Abstract
Background
The incidence of melanoma is increasing faster than any other major cancer both in Brazil and worldwide. Southeast Brazil has especially high incidences of melanoma, and early detection is low. Exposure to ultraviolet (UV) radiation is a primary risk factor for developing melanoma. Increasing attractiveness is a major motivation among adolescents for tanning. A medical student-delivered intervention that takes advantage of the broad availability of mobile phones and adolescents’ interest in their appearance indicated effectiveness in a recent study from Germany. However, the effect in a high-UV index country with a high melanoma prevalence and the capability of medical students to implement such an intervention remain unknown.
Objective
In this pilot study, our objective was to investigate the preliminary success and implementability of a photoaging intervention to prevent skin cancer in Brazilian adolescents.
Methods
We implemented a free photoaging mobile phone app (Sunface) in 15 secondary school classes in southeast Brazil. Medical students “mirrored” the pupils’ altered 3-dimensional (3D) selfies reacting to touch on tablets via a projector in front of their whole grade accompanied by a brief discussion of means of UV protection. An anonymous questionnaire capturing sociodemographic data and risk factors for melanoma measured the perceptions of the intervention on 5-point Likert scales among 356 pupils of both sexes (13-19 years old; median age 16 years) in grades 8 to 12 of 2 secondary schools in Brazil.
Results
We measured more than 90% agreement in both items that measured motivation to reduce UV exposure and only 5.6% disagreement: 322 (90.5%) agreed or strongly agreed that their 3D selfie motivated them to avoid using a tanning bed, and 321 (90.2%) that it motivated them to improve their sun protection; 20 pupils (5.6%) disagreed with both items. The perceived effect on motivation was higher in female pupils in both tanning bed avoidance (n=198, 92.6% agreement in females vs n=123, 87.2% agreement in males) and increased use of sun protection (n=197, 92.1% agreement in females vs n=123, 87.2% agreement in males) and independent of age or skin type. All medical students involved filled in a process evaluation revealing that they all perceived the intervention as effective and unproblematic, and that all pupils tried the app in their presence.
Conclusions
The photoaging intervention was effective in changing behavioral predictors for UV protection in Brazilian adolescents. The predictors measured indicated an even higher prospective effectiveness in southeast Brazil than in Germany (>90% agreement in Brazil vs >60% agreement in Germany to both items that measured motivation to reduce UV exposure) in accordance with the theory of planned behavior. Medical students are capable of complete implementation. A randomized controlled trial measuring prospective effects in Brazil is planned as a result of this study.
Keywords: skin neoplasms; primary prevention; adolescent; schools; students, medical; mobile applications; skin aging; smartphone
Introduction
According to the World Health Organization, the incidence of melanoma is increasing more rapidly than any other major cancer both in Brazil and worldwide. Melanoma is one of the most common cancers in young adults and poses substantial health and economic burdens [1].
Approximately 90% of melanomas are associated with ultraviolet (UV) exposure, in particular with the frequency of severe sunburns, and are therefore eminently preventable [2]. Multiple studies showed that daily use of a sunscreen with a sun protection factor above 30, as recommended by international dermatology guidelines, may prevent sunburns and skin cancer, including melanoma [3-6].
Brazil has one of the highest UV indexes on earth; additionally, tanning is culturally established, and Brazilians commonly experience unprotected overexposure to the sun, especially in their childhood and teenage years [7-11]. In a 2008 population-based survey with 1604 participants in the south of Brazil, 48.7% reported at least one sunburn in the prior year [10]. In an attempt to mitigate the health damage caused by excessive UV exposure, Brazil was the first country to prohibit indoor tanning in 2009, albeit with limited success [9]. The southeast of Brazil (the location of this study) is especially populated by citizens with a European ancestry and therefore has high incidences of melanoma (up to 23.5/100,000 inhabitants) with a lack of early diagnosis and an overall survival rate below worldwide rates [12-15].
Interventions encouraging sun protection habits are important, particularly among adolescents, as increased risk of skin cancer is associated with cumulative UV exposure and sunburns early in life [16-18]. In line with this association, recent experimental studies to test these effects in young target groups aimed at promoting sunscreen use as an end point [19-22], and others used various UV protection behaviors (including avoiding sunbeds) or behavior scores [23-34]. Given the substantial amount of time that children and adolescents of all social backgrounds spend in the school environment, addressing skin cancer prevention in this setting is crucial and provides a unique opportunity to propel skin cancer prevention programs [35].
Current Knowledge on School-Based Skin Cancer Prevention
Unhealthy behavior with respect to UV exposure is mostly initiated in early adolescence [36], commonly with the belief that a tan increases attractiveness [26,37,38], and the problems related to melanoma and skin atrophy are too far in the future for them to fathom.
A recent randomized trial with Australian high school students demonstrated that appearance-based videos on UV-induced premature aging were superior in encouraging sunscreen use to videos of the same length focusing exclusively on health aspects [19]. These findings are in line with international studies demonstrating the important influence of self-perceived attractiveness on self-esteem in adolescence [39,40]. Furthermore, enhancing one’s attractiveness is a primary motivation for tanning in adolescents both in Brazil and worldwide [36,37,41]. In addition, the success of appearance-based photoaging intervention mobile apps, in which an image is altered to predict future appearance, in the fields of tobacco and adiposity prevention have shown promise for these interventions in behavioral change settings [42-47].
In the setting of melanoma prevention, a quasi-experimental study by Williams et al demonstrated significantly higher scores for predictors of sun protection behavior in young women from the United Kingdom (70 participants in total) using a photoaging desktop program [48]. Furthermore, the photoaging software showed a promising reduction in young adults’ tanning intentions in a study with 10 participants in total (7 female and 3 male) [49]. However, prior studies were limited by their small sample size and limitations related to expanding the target population.
Introduction to the Sunface App
We harnessed the widespread availability of mobile phones and adolescents’ interest in appearance to develop the free mobile phone app Sunface, which enables the user to take a selfie and then offers a choice of 3 categories: daily sun protection, no sun protection, and weekly tanning, showing the altered face at 5 to 25 years in the future (Figures 1, 2, 3, and 4). All effects are based on the individual skin type that the user can choose at the start of the app (Figure 5). The app also shows the most common UV-induced skin cancers via extra buttons and calculates how the odds ratio is increased with different behaviors.
Figure 1.
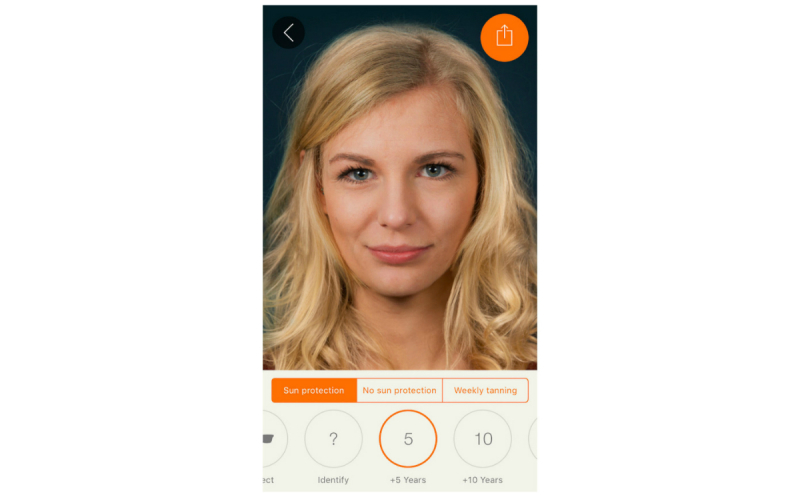
Effect view: 5 years of skin aging with sun protection.
