Abstract
Background
Since the 1990s, new techniques for the treatment of varicose veins have emerged, including radiofrequency ablation (RFA) and laser treatment. We performed a study to compare the safety, efficacy and outcomes of RFA compared to those of open surgery and laser ablation for the treatment of varicose veins. We also carried out a cost analysis of RFA compared to open surgery to assess whether RFA could help free up operating room time by being performed in an outpatient context.
Methods
We conducted a systematic literature review (publication date May 2010–September 2013 for articles in English, January 1991–September 2013 for those in French). We used several checklists to measure the quality of the studies. We also collected data on costing.
Results
The literature search identified 924 publications, of which 38 were retained for analysis: 15 literature reviews, 1 good-practice guideline and 22 new primary studies. The overall level of evidence was low to moderate owing to the limited sample sizes, lack of information on patient characteristics and lack of standardization of the outcome measures. However, the results obtained are consistent from study to study. In the short and medium term, RFA is considered as effective as open surgery or laser treatment (moderate level of evidence) and presents fewer major and minor complications than open surgery (low level of evidence). Radiofrequency ablation can be performed on an outpatient basis. We calculated that RFA would be about $110–$220 more expensive per patient than open surgery.
Conclusion
Radiofrequency ablation is a valuable alternative to open surgery and would free up operating room time in a context of low accessibility.
Abstract
Contexte
Depuis les années 1990, de nouvelles techniques pour le traitement des varices ont émergé, y compris l’ablation par radiofréquence (ARF) et le traitement au laser. Nous avons procédé à une étude afin de comparer l’innocuité, l’efficacité et les résultats de l’ARF à ceux de la chirurgie ouverte et de l’ablation par laser pour le traitement des varices. Nous avons aussi procédé à une analyse des coûts de l’ARF comparativement à la chirurgie pour vérifier si, en étant effectuée en consultation externe, l’ARF permet de libérer du temps de bloc opératoire.
Méthodes
Nous avons réalisé une revue systématique de la documentation (articles publiés entre mai 2010 et septembre 2013 en langue anglaise, et entre janvier 1991 et septembre 2013 en langue française). Nous avons utilisé plusieurs séries de critères pour mesurer la qualité des études. Nous avons aussi recueilli des données sur l’estimation des coûts.
Résultats
La recherche documentaire a permis de recenser 924 publications, dont 38 ont été retenues pour analyse : 15 examens documentaires, 1 directive de pratique optimale et 22 études principales. Le niveau de preuve global a été jugé de faible à modéré en raison de la taille limitée des échantillons, du manque d’information sur les caractéristiques des patients et de l’absence de normalisation des mesures paramétriques. Toutefois, les résultats obtenus concordent d’une étude à l’autre. À court et à moyen terme, l’ARF est considérée aussi efficace que la chirurgie ouverte ou que le traitement au laser (niveau de preuve modéré) et s’accompagne de moins de complications majeures et mineures que la chirurgie ouverte (faible niveau de preuve). L’ablation par radiofréquence peut être effectuée en consultation externe. Nous avons calculé que l’ARF couterait environ 110 à 220 $ de plus par patient comparativement à la chirurgie.
Conclusion
L’ablation par radiofréquence est une solution de rechange valable à la chirurgie ouverte et pourrait libérer du temps de bloc opératoire dans un contexte d’accès restreint.
Varicose veins affect about 25% of the adult population. The resulting complications are a major cause of morbidity.1–3 Crossectomy with vein stripping is currently the standard technique for treating varicose veins. This technique is invasive, however, and requires a recovery period of several weeks. Since the 1990s, new techniques have emerged, such as radiofrequency ablation (RFA) and laser treatment. These endovascular techniques are performed from the venous lumen without anatomic excision of the pathological vein but lead to its suppression at the pathophysiological level. The radiofrequency technique uses a radiofrequency catheter guided by medical imaging. The catheter heats the vein wall by means of thermal energy delivered by a generator. The rise in temperature causes a destruction of the intima and the media with contraction and thickening of the collagen fibres. These phenomena lead to fibrous changes, gradually leading to remote occlusion of the venous lumen.4 Tumescent local anesthesia is highly recommended for this procedure because, in addition to reducing the burning sensation, it produces a compression effect on the vein (physical hydrostatic compression and compression by spasms induced by the product used), which maximizes the ablative effects of RFA on the vein wall.4 Compared to the first-generation catheter used (ClosurePlus), the second-generation catheter (ClosureFAST), introduced to the market in 2006, produces more heat (85°C v. 120°C) and involves a segmental approach with 20-second cycles. The segmental approach can speed up the procedure and reduce the variability of the heat dosage delivered.
Our establishment is a university-affiliated hospital centre providing specialized and ultraspecialized care to a population of 1 million inhabitants. In addition, it serves as a local hospital for a population of nearly 300 000 inhabitants. Seventy-five operations for varicose veins are practised in our establishment per year, shared between 2 vascular surgeons and several general surgeons. Considering the rates of these procedures per 100 000 inhabitants performed in England and France, based on a local population of 300 000 inhabitants, the potential for operations at our facility is 550–1150 per year.5 De facto, lack of health care delivery in our region for varicose veins has led large numbers of patients to seek treatment in other hospitals or, most often, not to receive any treatment. One of the reasons for the limited health care supply is a shortage of elective and urgent time in the surgical unit leaving no time available to address this problem. It is thus considered that the introduction of RFA in our establishment has the potential to free up operating room time to the extent that it could be performed as an outpatient procedure with fewer staff. Also, the opening of an outpatient clinic for varicose veins could increase the volume of patients and thus reduce the gap between supply and demand, in addition to allowing a rebalancing between the services offered by private and public clinics.
The purpose of this systematic review was to compare the efficacy and security of the RFA technique and subsequent quality of life to those of open surgery and laser treatment. Moreover, we analyzed the utility of RFA in terms of duration of procedures and hospital stay and return to normal activities. Finally, we carried out a cost analysis of RFA compared to open surgery. We consider that such information will be useful for hospitals like ours that plan to perform varicose ablation as an outpatient procedure to overcome the limited availability of the surgical unit and increase the number of patients treated.
Methods
We conducted a systematic literature review combined with administrative data collection. We developed a protocol before the literature search. The search engines used were Embase, CINAHL, the Allied and Complementary Medicine Database, Ovid Healthstar, Ovid MEDLINE, MANTIS, PubMed Central, the Cochrane Database and the Centre for Reviews and Dissemination. We also consulted the websites of the National Institute for Excellence in Health and Social Services, the UK National Institute for Health Research Health Technology Assessment Programme, Joule’s CPG Infobase, BMJ and the Répertoire des recommandations de bonne pratique et de conférences de consensus francophones. Unlike in previous systematic reviews published in the field, we developed a strategy to include both English-language and French-language articles. The reference period for the former was May 2010–September 2013. Studies in English using the first-generation catheter that were published before May 2010 were thus considered through the systematic reviews identified. The reference period for French-language articles was January 1991–September 2013, since these articles were not included in previous reviews. The keywords used for the search were radiofrequency/radiofréquence, varicose/varice, venous insufficiency/insuffisance veineuse, saphenous vein/veine saphène, superficial system/système superficiel, stripping/éveinage and ligature. In PubMed, this gave the following search strategy in English: radiofrequency AND (varicose OR venous insufficiency OR saphenous vein OR superficial system OR stripping OR ligature). Studies identified as being in a language other than English, French, Italian, Spanish, Chinese or Hungarian were excluded.
