledge (83%) and confidence (78%) in having conversations with patients at high risk facing a life-threatening surgical emergency. After the intervention, 83% of residents intended to use BC/WC clinically. Most (94%) reported using BC/WC at least once in practice at the 6-month follow-up: 22% had used the tool often, 50% had used it sometimes, and 28% had used it infrequently. One-third of residents felt that their patients responded positively to BC/WC, 56% were neutral, and 11% did not agree.
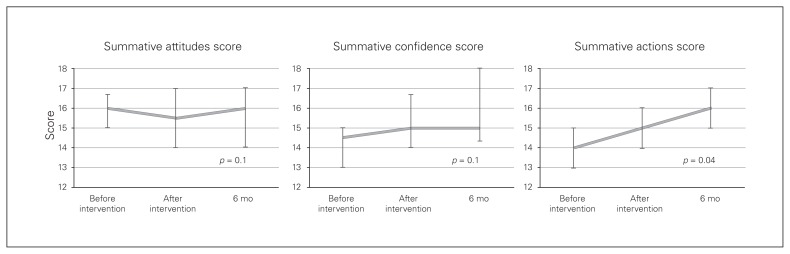
The summative attitudes, confidence and actions scores across the 3 time points are displayed in Fig. 2. Summative attitudes and confidence scores were not different before and after the intervention; however, action scores increased significantly (p = 0.04).
Fig. 2.
Summative attitudes, confidence and actions scores before the intervention, after the intervention and 6 months after the intervention. Each domain has a maximum score of 21. Differences were tested with the Friedman test.
On open-ended questioning, residents reported that BC/WC was simple and that the visual aid helped patients understand the possible outcomes of various treatment choices and acted as a useful guide to discussion. The training intervention was noted to be well prepared, and the opportunity to role play was felt to be a valuable component of the training program. Some residents felt that it was difficult to simulate real conversation during the practice session.
Residents noted some barriers to the use of BC/WC, with the most commonly mentioned barrier being time. These conversations can be time-consuming. It is unclear whether this is due to the tool or is just the nature of this type of conversation. Some felt that the subjectivity of the narrative description of the best cases and worst cases was a barrier, and some had difficulty in deciding what the best and worst cases might be. Residents pointed out that the BC/WC tool may not be appropriate in all situations (e.g., in cases of a language barriers), that some patients may not prefer this type of approach, and that this approach may be too complicated for some patients.
Discussion
Senior general surgery residents are amenable to training on communication skills specific to the situation of shared decision-making with patients with poor underlying prognosis experiencing life-threatening surgical emergencies. Half of invited residents made time to participate in this intervention, and most residents agreed they encounter patients in this situation and that a new communication tool would be useful. It is clear that residents believe this situation warrants specific communication skills and that this type of training is necessary despite communication training in medical education.
Most residents found the training useful. Almost all used the BC/WC tool in their clinical practice after training, with 72% using it at least sometimes. Largely, residents found the tool to be acceptable, but barriers to use included time constraints and difficulty defining precisely the best and worst cases. Attitudes and confidence scores did not improve, which suggests that senior residents already felt that these communications were important before training. However, self-reported actions scores increased, which suggests that residents more often completed the tasks emphasized by BC/WC for communication and shared decision-making in this situation after training. During observed performance evaluation, residents performed nearly all scored elements, but more emphasis needs to be placed on narrating the outcomes of a palliative treatment option, prompting deliberation and providing a treatment recommendation.
Our findings show that senior residents value training in this type of communication and that this type of decision-making and communication training should not be limited to faculty surgeons. Our findings are similar to those observed among practising surgeons.18 The surgeons also completed nearly all scored elements (10 of 11 elements). The element most commonly omitted was making a recommendation. In our study, residents also most often omitted making a recommendation, but they also commonly missed encouraging deliberation about options and had difficulty narrating palliative treatment options. The greatest differences between surgeons was the narrative they used to describe the best and worst cases.18 Similarly, in our study, the residents found the subjectivity of the narrative description of the best and worst cases to be a challenge, and some experienced difficulty in deciding what the best and worst cases might be. Like our participants, nearly all practising surgeons felt that BC/WC was easy to use, and most did not feel that it would save time. The proportion of participants who reported using the tool in clinical practice was higher among residents than practising surgeons (94% vs. 71%).
Most of our participants (56%) felt that patients responded neutrally to discussions using BC/WC. This likely reflects the nature of this kind of discussion, and positive responses may not be expected. However, prior focus groups showed that older adults responded positively to the use of this type of communication framework when presented with hypothetical scenarios.15 Further research should focus on patients’ experiences of these encounters with residents.