Figure 2.
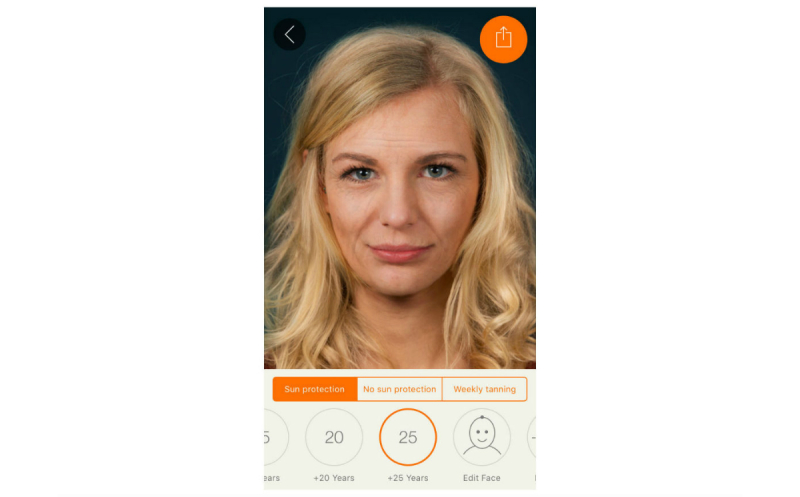
Effect view: 25 years of skin aging with sun protection.
Figure 3.
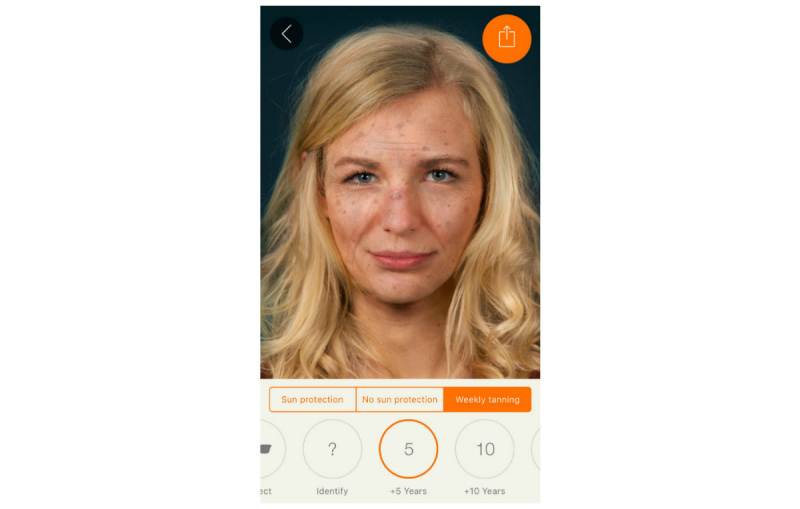
Effect view: 5 years of weekly tanning without sun protection.
Figure 4.
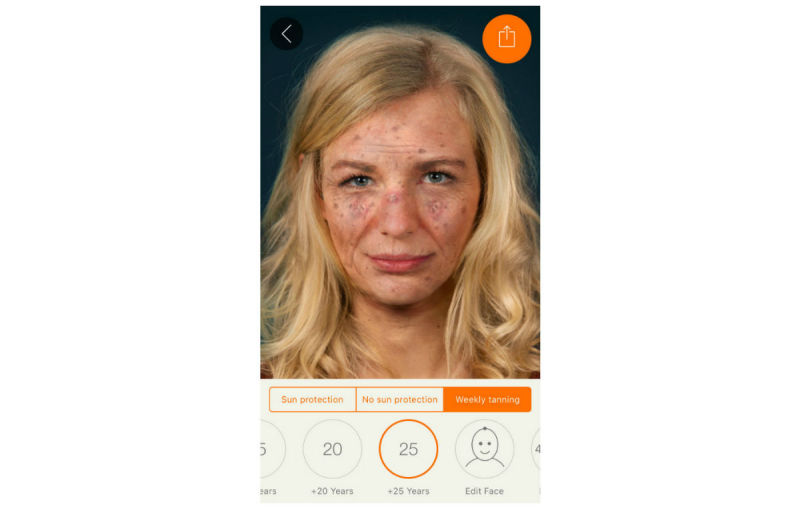
Maximum effect view: 25 years of UV damage due to weekly tanning.
Figure 5.
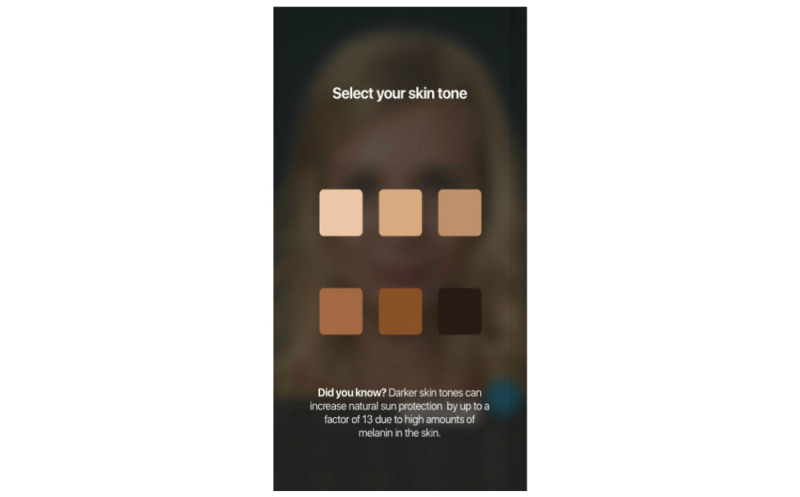
Start screen of the app prompts users to pick their skin type.
In addition, the app gives advice on sun protection, explains the facial changes, and encourages skin examinations using the ABCDE rule (asymmetry, border irregularity, color variety, diameter, and evolution [50]).
Afterward, the app offers many options for sharing (animated photo or video; see Multimedia Appendix 1) with family and friends. By this means, the social network of the user may also be informed about the various photoaging effects of excessive UV exposure and potential health consequences, as well as potentially learning about the benefits of using the app [34].
To produce realistic effects (Figure 6) and to show the user realistic odds ratios for the options they choose in the app for the three most strongly associated skin pathologies, an extensive review of the literature on UV-induced skin damage [51,52] was conducted for each specific skin type. As no trials with 25 years of follow-up were available, we had to extrapolate the evidence on UV-induced skin damage for the specific skin types. The evidence consists of more than 50 publications to create realistic effects from a clinician’s standpoint (which may differ from what the average person perceives as realistic).
Figure 6.