We selected all studies and reviews of the literature dealing with RFA efficacy, safety, associated quality of life and costs and learning how to use RFA. Single case studies and studies that focused on nonhuman subjects were excluded, as were studies involving subgroups of patients from a larger study. We focused on studies that addressed RFA of varicose veins by distinguishing between the 2 generations of catheter available. Studies that did not use the technology developed by VNUS Medical Technologies for radiofrequency were excluded because this is the only technology authorized by Health Canada. The classification grid used to assess the level of scientific evidence of the studies was that of Hailey and colleagues,6 which classifies studies according to their methodological design, from level I (highest) to level IX (lowest). We then evaluated each study according to the checklist of Downs and Black.7 We assessed literature reviews according to the criteria of the AMSTAR (A Mea-Surement Tool to Assess systematic Reviews) checklist and the AGREE (Appraisal of Guidelines, Research and Evaluation in Europe) Reporting Checklist. The 2 checklists have common characteristics but differ with respect to information collected on contextualization and operationalization of recommendations (AGREE) and research methodology (AMSTAR). We did not carry out a meta-analysis because the included studies showed mixed results and the indicators used are not standardized from one study to another. However, in establishing our conclusions, and in the presence of conflicting results, we gave more weight to studies with a score higher than 50% with either checklist.
To calculate the cost difference between open surgery and RFA in our hospital, we recorded acquisition costs of materials for RFA, the cost of consumables for each intervention and the necessary staff resources. Costs for administrative support, power supply and sterilization were considered identical between RFA and surgery and were not counted. We did not consider any difference related to the duration of the hospital stay since varicose vein surgery in our institution is currently practised in day surgery. The collecting of cost data was done in partnership with the Society of Physicians from the University of Sherbrooke, and purchase costs were provided by Covidien (distributor of VNUS products). No discount rate was retained as the data on costs were collected for the intervention and not for follow-up. The perspective of analysis was that of the health care system in Quebec.
Results
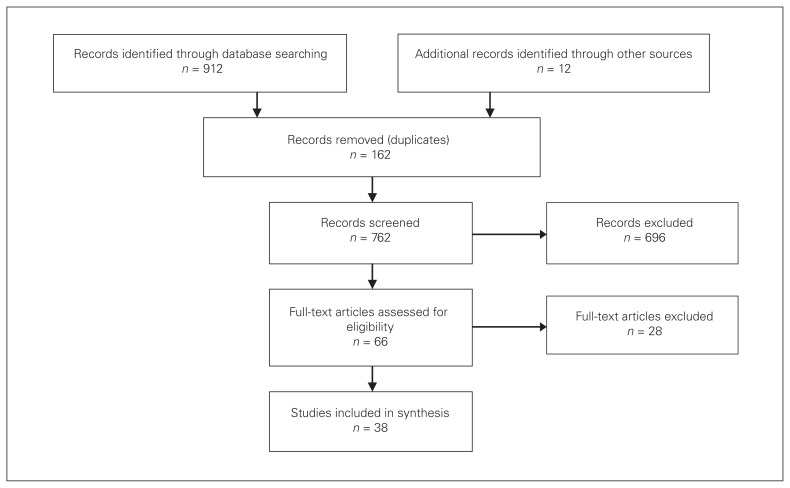
The literature search identified 924 publications, of which 38 were retained for analysis: 15 literature reviews, 1 good-practice guideline and 22 new primary studies. We excluded 4 primary studies in which a competing technology was used (Celon RFITT and Ellman Surgitron) as well as 2 studies each repeated twice.8,9 The other excluded studies involved case studies and technical discussions on the various technologies used. The details of the selection process are provided in Fig. 1.
Fig. 1.
Study selection.
Literature reviews
A summary of the 15 literature reviews and the good-practice guideline identified is presented in Table 1. The first information provided by these reviews is that, despite strong differences in quality, their findings, conclusions and recommendations differ little. Moreover, these reviews, despite their recent publication dates, deal mainly with the first-generation catheter system (ClosurePlus). The second-generation system (ClosureFAST) has been the subject of few studies published before August 2011, the most recent date covered by the literature reviews identified. For example, in the Ontario Medical Advisory Secretariat (MAS) review,20 most studies listed (24/27) evaluated the Closure-Plus system.
Table 1.
Summary of literature reviews on radiofrequency ablation
| Study | Type of review | Period covered | Procedure(s) evaluated | AMSTAR score* | AGREE score, % |
|---|---|---|---|---|---|
| Guias et al.10 | Narrative | NA | RFA, laser, sclerotherapy | 0 | 44.93 |
| Haute Autorité de Santé11 | Systematic | January 1997–March 2008 | RFA | 8 | 85.51 |
| Perrin12 | Narrative | NA | RFA | 0 | 37.68 |
| Uhl5 | Narrative | NA | RFA, laser, foam sclerotherapy | 0 | 23.19 |
| Brar et al.13 | Meta-analysis | 1950–April 2009 | RFA, laser | 7 | 47.83 |
| Gohel et al.14 | Meta-analysis | January 1970–February 2007 | RFA, laser, foam sclerotherapy | 5 | 71.01 |
| Lohr et al.15 | Narrative | NA | RFA | 2 | 42.03 |
| Feliciano et al.16 | Narrative | NA | RFA, laser, foam sclerotherapy | 1 | 34.78 |
| Kundu et al.17 | Narrative | NA | RFA, laser, foam sclerotherapy | 0 | 44.93 |
| Gloviczki et al.18 | Clinical practice guidelines | NA | RFA, laser, foam sclerotherapy | 4 | 82.60 |
| McBride19 | Systematic | NA | RFA, laser, foam sclerotherapy | 5 | 46.40 |
| Medical Advisory Secretariat20 | Systematic | Until March 2010 | RFA | 8 | 81.20 |
| Murad et al.21 | Meta-analysis | Until February 2008 | RFA, laser, foam sclerotherapy | 10 | 69.57 |
| Nesbitt et al.22 | Systematic | Until July 2010 | RFA, laser, foam sclerotherapy | 10 | 72.46 |
| Anwar et al.23 | Narrative | NA | RFA | 1 | 30.43 |
| Siribumrungwong et al.24 | Meta-analysis | 2000–August 2011 | RFA, laser, foam sclerotherapy | 10 | 52.17 |
AGREE = Appraisal of Guidelines, Research and Evaluation in Europe; AMSTAR = A MeaSurement Tool to Assess systematic Reviews; NA = not available; RFA = radiofrequency ablation.
On a scale of 0 to 11.
In the studies identified by these reviews, the majority of participants (60%–90%) were women, and the average age was 45–60 years.20,21 General anesthesia was used almost exclusively in most of the studies. Concomitant phlebectomy was performed in half of the studies, hence the importance of studying radiofrequency of the great saphenous vein under local anesthesia.
In general, the level of evidence was assessed as low to moderate because of small samples, a lack of information on methodology and a lack of subgroup comparisons based on patient characteristics. No study was listed as single- or double-blind.
New primary studies
The main results of the 22 new primary studies are presented in Table 2. Of the 22, 9 were cohort studies or case series, 4 were randomized trials (2 comparing RFA to laser treatment, 1 comparing RFA to open surgery and 1 comparing RFA to laser treatment and foam sclerotherapy), and 9 were controlled trials (4 comparing RFA to laser treatment, 3 comparing RFA to open surgery, 1 comparing RFA to mechanochemical endovenous ablation and 1 comparing the ClosurePlus catheter to the ClosureFAST catheter). Despite differences in quality between the studies, their findings and conclusions are consistent and reinforce the overall level of evidence. The level of evidence was considered low to moderate, for the same reasons as for the literature reviews. Only 1 study was double-blind.25
Table 2.
