Abstract
Among people with suicide ideation most do not attempt suicide or die by suicide. In this online study of adult US Facebook users (n=219), we examined capability for suicide, operationalized as fearlessness about death, and tolerance for psychological pain as potential variables that may explain why some people move from suicide ideation to suicidal behavior. Tolerance for psychological pain was significantly higher for participants who had never attempted suicide. Fearlessness about death was higher in participants who had attempted suicide, but not significantly. At high levels of psychological pain, one’s belief in the ability to cope with psychological pain, a dimension of tolerance for psychological pain, was lower in participants with a history of suicide attempt than in participants who had never attempted suicide. The odds of suicidal desire were almost cut in half with each unit increase in participants’ belief in their coping ability, whereas for each unit increase in fearlessness about death, the odds of suicidal desire increased by 65%. The Pearson correlation between tolerance for psychological pain and fearlessness about death was negligible. Our findings support a role for both tolerance for psychological pain and capability for suicide/fearlessness about death in the ideation-to-action framework of suicide.
Keywords: psychological pain, capability for suicide, ideation-to-action framework
1. Introduction
Clinical experience shows that among individuals with thoughts of suicide, most do not die by suicide (American Psychiatric Association, 2003; May and Klonsky, 2016). A reason why some and not others engage in suicidal behavior may be found in the individual ability to bear psychological pain, which is central to many theories that describe why people attempt and die by suicide (Baumeister, 1990; Leenaars, 1996; Maltsberger, 2004; Shneidman, 1993). Psychological pain is the extremely unpleasant feeling that results from unmet psychological needs, such as love, affiliation, achievement, and avoiding harm or shame (Shneidman, 1998, 1996). The importance of tolerance for psychological pain in the etiology of suicide was underscored by studying the motives for suicide attempts and analysis of suicide notes, which found escape from unbearable psychological pain to be the primary reason for suicide and suicide attempts (Chavez-Hernandez et al., 2009; May and Klonsky, 2013; O’Connor et al., 1999; Valente, 1994).
Empirical research regarding the role of tolerance for psychological pain in suicidal behavior has emerged only recently. Preliminary support for the importance of tolerance for psychological pain was found in young Israeli soldiers with low tolerance for psychological pain, who reported significantly stronger suicide ideation than soldiers with high tolerance for psychological pain, despite equally high levels of psychological pain (Shelef et al., 2015). Another study reported that tolerance for psychological pain was lower in young inpatients who had attempted suicide than in a nonclinical control group, but that tolerance for psychological pain did not contribute significantly to the prediction of suicidal behavior when controlling for psychological pain (Levinger et al., 2015). A study in a Greek general population sample reported that tolerance for psychological pain was inversely correlated with suicide risk and contributed unique variance to a regression model of suicide risk, while controlling for psychological pain (Soumani et al., 2011). Empirical data on tolerance for psychological pain are scarce and in need of additional study.
Another reason why some and not others engage in suicidal behavior is given by the interpersonal theory of suicide (Joiner, 2007; Van Orden et al., 2010), which contends that one needs to be capable of engaging in suicidal behavior. The interpersonal theory of suicide holds that the ability for suicidal behavior is acquired and arises from increased tolerance for physical pain and reduced fearlessness of death. It furthermore proposes that the capability for suicide, once acquired, is relatively stable and that the most direct way to acquire it is by engaging in suicidal behavior (e.g. preparing for an attempt, aborted suicide attempts). Empirical evidence obtained in psychiatric outpatients suggests that the capability for suicide increases with the number of suicide attempts (Van Orden et al., 2008). Furthermore, it is possible to have a capability for suicide without having a desire for suicide (Van Orden et al., 2010). It appears then that both tolerance for psychological pain and a capability for suicide affect suicidal behavior, but act during different stages of the process leading to suicide. Given a significant level of psychological pain, low tolerance for psychological pain is a necessary condition to develop a suicidal desire, whereas a high capability for suicide is necessary to actually attempt suicide. The relationship between tolerance for psychological pain and capability for suicide as well as their individual contributions to suicidal ideation and behavior have not been well studied.
The purpose of this study was to describe the relationships among tolerance for psychological pain, capability for suicide, in particular its fearlessness about death dimension, and suicidal ideation and behavior. Our hypotheses were threefold. First, we hypothesized that participants with a history of one or more suicide attempts would have lower tolerance for psychological pain and higher capability for suicide than participants who never attempted suicide. Second, we hypothesized that the relationship between suicide attempts and lower tolerance for pain would be strongest among individuals with high psychological pain. Third, for individuals who had never attempted suicide, we sought to understand the unique roles that tolerance for pain and capability for suicide might play in suicidal desire. Assuming that capability and tolerance are different constructs that may affect different stages of the suicidal process, we hypothesized that they would not be significantly correlated and that, in participants who had never attempted suicide, tolerance for psychological pain but not capability for suicide would contribute to current suicidal desire. Clarifying the role of these constructs in suicidal behavior will benefit our efforts to reduce suicide by enabling more precision-based targets for prevention efforts with individuals at risk for suicide.
