Abstract
Pseudoaneurysm (PA) of the cystic artery is rare. Most of the reported cases are iatrogenic and develop secondary to liver biopsy, laparoscopic cholecystectomy, ERCP, and liver transplant. Other reported causes include trauma, malignancy, arteriovenous malformations, and inflammation in the hepatobiliary and pancreatic system. Cystic artery psuedoaneurysm is usually asymptomatic but may also present as vague abdominal pain, intra-abdominal mass, and hemobilia. In the event of rupture, it may present as a catastrophic intra-peritoneal bleeding with hemorrhagic shock. Doppler ultrasound and contrast-enhanced CT scan are useful tools for the diagnosis of this condition. However, selective visceral angiography is confirmatory and offers the opportunity for therapeutic embolization. We report a case which presented with upper right quadrant abdominal pain, vomiting, and hypotension. Abdominal ultrasonography revealed subhepatic hematoma and pericholecystic fluid collection along with acute calculus cholecystitis and sludge in the bile duct. Subsequent contrast-enhanced CT and CT angiography confirmed the presence of ruptured cystic artery psuedoaneurysm with subhepatic hematoma. The patient after resuscitation underwent selective visceral angiography and successful coil embolization of the cystic artery pseudoaneurysm. During the same admission, ERCP and biliary stenting were also performed followed by laparoscopic cholecystectomy. This case reports a rare entity which was successfully treated using a multimodality strategy.
Keywords: Pseudoaneurysm, Cystic artery, Embolization, Laparoscopic cholecystectomy
Case History
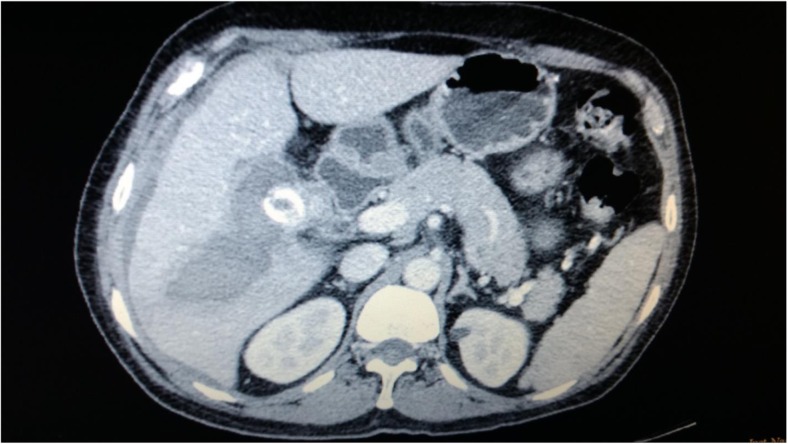
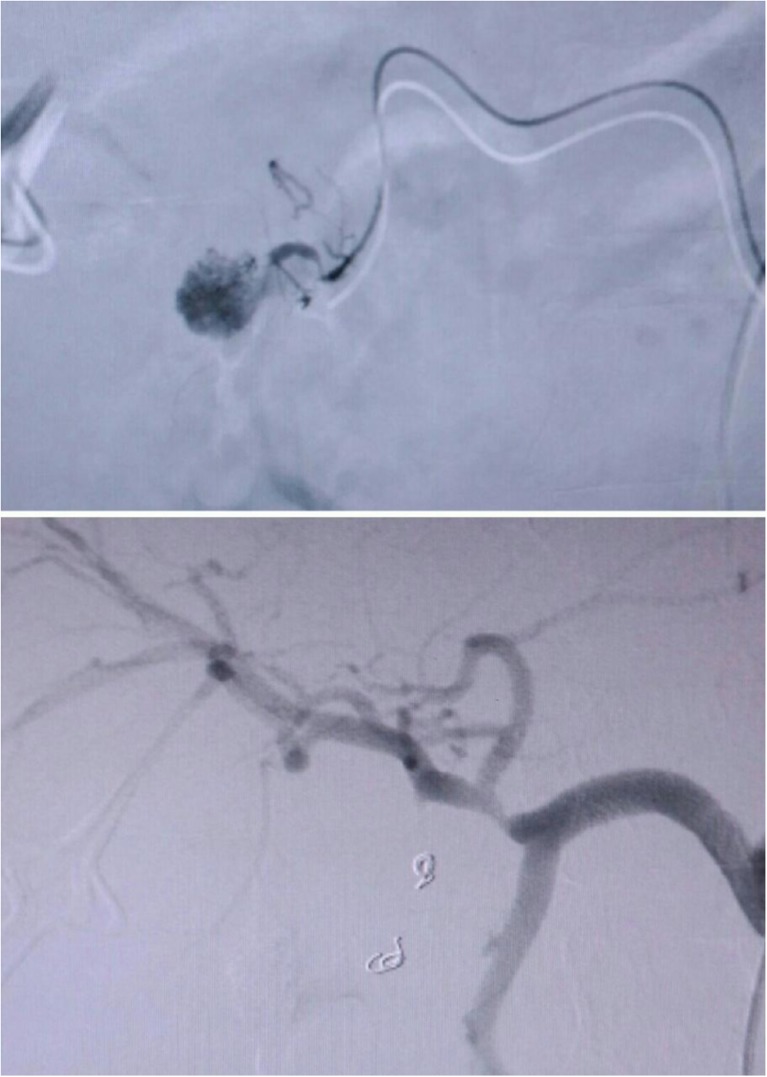
A 56-year-old gentleman presented with sudden onset of upper right quadrant abdominal pain, vomiting, and hypotension. Clinical examination revealed pallor, tachycardia, and tenderness over the right hypochondrium. Blood investigations showed low hemoglobin (8 g/dl), raised inflammatory markers (leucocytosis 13,000/dl, CRP 178 mg/L), and deranged liver enzymes. Abdominal ultrasonography showed acute calculus cholecystitis with pericholecystic collection and subhepatic hematoma. Further, abdominal contrast-enhanced CT and CT angiography revealed ruptured cystic artery pseudoaneurysm with collection of blood in the subhepatic region (Fig. 