Summary of primary studies published after April 2010*
| Study | Catheter | Comparison | No. of legs | Anesthesia | No. of cases of deep vein thrombosis | No. of cases of pulmonary embolism | Success rate, % | Hailey et al.6 score† | Downs and Black7 score‡ |
|---|---|---|---|---|---|---|---|---|---|
| Zan et al.26 | ClosurePlus | — | 24 | Local | 0 | 0 | 95.8 postoperatively, 95.8 at 24 mo | VI | 16 |
| García-Madrid et al.27 | ClosurePlus (first 40), ClosureFAST (subsequent) | — | 153 | Local | 0 | 0 | 100 postoperatively, 97 at 12 mo | VIII | 9 |
| Calcagno et al.28 | ClosureFAST | — | 338 | Local | 0 | 0 | 95 postoperatively, 99 at 6 mo | VI | 15 |
| Kapoor et al.29 | ClosureFAST | — | 100 | Local | 0 | — | 100 postoperatively, 97 at 12 mo | VI | 18 |
| Shepherd et al.30 | ClosureFAST | — | 443 | General | — | — | NA | IV | 21 |
| Proebstle et al.31 | ClosureFAST | — | 295 | Local | 0 | 0 | 99.7 postoperatively, 96.3 at 12 mo, 92.6 at 36 mo | IV | 23 |
| Bisang et al.32 | ClosureFAST | — | 232 | Local | 0 | 1 | 94.1 at 12 mo | VI | 20 |
| Choi et al.33 | ClosureFAST | — | 200 | Local and sometimes general | 0 | 0 | 94.6 at 24 mo | VIII | 20 |
| Tolva et al.34 | ClosureFAST | — | 407 | General or epidural | 0 | 0 | 99 at 1 wk and 12 mo | VIII | 13 |
| Eidson et al.35 | NA | v. open surgery | 100 v. 100 | General: 16% v. 95% | — | — | 99 v. NA at 6 mo | V | 17 |
| ElKaffas et al.36 | ClosurePlus | v. open surgery | 90 v. 90 | Local v. general | 0 v. 1 | 0 | 93.3 v. 100 postoperatively; 85.2 v. 90.1 at 24 mo | III | 21 |
| Pisano et al.37 | ClosurePlus | v. open surgery | 107 v. 20 | Epidural or spinal | 0 | 0 | 100 postoperatively, 100 at 60 mo | VI | 10 |
| Park et al.38 | ClosurePlus (initially), ClosureFAST (subsequently) | v. open surgery | 78 v. 194 | Local | 0 | 0 | 76.7 v. 83.9 at 12 mo | V | 22 |
| Rasmussen et al.39 | ClosureFAST | v. open surgery v. laser treatment v. foam sclerotherapy |
148 v. 142 v. 144 v. 144 |
Local | 0 v. 1 v. 0 v. 1 | 0 v. 0 v. 0 v. 1 | 100 v. 96 v. 100 v. 97 postoperatively; 100 v. 97 v. 99 v. 98 at 1 mo; 94 v. 96 v. 93 v. 80 at 12 mo | III | 23 |
| Ravi et al.40 | ClosurePlus | v. laser | 159 v. 2841 | Local | 0 | 96.3 v. 98 postoperatively; NA v. 88.1 at 80 mo | VI | 14 | |
| Gale et al.41 | ClosurePlus | v. laser | 70 v. 72 | Local | 0 v. 1 | — | 100 v. 100 postoperatively; 82.3 v. 96.9 at 12 mo | III | 21 |
| Marsh et al.42 | ClosurePlus | v. laser | 2470 v. 350 | RFA general, laser treatment local | 17 v. 4 | 1 v. 0 | NA | VI | 21 |
| Gandhi et al.43 | ClosureFAST | v. laser | 40 v. 131 | General | — | 0 | NA | VI | 11 |
| Dzieciuchowicz et al.44 | ClosureFAST | v. laser | 43 v. 128 | Local 91% | 0 v. 2 | 0 | 100 v. 98.4 postoperatively; 91 v. 85.9 at 12 mo | IV | 18 |
| Nordon et al.25 | ClosureFAST | v. laser | 79 v. 80 | General | 0 | 0 | 100 v. 100 postoperatively; 97 v. 96 at 3 mo | III | 27 |
| Zuniga et al.45 | ClosurePlus (first 312), ClosureFAST (subsequent) | ClosurePlus v. ClosureFAST | 312 v. 355 | Local | 11 v. 0 | 0 | 88 v. 98 at 1 wk | V | 16 |
| van Eekeren et al.46 | ClosureFAST | v. mechanochemical endovenous ablation | 34 v. 34 | Local | 0 | 0 | NA | IV | 18 |
NA = not available; RFA = radiofrequency ablation.
When the table shows v., the first result concerns RFA; otherwise the results are for RFA only.
On a scale of level I (highest) to level IX (lowest).
On a scale of 0 to 32.
Given the recent publication dates of the new studies selected, many (15/22) reported on the use of the Closure-FAST catheter.
Three studies reported cases classified as CEAP grade 0 or 1 (1%–9% of cases).31,42 46 The remaining studies dealt with cases classified as grade C2 or higher. Patients with grade C2 disease were the most numerous, with the exception of 2 studies in which most had grade C4 disease.40,45 The proportion of patients classified as having grade C5 or C6 disease was generally less than 10%. These data confirm that RFA is quite rarely used to treat patients with no visible varicose veins (grade C0–1) or with venous ulcers (grade C5–6). In studies that compared RFA to open surgery or laser treatment, CEAP classification differences were not significant. Unlike in the studies identified in previous reviews, in most of the new studies, local anesthesia with tumescent solution was used.
Efficacy
There are 3 main performance indicators of RFA: venous occlusion (most common), recanalization and absence of recurrent reflux. Across all studies, the occlusion rates at less than 3 months were usually 93%–100%,11,13,15,25,31,36,37,41 with a weighted average of 98% (weighting was performed according to the number of legs treated in each study). The venous occlusion rate at 6 months was reported as being close to 90% in 4 studies included in the MAS review20 but appeared to be higher in more recent studies, 98.6%–100%,8,26,28,35 for a weighted average of 98.8%. Longer-term follow-up results (≥ 1 yr) were rare. In 2 studies, the occlusion rate after 1 year was 76.7%–100%.37,38 After 24 months, the success rate was 85.2%–95.8%.26,36 Proebstle and colleagues31 reported a success rate of 92.6% at 36 months, and Pisano and colleagues37 indicated a success rate of 100% for follow-up of up to 5 years. In these last 2 studies, the attrition rate at 36 months and 60 months was, however, not provided. The 2010 meta-analysis of Brar and colleagues13 indicated an occlusion rate of 87.9% at 2 years. Another study reported in the MAS review,20 by the Closure Study Group,47 indicated an occlusion rate of 88.2% after 2 years and 83.8% after 5 years. Overall, the recent studies suggest better average results with the ClosureFAST catheter than with the ClosurePlus catheter after 1 year and 2 years (95 v. 87% and 94.5 v. 85.2%, respectively).
Treatment efficacy with RFA compared to open surgery, defined by absence of the vein (surgery) or occlusion thereof (RFA), appeared to be relatively similar in all studies reviewed.13,14,20–22,36,39 It should be noted that this comparison was carried out for follow-up of up to 1 or 2 years. The efficacy data at 5 years are not convincing for RFA (few patients, high proportions of patients lost to follow-up), so we were unable to compare results with those of surgery.
The various studies comparing RFA to laser treatment were carried out with lasers using different wavelengths, which limits the scope of the results. Reported efficacy varied, with some studies indicating better results with RFA than with laser treatment after 1 year or less and some not.18,20,25,39,41,44 No results are available for longer follow-up apart from indirect comparison in the meta-analysis of Brar and colleagues,13 which indicated a 2-year occlusion rate of 87.9% with RFA (first-generation catheter), compared to 91.5% with laser treatment.