2. Methods
2.1. Participants
We collected data from adult Facebook users in the United States (US), who responded to advertisements that invited them to complete an anonymous online survey. A similar approach was used successfully to collect data on suicidal behavior in an Australian online sample (Batterham et al., 2015). To draw people’s attention, ad texts focused on the link between psychological pain and suicide, the prevalence of suicide and suicide attempts, or that someone close to them may be experiencing unbearable pain. Another ad indicated that people of any race/ethnicity could participate, regardless of whether they were experiencing psychological pain. In addition, all ads showed a map of the United States and indication that this was a national survey. Inclusion criteria were being at least 18 years old, resident of the United States, and the ability to read and understand English. Of 708 individuals who visited the survey website, 389 (55%) provided consent to participate. Among those who consented, 133 (34%) individuals did not submit their responses. Final analysis was done on 219 respondents with complete tolerance for psychological pain and capability for suicide data.
Table 1 shows sociodemographic and clinical characteristics of respondents. Compared to the 2010 U.S. census records (U.S. Census Bureau, 2016), our sample was younger and more often female. Regarding race, our sample was less often of white or Asian descent and more often of Black/African American, American Indian/Alaska Native, Native Hawaiian and other Pacific Islander, or of mixed descent. In our sample, 7% of respondents reported having attempted suicide during the past year and 20% reported having a mental illness. This compares to data from U.S. adults, indicating 0.6% having attempted suicide during the past year and 18.5% having any mental illness (Substance Abuse and Mental Health Services Administration, 2014).
Table 1.
Characteristics of participants with and without a wish to be dead during the past week.
| Current Wish to be Dead | Total (N = 218)a |
|||
|---|---|---|---|---|
| No (n = 168) |
Yes (n = 50) |
|||
| Mean age in years (SD) | 34.0 (15.8) | 26.5 (12.3) | 32.3 (15.3) | t = 3.564 *** |
| Gender | χ2 = 4.086b | |||
| Male | 65 | 25 | 90 | |
| Female | 100 | 23 | 123 | |
| Do not use either label | 2 | 2 | 4 | |
| Race | χ2 = 0.886b | |||
| American Indian/Alaska Native | 5 | 2 | 7 | |
| Asian | 3 | 1 | 4 | |
| Native Hawaiian/other PI | 2 | 0 | 2 | |
| Black/African American | 24 | 6 | 30 | |
| White | 101 | 30 | 131 | |
| Mixed | 15 | 4 | 19 | |
| Hispanic/Latino Ethnicity | χ2 = 0.259 | |||
| No | 123 | 35 | 158 | |
| Yes | 44 | 15 | 59 | |
| English as first language | χ2 = 0.065 | |||
| No | 26 | 7 | 33 | |
| Yes | 142 | 43 | 185 | |
| Diagnosed with mental illness | χ2 = 7.688 ** | |||
| No | 141 | 33 | 174 | |
| Yes | 27 | 17 | 44 | |
| Experienced psychological pain | χ2 = 11.39b ** | |||
| Past week | 101 | 42 | 143 | |
| Past month | 17 | 1 | 18 | |
| Past year | 21 | 5 | 26 | |
| Longer ago | 29 | 2 | 31 | |
| Worst psychological pain | χ2 = 13.81b ** | |||
| Past week | 16 | 13 | 29 | |
| Past month | 26 | 8 | 34 | |
| Past year | 43 | 17 | 60 | |
| Longer ago | 80 | 12 | 92 | |
| History of suicide attempts | χ2 = 14.50 *** | |||
| No | 138 | 28 | 166 | |
| Yes | 30 | 22 | 52 | |
Note. PI: Pacific Islander.
counts do not always add up to N due to missing data.
test included cells with expected counts less than 5.
p < .01,
p < .001.
2.2. Measures
To ease participants into more sensitive survey content that could create anxiety or avoidance, the survey questions were administered in order from least to most sensitive. The survey started with demographic questions and asked whether participants had been diagnosed with a mental illness. It then continued with scales for psychological pain and tolerance for psychological pain (described below). At this point, participants were asked when they had last experienced psychological pain and when they had experienced their worst psychological pain (past week, month, year, or longer ago). The survey then asked about their history of suicide attempts and current suicidal desire. Suicidal desire was operationalized as the response to the question “During the past week, including today, did you seriously wish you were dead?” The ‘wish to be dead’ criterion was used, as it often features among initial questions to assess suicide risk; for example, in the Columbia Suicide Severity Rating scale (Posner et al., 2011) and in the MINI Neuropsychiatric interview (Sheehan et al., 1998). The survey ended with fearlessness about death questions, using the scale described below.
2.2.1. Tolerance for mental pain scale
Tolerance for psychological pain was assessed with the Tolerance for Mental Pain Scale ([TMPS], Orbach et al., 2004). The TMPS consists of 20 self-rated statements about the psychological pain experience (e.g. “I believe that my pain will go away”, “I think about the pain all the time”, “I feel that I must get rid of the pain immediately”). Factor analysis has revealed three underlying factors of the TMPS: “Surfeit of pain”, “Belief in the ability to cope with the pain”, and “Containing the pain”. Respondents endorse items on a 5-point scale ranging from “Not true” to “Very true”, which corresponds to a value of 1 – 5. Factor scores are obtained by summing individual item scores, while accounting for reverse items, and dividing by the number of items per factor. A higher average score indicates higher tolerance for psychological pain.