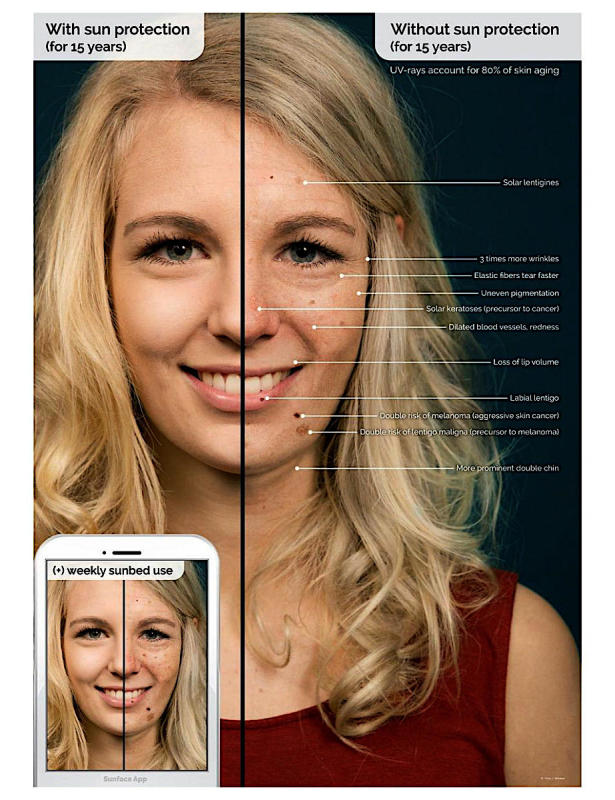
Explanatory graphic of the effects within the app.
We recently implemented this app in 2 German secondary schools via a method called mirroring. Mirroring means that the student’s altered 3-dimensional (3D) selfies are “mirrored” via a projector in front of the entire class. Using an anonymous questionnaire, we then measured sociodemographic data and risk factors for melanoma, as well as the perceptions of the intervention on a 5-point Likert scale among 205 students of both sexes aged 13 to 19 years (median 15 years).
In our pilot study, we found more than 60% agreement in both items measuring motivation to reduce UV exposure and only 12.5% disagreement: 126 (63.0%) agreed or strongly agreed that their 3D selfie motivated them to avoid using a tanning bed, and 124 (61.7%) agreed or strongly agreed to increase their use of sun protection; only 25 (12.5%) disagreed with both items. [33].
An explanation for these results is offered by the theory of planned behavior, according to which the subjective norm (eg, “my friends think that tanning makes you unattractive”), attitudes (consisting of beliefs, such as “tanning leads to unattractiveness”), and perceived behavioral control (eg, “I can apply sunscreen correctly”) influence both the behavioral intentions of a person and his or her behavior. Photoaging interventions have the potential to affect all three of these predictors, and the mirroring intervention specifically had a strong influence on the subjective norm in the previous pilot study [33].
This study investigated whether the results of our novel photoaging intervention would be reproducible in Brazil, a country with a high UV index and, thus, higher prevalences of malignant melanoma and an even stronger need for effective skin cancer prevention programs. Also, a process evaluation investigated whether volunteering medical students would be capable of complete implementation.
Methods
Setting
We conducted the study in 2 regular public secondary schools in the city of Ponte Nova, southeast Brazil. Students who were 13 to 19 years of age and attending regular secondary schools in the city of Ponte Nova were eligible.
Intervention
The mirroring approach was implemented by medical students from the Education Against Tobacco nonprofit organization who were attending the Federal University of Ouro Preto in Brazil [46,53]. To increase the pupils’ familiarity with the Sunface photoaging app and their participation in the mirroring intervention, we asked them to download the app before our visit, via a letter 1 week in advance. When we visited the schools, 12.6% (45/356) had the app on their mobile phones.
The intervention consisted of a 45-minute app-based mirroring educational module in the classroom setting. It was presented by 2 medical students per classroom to approximately 24 students at a time (mean 23.7, SD 6.1 students).
In the first 10-minute phase, the displayed face of one student volunteer was used to show the app’s altering features to the peer group, providing an incentive for the rest of the class to test the app. In front of their peers and teachers, students could interact with their own animated face via touch (coughing, sneezing, etc) and display their future self based on their skin type and use of sun protection or tanning beds 5, 10, 15, 20, or 25 years in the future. Multiple device displays could be projected simultaneously, which we used to consolidate the altering measures with graphics (eg, to explain skin atrophy and solar elastosis). We implemented mirroring with 10 Galaxy Tab A tablets (Samsung, Seoul, South Korea) via Apple’s AirPlay interface (Apple Inc) using the app Mirroring360 (Splashtop Inc) for the Android operating system (Google Inc).
In the second 15-minute phase, students were encouraged to try the app on one of the tablet computers. We calculated the number of provided tablet computers so that this phase would take up to 12 minutes at most after factoring in a use time of approximately 4 minutes per student. By this calculation, 25 minutes of the mirroring intervention and 10 provided tablets were sufficient to have every student within a class of 40 pupils successfully photoaged at least once.
In the following 15 minutes, the medical students discussed the remaining functions of the app with the students: facial changes, the ABCDE rule, and the guidelines for sun protection were addressed in an interactive setting. In the last 5 minutes, we measured the students’ perception of the intervention via an anonymous paper-and-pencil questionnaire.
Data Collection
We measured the students’ sociodemographic data (sex, age, school type) and their risk profile (skin type, sex, age, sunburn in the past, sunbed use) directly after the intervention via an anonymous survey. The reactions to the intervention were captured via 6 items on 5-point Likert scales: (1) increase of UV protection intentions due to the photoaging intervention (2 items: indoor vs outdoor tanning); (2) perceived reactions of the peer group on change in attractiveness (2 items: indoor vs outdoor tanning), whether they perceived the intervention as fun (1 item), and the effects of the app as realistic (1 item).
The items used were transferred from previously published studies [33,43,54] and pretested in advance in accordance with the guidelines for good epidemiologic practice [55].
The medical students filled out a brief process evaluation consisting of 6 items capturing the complete implementation of the intervention, as well as how the medical students perceived its effectiveness when in class.
Results
Participants
We included 356 Brazilian secondary school students of both sexes in the age group of 13 to 19 years (mean 15.95, SD 1.73 years; 141/356, 39.7% male; 214/356, 60.3% female) in this cross-sectional pilot study. They were attending 2 regular public secondary schools in the city of Ponte Nova in southeast Brazil. Almost all participants (336/356, 94.4%) owned a smartphone.
From a risk profile standpoint, 43.9% (156/356) of the participants had a Fitzpatrick skin type of 1 or 2 [56]; indoor tanning bed use in the past year was reported by 2.0% (7/356) and use at least once in their life was reported by 4.5% (16/356) [57]. Most students (205/356, 57.6%) remembered at least one sunburn in the past [58], 18.3% (65/356) reported one or more sunburns in the last 12 months, and 15.8% (56/356) reported that they frequently went out in the sun to get a tan.
We analyzed and illustrated all data in regard to overall perceptions of the intervention within the whole sample (Figure 7), but also to learn about how well the app was received by students of different Fitzpatrick skin types (Figure 8), sex (Figure 9), and age groups (Figure 10).
Figure 7.
