Abstract
Over the past few decades, Streptococcus dysgalactiae subspecies equisimilis (SDSE) have been considered as weak pathogenicity compared with S. pyogenes (GAS). Some recent reports argue that SDSE may bring severe soft tissue infection as same as GAS. No reports have been tried to reveal the clinical characteristics and autopsy images of fulminant SDSE infection. In this case report, we aimed to present a case of fatal necrotizing myositis from fulminant SDSE infection at iliopsoas, including autopsy appearance.
Keywords: autopsy image, necrotizing myositis, Streptococcus dysgalactiae subsp. equisimilis
1. INTRODUCTION
Streptococcus dysgalactiae (SD) is a pyogenic species pathogenic both for humans and animals. It has been considered an exclusive animal pathogen causing infections among wild animals, livestock, and pets. Over the past few decades, Streptococcus dysgalactiae subspecies equisimilis (SDSE) have been considered as weak pathogenicity compared with S. pyogenes (GAS).1 In particular, fulminant infections, like streptococcal toxic shock syndrome (STSS), are mostly caused by GAS.2, 3, 4, 5 Recent some reports argue about severe infection of SDSE. Severity of SDSE infection in human has been recently brought to light by these reports.6
While initial symptoms of SDSE infection present very slight changes, like skin and soft tissue infections, however, it may cause cellulitis, necrotizing fasciitis, endocarditis, and streptococcal toxic shock‐like syndrome. Thus, we need to identify invasive SDSE infections accurately.
2. CASE REPORT
A 77‐year‐old man was complying his left knee joint pain, but whole body condition was well, he did not visit hospital. The next day, he vomited his breakfast and lost appetite. He was barely able to do some yard work. However, in the afternoon, he could not do anything but get lying down because of severe left knee joint and left shoulder pain. Another next day, he could not move anymore. Thus, he decided to call for ambulance finally.
When he came to our emergency department, he presented tachycardia, tachypnea, and hypoxia. His left knee joint was swelling and reddening. We got purulent fluid at puncture site. Blood gas testing revealed acidemia, hypocapnia, and remarkable elevation of lactic acid. In addition, his biochemistry data revealed severe inflammation, acute kidney injury, liver dysfunction, marked elevation of creatine kinase and abnormal coagulation profile (Table 1).
Table 1.
His biochemistry data revealed severe inflammation, acute kidney injury, liver dysfunction, marked elevation of creatine kinase, and abnormal coagulation profile. Numbers with red mean high value compared with standard value. In addition, numbers with blue mean low value compared with standard
| Laboratory Data at admission | |||
|---|---|---|---|
| T.P | 7.4 g/dL | PBS | 71 mg/dL |
| Alb | 3.2 g/dL | CRP | 33.45 mg/dL |
| BUN | 38.8 mg/dL | ||
| UA | 16.0 mg/dL | WBC | 15 600 /μL |
| Cre | 2.73 mg/dL | RBC | 447 |
| Na | 133 mEq/L | Hb | 12.6 g/dL |
| K | 5.3 mEq/L | Hct | 39.0 % |
| Cl | 93 mEq/L | MCV | 87.2 fl |
| Ca | 7.7 mEq/L | Plet | 5.1 |
| T.Bil | 1.6 mg/dL | PT% | 35.7 % |
| AST | 534 U/L | PT‐INR | 1.81 |
| ALT | 162 U/L | DD‐FDP | 34.6 μg/mL |
| LDH | 1051 U/L | ||
| CK | 31 200 U/L | Urine Sugar/Protein | (++)/(‐) |
We suspected he suffered severe sepsis, septic disseminated intravascular coagulation (DIC), and multiorgan failure. Emergency CT revealed swelling of right iliopsoas (Figure 1). We identified it as another infection site. We started to treat him with adequate dose of meropenem with considering renal function. After several hours, he went in cardiopulmonary arrest suddenly. He got return of spontaneous circulation soon after cardiopulmonary resuscitation.
Figure 1.