Limitations
Our findings must be interpreted in the context of our study’s limitations. The actions summative score is a self-reported score and may not reflect true clinical activity. However, the formative performance evaluation supports the accurate use of BC/WC by senior residents in a simulated setting. Although we followed up at 6 months, this follow-up was on a paper-based questionnaire and not observed practice. Further investigations with direct observation at longer follow-up times are required to determine the longevity of the learning obtained with this training intervention. The impact of the use of BC/WC by residents on patients and their families and on how decisions are made requires further investigation. It is not clear whether these findings are generalizable to more junior trainees. Likewise, given the degree of graduated responsibility provided in the training environment of this study, whereby senior residents commonly initiate these discussions with the support of faculty surgeons, these results may not be generalizable to training environments that do not allow for this. In Canada, the new availability of medical assistance in dying provides yet another treatment option available to patients with a grievous and irremediable medical condition if all requirements are met.29 One requirement that may not be met by patients with sudden life-threatening surgical emergencies is that of a 10-day period of reflection. It is not clear whether the availability of medical assistance in dying will change the conversations surgeons have with their patients; however, it remains the role of surgeons to guide responsible and thoughtful communication with their patients experiencing life-threatening conditions. Medical assistance in dying may be one of the legitimate options available to eligible patients, along with alternative, less-invasive surgical interventions, time-limited trials, medical options and palliative care. Adequately supporting our patients who are experiencing life-threatening emergencies with poor underlying prognosis is paramount as they make high-stakes decisions in the face of uncertainty.
Conclusion
Residents encounter patients with poor underlying prognosis experiencing life-threatening surgical emergencies and feel that training for this is needed. Senior general surgery residents find BC/WC to be acceptable and useful to enhance preference-sensitive communications in these situations. Senior residents are amenable to training in this type of communication and shared decision-making and do not feel that this should limited to faculty surgeons. The fact that attitudes and confidence scores did not improve after training may reflect residents’ feelings that these communications were important even before training. Observed performance was accurate. More emphasis needs to be placed on narrating the possible outcomes of a palliative treatment, prompting deliberation and providing a treatment recommendation.
Footnotes
Competing interests: None declared.
Contributors: Both authors designed the study and acquired and analyzed the data. T. Chesney wrote the article, which both authors reviewed and approved for publication.
References
- 1.Yadav KN, Gabler NB, Cooney E, et al. Approximately one in three US adults completes any type of advance directive for end-of-life care. Health Aff. 2017;36:1244–51. doi: 10.1377/hlthaff.2017.0175. [DOI] [PubMed] [Google Scholar]
- 2.Kruser JM, Pecanac KE, Brasel KJ, et al. “And I think that we can fix it”: mental models used in high-risk surgical decision making. Ann Surg. 2015;261:678–84. doi: 10.1097/SLA.0000000000000714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kwok AC, Semel ME, Lipsitz SR, et al. The intensity and variation of surgical care at the end of life: a retrospective cohort study. Lancet. 2011;378:1408–13. doi: 10.1016/S0140-6736(11)61268-3. [DOI] [PubMed] [Google Scholar]
- 4.Yourman LC, Lee SJ, Schonberg MA, et al. Prognostic indices for older adults: a systematic review. JAMA. 2012;307:182–92. doi: 10.1001/jama.2011.1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fried TR, Van Ness PH, Byers AL, et al. Changes in preferences for life-sustaining treatment among older persons with advanced illness. J Gen Intern Med. 2007;22:495–501. doi: 10.1007/s11606-007-0104-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Barnato AE, Herndon MB, Anthony DL, et al. Are regional variations in end-of-life care intensity explained by patient preferences? A study of the US Medicare population. Med Care. 2007;45:386. doi: 10.1097/01.mlr.0000255248.79308.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Teno JM, Fisher ES, Hamel MB, et al. Medical care inconsistent with patients’ treatment goals: association with 1-year Medicare resource use and survival. J Am Geriatr Soc. 2002;50:496–500. doi: 10.1046/j.1532-5415.2002.50116.x. [DOI] [PubMed] [Google Scholar]