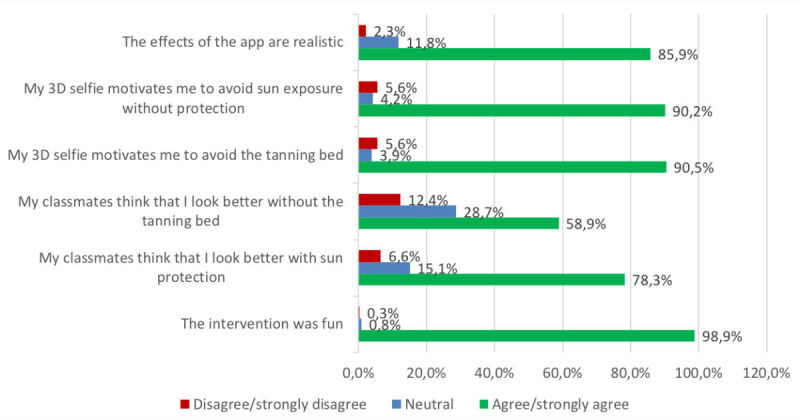
Overall results of the whole sample. 3D: 3-dimensional.
Figure 8.
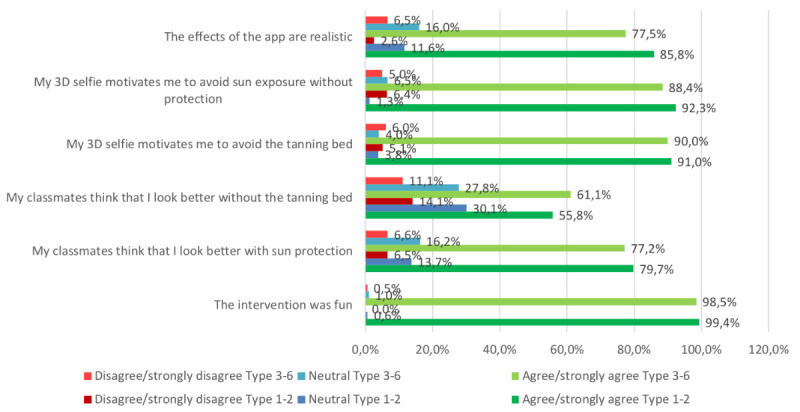
Results in Fitzpatrick skin types 1-2 versus 3-6. 3D: 3-dimensional.
Figure 9.
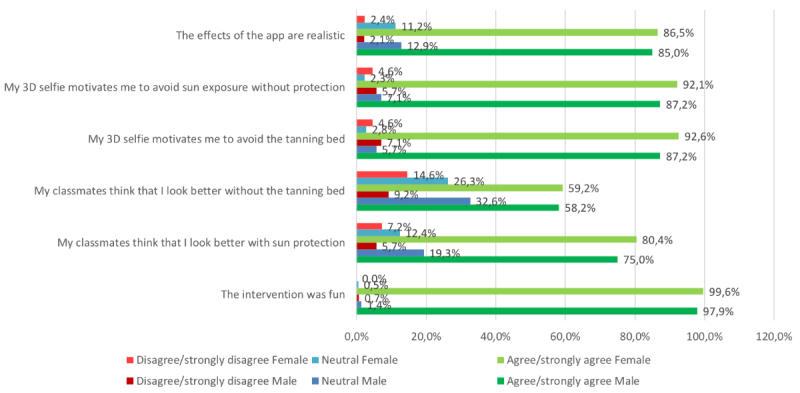
Results in male versus female participants. 3D: 3-dimensional.
Figure 10.
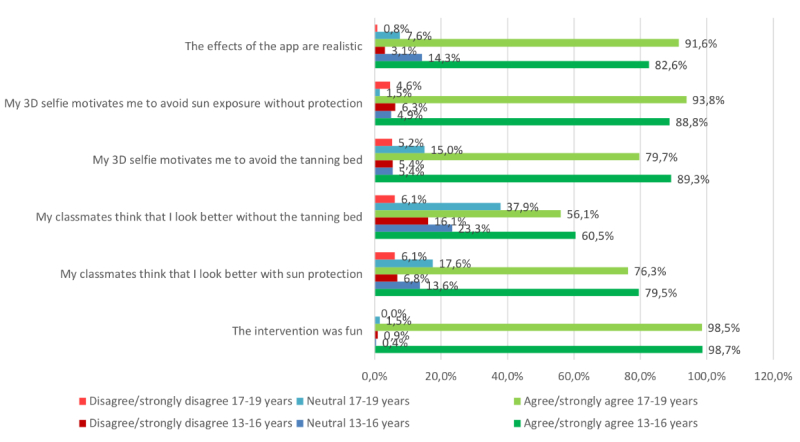
Results in 13- to 16-year-old versus 17- to 19-year-old participants. 3D: 3-dimensional.
Realism of the Created Selfies
In our sample, we measured overall agreement with the subjective realism of the created selfies (n=305, 85.9% strongly agreed or agreed on realism, while only n=8, 2.3% disagreed or strongly disagreed; Figure 7). These results did not vary notably between male (n=119, 85.0% agreement; n=3, 2.1% disagreement) and female participants (n=185, 86.5% agreement; n=5, 2.4% disagreement; Figure 9). However, the 13- to 16-year-olds (n=185, 82.6% agreement; n=7, 3.1% disagreement) and those with skin types 1 and 2 (n=133, 85.8% agreement; n=4, 2.6% disagreement) tended to perceive the selfies as less realistic, as opposed to 17- to 19-year-olds (n=120, 91.6% agreement; n=1, 0.8% disagreement) and participants with skin types 3 to 6 (n=155, 77.5% agreement; n=13, 6.5% disagreement; Figure 8 and Figure 10). The group that reported at least one sunburn in the last 12 months had a 92.3% (n=60) agreement and 1.5% (n=1) disagreement compared with 84.5% (n=245) agreement and 2.4% (n=7) disagreement among participants without sunburns in the past 12 months.
Motivation to Reduce Ultraviolet Exposure
We measured more than 90% agreement in both items that measured motivation to reduce UV exposure and only 5.6% disagreement (n=322, 90.5% agreed or fully agreed that their 3D selfie would motivate them to avoid the tanning bed; n=321, 90.2% agreed or fully agreed that they would increase their use of sun protection); only 20 (5.6%) disagreed or fully disagreed with both items. The perceived effect on motivation was similar between participants with different Fitzpatrick skin types in both tanning bed avoidance (n=142, 91.0% agreement in skin types 1-2 vs n=179, 90.0% agreement in types 3-6) and increased use of sun protection (n=144, 92.3% agreement in skin types 1-2 vs n=176, 88.4% agreement in types 3-6; Figure 8), and also similar between the age groups (Figure 10). Comparing by sex, the perceived effect on motivation was higher in female pupils in both tanning bed avoidance (n=198, 92.6% agreement in female vs n=123, 87.2% agreement in male participants) and increased use of sun protection (n=197, 92.1% agreement in female vs n=123, 87.2% agreement in male participants).