1). Magnetic resonance cholangiopancreatography (MRCP) showed multiple gall bladder calculi along with sludge in the bile duct. After initial resuscitation with intravenous fluids, selective visceral angiography was performed confirming ruptured cystic artery pseudoaneurysm which was coil embolized (Fig. 2). Subsequently, endoscopic sphincterotomy and biliary stenting were done followed by laparoscopic cholecystectomy. Biliary stent was removed after a month. At 6-month follow-up, patient remains well and asymptomatic.
Fig. 1.
CECT of whole abdomen showing brightly enhancing rounded pseudoaneurysm along with subhepatic hematoma
Fig. 2.
Digital subtraction angiography (DSA) showing pre- and post-coil embolization of cystic artery pseudoaneurysm
Discussion
Pseudoaneurysms of the visceral arteries are usually secondary to intra-abdominal inflammatory processes such as pancreatitis, cholecystitis, or other long-standing infections [1]. In recent times, iatrogenic causes, following ERCP, liver biopsy, or liver transplantation, have become the leading etiological factor for pseudoaneurysm formation. Inadvertent vascular injury during laparoscopic cholecystectomy particularly by monopolar diathermy is also an important cause for formation of pseudoaneurysm. Reports of cases of pseudoaneurysm formation are sporadic and limited to small series with varying clinical presentation ranging from mild abdominal discomfort to hemobilia or intra-peritoneal bleeding [1, 2]. Moreover, the association of cystic artery pseudoaneurysm in the presence of gallstone disease is extremely rare [3, 4]. Management of this condition has also been diverse. In one such report that described the presence of incidental cystic artery unruptured pseudoaneurysm along with acute cholecystitis, laparoscopic cholecystectomy was performed as primary definite treatment [5]. In another case presenting with hemobilia, prior embolization of cystic artery pseudoaneurysm was done followed by laparoscopic cholecystectomy [6]. Our case of ruptured cystic artery, PA with acute calculus cholecystitis was successfully treated with a multimodality management approach.
While abdominal ultrasonography is the initial investigation for gallstone disease and related complications, abdominal contrast-enhanced CT and angiography remain the preferred modality to diagnose cystic artery pseudoaneurysm [7].