The TMPS was developed and tested in three samples of adolescents and young adults ranging in age from 13 to 23 and included high school students and psychiatric inpatients (M. Mikulincer, personal communication, October 21, 2014). The three factors accounted for 72% of the variance in tolerance for psychological pain. Cronbach’s α, a measure of internal consistency reliability, was .91 for “Surfeit of pain”, .81 for “Belief in the ability to cope with the pain”, and .71 for “Containing the pain”. Levinger et al. (2015) reported Cronbach’s α for the TMPS between .83 – .93 for graduate students and young psychiatric inpatients, and Soumani et al. (2011) reported .72 – .87 in general population adults. We found Cronbach’s α of .93, .79, and .61 for “Surfeit of pain”, “Belief in the ability to cope with the pain”, and “Containing the pain”, respectively. As internal consistency reliability below .7 is typically considered unacceptable (Cicchetti, 1994), we calculated a total TMPS score by averaging over the first two factors only.
2.2.2. Acquired capability for suicide scale – fearlessness about death
Capability for suicide was assessed with the Acquired Capability for Suicide Scale - Fearlessness about Death (Ribeiro et al., 2014). The ACSS-FAD is a refinement of earlier ACSS versions and was developed in the context of the interpersonal theory of suicide. Its seven self-rated statements specifically assess the fearlessness-about-death dimension of a capability for suicide (e.g. “I am not at all afraid to die”, “The pain involved in dying frightens me”). Items are endorsed on a 5-point Likert scale ranging from “Not at all like me” to “Very much like me”, which corresponds to a value of 0 – 4. A total score is obtained by summing individual item scores, while accounting for reverse items, and dividing by the number of items. A higher score indicates a higher capability for suicide.
Adequate to good internal consistency reliability was observed with this scale in multiple samples of undergraduate students (Cronbach’s α: .77 – .85), an inpatient sample (Cronbach’s α: 0.81), and a general population sample (Cronbach’s α: 0.76) (Ribeiro et al., 2014). Cronbach’s α was .73 in our sample.
2.2.3. Psychache scale
Psychological pain was assessed on the Psychache Scale, which describes psychological pain as “a hurting feeling inside, often described as pain you feel in your heart or mind. It indicates how much you hurt emotionally or mentally” (Holden et al., 2001). The PS has 13 items with higher scores reflecting greater psychological pain. Nine items are scored on a 5-point frequency scale ranging from never to always, corresponding to a value of 1 – 5. Four more items, reflecting pain intensity, are scored on a 5-point symmetrical scale ranging from strongly disagree to strongly agree, also corresponding to a value of 1 – 5. The total score is obtained by summing the item scores, resulting in a total score between 13 and 65.
The Psychache Scale is well validated in diverse populations, including university students, homeless men, outpatients with depression, and male prison inmates (Li et al., 2014; Mills et al., 2005; Patterson and Holden, 2012; Troister and Holden, 2012; Xie et al., 2014). In terms of reliability, we found excellent internal consistency for our sample with Cronbach’s α = .96.
2.3. Procedure
Data were collected from September 2015 – June 2016. We used Research Electronic Data Capture (REDCap™) to develop our online survey and collect the data. REDCap™ is a secure and HIPAA-compliant electronic data capture tool (Harris et al., 2009). Visitors to the survey web site first arrived on the informed consent page, describing the nature of the survey and resources available to them should the survey make them feel uncomfortable or upset (e.g. the National Suicide Prevention Lifeline phone number). By submitting their age, city, and ZIP code on the consent page, respondents self-identified as being eligible and initiated the actual survey. To boost response rate, respondents were offered a choice to participate in a drawing to win a $50 debit card upon completion of the survey.
As this was an anonymous survey and respondents could submit their data more than once, even though they were instructed not to, we developed an algorithm to search the data for potential duplicate entries. The algorithm compared age, gender, city, and ZIP code. We then manually compared these entries and retained the first entry without missing data. Of potential duplicates identified by the algorithm, five entries were considered actual duplicates and discarded. The Institutional Review Board at the University of California, San Francisco, approved the study (IRB# 16-18686).
2.4. Data analysis
Both the TMPS score and ACSS-FAD score were found to be normally distributed, allowing for parametric analysis. To test hypothesis 1, we used 2 × 2 ANOVAs, with TMPS and ACSS-FAD as dependent variables and gender (male/female) and a history of suicide attempts (yes/no) as between-group factors. Gender was included because differences have been reported, with men indicating higher fearlessness about death than women (Ribeiro et al., 2014; Spangenberg et al., 2016). We tested hypothesis 2 with a 2 × 3 ANOVA, with tolerance for psychological pain as the dependent variable and psychological pain level (low, medium, high) and a history of suicide attempts (yes/no) as between-group factors. We differentiated the low-pain group (n=141) as having a Psychache Scale score < 37, on the basis of a cutoff value for current suicide ideation published elsewhere (Meerwijk and Weiss, 2017). The high-pain group (n=36) was defined as having a Psychache Scale score ≥ 46, based on preliminary data obtained in the same sample to establish a cutoff value that identified participants with current suicide ideation and a suicide attempt during the past year. The remaining participants comprised the medium-pain group (n=33). Our third hypothesis was addressed with Pearson correlations, and binomial logistic regression with current suicidal desire as dichotomous dependent variable (yes/no), while controlling for psychological pain and other covariates. R version 3.4.0 was used for all analyses, and statistical significance was assumed at p < .05.