Perceived Subjective Norm During the Mirroring Intervention
The 2 items measuring the perceived reactions of the peer group toward the individual selfie showed positive peer pressure in regard to both use of sun protection (n=275, 78.3%) and tanning bed avoidance (n=209, 58.9%; Figure 7). The subjective norm on decreasing UV exposure in order to look more attractive was similarly perceived between the different age groups (Figure 10). However, female participants (n=169, 80.4% agreement; n=15, 7.2% disagreement) tended to feel a stronger urge to increase the use of sun protection due to the behavior of their classmates than did male participants (n=105, 75% agreement; n=8, 5.7% disagreement). Participants with Fitzpatrick skin types 1 and 2 (n=87, 55.8% agreement; n=22, 14.1% disagreement) tended to perceive less peer pressure for avoiding tanning beds than did skin types 3 to 6 (n=121, 61.1% agreement; n=22, 11.1% disagreement). Participants with at least one sunburn in the last 12 months had a higher agreement in the increased use of sun protection item (n=49, 75.4% agreement; n=5, 7.7% disagreement vs n=197, 67.9% agreement; n=26, 9% disagreement in participants without sunburn in the past 12 months) and in the avoidance of sunbeds item (n=55, 84.6% agreement; n=5, 7.7% disagreement vs n=220, 76.9% agreement; n=18, 6.2% disagreement, respectively).
Global Feedback
Most participants claimed that they perceived the intervention as fun (n=351, 98.9% agreement vs n=1, 0.3% disagreement), and this fraction of agreement was similar throughout all subgroups. Most participants (n=271, 77.0%) reported that they would try the app again later on, 283 (80.2%) planned to show the app to another person after school, and 352 (98.9%) agreed that they had learned new things about the advantages of sun protection.
Data Obtained From the Medical Students
Our process evaluation conducted among all of the 6 volunteering medical students via a short questionnaire after every classroom visit revealed that 100% of the secondary school students received the mirroring intervention as outlined in the methods section, and that 100% of the medical students were capable of having an empathic communication with the students and regarded the intervention as enjoyable.
Discussion
Principal Findings
Our data showed that the mirroring intervention was effective in changing the predictors of behavior in young risk groups living in Brazil, a country with a high UV index and where tanning is culturally established. The predictors measured indicated an even higher prospective effectiveness in southeast Brazil than in Germany (>90% agreement in Brazil vs >60% agreement in Germany to both items that measured motivation to reduce UV exposure [33]).
While teledermatology [59,60] and, more specifically, skin cancer diagnostic apps [61-65] are emerging, early diagnostics may only be successful if a patient is sensitized for an eventual skin cancer risk and about skin cancer in general. Photoaging smartphone apps seem capable of filling this important gap by appealing to vanity.
Interpretation
Available data on appearance-based behavioral change settings for adolescents reveal that photoaging interventions appear to be more effective for girls [46]. Also, data from our recent study in Germany indicated that the intervention was more effective in changing motivational predictors in those with Fitzpatrick skin types 1 and 2, as well as in older adolescents. In our sample, the perceived effect on motivation was higher among female pupils in both tanning bed avoidance (n=198, 92.6% agreement in female vs n=123, 87.2% agreement in male participants) and increased use of sun protection (n=197, 92.1% agreement in female vs n=123, 87.2% agreement in male participants), while it was independent of age or skin type. We hypothesize that the most likely explanation for this is that gender roles are more established in southeast Brazil than they are in Germany and that peer pressure plays a larger role, which thus flattened out the differences for age and skin type that we found in our German study [33]. Accordingly, this hypothesis is in line with the finding that an intervention like the mirroring intervention, which aims at yielding peer pressure effects and addresses social norms, had a larger impact in a country like Brazil, where social norms play a larger role than in Germany.
Limitations
As we conducted this study only in Brazil, our results might not be generalizable to other cultural or national settings. However, cosmetics are used by adolescents in most countries and appearance is a strong motivator for behavior in different cultural contexts [39,66].
In addition, our results stemmed from anonymous self-reports via paper-and-pencil questionnaires filled out after the intervention. While anonymity decreases social desirability bias in self-reports, they may not be regarded to be as objective as externally measurable markers, such as biochemical findings or clinical observation. Furthermore, handing the questionnaires out after the intervention rather than before might provoke a social desirability bias despite anonymity.
Conclusions
The photoaging intervention was effective in generating an increased intention for UV protective behavior in Brazilian adolescents. The predictors measured indicated an even higher prospective effectiveness in southeast Brazil than in Germany (>90% agreement in Brazil vs >60% agreement in Germany to both items that measured motivation to reduce UV exposure) in accordance with the theory of planned behavior. Medical students are capable of complete implementation. A randomized controlled trial measuring prospective effects in Brazil is planned as a result of this study [67].
Acknowledgments
The authors would like to thank all participating schools, students, volunteering medical students, and teachers who helped organize the classroom visits in the city of Ponte Nova.
The tablets were funded by the Young Research Award Research Grant from La Fondation La Roche Posay awarded to TJB for his research on the Sunface app. The Federal University of Ouro Preto contributed by providing logistic support for the project and copies of all questionnaires. La Fondation La Roche Posay and the Federal University of Ouro Preto Funding Board had no role in the design and conduct of this study or in the preparation, review, or approval of this manuscript.
Abbreviations
- 3D
3-dimensional
- ABCDE
asymmetry, border irregularity, color variety, diameter, and evolution
- UV
ultraviolet
Animated version of the Sunface App effect view.
Footnotes
Authors' Contributions: TJB initiated the study; invented, designed, and organized the intervention; wrote the manuscript; drafted the design of the study; and performed the statistical analyses. BBS participated in the conception of the study. HRR, CAS, BBS, MG, SS, MVH, MCK, MH, and DS contributed to the design of the study, data collection, data analyses, and proofreading of the manuscript. BBS contributed to the logistics of the study, assisted with the translation of classroom materials, and reviewed the final version of the manuscript. All authors declare responsibility for the data and findings presented and have full access to the dataset.
Conflicts of Interest: None declared.