Complications
We used the definition of various types of adverse events given by the Society of Interventional Radiology and the Society of Vascular Surgery.48 Major adverse events included deep vein thrombosis (DVT), pulmonary embolism, infection, nerve damage and skin burns. Other events requiring additional treatment or hospital admission are also considered major adverse events. All other events are considered minor adverse events.
Major complications
Complications were not systematically reported in the studies identified by the previous reviews, and none reported relative risk. The reporting rate is often less than 50%.11 In the newer primary studies, this rate is over 86%. According to the MAS review, the major complication rate in cohort studies is 2.9% (105/3664) with RFA.20 This rate includes cases of DVT (1.8%), infection (0.4%), skin burns (0.3%), nerve damage (0.3%) and pulmonary embolism (0.03%). With the exception of the study by Marsh and colleagues42 involving 2470 patients treated with RFA, with a DVT rate of 0.7%, and the study by Zuniga and colleagues45 reporting on DVT only for first-generation catheters (3.5%), none of the other studies indicated the presence of DVT. Similarly, only 2 studies indicated pulmonary embolism (1.4% [1/73]32 and 0.04% [1/2470]42). Only 1 study indicated skin burns: 1.3% of patients treated with RFA had this complication, compared to 2.6% of those who received laser treatment.25 No cases of neurologic injury were mentioned, and infections were rarely mentioned.
In the studies listed by the MAS20 that compared RFA to surgery, the overall rate of major complications was 6.3% (9/142) in the RFA group and 11.3% (17/150) in the open-surgery group. None of the 6 comparative studies listed, however, indicated DVT or pulmonary embolism. In the newer comparative studies, rates of 0%–3.5% were reported for DVT with RFA (ClosurePlus).36,39,41,42,44 These same studies indicated DVT rates for surgery and laser treatment of 0%–1.6%. The meta-analysis of Brar and colleagues13 nonetheless showed that DVT was more frequent with RFA than with laser treatment (1.3% v. 0.2%). The newer studies indicate a pulmonary embolism rate of 0.07% (2/2735) with RFA, 0% (0/110) with open surgery and 0% (0/502) with laser treatment. Skin burns are present only with RFA and laser treatment and are generally avoided thanks to local anesthesia by tumescence. Merchant and colleagues47 reported a decrease in the burn rate from 1.8% to 0.5% after its introduction. Contrary to Nordon and colleagues, 25 Brar and colleagues13 indicated that burns are more common with RFA than with laser treatment (1.3% v. 2.6% and 1.1% v. 0.5%, respectively). This difference is due to the use of second-generation catheters in the study by Nordon and colleagues.25 Surgery, however, is more implicated in infections and nerve damage than RFA or laser treatment.13,49 According to Perrin,12 infections and lymphatic complications have completely disappeared with endoluminal procedures. In fact, several investigators report having observed no infections following treatment with RFA.25,29,36,37 In contrast, ElKaffas and colleagues36 reported an infection rate of 3.3% with open surgery.
Ultimately, it appears that the risk of DVT or pulmonary embolism is relatively comparable between RFA, surgery and laser treatment (particularly with the use of second-generation catheters) (Table 3). However, RFA may allow better results than laser treatment regarding skin burns, particularly with the use of the second-generation catheter. It may also give better results than surgery with regard to infection.
Table 3.
Comparison of the occurrence of major and minor complications between radiofrequency ablation, open surgery and laser treatment
| Complication | RFA v. surgery | RFA v. laser treatment |
|---|---|---|
| Major | RFA < surgery | RFA = laser treatment |
| Deep vein thrombosis | RFA = surgery | RFA = laser treatment |
| Pulmonary embolism | RFA = surgery | RFA = laser treatment |
| Infection | RFA < surgery | RFA = laser treatment |
| Nerve damage | RFA < surgery | RFA = laser treatment |
| Skin burns | RFA > surgery | RFA < laser treatment |
| Minor | RFA < surgery | RFA < laser treatment |
| Thrombophlebitis | RFA > surgery | RFA < laser treatment |
| Hematomas | RFA < surgery | RFA < laser treatment |
| Bruising | RFA < surgery | RFA < laser treatment |
| Paresthesia | RFA > surgery | RFA > laser treatment |
| Pain | RFA < surgery | RFA < laser treatment |
RFA = radiofrequency ablation.
Minor complications
Minor complications such as swelling, inflammation, paresthesia, bruising, hematoma and pain in the legs are relatively common after RFA.13,19,38 However, it is not clear whether all of these complications are attributable to RFA, because in most studies it is carried out with concomitant procedures such as phlebectomy.
Overall, analysis of the studies indicates that RFA leads to less pain, contusion and hematoma than surgery and less bruising than laser treatment (Table 3). However, the paresthesia rate is higher with RFA than with surgery or laser treatment. Few comparative studies have been conducted on the topic of minor complications; nevertheless, the level of evidence for these findings remains low.
Duration of procedure, hospital admission, and return to normal activities and work
Earlier studies showed the average duration of the procedure was longer with RFA than with surgery (83.6 [standard deviation (SD) 14.5] min v. 55.7 (SD 10.9) min) (p < 0.001).20 With the ClosureFAST catheter and anesthesia with tumescence, ElKaffas and colleagues36 reported a shorter time with RFA (40 [SD 12] min) than with surgery (45 [SD 13] min) (p = 0.04). Similarly, Nordon and colleagues25 did not find any difference between RFA and laser treatment (30 min each). In the study by Dzieciuchowicz and colleagues,44 there was no difference between RFA and laser treatment in procedure time (average 98 min for both) or the duration of convalescence in the recovery ward (average 200 min for both). A reduction in procedure time was observed between the 2 generations of catheter. Zuniga and colleagues45 reported a duration of 18–22 minutes with the ClosurePlus catheter and 5 minutes with the ClosureFAST catheter for a 45-cm vein.
In the study by Proebstle and colleagues,50 the corresponding times were 41 and 16.4 minutes for a 37-cm vein. In studies that indicated the length of hospital stay, this was often less than 1 day with RFA. A significantly shorter hospital stay with RFA than with surgery was reported (0.03 d v. 0.82 d [p < 0.001] and 0.6 d v. 1.25 d [p = 0.01], respectively).35,36 With the exception of 16% of RFA cases in the study by Eidson and colleagues,35 surgery was performed under general anesthesia, whereas RFA was not.
The time required to return to normal activities and work was, on average, 1 week shorter with RFA than with open surgery.13,18,20 The time required to return to normal activities appears to be highly influenced by the type of anesthesia. Studies in which tumescent local anesthesia was practised indicated that return to normal activities was often on the same day,27,29,37,39 whereas a hospital stay of 6–7 days was reported with general anesthesia.20 This time difference is also due to the more invasive nature of surgery compared to RFA.51,52 The time required before going back to work was generally shorter with RFA than with surgery or laser treatment.39,51
Overall, RFA allows a shorter hospital stay and a faster return to normal activities and work than surgery or laser treatment. Contrary to what had been observed in studies published before May 2010, it now appears that procedures are faster with RFA and laser treatment than with surgery.
Quality of life, pain and satisfaction
In all studies that provided data in this area, there was significant resolution of venous symptoms (Venous Clinical Severity Score, CEAP) and improvement in quality of life from baseline, regardless of the treatment used.19,32,46 The improvement in the perioperative period was better with RFA than with open surgery;18,19,21 however, this difference disappeared after a few weeks. Gale and colleagues41 reported no significant difference in improvement in quality of life between RFA and laser treatment. The meta-analysis by Gohel and colleagues14 showed identical gains in quality-adjusted life-years over 5 years between RFA, surgery and laser treatment (3.9 quality-adjusted life-years).