3. Results
Table 2 shows TMPS and ACSS-FAD scores for participants with and without a history of suicide attempt. Hypothesis 1 was partially supported. TMPS was significantly higher for participants who had never attempted suicide (3.49 [SD .73] vs. 2.88 [SD .71], t = 5.39, p < .0001). As expected, a significant main effect of gender did exist for ACSS-FAD (F(1,215) = 6.38, p = .01), with lower scores for female participants (see Table 2); no interaction between gender and attempt status was observed (F(1,215) = 0.003, p = .96). Across both genders, the ACSS-FAD score was higher in participants who had attempted suicide, but not significantly (F(1,215) = 2.72, p = .10, Cohen’s d = 0.28).
Table 2.
Mean (SD) instrument scores by gender and suicide attempt history (N = 219)
| No Attempts | One or More Attempts | Total | |||
|---|---|---|---|---|---|
| Male (n = 69) | Female (n = 97) | Male (n = 24) | Female (n = 29) | ||
| TMPS | 3.53 (0.58) | 3.45 (0.82) | 2.76 (0.67) | 2.97 (0.74) | 3.34 (0.77) |
| Surfeit of pain | 3.72 (0.97) | 3.46 (1.11) | 2.55 (0.82) | 2.80 (0.95) | 3.36 (1.09) |
| Cope with pain | 3.34 (0.99) | 3.44 (0.98) | 2.97 (0.89) | 3.14 (0.81) | 3.32 (0.96) |
| ACSS-FAD | 2.41 (0.95) | 2.11 (0.86) | 2.66 (0.71) | 2.34 (0.99) | 2.30 (0.91) |
| PSa | 25.0 (11.2) | 29.6 (13.4) | 41.4 (11.0) | 37.6 (10.2) | 30.4 (13.2) |
Note. TMPS: Tolerance for Mental Pain Scale, ACSS-FAD: Acquired Capability for Suicide – Fearlessness about Death, PS: Psychache Scale.
N = 210 due to missing data.
When Hypothesis 2 was tested, significant main effects were observed in tolerance for psychological pain for both pain level (F(2,204) = 50.44, p < .0001) and attempt status (F(1,204) = 6.59, p = .01). See Figure 1. However, no interaction was observed between attempt and psychological pain level (F(2,204) = 0.15, p = .86). Scheffe post-hoc comparisons showed that TMPS scores in the low pain group were significantly higher than in the medium pain group (3.65 [SD 0.63] vs. 2.94 [SD 0.50], p = .002), and that TMPS scores in the medium pain group were significantly higher than in the high pain group (2.94 [SD 0.50] vs. 2.45 [SD 0.61], p = .03). A strong inverse correlation between psychological pain and the TMPS ‘Surfeit of Pain’ factor (r = − .85, p < .0001) prompted us to conduct a similar analysis of the TMPS score without the ‘Surfeit of Pain’ score. Note that this essentially reduced the TMPS score to the ‘Belief in the Ability to Cope with Pain’ factor score in our sample. While no significant interaction was observed between attempt status and psychological pain level (F(2,204) = 1.49, p = 0.23), the interaction plot (see Figure 2) suggested that at high psychological pain, ‘Belief in the Ability to Cope with Pain’ was lower in participants with a history of suicide attempt than in participants who never attempted suicide (Cohen’s d = 0.69), whereas a negligible difference appeared to exist between the two groups in participants with low psychological pain (Cohen’s d = 0.03). At medium psychological pain, the observed effect size was 0.51.
Figure 1.
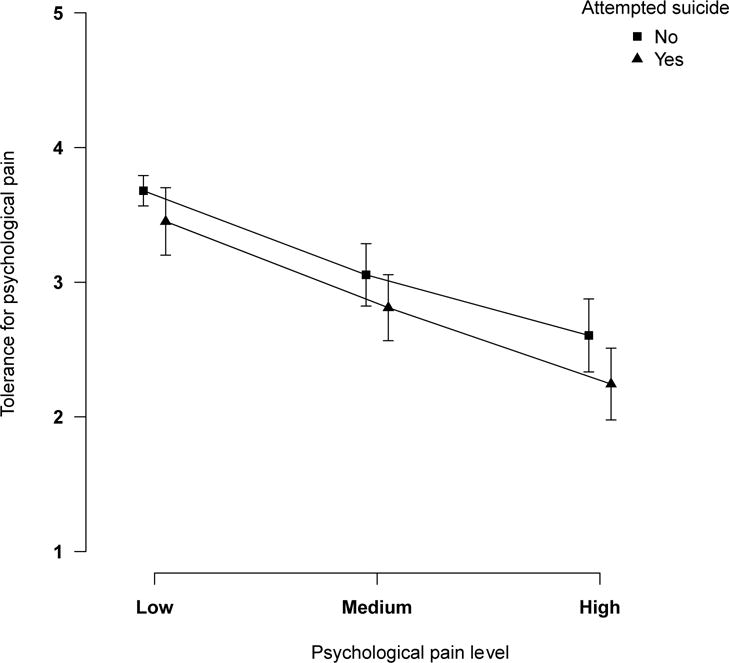
Tolerance for psychological pain by attempt status and psychological pain level. Error bars indicate one standard error of the mean.
