Abstract
Background
Subdural empyema (SDE) in children is a severe intracranial infection. Many pathogens can cause SDE.
Case Details
In this articlewe present a 15-month old Indonesian boy diagnosed as SDE based on the clinical symptoms and neuroimaging. A complete blood count showed white blood cell count of 13.800/mm3 and the CRP level was 8.3 mg/L. Craniotomy following burr hole drainage procedure was performed to decrease intracranial pressure. The liquor culture indicated Bacillus cereus. A meropenem injection and metronidazole infusion were administered appropriately with antibiotic sensitivity for several weeks. Immediate initiation of appropriate antibiotic therapy related to an accelerated surgical drainage can improve the outcome.
Conclusion
The combination of medication and surgery treatment for Bacillus cereus in SDE resulted in a good response, leaving neurological sequelae.
Keywords: Subdural empyema, children, bacillus cereus
Introduction
Subdural empyema (SDE) is a collection of purulent material between the dura mater and the arachnoid mater that usually occurs secondary to middle ear infection, meningitis, brain surgery, paranasal sinusitis, head trauma, or via hematogenous spread. The classic clinical syndrome is an acute febrile illness punctuated by rapid progressive neurological alterations and sometimes leads to coma with fatal outcome (1). Subdural empyema is a severe intracranial infection accounting for 15% to 25% of pyogenic suppuration and causing a mortality rate of approximately 15% to 40%. However, early detection, prompt removal of the site of infection, subdural pus drainage, and appropriate systemic antibiotic treatment may improve morbidity and mortality rate (1). Many pathogens can cause SDE, depending on the age of the patient and the route of the infection (1,2).
Bacillus cereus is a ubiquitous, spore-forming, motile, facultatively anaerobic, gram positive microorganism in which the spores are relatively resistant to extreme environmental conditions such as heating, freezing,drying and radiation (2). The usual form of the disease in the natural host is mild and self-limited. However, in the immunocompromised host, it can cause severe infection including bacteremia, pneumonia, endocarditis, meningitis, brain abscesses and gas gangrene (2). Here, we report uncommon pathogen Bacillus cereus that caused subdural empyema in a child.
Case Report
A 15-month old, previously healthy Indonesian boy with body weight 9.4 kg, experienced prolonged high-grade fever, projectile vomiting, generalized tonic seizure and reduction in consciousness. The patient had a history of several hospitalizations due to recurrent pneumonia, acute diarrhea with dehydration, hyperpyrexia, seizures, and unconsciousness. A 2 kg weight loss had been noted over the last two months of fever period. The bodyweight percentile decreased from 40th percentile to 5th percentile. The body length was in the 74th percentile. He could sit with assistance. The development of milestone was delayed. There was no history of hydrocephalus, neonatal infection or intrauterine infection. He was lethargic, with GCS 12, equally dilated pupils and slight left hemiparesis with an increase in physiological reflexes and spasticity. A complete blood count showed a white blood cell count of 13.800/mm3 and a platelet count of 503.000/mm3; the CRP level was 8.3 mg/L. A head MRI with contrast showed bilateral subdural empyema in the frontotemporoparietooccipital region, slight parenchymal hemorrhage, communicating hydrocephalus and meningoencephalitis (Figure 1). Intravenous ceftriaxone was regulated based on an empirical treatment of SDE. A craniotomy was performed following a burr hole drainage procedure to decrease the intracranial pressure. Liquor analysis demonstrated a purulent liquid, and the gram-positive microbe Bacillus cereus was identified from the culture. The histology of the empyema's wall supported a process of suppurative inflammation. A retroviral screening test was not performed. A decision to change the antibiotic was considered since ceftriaxone is known to be resistant to Bacillus cereus. Meropenem injection and metronidazole infusion were then administered according to the sensitivity of bacteria. The antibiotics were given for 42 consecutive days.
Figure 1.
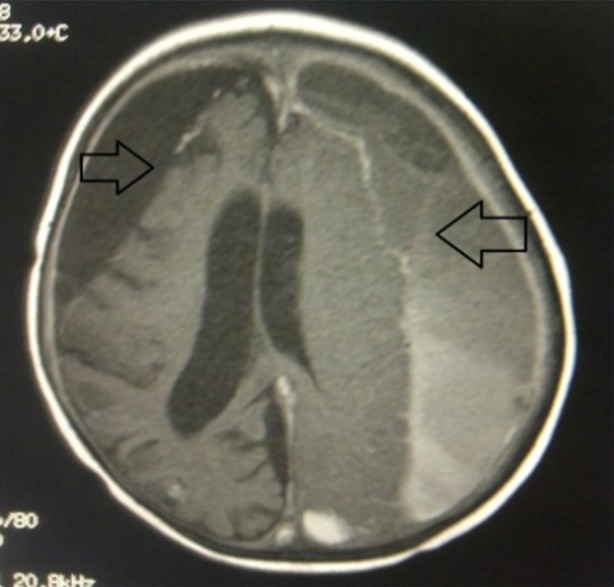
Head MRI with contrast showing bilateral subdural empyema in the frontotemporoparietooccipital region (arrows), slight parenchymal hemorrhage, communicating hydrocephalus and meningoencephalitis
An evaluation using head CT scan was performed after six weeks of treatment. This showed the left subdural hygroma frontotemporoparietal region, communicating hydrocephalus and left temporoparietal defect (Figure 2). Lumbar puncture revealed clear fluid, average cell count, glucose level of 43 g/L, protein level of 21 g/L with no microbes in gram staining. The patient was discharged, leaving spasticity in the extremities. The patient was then scheduled in a rehabilitation program.
Figure 2.