References
- 1.Livingstone E, Windemuth-Kieselbach C, Eigentler TK, Rompel R, Trefzer U, Nashan D, Rotterdam S, Ugurel S, Schadendorf D. A first prospective population-based analysis investigating the actual practice of melanoma diagnosis, treatment and follow-up. Eur J Cancer. 2011 Sep;47(13):1977–89. doi: 10.1016/j.ejca.2011.04.029. [DOI] [PubMed] [Google Scholar]
- 2.The Lancet Editorial Board Skin cancer: prevention is better than cure. Lancet. 2014 Aug 09;384(9942):470. doi: 10.1016/S0140-6736(14)61320-9. [DOI] [PubMed] [Google Scholar]
- 3.Green AC, Williams GM, Logan V, Strutton GM. Reduced melanoma after regular sunscreen use: randomized trial follow-up. J Clin Oncol. 2011 Jan 20;29(3):257–63. doi: 10.1200/JCO.2010.28.7078. [DOI] [PubMed] [Google Scholar]
- 4.Ghiasvand R, Weiderpass E, Green AC, Lund E, Veierød MB. Sunscreen use and subsequent melanoma risk: a population-based cohort study. J Clin Oncol. 2016 Nov 20;34(33):3976–3983. doi: 10.1200/JCO.2016.67.5934. [DOI] [PubMed] [Google Scholar]
- 5.Nijsten T. Sunscreen use in the prevention of melanoma: common sense rules. J Clin Oncol. 2016 Nov 20;34(33):3956–3958. doi: 10.1200/JCO.2016.69.5874. [DOI] [PubMed] [Google Scholar]
- 6.Ou-Yang H, Jiang LI, Meyer K, Wang SQ, Farberg AS, Rigel DS. Sun protection by beach umbrella vs sunscreen with a high sun protection factor: a randomized clinical trial. JAMA Dermatol. 2017 Mar 01;153(3):304–308. doi: 10.1001/jamadermatol.2016.4922. [DOI] [PubMed] [Google Scholar]
- 7.Benvenuto-Andrade C, Zen B, Fonseca G, De Villa VD, Cestari T. Sun exposure and sun protection habits among high-school adolescents in Porto Alegre, Brazil. Photochem Photobiol. 2005;81(3):630–5. doi: 10.1562/2005-01-25-RA-428. [DOI] [PubMed] [Google Scholar]
- 8.Purim KSM, Wroblevski FC. Exposição e proteção solar dos estudantes de medicina de Curitiba (PR) Rev Bras Educ Med. 2014 Dec;38(4):477–485. doi: 10.1590/S0100-55022014000400009. [DOI] [Google Scholar]
- 9.Schalka S, Steiner D, Ravelli FN, Steiner T, Terena AC, Marçon CR, Ayres EL, Addor FAS, Miot HA, Ponzio H, Duarte I, Neffá J, Cunha JAJD, Boza JC, Samorano LDP, Corrêa MDP, Maia M, Nasser N, Leite OMRR, Lopes OS, Oliveira PD, Meyer RLB, Cestari T, Reis VMSD, Rego VRPDA, Brazilian Society of Dermatology Brazilian consensus on photoprotection. An Bras Dermatol. 2014;89(6 Suppl 1):1–74. doi: 10.1590/abd1806-4841.20143971. http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0365-05962014000700001&lng=en&nrm=iso&tlng=en. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Haack RL, Horta BL, Cesar JA. [Sunburn in young people: population-based study in Southern Brazil] Rev Saude Publica. 2008 Feb;42(1):26–33. doi: 10.1590/s0034-89102008000100004. http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0034-89102008000100004&lng=en&nrm=iso&tlng=en. [DOI] [PubMed] [Google Scholar]
- 11.Silva AA. Outdoor exposure to solar ultraviolet radiation and legislation in Brazil. Health Phys. 2016 Dec;110(6):623–6. doi: 10.1097/HP.0000000000000489. [DOI] [PubMed] [Google Scholar]
- 12.Lima ASD, Stein CE, Casemiro KP, Rovere RK. Epidemiology of melanoma in the South of Brazil: study of a city in the Vale do Itajaí from 1999 to 2013. An Bras Dermatol. 2015;90(2):185–9. doi: 10.1590/abd1806-4841.20153076. http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0365-05962015000200185&lng=en&nrm=iso&tlng=en. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.de Lima Vazquez V, Silva TB, de Andrade Vieira M, de Oliveira ATT, Lisboa MV, de Andrade DAP, Fregnani JHTG, Carneseca EC. Melanoma characteristics in Brazil: demographics, treatment, and survival analysis. BMC Res Notes. 2015 Jan 16;8:4. doi: 10.1186/s13104-015-0972-8. https://bmcresnotes.biomedcentral.com/articles/10.1186/s13104-015-0972-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Amancio CT, Nascimento LFC. Cutaneous melanoma in the State of São Paulo: a spatial approach. An Bras Dermatol. 2014;89(3):442–6. doi: 10.1590/abd1806-4841.20142722. http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0365-05962014000300442&lng=en&nrm=iso&tlng=en. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Naser N. Cutaneous melanoma: a 30-year-long epidemiological study conducted in a city in southern Brazil, from 1980-2009. An Bras Dermatol. 2011;86(5):932–41. doi: 10.1590/s0365-05962011000500011. http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0365-05962011000500011&lng=en&nrm=iso&tlng=en. [DOI] [PubMed] [Google Scholar]
- 16.Lo JA, Fisher DE. The melanoma revolution: from UV carcinogenesis to a new era in therapeutics. Science. 2014 Nov 21;346(6212):945–9. doi: 10.1126/science.1253735. http://europepmc.org/abstract/MED/25414302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wu S, Han J, Laden F, Qureshi AA. Long-term ultraviolet flux, other potential risk factors, and skin cancer risk: a cohort study. Cancer Epidemiol Biomarkers Prev. 2014 Jun;23(6):1080–9. doi: 10.1158/1055-9965.EPI-13-0821. http://cebp.aacrjournals.org/cgi/pmidlookup?view=long&pmid=24876226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Barton MK. Indoor tanning increases melanoma risk, even in the absence of a sunburn. CA Cancer J Clin. 2014;64(6):367–8. doi: 10.3322/caac.21248. doi: 10.3322/caac.21248. [DOI] [PubMed] [Google Scholar]
- 19.Tuong W, Armstrong AW. Effect of appearance-based education compared with health-based education on sunscreen use and knowledge: a randomized controlled trial. J Am Acad Dermatol. 2014 Apr;70(4):665–9. doi: 10.1016/j.jaad.2013.12.007. [DOI] [PubMed] [Google Scholar]
- 20.Craciun C, Schüz N, Lippke S, Schwarzer R. Facilitating sunscreen use in women by a theory-based online intervention: a randomized controlled trial. J Health Psychol. 2012 Mar;17(2):207–16. doi: 10.1177/1359105311414955. [DOI] [PubMed] [Google Scholar]
- 21.Hirst NG, Gordon LG, Scuffham PA, Green AC. Lifetime cost-effectiveness of skin cancer prevention through promotion of daily sunscreen use. Value Health. 2012;15(2):261–8. doi: 10.1016/j.jval.2011.10.009. https://linkinghub.elsevier.com/retrieve/pii/S1098-3015(11)03530-3. [DOI] [PubMed] [Google Scholar]
- 22.Sakoufaki M, Stergiopoulou A, Stratigos A. Design and implementation of a health promotion program to prevent the harmful effects of ultraviolet radiation at primary school students of rural areas of Greece. Int J Res Dermatol. 2017 Aug 24;3(3):306. doi: 10.18203/issn.2455-4529.IntJResDermatol20172505. [DOI] [Google Scholar]
- 23.Miller KA, Langholz BM, Ly T, Harris SC, Richardson JL, Peng DH, Cockburn MG. SunSmart: evaluation of a pilot school-based sun protection intervention in Hispanic early adolescents. Health Educ Res. 2015 Jun;30(3):371–9. doi: 10.1093/her/cyv011. http://europepmc.org/abstract/MED/25801103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Aarestrup C, Bonnesen CT, Thygesen LC, Krarup AF, Waagstein AB, Jensen PD, Bentzen J. The effect of a school-based intervention on sunbed use in Danish pupils at continuation schools: a cluster-randomized controlled trial. J Adolesc Health. 2014 Feb;54(2):214–20. doi: 10.1016/j.jadohealth.2013.08.011. [DOI] [PubMed] [Google Scholar]