Figure 2.
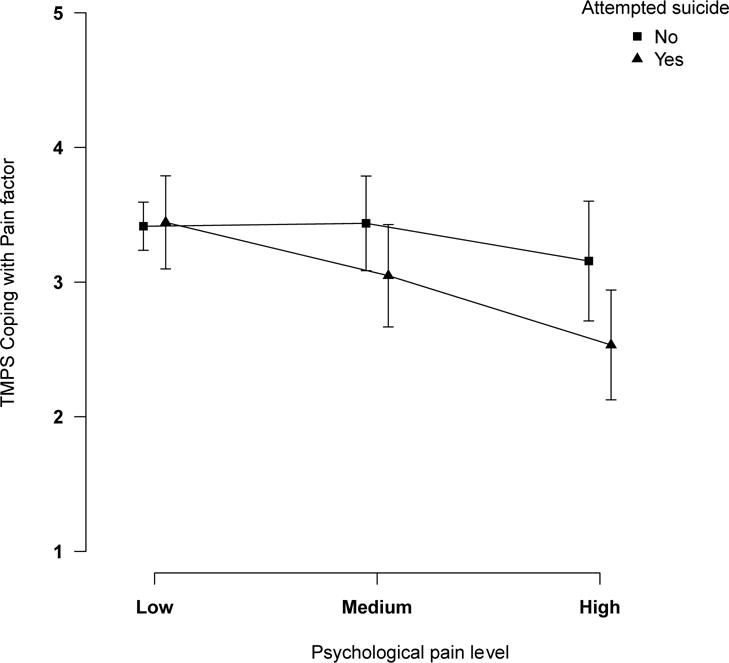
Belief in the ability to cope with psychological pain by attempt status and psychological pain level. Error bars indicate one standard error of the mean. TMPS: Tolerance for Mental Pain Scale
Given our preliminary findings, which showed a strong inverse relationship between psychological pain and the TMPS ‘Surfeit of Pain’ factor, as well as the weak internal reliability of the TMPS ‘Containing the Pain’ factor, we used only the ‘Belief in the Ability to Cope with the Pain’ factor to test Hypothesis 3. Use of this single factor increased the potential for having a reliable and valid measure of tolerance for psychological pain in our sample. Results for the logistic regression of current suicidal desire among participants who never attempted suicide are shown in Table 3. Age, psychological pain score, recency of worst psychological pain (reference: past week), and diagnosis of mental illness (yes/no) were entered as covariates in the first block, as they were found to differ significantly between participants with and without a suicidal desire. To avoid issues of collinearity with the psychological pain score, we did not include the variable indicating when participants last experienced any psychological pain in the regression analysis, but we did include when they experienced their worst psychological pain. In the second block, the TMPS ‘Belief in the Ability to Cope with the Pain’ and ACSS-FAD scores were added and contributed significantly to the model (χ2 = 6.95, p = .03). Wald tests for individual contributions indicated that they both contributed to suicidal desire, with ACSS-FAD only just above our level of significance. With each unit increase in TMPS ‘Belief in the Ability to Cope with the Pain’, the odds of suicidal desire were almost cut in half (OR = 0.55, p = .03), whereas for each unit increase in ACSS-FAD, the odds of suicidal desire increased by 65% (OR = 1.65, p = .06). The Pearson correlation examining the relationship between tolerance for psychological pain (TMPS score) and capability for suicide (ACSS-FAD score) was negligible and not significant (r = .04, p = .54).
Table 3.
Logistic Regression Predicting Suicidal Desire in Participants who Never Attempted Suicide (n = 166)
| OR | 95% CI | ||
|---|---|---|---|
| Age | 0.96* | 0.91 | 0.99 |
| Psychological pain | 1.05* | 1.01 | 1.10 |
| Diagnosed with mental illnessa | 2.15 | 0.54 | 8.56 |
| Worst psychological pain:b | |||
| past month | 0.70 | 0.15 | 3.18 |
| past year | 0.95 | 0.24 | 4.09 |
| Longer ago | 0.47 | 0.11 | 2.16 |
| TMPS Coping with Pain factor | 0.55* | 0.31 | 0.94 |
| ACSS-FAD | 1.65 | 1.00 | 2.83 |
Note. The overall model was significant (χ2 = 36.56, p < .0001), indicating that the predictors significantly distinguished participants with and without suicidal desire. OR: Odds Ratio, TMPS: Tolerance for Mental Pain Scale, ACSS-FAD: Acquired Capability for Suicide – Fearlessness about Death.
reference “No”,
reference “Past week”.
p < .05
4. Discussion
The purpose of this study was to describe the relationships among tolerance for psychological pain and capability for suicide/fearlessness about death with respect to suicide ideation and suicide attempts in general population adults. In line with findings reported by Shelef et al. (2015), our data indicated that participants with a history of one or more suicide attempts have lower tolerance for psychological pain than participants who never attempted suicide, and support the notion that suicidal behavior in response to psychological pain may depend, at least in part, on the ability to cope with psychological pain (Shneidman, 1993). While not statistically significant, less belief in one’s ability to cope with psychological pain suggested a greater risk for suicide attempts for individuals with high levels of psychological pain (medium effect size, d=0.69) than for individuals with less psychological pain.