RFA was reported to be less painful than surgery.13,19,38 Similarly, pain was less with RFA than with laser treatment in the 2 weeks following treatment,25,53 but this difference then disappeared.18,20
Finally, patient satisfaction was higher with RFA than with surgery.20,21,35,37 No evidence was reported regarding a comparison with laser treatment.41
Costs
The cost of treatment with RFA was reported to be higher than that for surgery.20,36,54,55 For example, the MAS review indicated a cost of $2029 for RFA versus $1799 for surgery.20 However, if one takes into account the shorter period required before returning to work with RFA, the costs to society with RFA are lower than with surgery.36,56 The main problem of cost for RFA lies in the selling price of the catheter, which is about €500 (Can$650).10
Goode and colleagues57 found that only 55% of patients were suitable for and could benefit from RFA. In our institution, 75 open surgical procedures for varicose veins are carried out annually, and patients stay an average of 1 day. The introduction of RFA in our establishment would thus free up some 40 time slots in the operating block (0.55 × 75). These additional time slots would make it possible to treat other patients with venous insufficiency or those in need of treatment in another medical specialty. For this to be feasible, treatment with RFA should be performed in an annex room in the surgery department under tumescent local anesthesia, thus reducing waiting times previously lengthened by the lack of availability of the operating room and increasing the volume of treated patients.
The cost of the generator is $27 500 (option 1). This generator can, however, be lent via an agreement for purchase of supplies for a period of 5 years and would become the property of the hospital once 200 catheters have been purchased (option 2). The price of consumables is $800–$830 per procedure; this includes the disposable catheter, the microinductor kit, the procedure equipment, the tumescent infiltration kit and the guide for the catheter. The cost of a Doppler ultrasonography machine was excluded because it would be loaned by the medical imaging service. If this were not the case, a purchase price of $100 000 would be expected. A minimum of 40 patients per year is expected over a period of 5 years. The cost of consumables for open surgery is $210 (including $9 for the medication). The most recent study comparing operating time between RFA (outpatient) and open surgery showed that they are comparable.36 In our institution, the average time for surgery in the operating room is about 2.5 hours. We therefore used this time for our cost calculations. Human resources costs for RFA are thus $528 (including payment of the physician, and payroll taxes and fringe benefits for employees), compared to $1040 for open surgery.
The sum of these costs is $1358–$1465.50 for RFA and $1250 for open surgery (Table 4). From a societal point of view, if we consider that RFA allows a faster return to work, the additional costs of $110–$220 are cancelled out when the time difference exceeds 2 days, which is quite often the case, as found in our literature review.
Table 4.
Costs per patient for radiofrequency ablation versus open surgery
| Cost component | Cost, 2013 Canadian dollars | ||
|---|---|---|---|
| RFA option 1: immediate acquisition of generator | RFA option 2: acquisition of generator via catheter purchase | Open surgery | |
| Depreciation over 5 yr | 137.50* | — | — |
| Supplies | 800.00 | 830.00 | 210.00 |
| Human resources | 528.00† | 528.00† | 1040.00‡ |
| Total | 1465.50 | 1358.00 | 1250.00 |
RFA = radiofrequency ablation.
Generator.
One vascular surgeon, 1 resident, 1 radiology technician, 1 nurse.
One vascular surgeon, 1 anesthetist, 2 residents, 2 nurses, 1 respiratory therapist, 1 porter.
Discussion
Results reported in this systematic review of the literature indicate that RFA of varicose veins is a valuable alternative to open surgery. The safety of the procedure is proven by the low complication rate (comparable to or lower than that for surgery), and its clinical efficacy appears to be similar to that of open surgery.18,20 Moreover, radiofrequency allows ablation under tumescent local anesthesia, which means that the procedure can be performed on an outpatient basis. This technique is less invasive and causes less pain for the patient than open surgery. Finally, the period required before return to normal activities is significantly shorter with RFA than with surgery. It is also noteworthy that all cases of DVT associated with RFA occurred during procedures with the first-generation catheter and that, after the introduction of the ClosureFAST catheter, no cases of DVT were identified. This might be related to a change in practice, because with the ClosureFAST catheter ablation now begins 2 cm from the saphenofemoral junction, compared to 1 cm before.45
Although the studies we analyzed all indicated that RFA is safe and effective, their methodology was not always of good quality. A relatively large number of biases were therefore identified, and the diversity of indicators used made their comparison difficult. Indeed, in their review, Thakur and colleagues58 listed no fewer than 31 different indicators for 28 randomized studies of endovenous interventions for varicose veins (cryostripping, sclerotherapy, laser treatment and RFA) as well as the use of 13 validated quality-of-life questionnaires, 30 types of complications and 38 time points for measuring recurrence (from 3 wk to 10 yr). We observed similar diversity in our review, perhaps reinforced by our strategy to consider all types of study designs except single case studies (based on work indicating that randomized studies do not provide all the evidence and are not always of better quality than nonrandomized studies59,60). Outcome measures most frequently used were rate of occlusion, rate of recanalization and absence of reflux. These indicators may appear similar; however, their measurement could lead to divergences, particularly regarding absence of reflux. Furthermore, some investigators reported their results as rates per patient, whereas others did so as rates per treated leg, which introduces a problem of consistency. Similarly, the heterogeneity of follow-up periods prevents adequate comparison of treatments. In the study by ElKaffas and colleagues, 36 recurrence occurred between 21 and 24 months (mean duration of follow-up 20.9 mo) for both RFA and surgery. Consequently, it appears difficult to judge the recurrence rate with less than 24 months of follow-up. In this regard, Kundu and colleagues48 recommended standard follow-up at 3 days, 1 month, 1 year and then annually. All these indicators prevented us from performing a meta-analysis owing to the high heterogeneity in results.
Another problem we encountered was the lack of information on the demographic characteristics of patients and the severity of their venous problems. Factors such as body mass index and type of occupation are risk factors affecting the complications that may occur following treatment of varicose veins, such as infections.61,62 Similarly, the CEAP grade was not always reported or insufficient details were given, with some categories being grouped together. Better description of the prevalence of different stages of chronic venous insufficiency in study populations is important, however, because CEAP grade can be associated with limitations or counterindications to the type of treatment offered. There was also very little information on the diameter, length and location of the treated veins, which can seriously affect the efficacy of the procedure, particularly for endovenous treatments. In many cases, details of inclusion and exclusion criteria were sparse or absent, which made it impossible to thoroughly analyze the results and identify factors contributing to success or failure. Finally, the imbalance in group size may suggest some expertise in or preference for a certain procedure and may have skewed the results.
The characteristics of the procedures were also not well reported. In fact, some studies did not detail the type of catheter used for RFA or, in the case of the ClosurePlus catheter, the catheter withdrawal rate. The fact that phlebectomy was performed in some cases but not in others skews the results on pain, quality of life and time required before returning to normal activities. This issue also hinders comparison of the effect of 2 treatments on these indicators and when randomization has been conducted between the 2 legs of the same patient. Furthermore, no information is generally available on the number of operators performing the procedure and their training and experience. It is also not known whether the operator and the specialist who evaluated the success of the treatment were the same person. In general, it seems there is no blind testing of treatment outcomes, which would have been easily achieved in most of the studies; this limits the validity of the results presented.
Overall, the quality of studies on RFA appears limited by all these biases, which prevents us from making a robust conclusion. Nevertheless, considering the consistency of the results obtained, it is likely that RFA continues to be regarded as effective and safe. The level of evidence showing comparable efficacy of RFA and open surgery is considered moderate, as is the evidence with regard to the reduced time required before returning to normal activities after RFA compared to open surgery. On the other hand, regarding the rate of major and minor complications, the level of evidence that RFA is safer is considered low.