- 25.Holman DM, Fox KA, Glenn JD, Guy GP, Watson M, Baker K, Cokkinides V, Gottlieb M, Lazovich D, Perna FM, Sampson BP, Seidenberg AB, Sinclair C, Geller AC. Strategies to reduce indoor tanning: current research gaps and future opportunities for prevention. Am J Prev Med. 2013 Jun;44(6):672–81. doi: 10.1016/j.amepre.2013.02.014. http://europepmc.org/abstract/MED/23683986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hillhouse J, Turrisi R, Scaglione NM, Cleveland MJ, Baker K, Florence LC. A web-based intervention to reduce indoor tanning motivations in adolescents: a randomized controlled trial. Prev Sci. 2017 Feb;18(2):131–140. doi: 10.1007/s11121-016-0698-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stapleton JL, Hillhouse J, Levonyan-Radloff K, Manne SL. Review of interventions to reduce ultraviolet tanning: need for treatments targeting excessive tanning, an emerging addictive behavior. Psychol Addict Behav. 2017 Jun 22;31(8):962–978. doi: 10.1037/adb0000289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Olson AL, Gaffney C, Starr P, Gibson JJ, Cole BF, Dietrich AJ. SunSafe in the Middle School Years: a community-wide intervention to change early-adolescent sun protection. Pediatrics. 2007 Jan;119(1):e247–56. doi: 10.1542/peds.2006-1579. [DOI] [PubMed] [Google Scholar]
- 29.Miller KA, Huh J, Unger JB, Richardson JL, Allen MW, Peng DH, Cockburn MG. Patterns of sun protective behaviors among Hispanic children in a skin cancer prevention intervention. Prev Med. 2015 Dec;81:303–8. doi: 10.1016/j.ypmed.2015.09.027. http://europepmc.org/abstract/MED/26436682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Turner D, Harrison SL, Buettner P, Nowak M. Does being a “SunSmart School” influence hat-wearing compliance? An ecological study of hat-wearing rates at Australian primary schools in a region of high sun exposure. Prev Med. 2014 Mar;60:107–14. doi: 10.1016/j.ypmed.2013.12.020. [DOI] [PubMed] [Google Scholar]
- 31.Buller DB, Andersen PA, Walkosz BJ, Scott MD, Beck L, Cutter GR. Rationale, design, samples, and baseline sun protection in a randomized trial on a skin cancer prevention intervention in resort environments. Contemp Clin Trials. 2016 Jan;46:67–76. doi: 10.1016/j.cct.2015.11.015. http://europepmc.org/abstract/MED/26593781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sontag JM, Noar SM. Assessing the potential effectiveness of pictorial messages to deter young women from indoor tanning: an experimental study. J Health Commun. 2017 Apr;22(4):294–303. doi: 10.1080/10810730.2017.1281361. [DOI] [PubMed] [Google Scholar]
- 33.Brinker TJ, Brieske CM, Schaefer CM, Buslaff F, Gatzka M, Petri MP, Sondermann W, Schadendorf D, Stoffels I, Klode J. Photoaging mobile apps in school-based melanoma prevention: pilot study. J Med Internet Res. 2017 Sep 08;19(9):e319. doi: 10.2196/jmir.8661. http://www.jmir.org/2017/9/e319/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Brinker TJ, Schadendorf D, Klode J, Cosgarea I, Rösch A, Jansen P, Stoffels I, Izar B. Photoaging mobile apps as a novel opportunity for melanoma prevention: pilot study. JMIR Mhealth Uhealth. 2017 Jul 26;5(7):e101. doi: 10.2196/mhealth.8231. http://mhealth.jmir.org/2017/7/e101/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Guy GP, Holman DM, Watson M. The important role of schools in the prevention of skin cancer. JAMA Dermatol. 2016 Oct 01;152(10):1083–1084. doi: 10.1001/jamadermatol.2016.3453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Görig T, Diehl K, Greinert R, Breitbart EW, Schneider S. Prevalence of sun-protective behaviour and intentional sun tanning in German adolescents and adults: results of a nationwide telephone survey. J Eur Acad Dermatol Venereol. 2018 Feb;32(2):225–235. doi: 10.1111/jdv.14376. [DOI] [PubMed] [Google Scholar]
- 37.Schneider S, Diehl K, Bock C, Schlüter M, Breitbart EW, Volkmer B, Greinert R. Sunbed use, user characteristics, and motivations for tanning: results from the German population-based SUN-Study 2012. JAMA Dermatol. 2013 Jan;149(1):43–9. doi: 10.1001/2013.jamadermatol.562. [DOI] [PubMed] [Google Scholar]
- 38.Hillhouse J, Turrisi R, Cleveland MJ, Scaglione NM, Baker K, Florence LC. Theory-driven longitudinal study exploring indoor tanning initiation in teens using a person-centered approach. Ann Behav Med. 2016 Feb;50(1):48–57. doi: 10.1007/s12160-015-9731-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Baudson TG, Weber KE, Freund PA. More than only skin deep: appearance self-concept predicts most of secondary school students' self-esteem. Front Psychol. 2016;7:1568. doi: 10.3389/fpsyg.2016.01568. doi: 10.3389/fpsyg.2016.01568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wichstrøm L, von Soest T. Reciprocal relations between body satisfaction and self-esteem: a large 13-year prospective study of adolescents. J Adolesc. 2016 Feb;47:16–27. doi: 10.1016/j.adolescence.2015.12.003. [DOI] [PubMed] [Google Scholar]
- 41.Bränström R, Kasparian NA, Chang Y, Affleck P, Tibben A, Aspinwall LG, Azizi E, Baron-Epel O, Battistuzzi L, Bergman W, Bruno W, Chan M, Cuellar F, Debniak T, Pjanova D, Ertmanski S, Figl A, Gonzalez M, Hayward NK, Hocevar M, Kanetsky PA, Leachman SA, Heisele O, Palmer J, Peric B, Puig S, Schadendorf D, Gruis NA, Newton-Bishop J, Brandberg Y. Predictors of sun protection behaviors and severe sunburn in an international online study. Cancer Epidemiol Biomarkers Prev. 2010 Sep;19(9):2199–210. doi: 10.1158/1055-9965.EPI-10-0196. http://cebp.aacrjournals.org/cgi/pmidlookup?view=long&pmid=20643826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Brinker TJ, Seeger W. Photoaging mobile apps: a novel opportunity for smoking cessation? J Med Internet Res. 2015 Jul 27;17(7):e186. doi: 10.2196/jmir.4792. http://www.jmir.org/2015/7/e186/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Brinker TJ, Seeger W, Buslaff F. Photoaging mobile apps in school-based tobacco prevention: the mirroring approach. J Med Internet Res. 2016 Jun 28;18(6):e183. doi: 10.2196/jmir.6016. http://www.jmir.org/2016/6/e183/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Burford O, Jiwa M, Carter O, Parsons R, Hendrie D. Internet-based photoaging within Australian pharmacies to promote smoking cessation: randomized controlled trial. J Med Internet Res. 2013 Mar 26;15(3):e64. doi: 10.2196/jmir.2337. http://www.jmir.org/2013/3/e64/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jiwa M, Burford O, Parsons R. Preliminary findings of how visual demonstrations of changes to physical appearance may enhance weight loss attempts. Eur J Public Health. 2015 Apr;25(2):283–5. doi: 10.1093/eurpub/cku249. [DOI] [PubMed] [Google Scholar]