Bulut et al. in their literature review reported 54 cholecystectomy-related pseudoaneurysms arising mostly from the right hepatic artery in 61% cases followed by common hepatic artery in 27% of the cases. Only one patient had cystic artery pseudoaneurysm. Therapeutic arterial embolization was performed in 82% of the cases, and the remaining 18% required surgery [1].
Although there are stray reports of successful non-operative management of traumatic hemobilia, majority recommend interventional treatment in the form of selective visceral angiography and embolization or surgery for pseudoaneurysm [8]. Selective visceral angiography along with confirming the diagnosis of cystic artery pseudoaneurysm also offers the advantage of therapeutic intervention at the same time.
In this particular case, abdominal ultrasonography showed multiple calculi in gall bladder and subhepatic hematoma which were subsequently confirmed on contrast-enhanced CT scan as ruptured cystic artery pseudoaneurysm with subhepatic hematoma. The diagnosis was reconfirmed during visceral angiography, and selective coil embolization of cystic artery pseudoaneurysm was performed at the same time. As the patient had deranged, liver function tests and MRCP showed the dilated common bile duct with presence of sludge. An ERCP was performed along with bile duct stenting with 5-French, 10-cm plastic stent. This was followed by laparoscopic cholecystectomy.
To our knowledge, this is a rare case of ruptured cystic artery pseudoaneurysm following acute calculus cholecystitis which was successfully treated with coil embolization of pseudoaneurysm followed by laparoscopic cholecystectomy during the same admission.
Conclusion
Ruptured pseudoaneurysm of cystic artery due to inflammation of biliary system is rare and requires contrast-enhanced CT and visceral angiography for establishing the diagnosis. The advent of interventional radiology has allowed minimally invasive treatment of pseudoaneurysms. Optimum outcome can be achieved with multidisciplinary approach with radiological, endoscopic, and laparoscopic intervention and is recommended.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they have no conflict of interest.
References
- 1.Bulut T, Yamaner S, Bugra D, et al. False aneurysm of hepatic artery after laparoscopic cholecystectomy. Acta Chir Belg. 2002;102(6):459–463. doi: 10.1080/00015458.2002.11679352. [DOI] [PubMed] [Google Scholar]
- 2.Madanur MA, Battula N, Sethi H et al Pseudoaneurysm following laparoscopic cholecystectomy. Hepatobiliary Pancreat Dis Int 6:294–298 [PubMed]
- 3.De Molla Neto OL, Ribeiro MAF, Saad WA. Pseudoaneurysm of cystic artery after laparoscopic cholecystectomy. HPB :Off J Int Hepato Pancreato Biliary Assoc. 2006;8(4):318–319. doi: 10.1080/13651820600869628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Petrou A, Brennan N, Soonawalla Z, et al. Hemobilia due to cystic artery stump pseudoaneurysm following laparoscopic cholecystectomy: case presentation and literature review. Int Surg. 2012;97(2):140–144. doi: 10.9738/CC52.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Loizides S, Ali A, Newton R, Singh KK. Laparoscopic management of a cystic artery pseudoaneurysm in a patient with calculus cholecystitis. Int J Surg Case Rep. 2015;14:182–185. doi: 10.1016/j.ijscr.2015.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Siddiqui NA, Chawla T, Nadeem M. Cystic artery pseudoaneurysm secondary to acute cholecystitis as cause of haemobilia. BMJ Case Rep. 2011 [DOI] [PMC free article] [PubMed]
- 7.Maeda A, Kunou T, Saeki S. Pseudoaneurysm of the cystic artery with hemobilia treated by arterial embolization and elective cholecystectomy. J Hepato-Biliary-Pancreat Surg. 2002;9(6):755–758. doi: 10.1007/s005340200105. [DOI] [PubMed] [Google Scholar]
- 8.Akatsu T, Tanabe M, Shimizu T, et al. Pseudoaneurysm of the cystic artery secondary to cholecystitis as a cause of hemobilia: report of a case. Surg Today. 2007;37(5):412–417. doi: 10.1007/s00595-006-3423-2. [DOI] [PubMed] [Google Scholar]