Limitations
A limitation of our study is that additional publications on RFA have been published since we completed our review, in 2014. However, these new publications do not present results different from those presented here with the VNUS technology.63–66 Indeed, these studies indicate that RFA is a safe procedure with minimal complications and with a clinical efficacy similar to that of open surgery. Importantly, one of the few studies with 5-year results indicates that RFA maintains occlusion rates of 91.9% and freedom from reflux in 94.9% of legs.64 Such rates are similar to and even better than those reported for open surgery in Table 2. Another limit is that the price system used to calculate the cost of RFA and open surgery in our hospital may be different from that used in other hospital settings. However, we are confident that the cost difference between the 2 treatments would remain small in other hospitals since RFA and open surgery for varicose veins are highly standardized procedures. Considering the small volume of patients undergoing varicose surgery in our hospital, the cost difference of about $110–$220 would likely be smaller in hospitals with higher volume, since these hospitals may have the opportunity to negotiate a better price for RFA consumables. For example, in 2016, Aherne and colleagues63 indicated a cost difference of only €53 (about Can$80 in 2016) (€971 v. €1024) in favour of open surgery with a higher volume of patients. Finally, our conclusions are similar to those formulated in international guidelines for the management of varicose veins.67–69 In particular, in the 2 most recent guidelines,68,69 the efficacy of RFA is considered to be similar to that of open surgery, with fewer complications.
Conclusion
Although the quality of the studies that we analyzed was highly variable and the overall quality was considered to be moderate, our literature review confirms that RFA is as safe and effective as open surgery or laser treatment in the short and medium term. In particular, RFA has the advantage of being less painful, presenting fewer minor complications and promoting a rapid return to normal activities following a reduced recovery time compared to open surgery.18,19 In addition, the introduction of the second-generation catheter on the market has allowed better control of the radiofrequency procedure, reducing its duration and increasing its efficacy.18,20,45 However, a lack of evidence prevents us from making a judgment regarding the superior efficacy of RFA in the long term compared to other treatments.
In the context of Quebec and the rest of Canada, the introduction of RFA is a valuable option, especially if introduced on an outpatient basis. Radiofrequency ablation would allow our hospital to free up 40 operating theatre slots, and the additional cost of $110–$220 per patient would be due mainly to the cost of consumables since RFA requires half the staff as does open surgery.
Footnotes
Competing interests: None declared.
Contributors: T. Poder, S. Bédard and M.-A. Despatis designed the study. T. Poder, J.-F. Fisette and S. Bédard acquired the data, which all authors analyzed. T. Poder wrote the article, which all authors reviewed and approved for publication.
References
- 1.Callam MJ. Epidemiology of varicose veins. Br J Surg. 1994;81:167–73. doi: 10.1002/bjs.1800810204. [DOI] [PubMed] [Google Scholar]
- 2.Evans CJ, Allan PL, Lee AJ, et al. Prevalence of venous reflux in the general population on duplex scanning: the Edinburgh Vein Study. J Vasc Surg. 1998;28:767–76. doi: 10.1016/s0741-5214(98)70051-5. [DOI] [PubMed] [Google Scholar]
- 3.Adhikari A, Criqui MH, Wooll V, et al. The epidemiology of chronic venous diseases. Phlebology. 2000;15:2–18. [Google Scholar]
- 4.Perrin M. Traitement chirurgical endovasculaire des varices des membres inférieurs. Techniques et résultats. Tech Chir Chir Vasc. 2007;43(161 C) doi: 10.1016/S0246-0459(07)43331-7. [DOI] [Google Scholar]
- 5.Uhl JF. Les nouvelles stratégies thérapeutiques pour la chirurgie des varices des membres inférieurs. Emem Acad Natl Chir. 2009;8:12–22. [Google Scholar]
- 6.Hailey D, Roine R, Ohinmaa A. Systematic review of evidence for the benefits of telemedicine. J Telemed Telecare. 2002;8(Suppl 1):1–30. doi: 10.1258/1357633021937604. [DOI] [PubMed] [Google Scholar]
- 7.Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52:377–84. doi: 10.1136/jech.52.6.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Creton D, Pichot O, Sessa C, et al. ClosureFast Europe Group. Radiofrequency-powered segmental thermal obliteration carried out with the ClosureFast procedure: results at 1 year. Ann Vasc Surg. 2010;24:360–6. doi: 10.1016/j.avsg.2009.09.019. [DOI] [PubMed] [Google Scholar]
- 9.García-Madrid C, Manrique JÓP, Sánchez VA, et al. Endovenous radiofrequency ablation (Venefit procedure): impact of different energy rates on great saphenous vein shrinkage. Ann Vasc Surg. 2013;27:314–21. doi: 10.1016/j.avsg.2012.06.015. [DOI] [PubMed] [Google Scholar]
- 10.Guias B, Desnos CH, Gouny P, et al. Varices essentielles : orientations thérapeutiques en 2005 ? Med Ther. 2005;11:108–16. [Google Scholar]
- 11.Occlusion de grande veine saphène par radiofréquence par voie veineuse transcutanée. Saint-Denis La Plaine (France): Service évaluation des actes professionnels, Haute Autorité de Santé; 2008. [accessed 2018 Jan 2]. Available: www.has-sante.fr/portail/upload/docs/application/pdf/2008-07/synthese_radiofrequence_saphene_vd.pdf. [Google Scholar]
- 12.Perrin MR. Traitement des varices par la radiofréquence. Sang Thromb Vaiss. 2008;20:166–82. [Google Scholar]
- 13.Brar R, Nordon IM, Hinchliffe RJ, et al. Surgical management of varicose veins: meta-analysis. Vascular. 2010;18:205–20. doi: 10.2310/6670.2010.00013. [DOI] [PubMed] [Google Scholar]
- 14.Gohel MS, Epstein DM, Davies AH. Cost-effectiveness of traditional and endovenous treatments for varicose veins. Br J Surg. 2010;97:1815–23. doi: 10.1002/bjs.7256. [DOI] [PubMed] [Google Scholar]
- 15.Lohr J, Kulwicki A. Radiofrequency ablation: evolution of a treatment. Semin Vasc Surg. 2010;23:90–100. doi: 10.1053/j.semvascsurg.2010.01.004. [DOI] [PubMed] [Google Scholar]
- 16.Feliciano BA, Dalsing MC. Varicose vein: current management. Adv Surg. 2011;45:45–62. doi: 10.1016/j.yasu.2011.03.005. [DOI] [PubMed] [Google Scholar]
- 17.Kundu S, Modabber M. Endovenous ablation for the treatment of varicose veins and lower extremity venous insufficiency. J Radiol Nurs. 2011;30:36–42. [Google Scholar]
- 18.Gloviczki P, Comerota AJ, Dalsing MC, et al. The care of patients with varicose veins and associated chronic venous diseases: clinical practice guidelines of the Society for Vascular Surgery and the American Venous Forum. J Vasc Surg. 2011;53:2S–48S. doi: 10.1016/j.jvs.2011.01.079. [DOI] [PubMed] [Google Scholar]