- 8.Whitney SN, McGuire AL, McCullough LB. A typology of shared decision making, informed consent, and simple consent. Ann Intern Med. 2004;140:54–9. doi: 10.7326/0003-4819-140-1-200401060-00012. [DOI] [PubMed] [Google Scholar]
- 9.Nabozny MJ, Kruser JM, Steffens NM, et al. Constructing high-stakes surgical decisions: It’s better to die trying. Ann Surg. 2016;263:64–70. doi: 10.1097/SLA.0000000000001081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chesney TR, Pang G, Ahmed N. Caring for older surgical patients: contemporary attitudes, knowledge, practices, and needs of general surgeons and residents. Ann Surg. 2017 Jun 6; doi: 10.1097/SLA.0000000000002363. [DOI] [PubMed] [Google Scholar]
- 11.Taylor LJ, Nabozny MJ, Steffens NM, et al. A framework to improve surgeon communication in high-stakes surgical decisions: Best Case/Worst Case. JAMA Surg. 2017;152:531–8. doi: 10.1001/jamasurg.2016.5674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Neuman MD, Bosk CL. What we talk about when we talk about risk: refining surgery’s hazards in medical thought. Milbank Q. 2012;90:135–59. doi: 10.1111/j.1468-0009.2011.00657.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schwarze ML, Kehler JM, Campbell TC. Navigating high risk procedures with more than just a street map. J Palliat Med. 2013;16:1169–71. doi: 10.1089/jpm.2013.0221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schwarze ML, Nabozny MJ. How people die in 2014. Ann Surg. 2014;260:958–9. doi: 10.1097/SLA.0000000000000847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kruser JM, Nabozny MJ, Steffens NM, et al. “Best Case/Worst Case”: qualitative evaluation of a novel communication tool for difficult in-the-moment surgical decisions. J Am Geriatr Soc. 2015;63:1805–11. doi: 10.1111/jgs.13615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cooper Z, Courtwright A, Karlage A, et al. Pitfalls in communication that lead to nonbeneficial emergency surgery in elderly patients with serious illness: description of the problem and elements of a solution. Ann Surg. 2014;260:949–57. doi: 10.1097/SLA.0000000000000721. [DOI] [PubMed] [Google Scholar]
- 17.Cooper Z, Koritsanszky LA, Cauley CE, et al. Recommendations for best communication practices to facilitate goal-concordant care for seriously ill older patients with emergency surgical conditions. Ann Surg. 2016;263:1–6. doi: 10.1097/SLA.0000000000001491. [DOI] [PubMed] [Google Scholar]
- 18.Kruser JM, Taylor LJ, Campbell TC, et al. “Best Case/Worst Case”: training surgeons to use a novel communication tool for high-risk acute surgical problems. J Pain Symptom Manage. 2017;53:711–9. e5. doi: 10.1016/j.jpainsymman.2016.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Barbas AS, Haney JC, Henry BV, et al. Development and implementation of a formalized geriatric surgery curriculum for general surgery residents. Gerontol Geriatr Educ. 2014;35:380–94. doi: 10.1080/02701960.2013.879444. [DOI] [PubMed] [Google Scholar]
- 20.Bradley CT, Webb TP, Schmitz CC, et al. Structured teaching versus experiential learning of palliative care for surgical residents. Am J Surg. 2010;200:542–7. doi: 10.1016/j.amjsurg.2009.12.014. [DOI] [PubMed] [Google Scholar]
- 21.Webb TP, Duthie E. Geriatrics for surgeons: infusing life into an aging subject. J Surg Educ. 2008;65:91–4. doi: 10.1016/j.jsurg.2007.12.004. [DOI] [PubMed] [Google Scholar]
- 22.Duane TM, Fan L, Bohannon A, et al. Geriatric education for surgical residents: identifying a major need. Am Surg. 2011;77:826–31. [PubMed] [Google Scholar]
- 23.Petronovich J, Wade TJ, Denson K, et al. Elderly surgical patients: Are there gaps in residency education? J Surg Educ. 2014;71:825–8. doi: 10.1016/j.jsurg.2014.04.001. [DOI] [PubMed] [Google Scholar]
- 24.Charles C, Gafni A, Whelan T. Shared decision-making in the medical encounter: What does it mean? (or it takes at least two to tango) Soc Sci Med. 1997;44:681–92. doi: 10.1016/s0277-9536(96)00221-3. [DOI] [PubMed] [Google Scholar]
- 25.Knops AM, Legemate DA, Goossens A, et al. Decision aids for patients facing a surgical treatment decision: a systematic review and meta-analysis. Ann Surg. 2013;257:860–6. doi: 10.1097/SLA.0b013e3182864fd6. [DOI] [PubMed] [Google Scholar]
- 26.Patient Decision Aids Research Group. Ottawa Decision Support Framework: Acceptability. 2002. [accessed 2018 Feb 28]. Available: https://decisionaid.ohri.ca/docs/develop/User_Manuals/UM_Acceptability.pdf.
- 27.Burns KE, Duffett M, Kho ME, et al. A guide for the design and conduct of self-administered surveys of clinicians. CMAJ. 2008;179:245–52. doi: 10.1503/cmaj.080372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dillman DA. Mail and internet surveys: the tailored design method. 2nd ed. Hoboken (NJ): John Wiley & Sons; 2011. [Google Scholar]
- 29.Canadian Medical Association. CMA Policy: Medical assistance in dying. 2017. [accessed 2017 Aug 31]. Available: https://www.cma.ca/Assets/assets-library/document/en/advocacy/policy-research/cma_policy_medical_assistance_in_dying_pd17-03-e.pdf.