- 46.Brinker TJ, Owczarek AD, Seeger W, Groneberg DA, Brieske CM, Jansen P, Klode J, Stoffels I, Schadendorf D, Izar B, Fries FN, Hofmann FJ. A medical student-delivered smoking prevention program, education against tobacco, for secondary schools in germany: randomized controlled trial. J Med Internet Res. 2017 Jun 06;19(6):e199. doi: 10.2196/jmir.7906. http://www.jmir.org/2017/6/e199/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Brinker TJ, Enk A, Gatzka M, Nakamura Y, Sondermann W, Omlor AJ, Petri MP, Karoglan A, Seeger W, Klode J, von Kalle C, Schadendorf D. A dermatologist's ammunition in the war against smoking: a photoaging app. J Med Internet Res. 2017 Sep 21;19(9):e326. doi: 10.2196/jmir.8743. http://www.jmir.org/2017/9/e326/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Williams AL, Grogan S, Clark-Carter D, Buckley E. Impact of a facial-ageing intervention versus a health literature intervention on women's sun protection attitudes and behavioural intentions. Psychol Health. 2013;28(9):993–1008. doi: 10.1080/08870446.2013.777965. [DOI] [PubMed] [Google Scholar]
- 49.Lo PL, Chang P, Taylor MF. Young Australian adults' reactions to viewing personalised UV photoaged photographs. Australas Med J. 2014;7(11):454–61. doi: 10.4066/AMJ.2014.2253. http://europepmc.org/abstract/MED/25550717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Robinson JK, Wayne JD, Martini MC, Hultgren BA, Mallett KA, Turrisi R. Early detection of new melanomas by patients with melanoma and their partners using a structured skin self-examination skills training intervention: a randomized clinical trial. JAMA Dermatol. 2016 Sep 01;152(9):979–85. doi: 10.1001/jamadermatol.2016.1985. http://europepmc.org/abstract/MED/27367303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.D'Orazio J, Jarrett S, Amaro-Ortiz A, Scott T. UV radiation and the skin. Int J Mol Sci. 2013 Jun 07;14(6):12222–48. doi: 10.3390/ijms140612222. http://www.mdpi.com/resolver?pii=ijms140612222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kammeyer A, Luiten RM. Oxidation events and skin aging. Ageing Res Rev. 2015 May;21:16–29. doi: 10.1016/j.arr.2015.01.001. [DOI] [PubMed] [Google Scholar]
- 53.Brinker TJ, Stamm-Balderjahn S, Seeger W, Klingelhöfer D, Groneberg DA. Education Against Tobacco (EAT): a quasi-experimental prospective evaluation of a multinational medical-student-delivered smoking prevention programme for secondary schools in Germany. BMJ Open. 2015 Sep 18;5(9):e008093. doi: 10.1136/bmjopen-2015-008093. http://bmjopen.bmj.com/cgi/pmidlookup?view=long&pmid=26384722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Detert H, Hedlund S, Anderson CD, Rodvall Y, Festin K, Whiteman DC, Falk M. Validation of sun exposure and protection index (SEPI) for estimation of sun habits. Cancer Epidemiol. 2015 Dec;39(6):986–93. doi: 10.1016/j.canep.2015.10.022. https://linkinghub.elsevier.com/retrieve/pii/S1877-7821(15)00233-7. [DOI] [PubMed] [Google Scholar]
- 55.Hoffmann W, Latza U, Terschüren C, Deutsche Arbeitsgemeinschaft für Epidemiologie (DAE)‚ Deutsche Gesellschaft für Medizinische Informatik‚ Biometrie und Epidemiologie (GMDS)‚ Deutsche Gesellschaft für Sozialmedizin und Prävention (DGSMP)‚ Deutsche Region der Internationalen Biometrischen Gesellschaft (DR-IBS) [Guidelines and recommendations for ensuring Good Epidemiological Practice (GEP) -- revised version after evaluation] Gesundheitswesen. 2005 Mar;67(3):217–25. doi: 10.1055/s-2004-813850. [DOI] [PubMed] [Google Scholar]
- 56.Roider EM, Fisher DE. Red hair, light skin, and UV-independent risk for melanoma development in humans. JAMA Dermatol. 2016 Jul 01;152(7):751–3. doi: 10.1001/jamadermatol.2016.0524. http://europepmc.org/abstract/MED/27050924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ghiasvand R, Rueegg CS, Weiderpass E, Green AC, Lund E, Veierød MB. Indoor tanning and melanoma risk: long-term evidence from a prospective population-based cohort study. Am J Epidemiol. 2017 Dec 01;185(3):147–156. doi: 10.1093/aje/kww148. [DOI] [PubMed] [Google Scholar]
- 58.Wu S, Cho E, Li W, Weinstock MA, Han J, Qureshi AA. History of severe sunburn and risk of skin cancer among women and men in 2 prospective cohort studies. Am J Epidemiol. 2016 May 01;183(9):824–33. doi: 10.1093/aje/kwv282. http://europepmc.org/abstract/MED/27045074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Cotes ME, Albers LN, Sargen M, Chen SC. Diagnostic accuracy of teledermatology for nonmelanoma skin cancer: can patients be referred directly for surgical management? J Am Acad Dermatol. 2017 Sep 22;pii: S0190-9622(17):32434–32439. doi: 10.1016/j.jaad.2017.09.029. [DOI] [PubMed] [Google Scholar]
- 60.Dias P, Timm R, Siqueira E, Sparenberg A, Rodrigues C, Goldmeier S. Implementation and assessment of a tele-dermatology strategy for identification and treatment of skin lesions in elderly people. J Int Soc Telem eHealth (GKR) 2017;5:e19. [Google Scholar]
- 61.Dorairaj JJ, Healy GM, McInerney A, Hussey AJ. Validation of a melanoma risk assessment smartphone application. Dermatol Surg. 2017 Feb;43(2):299–302. doi: 10.1097/DSS.0000000000000916. [DOI] [PubMed] [Google Scholar]
- 62.Ngoo A, Finnane A, McMeniman E, Tan J, Janda M, Soyer HP. Efficacy of smartphone applications in high-risk pigmented lesions. Australas J Dermatol. 2017 Feb 27; doi: 10.1111/ajd.12599. [DOI] [PubMed] [Google Scholar]
- 63.Di Leo G, Liguori C, Paciello V, Pietrosanto A, Sommella P. I3DermoscopyApp: hacking melanoma thanks to IoT technologies. 50th Hawaii International Conference on System Sciences; Jan 4-7, 2017; Waikoloa Village, HI, USA. 2017. [Google Scholar]
- 64.Chao E, Meenan CK, Ferris LK. Smartphone-based applications for skin monitoring and melanoma detection. Dermatol Clin. 2017 Oct;35(4):551–557. doi: 10.1016/j.det.2017.06.014. [DOI] [PubMed] [Google Scholar]
- 65.Nabil R, Bergman W, Kukutsch NA. Conflicting results between the analysis of skin lesions using a mobile-phone application and a dermatologist's clinical diagnosis: a pilot study. Br J Dermatol. 2017 Mar 10;177(2):583–584. doi: 10.1111/bjd.15443. [DOI] [PubMed] [Google Scholar]
- 66.Harter S. The Plenum Series in Social / Clinical Psychology. Boston, MA: Springer; 1993. Causes and consequences of low self-esteem in children and adolescents; pp. 87–116. [Google Scholar]
- 67.Brinker TJ, Faria BL, Gatzka M. A skin cancer prevention photoageing intervention for secondary schools in Brazil delivered by medical students: protocol for a randomised controlled trial. BMJ Open. 2018:e018299. doi: 10.1136/bmjopen-2017-018299. (forthcoming) [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Animated version of the Sunface App effect view.