- 19.McBride KD. Changing to endovenous treatment for varicose veins: How much more evidence is needed? Surgeon. 2011;9:150–9. doi: 10.1016/j.surge.2010.11.002. [DOI] [PubMed] [Google Scholar]
- 20.Ontario Health Technology Assessment Series. 1. Vol. 11. Toronto: Medical Advisory Secretariat, Ministry of Health and Long-Term Care; 2011. [accessed 2018 Jan 2]. Endovascular radiofrequency ablation for varicose veins: an evidence-based analysis. Available: www.hqontario.ca/Portals/0/Documents/evidence/reports/rev_rfa_vv_20110216.pdf. [PMC free article] [PubMed] [Google Scholar]
- 21.Murad MH, Coto-Yglesias F, Zumaeta-Garcia M, et al. A systematic review and meta-analysis of the treatments of varicose veins. J Vasc Surg. 2011;53(Suppl):49S–65S. doi: 10.1016/j.jvs.2011.02.031. [DOI] [PubMed] [Google Scholar]
- 22.Nesbitt C, Eifell RK, Coyne P, et al. Endovenous ablation (radiofrequency and laser) and foam sclerotherapy versus conventional surgery for great saphenous vein varices. Cochrane Database Syst Rev. 2011;(10):CD005624. doi: 10.1002/14651858.CD005624.pub2. [DOI] [PubMed] [Google Scholar]
- 23.Anwar MA, Lane TR, Davies AH, et al. Complications of radiofrequency ablation of varicose veins. Phlebology. 2012;27(Suppl 1):34–9. doi: 10.1258/phleb.2012.012s21. [DOI] [PubMed] [Google Scholar]
- 24.Siribumrungwong B, Noorit P, Wilasrusmee C, et al. A systematic review and meta-analysis of randomised controlled trials comparing endovenous ablation and surgical intervention in patients with varicose vein. Eur J Vasc Endovasc Surg. 2012;44:214–23. doi: 10.1016/j.ejvs.2012.05.017. [DOI] [PubMed] [Google Scholar]
- 25.Nordon IM, Hinchliffe RJ, Brar R, et al. A prospective double-blind randomized controlled trial of radiofrequency versus laser treatment of the great saphenous vein in patients with varicose veins. Ann Surg. 2011;254:876–81. doi: 10.1097/SLA.0b013e318230af5a. [DOI] [PubMed] [Google Scholar]
- 26.Zan S, Contessa L, Varetto G, et al. Radiofrequency minimally invasive endovascular treatment of lower limbs varicose veins: clinical experience and literature review. Minerva Cardioangiol. 2007;55:443–58. [PubMed] [Google Scholar]
- 27.García-Madrid C, Manrique JÓP, Gómez Blasco FG, et al. New advances in the treatment of varicose veins: endovenous radiofrequency VNUS Closure® [article in Spanish] Cir Esp. 2011;89:420–6. doi: 10.1016/j.ciresp.2011.04.010. [DOI] [PubMed] [Google Scholar]
- 28.Calcagno D, Rossi JA, Ha C. Effect of saphenous vein diameter on closure rate with ClosureFAST radiofrequency catheter. Vasc Endovascular Surg. 2009;43:567–70. doi: 10.1177/1538574409345026. [DOI] [PubMed] [Google Scholar]
- 29.Kapoor A, Mahajan G. Endovenous ablation of saphenofemoral insufficiency: analysis of 100 patients using RF ClosureFast technique. Indian J Surg. 2010;72:458–62. doi: 10.1007/s12262-010-0160-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shepherd AC, Gohel MS, Lim CS, et al. A study to compare disease-specific quality of life with clinical anatomical and hemodynamic assessments in patients with varicose veins. J Vasc Surg. 2011;53:374–82. doi: 10.1016/j.jvs.2010.09.022. [DOI] [PubMed] [Google Scholar]
- 31.Proebstle TM, Alm J, Gockeritz O, et al. Three-year European follow-up of endovenous radiofrequency-powered segmental thermal ablation of the great saphenous vein with or without treatment of calf varicosities. J Vasc Surg. 2011;54:146–52. doi: 10.1016/j.jvs.2010.12.051. [DOI] [PubMed] [Google Scholar]
- 32.Bisang U, Meier TO, Enzler M, et al. Results of endovenous ClosureFast treatment for varicose veins in an outpatient setting. Phlebology. 2012;27:118–23. doi: 10.1258/phleb.2010.010089. [DOI] [PubMed] [Google Scholar]
- 33.Choi JH, Park HC, Joh JH. The occlusion rate and patterns of saphenous vein after radiofrequency ablation. J Korean Surg Soc. 2013;84:107–13. doi: 10.4174/jkss.2013.84.2.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tolva VS, Cireni LV, Bianchi PG, et al. Radiofrequency ablation of the great saphenous vein with the ClosureFAST procedure: mid-term experience on 400 patients from a single centre. Surg Today. 2012;43:741–4. doi: 10.1007/s00595-012-0296-4. [DOI] [PubMed] [Google Scholar]
- 35.Eidson JL, Atkins MD, Bohannon WT, et al. Economic and outcomes-based analysis of the care of symptomatic varicose veins. J Surg Res. 2011;168:5–8. doi: 10.1016/j.jss.2010.12.027. [DOI] [PubMed] [Google Scholar]
- 36.ElKaffas KH, ElKashef O, ElBaz W. Great saphenous vein radiofrequency ablation versus standard stripping in the management of primary varicose veins — a randomized clinical trial. Angiology. 2011;62:49–54. doi: 10.1177/0003319710380680. [DOI] [PubMed] [Google Scholar]
- 37.Pisano IP, Pala C, Scognamillo F, et al. Endovenous radiofrequency obliteration of the saphenous veins in the treatment of venous insufficiency of lower legs. Our experience [article in Italian] Ann Ital Chir. 2008;79:193–6. [PubMed] [Google Scholar]
- 38.Park HS, Kwon Y, Eom BW, et al. Prospective nonrandomized comparison of quality of life and recurrence between high ligation and stripping and radiofrequency ablation for varicose veins. J Korean Surg Soc. 2013;84:48–56. doi: 10.4174/jkss.2013.84.1.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rasmussen LH, Lawaetz M, Bjoern L, et al. Randomized clinical trial comparing endovenous laser ablation, radiofrequency ablation, foam sclerotherapy and surgical stripping for great saphenous varicose veins. Br J Surg. 2011;98:1079–87. doi: 10.1002/bjs.7555. [DOI] [PubMed] [Google Scholar]
- 40.Ravi R, Trayler EA, Barrett DA, et al. Endovenous thermal ablation of superficial venous insufficiency of the lower extremity: single-center experience with 3000 limbs treated in a 7-year period. J Endovasc Ther. 2009;16:500–5. doi: 10.1583/09-2750.1. [DOI] [PubMed] [Google Scholar]
- 41.Gale SS, Lee JN, Walsh ME, et al. A randomized, controlled trial of endovenous thermal ablation using the 810-nm wavelength laser and the ClosurePLUS radiofrequency ablation methods for superficial venous insufficiency of the great saphenous vein. J Vasc Surg. 2010;52:645–50. doi: 10.1016/j.jvs.2010.04.030. [DOI] [PubMed] [Google Scholar]
- 42.Marsh P, Price BA, Holdstock J, et al. Deep vein thrombosis (DVT) after venous thermoablation techniques: rates of endovenous heat-induced thrombosis (EHIT) and classical DVT after radiofrequency and endovenous laser ablation in a single centre. Eur J Vasc Endovasc Surg. 2010;40:521–7. doi: 10.1016/j.ejvs.2010.05.011. [DOI] [PubMed] [Google Scholar]
- 43.Gandhi A, Froghi F, Shepherd AC, et al. A study of patient satisfaction following endothermal ablation for varicose veins. Vasc Endovascular Surg. 2010;44:274–8. doi: 10.1177/1538574410363834. [DOI] [PubMed] [Google Scholar]
- 44.Dzieciuchowicz Ł, Krasinski Z, Gabriel M, et al. A prospective comparison of four methods of endovenous thermal ablation. Pol Przegl Chir. 2011;83:597–605. doi: 10.2478/v10035-011-0095-4. [DOI] [PubMed] [Google Scholar]