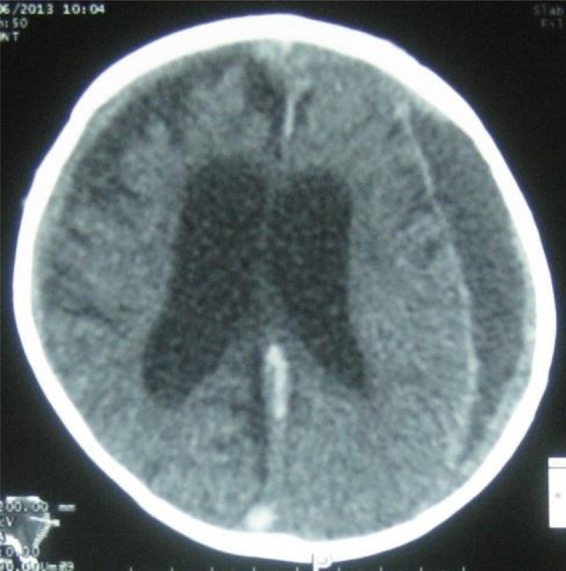
Head CT Scan after treatm
Discussion
Common causative organisms in intracranial SDE are anaerobes such as streptococci, staphylococci, Haemophilus influenza, Streptococcus pneumonia, and other gram-negative bacilli (1). Bacillus cereus has emerged as one of the new aerobic or facultative anaerobic gram-positive pathogens; it has spore-forming rods, is ubiquitous in the environment and may be part of the normal flora, particularly in patients with prolonged hospitalization (2,3). The presence of B. cereus in CSF must be evaluated regarding whether it is a contaminant or pathogenic microbe. The isolation of B. cereus in the CSF culture from an immunocompromised patient should not be viewed routinely as a contaminant but as a potential pathogen (2,3). Predisposing risk factors for opportunistic B. cereus infections include an altered host barrier defense, thereby permitting B. cereus an unconventional route of entry such as via traumatic and surgical wounds, intravenous drug use, burns, hemodialysis and indwelling catheters (3). Other factors include impaired neutrophil killing secondary to meningitis, paranasal sinusitis, middle ear infection, trauma, brain surgery, or via hematogenous spread (2,3). Our patient was suspected of being in an immunocompromised condition based on the clinical setting of recurrent infection, antibiotic therapy, and weight loss, although specific markers were not clearly identified. A history of indwelling catheters possibly played an important role in the development of B. cereus infections. The clinical manifestation supported the possibility of intracranial infection.
Ceftriaxone injection as empirical treatment was changed to meropenem injection and metronidazole infusion after neurosurgical drainage. Bacillus cereus isolates were susceptible to cefepime, carbapenems, aminoglycosides and vancomycin. Meropenem is part of the carbapenems group, which is highly resistant to degradation by the β-lactamases that have been reported among B. cereus strains (3,4). Metronidazole was also given in subdural empyema as this can reduce the mortality rate of intracranial suppuration from 42% to 9.7% (1,3). Intravenous antibiotics can be administered for three to six weeks on either an inpatient or outpatient basis. The duration of antibiotic treatment differs between practices. For instance, one method proposes a minimum of two weeks using the intravenous route, followed by six weeks of oral therapy (3).
A burr hole surgical procedure was performed in the operating room. A craniotomy procedure was then conducted, given the amount of pus production following burr hole surgery (5). In some situations, burr holes are recommended over craniotomies, for instance, in patients with para falcineempyemas or sepsis. Other indications for the use of burr holes include emergency conditions and those in which the patient is considered to be frail. The disadvantages of a burr hole are that the technique is not optimal for multi-loculated subdural fluid collections, and that it may lead to secondary injury of the cortex, thereby possibly exacerbating infections.
This condition is rare; only 11 reports of brain abscess and one report of B. cereus meningitis in children have previously been made. This infection has the potential to cause brain empyema in immunocompromised patients (4). The immediate initiation of antibiotic therapy related to an accelerated surgical drainage can improve the outcome of these patients. On follow-up, spasticity remained a problem following intracranial infection. Physical therapy was instituted to preserve muscles strength from the beginning.
In conclusion, SDE can be life-threatening if not managed properly. Bacillus cereus is a rare pathogenic bacteria as the cause of SDE. In this case, combined management using surgical procedures and antibiotics resulted in a good response, leaving neurological sequelae.
Acknowledgement
The authors would thank to Pherenice Charisti for helping managing the case.
References
- 1.Hendaus MA. Subdural empyema in children. Glob J Health Sci. 2013;5:54–59. doi: 10.5539/gjhs.v5n6p54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kotiranta A, Lounatmaa K, Haapasalo M. Epidemiology and pathogenesis of Bacilluscereus infections. Microbes and infection. 2000;2:189–198. doi: 10.1016/s1286-4579(00)00269-0. [DOI] [PubMed] [Google Scholar]
- 3.Jenson HB, Levy SR, Duncan C, Mcintosh S. Treatment of multiple brain abscesses caused by Bacilluscereus. Pediatr Infect Dis J. 1989;8:795–798. doi: 10.1097/00006454-198911000-00013. [DOI] [PubMed] [Google Scholar]
- 4.Barrie D, Wilson JA, Hoffman PN, Kramer JM. Bacillus cereus meningitis in two neurosurgical patients: an investigation into the source of the organism. J Infect. 1992;25:291–297. doi: 10.1016/0163-4453(92)91579-z. [DOI] [PubMed] [Google Scholar]
- 5.Gunawan PI, Suryaningtyas W. Giant subdural empyema following ventriculo-peritoneal shunt in a child. Pan Afr Med J. 2017;26:120. doi: 10.11604/pamj.2017.26.120.11866. [DOI] [PMC free article] [PubMed] [Google Scholar]