The relationship between the fear about death dimension of a capability for suicide and a suicide attempt history was less pronounced, albeit in the expected direction. Participants with one or more suicide attempts reported greater fearlessness about death, that is higher capability for suicide, than those who had never attempted suicide; but this difference was not statistically significant and represented only a small effect. The negligible correlation between fearlessness about death and tolerance for psychological pain did corroborate our hypothesis that they are different constructs and suggests that each has a potentially unique role in the etiology of suicide. This is further supported by our finding that they both made unique contributions to a model that distinguished participants based on their current suicide ideation. Of note, severity of psychological pain also contributed significantly to this model of suicide ideation. Psychological pain severity and capability for suicide feature prominently in the three-step theory of suicide (Klonsky and May, 2015). Klonsky and May (2015) reported a small correlation between the level of psychological pain and an earlier version of the acquired capability for suicide scale. It is also noteworthy that they further distinguished a capability for suicide into a dispositional dimension (e.g. genetically determined pain sensitivity), an acquired dimension, and a practical dimension (e.g. having access to means). In our study, only the acquired dimension was addressed with fearlessness about death.
Although research indicates that people can have a capability for suicide and not be suicidal (Van Orden et al., 2010), our data suggest that a substantial level of fearlessness about death contributes to suicide ideation. We controlled for a history of suicide attempt in our analysis, but an ability for suicide can evolve in many ways that habituate people to pain and fear of death; for example, through exposure to violence and abuse, or nonsuicidal self-harm (Joiner, 2007). Our operationalization of a capability for suicide focused on the fearlessness about death dimension, while an ability for suicide is also affected by tolerance for physical pain (Van Orden et al., 2010). Research has shown that physical pain tolerance accounts for significant variance in the association between these painful experiences and capability for suicide (Franklin et al., 2011). It has also been suggested that physical pain tolerance plays a role in the lethality of suicidal acts (George et al., 2016; Van Orden et al., 2010).
Limitations of our study include that the sample was restricted to adult US Facebook users and that our survey, as is generally the case with surveys, may be affected by recall bias. The latter may apply in particular to the questions asking participants when they last experienced psychological pain or when they experienced their worst psychological pain. Furthermore, our operationalization of suicidal desire was based on a single question only. It does not, for example, distinguish between an active and passive suicidal desire. Also, our question about mental illness did not distinguish between current or lifetime diagnosis of mental illness. Comparison of our sample’s responses to census data suggests that participants interpreted the question as currently diagnosed with mental illness. Our study sample appeared more vulnerable than the US population in general (i.e. a higher prevalence of mental illness and particularly prior suicide attempts). However, the average tolerance for psychological pain was only slightly less than reported for a Greek general population sample (Soumani et al., 2011), and almost a full point lower than reported in healthy Israeli adolescents and young adults (Levinger et al., 2015). The average fearlessness about death score in our sample was lower than scores obtained both in undergraduate student samples and in psychiatric inpatients (Ribeiro et al., 2014), indicating lower capability for suicide in our sample. But we do not recommend generalizing our results to general population US adults until further research occurs with a larger sample that is more broadly distributed on suicide risk.
Our findings indicate potential reliability and validity issues with the TMPS, and we recommend additional psychometric analysis (e.g. factor analysis) of this instrument in the general population. Although adequate internal consistency reliability has been reported for the TMPS ‘Containing the Pain’ factor (Levinger et al., 2015; Soumani et al., 2011), we found a low Cronbach’s α, despite what seems an adequate sample size. The ‘Surfeit of Pain’ factor of the TMPS correlated strongly with our measure of psychological pain, suggesting that it assessed level of pain rather than tolerance. Thus, we ran parts of our analysis using only the TMPS ‘Belief in the Ability to Cope with the Pain’ factor. While this operationalization of tolerance for psychological pain may be questioned, it can be argued that the ability to cope with pain represents the essence of tolerance.
Overall, our findings provide corroborating evidence that both tolerance for psychological pain and capability for suicide, operationalized as fearlessness about death, play a role in the process that triggers suicidal thoughts and behaviors. In addition to psychological pain and other well-known suicide risk factors (see for example Rizvi et al., 2017; Turecki and Brent, 2016; Verrocchio et al., 2016), tolerance for psychological pain and capability for suicide/fearlessness about death may be factors to consider when assessing suicide risk. However, we recommend additional research to corroborate our findings before applying them in a clinical setting.
Highlights.
Compared to people who did not attempt suicide, tolerance for psychological pain was lower in people who did attempt suicide.
Comparing groups at high psychological pain, tolerance for psychological pain was lower in people who did attempt suicide.
Capability for suicide, operationalized as fearlessness about death, and tolerance for psychological pain were not correlated.
Both tolerance for psychological pain and capability for suicide contributed to a model of suicidal desire.