- 45.Zuniga JM, Hingorani A, Ascher E, et al. Short-term outcome analysis of radiofrequency ablation using ClosurePlus vs ClosureFast catheters in the treatment of incompetent great saphenous vein. J Vasc Surg. 2012;55:1048–51. doi: 10.1016/j.jvs.2011.11.050. [DOI] [PubMed] [Google Scholar]
- 46.van Eekeren RR, Boersma D, Konijn V, et al. Postoperative pain and early quality of life after radiofrequency ablation and mechanochemical endovenous ablation of incompetent great saphenous veins. J Vasc Surg. 2013;57:445–50. doi: 10.1016/j.jvs.2012.07.049. [DOI] [PubMed] [Google Scholar]
- 47.Merchant RF, Pichot O Closure Study Group. Long-term outcomes of endovenous radiofrequency obliteration of saphenous reflux as a treatment for superficial venous insufficiency. J Vasc Surg. 2005;42:502–9. doi: 10.1016/j.jvs.2005.05.007. discussion 509. [DOI] [PubMed] [Google Scholar]
- 48.Kundu S, Lurie F, Millward SF, et al. Recommended reporting standards for endovenous ablation for the treatment of venous insufficiency: joint statement of the American Venous Forum and the Society of Interventional Radiology. J Vasc Surg. 2007;46:582–9. doi: 10.1016/j.jvs.2007.05.025. [DOI] [PubMed] [Google Scholar]
- 49.Morrison C, Dalsing MC. Signs and symptoms of saphenous nerve injury after greater saphenous vein stripping: prevalence, severity, and relevance for modern practice. J Vasc Surg. 2003;38:886–90. doi: 10.1016/s0741-5214(03)00790-0. [DOI] [PubMed] [Google Scholar]
- 50.Proebstle TM, Vago B, Alm J, et al. Treatment of the incompetent great saphenous vein by endovenous radiofrequency powered segmental thermal ablation: first clinical experience. J Vasc Surg. 2008;47:151–6. doi: 10.1016/j.jvs.2007.08.056. [DOI] [PubMed] [Google Scholar]
- 51.Shepherd AC, Gohel MS, Lim CS, et al. Pain following 980-nm endovenous laser ablation and segmental radiofrequency ablation for varicose veins: a prospective observational study. Vasc Endovasc Surg. 2010;44:212–6. doi: 10.1177/1538574409359337. [DOI] [PubMed] [Google Scholar]
- 52.Shepherd AC, Gohel MS, Lim CS, et al. The treatment of varicose veins: an investigation of patient preferences and expectations. Phlebology. 2010;25:54–65. doi: 10.1258/phleb.2009.009008. [DOI] [PubMed] [Google Scholar]
- 53.Shepherd AC, Gohel MS, Brown LC, et al. Randomized clinical trial of VNUS ClosureFAST radiofrequency ablation versus laser for varicose veins. Br J Surg. 2010;97:810–8. doi: 10.1002/bjs.7091. [DOI] [PubMed] [Google Scholar]
- 54.Rautio T, Ohinmaa A, Perala J, et al. Endovenous obliteration versus conventional stripping operation in the treatment of primary varicose veins: a randomized controlled trial with comparison of the costs. J Vasc Surg. 2002;35:958–65. doi: 10.1067/mva.2002.123096. [DOI] [PubMed] [Google Scholar]
- 55.Subramonia S, Lees T. Radiofrequency ablation vs conventional surgery for varicose veins — a comparison of treatment costs in a randomised trial. Eur J Vasc Endovasc Surg. 2010;39:104–11. doi: 10.1016/j.ejvs.2009.09.012. [DOI] [PubMed] [Google Scholar]
- 56.Perala J, Rautio T, Biancari F, et al. Radiofrequency endovenous obliteration versus stripping of the long saphenous vein in the management of primary varicose veins: 3-year outcome of a randomized study. Ann Vasc Surg. 2005;19:669–72. doi: 10.1007/s10016-005-6613-2. [DOI] [PubMed] [Google Scholar]
- 57.Goode SD, Kuhan G, Altaf N, et al. Suitability of varicose veins for endovenous treatments. Cardiovasc Intervent Radiol. 2009;32:988–91. doi: 10.1007/s00270-009-9616-5. [DOI] [PubMed] [Google Scholar]
- 58.Thakur B, Shalhoub J, Hill AM, et al. Heterogeneity of reporting standards in randomised clinical trials of endovenous interventions for varicose veins. Eur J Vasc Endovasc Surg. 2010;40:528–33. doi: 10.1016/j.ejvs.2010.06.018. [DOI] [PubMed] [Google Scholar]
- 59.Benson K, Hartz AJ. A comparison of observational studies and randomized, controlled trials. N Engl J Med. 2000;342:1878–86. doi: 10.1056/NEJM200006223422506. [DOI] [PubMed] [Google Scholar]
- 60.Concato J, Shah N, Horwitz RI. Randomized, controlled trials, observational studies, and the hierarchy of research designs. N Engl J Med. 2000;342:1887–92. doi: 10.1056/NEJM200006223422507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Yeung TM, Cope AC, Whittome N, et al. Raised BMI is an independent risk factor for groin surgical site infections in patients undergoing varicose vein surgery. Am J Infect Control. 2008;36:152–3. doi: 10.1016/j.ajic.2007.08.002. [DOI] [PubMed] [Google Scholar]
- 62.Mekako AI, Chetter IC, Coughlin PA, et al. Hull Antibiotic pRophylaxis in varicose Vein Surgery Trialists (HARVEST) Randomized clinical trial of co-amoxiclav versus no antibiotic prophylaxis in varicose vein surgery. Br J Surg. 2010;97:29–36. doi: 10.1002/bjs.6849. [DOI] [PubMed] [Google Scholar]
- 63.Aherne T, McHugh SM, Tashkandi W, et al. Radiofrequency ablation: an assessment of clinical and cost efficacy. Ir J Med Sci. 2016;185:107–10. doi: 10.1007/s11845-014-1229-6. [DOI] [PubMed] [Google Scholar]
- 64.Proebstle TM, Alm BJ, Göckeritz O, et al. Five-year results from the prospective European multicentre cohort study on radiofrequency segmental thermal ablation for incompetent great saphenous veins. Br J Surg. 2015;102:212–8. doi: 10.1002/bjs.9679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kayssi A, Pope M, Vucemilo I, et al. Endovenous radiofrequency ablation for the treatment of varicose veins. Can J Surg. 2015;58:85–6. doi: 10.1503/cjs.014914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Rasmussen L, Lawaetz M, Serup J, et al. Randomized clinical trial comparing endovenous laser ablation, radiofrequency ablation, foam sclerotherapy, and surgical stripping for great saphenous varicose veins with 3-year follow-up. J Vasc Surg Venous Lymphat Disord. 2013;1:349–56. doi: 10.1016/j.jvsv.2013.04.008. [DOI] [PubMed] [Google Scholar]
- 67.Clinical guideline. London (UK): National Institute for Health and Care Excellence; 2013. [accessed 2018 Jan 2]. Varicose veins: diagnosis and management. Available: www.nice.org.uk/guidance/cg168/resources/varicose-veins-diagnosis-and-management-pdf-35109698485957. [Google Scholar]
- 68.Wittens C, Davies AH, Baekgaard N, et al. European Society for Vascular Surgery. Management of chronic venous disease: clinical practice guidelines of the European Society for Vascular Surgery (ESVS) Eur J Vasc Endovasc Surg. 2015;49:678–737. doi: 10.1016/j.ejvs.2015.02.007. [DOI] [PubMed] [Google Scholar]
- 69.O’Donnell TF, Passman MA, Marston WA, et al. Management of venous leg ulcers: clinical practice guidelines of the Society for Vascular Surgery and the American Venous Forum. J Vasc Surg. 2014;60:3S–59S. doi: 10.1016/j.jvs.2014.04.049. [DOI] [PubMed] [Google Scholar]