Acknowledgments
This research was supported by the National Institute of Nursing Research Grant No. T32 NR07088.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Psychiatric Association. Practice Guideline for the Assessment and Treatment of Patients with Suicidal Behaviors. author; Arlington: 2003. [PubMed] [Google Scholar]
- Batterham PJ, Calear AL, van Spijker BAJ. The Specificity of the Interpersonal-Psychological Theory of Suicidal Behavior for Identifying Suicidal Ideation in an Online Sample. Suicide Life-Threatening Behav. 2015;45:448–460. doi: 10.1111/sltb.12140. https://doi.org/10.1111/sltb.12140. [DOI] [PubMed] [Google Scholar]
- Baumeister RF. Suicide as escape from self. Psychol Rev. 1990;97:90–113. doi: 10.1037/0033-295x.97.1.90. [DOI] [PubMed] [Google Scholar]
- Chavez-Hernandez AM, Leenaars AA, Chavez-de Sanchez MI, Leenaars L. Suicide notes from Mexico and the United States: a thematic analysis. Salud Publica Mex. 2009;51:314–320. doi: 10.1590/s0036-36342009000400008. [DOI] [PubMed] [Google Scholar]
- Cicchetti DV. Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychol Assess. 1994;6:284–290. [Google Scholar]
- Franklin JC, Hessel ET, Prinstein MJ. Clarifying the role of pain tolerance in suicidal capability. Psychiatry Res. 2011;189:362–7. doi: 10.1016/j.psychres.2011.08.001. https://doi.org/10.1016/j.psychres.2011.08.001. [DOI] [PubMed] [Google Scholar]
- George SE, Page AC, Hooke GR, Stritzke WGK. Multifacet assessment of capability for suicide: Development and prospective validation of the Acquired Capability With Rehearsal for Suicide Scale. Psychol Assess. 2016;28:1452–1464. doi: 10.1037/pas0000276. https://doi.org/10.1037/pas0000276. [DOI] [PubMed] [Google Scholar]
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–81. doi: 10.1016/j.jbi.2008.08.010. https://doi.org/10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holden RR, Mehta K, Cunningham EJ, McLeod LD. Development and preliminary validation of a scale of psychache. Can J Behav Sci. 2001;33:224–232. [Google Scholar]
- Joiner TE. Why people die by suicide. Harvard University Press; Cambridge, MA: 2007. [Google Scholar]
- Klonsky ED, May AM. The Three-Step Theory (3ST): A New Theory of Suicide Rooted in the “Ideation-to-Action” Framework. Int J Cogn Ther. 2015;8:114–129. https://doi.org/10.1521/ijct.2015.8.2.114. [Google Scholar]
- Leenaars AA. Suicide: a multidimensional malaise. Suicide Life-Threatening Behav. 1996;26:221–236. [PubMed] [Google Scholar]
- Levinger S, Somer E, Holden RR. The importance of mental pain and physical dissociation in youth suicidality. J trauma dissociation. 2015;16:322–39. doi: 10.1080/15299732.2014.989644. https://doi.org/10.1080/15299732.2014.989644. [DOI] [PubMed] [Google Scholar]
- Li H, Xie W, Luo X, Fu R, Shi C, Ying X, Wang N, Yin Q, Wang X. Clarifying the role of psychological pain in the risks of suicidal ideation and suicidal acts among patients with major depressive episodes. Suicide Life Threat Behav. 2014;44:78–88. doi: 10.1111/sltb.12056. https://doi.org/10.1111/sltb.12056. [DOI] [PubMed] [Google Scholar]
- Maltsberger JT. The descent into suicide. Int J Psychoanal. 2004;85:653–667. doi: 10.1516/002075704774200799. https://doi.org/10.1516/002075704774200799. [DOI] [PubMed] [Google Scholar]
- May AM, Klonsky ED. What Distinguishes Suicide Attempters From Suicide Ideators? A Meta-Analysis of Potential Factors. Clin Psychol Sci Pract. 2016;23:5–20. https://doi.org/10.1111/cpsp.12136. [Google Scholar]
- May AM, Klonsky ED. Assessing motivations for suicide attempts: development and psychometric properties of the inventory of motivations for suicide attempts. Suicide Life Threat Behav. 2013;43:532–46. doi: 10.1111/sltb.12037. https://doi.org/10.1111/sltb.12037. [DOI] [PubMed] [Google Scholar]
- Meerwijk EL, Weiss SJ. Utility of a time frame in assessing psychological pain and suicide ideation. PeerJ. 2017;5:e3491. doi: 10.7717/peerj.3491. https://doi.org/10.7717/peerj.3491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mills JF, Green K, Reddon JR. An evaluation of the psychache scale on an offender population. Suicide Life-Threatening Behav. 2005;35:570–580. doi: 10.1521/suli.2005.35.5.570. [DOI] [PubMed] [Google Scholar]
- O’Connor RC, Sheehy NP, O’Connor DB. A thematic analysis of suicide notes. Crisis. 1999;20:106–114. doi: 10.1027//0227-5910.20.3.106. [DOI] [PubMed] [Google Scholar]
- Orbach I, Gilboa-Schechtman E, Johan M, Mikulincer M. Tolerance for Mental Pain Scale. Bar-Ilan University; Ramat-Gan, Israel: 2004. [Google Scholar]
- Patterson AA, Holden RR. Psychache and suicide ideation among men who are homeless: a test of Shneidman’s model. Suicide Life-Threatening Behav. 2012;42:147–156. doi: 10.1111/j.1943-278X.2011.00078.x. https://doi.org/10.1111/j.1943-278X.2011.00078.x. [DOI] [PubMed] [Google Scholar]
- Posner K, Brown GK, Stanley B, Brent DA, Yershova KV, Oquendo MA, Currier GW, Melvin GA, Greenhill L, Shen S, Mann JJ. The Columbia-Suicide Severity Rating Scale: initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am J Psychiatry. 2011;168:1266–1277. doi: 10.1176/appi.ajp.2011.10111704. https://doi.org/10.1176/appi.ajp.2011.10111704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ribeiro JD, Witte TK, Van Orden KA, Selby EA, Gordon KH, Bender TW, Joiner TE. Fearlessness about death: the psychometric properties and construct validity of the revision to the acquired capability for suicide scale. Psychol Assess. 2014;26:115–26. doi: 10.1037/a0034858. https://doi.org/10.1037/a0034858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rizvi SJ, Iskric A, Calati R, Courtet P. Psychological and physical pain as predictors of suicide risk: evidence from clinical and neuroimaging findings. Curr Opin Psychiatry. 2017;30:159–167. doi: 10.1097/YCO.0000000000000314. https://doi.org/10.1097/YCO.0000000000000314. [DOI] [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar GC. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 2):22–57. [PubMed] [Google Scholar]
- Shelef L, Fruchter E, Hassidim A, Zalsman G. Emotional regulation of mental pain as moderator of suicidal ideation in military settings. Eur Psychiatry. 2015;30:765–769. doi: 10.1016/j.eurpsy.2014.12.004. https://doi.org/10.1016/j.eurpsy.2014.12.004. [DOI] [PubMed] [Google Scholar]
- Shneidman ES. Perspectives on suicidology: Further reflections on suicide and psychache. Suicide Life-Threatening Behav. 1998;28:245–250. [PubMed] [Google Scholar]
- Shneidman ES. The suicidal mind. Oxford University Press; New York, NY: 1996. [Google Scholar]
- Shneidman ES. Commentary: Suicide as psychache. J Nerv Ment Dis. 1993;181:145–147. doi: 10.1097/00005053-199303000-00001. [DOI] [PubMed] [Google Scholar]
- Soumani A, Damigos D, Oulis P, Masdrakis V, Ploumpidis D, Mavreas V, Konstantakopoulos G. Mental pain and suicide risk: Application of the greek version of the Mental Pain and the Tolerance of Mental Pain scale. Psychiatriki. 2011;22:330–340. [PubMed] [Google Scholar]
- Spangenberg L, Hallensleben N, Friedrich M, Teismann T, Kapusta ND, Glaesmer H. Dimensionality, psychometric properties and population-based norms of the German version of the Revised Acquired Capability for Suicide Scale (ACSS-FAD) Psychiatry Res. 2016;238:46–52. doi: 10.1016/j.psychres.2016.01.052. https://doi.org/10.1016/j.psychres.2016.01.052. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. The NSDUH Report: Substance Use and Mental Health Estimates from the 2013 National Survey on Drug Use and Health: Overview of Findings. Rockville, MD: 2014. [PubMed] [Google Scholar]
- Troister T, Holden RR. A two-year prospective study of psychache and its relationship to suicidality among high-risk undergraduates. J Clin Psychol. 2012;68:1019–1027. doi: 10.1002/jclp.21869. https://doi.org/10.1002/jclp.21869. [DOI] [PubMed] [Google Scholar]
- Turecki G, Brent DA. Suicide and suicidal behaviour. Lancet. 2016;387:1227–39. doi: 10.1016/S0140-6736(15)00234-2. https://doi.org/10.1016/S0140-6736(15)00234-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Census Bureau. US Census Quick Facts [WWW Document] 2016 URL https://www.census.gov/quickfacts/table/PST045215/00 (accessed 5.23.16)
- Valente SM. Messages of psychiatric patients who attempted or committed suicide. Clin Nurs Res. 1994;3:316–333. doi: 10.1177/105477389400300404. https://doi.org/10.1177/105477389400300404. [DOI] [PubMed] [Google Scholar]
- Van Orden KA, Witte TK, Cukrowicz KC, Braithwaite SR, Selby EA, Joiner TE. The interpersonal theory of suicide. Psychol Rev. 2010;117:575–600. doi: 10.1037/a0018697. https://doi.org/10.1037/a0018697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Orden KA, Witte TK, Gordon KH, Bender TW, Joiner TE. Suicidal desire and the capability for suicide: tests of the interpersonal-psychological theory of suicidal behavior among adults. J Consult Clin Psychol. 2008;76:72–83. doi: 10.1037/0022-006X.76.1.72. https://doi.org/10.1037/0022-006X.76.1.72. [DOI] [PubMed] [Google Scholar]
- Verrocchio MC, Carrozzino D, Marchetti D, Andreasson K, Fulcheri M, Bech P. Mental Pain and Suicide: A Systematic Review of the Literature. Front psychiatry. 2016;7:1–14. doi: 10.3389/fpsyt.2016.00108. https://doi.org/10.3389/fpsyt.2016.00108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie W, Li H, Luo X, Fu R, Ying X, Wang N, Yin Q, Zou Y, Cui Y, Wang X, Shi C. Anhedonia and pain avoidance in the suicidal mind: behavioral evidence for motivational manifestations of suicidal ideation in patients with major depressive disorder. J Clin Psychol. 2014;70:681–92. doi: 10.1002/jclp.22055. https://doi.org/10.1002/jclp.22055. [DOI] [PubMed] [Google Scholar]