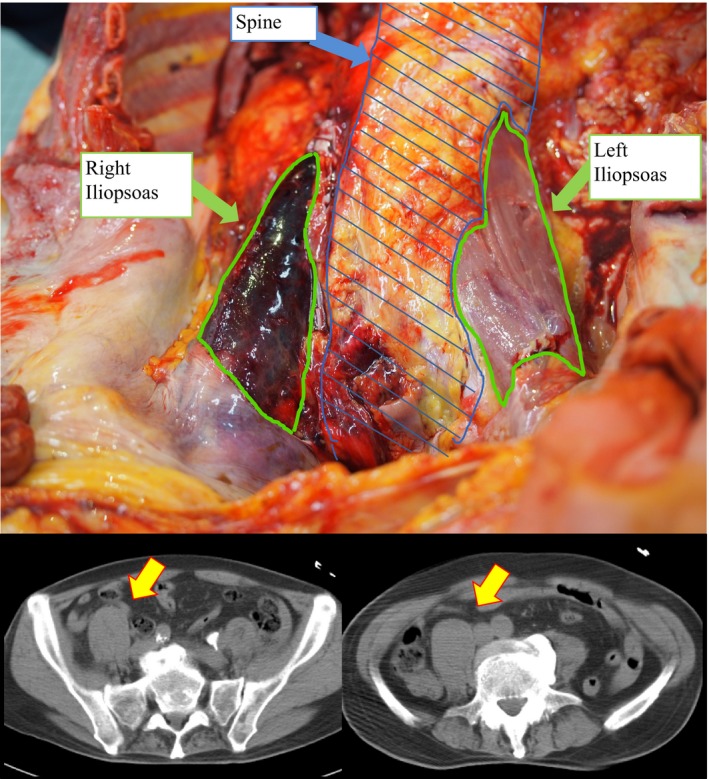
Comparison between autopsy and CT images (Pelvic level). CT images; Yellow arrow indicates swelling iliopsoas muscle. Autopsy images; Right iliopsoas muscle is swelling and necrosis. In contrast, left iliopsoas muscle is normal appearance
Same time, Gram stain from swelling knee joint puncture provided a definitive diagnosis of SDSE infection as causative organism. However, he could not maintain his circulation any more. Soon, he died of STSS within a day after admission. After his death, we could detect SDSE from two bottles of blood culture incubation. His autopsy revealed complete necrosis of right iliopsoas muscle macroscopically and hemorrhagic necrotizing myositis microscopically, which plain CT indicated (Figure 1). Curiously, despite of dynamic clinical course, we could not find any bacteria but many inflammatory cells from pathological appearance. We could find no vegetations in his heart and no other abscess among key organ in spite of severe bacteremia. Physicians have to remember the importance and severity of SDSE infection, which has been better recognized recently.1
3. DISCUSSION
Streptococcal toxic shock syndrome is known as serious infection with high mortality. Major part of STSS occupied with Streptococcus pyogenes. In the last few years, several articles have been devoted to the study of another causative organism among STSS, such as SD and SDSE. These are not common as disease‐causing bacterium of STSS. Among them, even within a species, there have many genetic differences and genetic mutation. The details of expression manner and mechanisms underlying gene polymorphism are still in controversy. Herein, we reported necrotizing myositis from fulminant SDSE infection. In this case, infection site was left iliopsoas muscle. His vital status was not stable at all. Some successful treatment of necrotizing myositis and fasciitis reported that the best strategy for treatment was amputation with surgical approach. We could not approach his iliopsoas muscle surgically, because of regional problem and unstable circulation status. Thus, with all things considered, we could not save his life.
Autopsy image of macro revealed complete necrosis of iliopsoas muscle. Curiously, despite of dynamic clinical course, we could not find any bacteria but many inflammatory cells from pathological appearance. Clinically, severity of STSS is associated with level of toxicity and dose of toxin. M protein and interleukin‐8 play a substantial role in “cytokine storm” of STSS. Toxin‐related cytokine storm from left knee joint might bring necrosis of left iliopsoas muscle. We could detect SDSE from two bottles of blood culture incubation. Systemic cytokine storm was associated with positive blood culture, but it might not be responsible for local iliopsoas necrosis totally.
In our speculation, not only toxins but also many bacteria were carried by the blood stream. Necrosis of iliopsoas muscle was obviously brought by toxin and bacteria. Necrotizing myositis was grading according the spreading levels of bacteria and neutrophilic responses pathologically. In this case with microscopic approach, we could observe no bacteria in necrotic site; however, we could find significant numbers of inflammatory cells.7, 8 Of course, it is not the same condition between pathology and autopsy imaging. To detect bacteria in autopsy imaging and to detect it in pathological examination are alike. This is the first case to present these interesting relations among necrotic site. Curiously, in this case, we conclude concentration of bacteria in local site seems to have no relation with degree of severity.
4. CONCLUSION
Streptococcus dysgalactiae subsp. equisimilis (SDSE) infection might bring severe organ failure such as STSS. Physicians have to remember the importance and severity of SDSE infection.
CONFLICT OF INTEREST
The authors have stated explicitly that there are no conflicts of interest in connection with this article.
Izumi M, Hiraiwa T, Tomioka H, Komura M, Hayashi Y. Fatal necrotizing myositis from fulminant Streptococcus dysgalactiae subspecies equisimilis (SDSE) infection: A case report of autopsy images. J Gen Fam Med. 2018;19:50–52. https://doi.org/10.1002/jgf2.154
REFERENCES
- 1. Lewis RT. Soft tissue infections. World J Surg. 1998;22:146–51. [DOI] [PubMed] [Google Scholar]
- 2. Baevsky RH, Ishida JT, Lieberman SA. Group A beta hemolytic streptococcal glossal necrotizing myositis—case report and review. MedGenMed. 2005;7:8. [PMC free article] [PubMed] [Google Scholar]
- 3. Stevens DL, Tanner MH, Winship J, et al. Severe group A streptococcal infections associated with a toxic shock‐like syndrome and scarlet fever toxin A. N Engl J Med. 1989;321:1–7. [DOI] [PubMed] [Google Scholar]
- 4. Subramanian KN, Lam KS. Malignant necrotising streptococcal myositis: a rare and fatal condition. J Bone Joint Surg. 2003;85:277–8. [DOI] [PubMed] [Google Scholar]
- 5. Sarani B, Strong M, Pascual J, et al. Necrotizing fasciitis: current concepts and review of the literature. J Am Coll Surg. 2009;208:279–88. [DOI] [PubMed] [Google Scholar]
- 6. Rantala S. Streptococcus dysgalactiae subsp. equisimilis bacteremia: an emerging infection. Eur J Clin Microbiol Infect Dis. 2014;33:1303–10. [DOI] [PubMed] [Google Scholar]
- 7. Wong CH, Khin LW, Heng KS, et al. The LRINEC (Laboratory Risk Indicator for Necrotizing Fasciitis) score: a tool for distinguishing necrotizing fasciitis from other soft tissue infections. Crit Care Med. 2004;32:1535–41. [DOI] [PubMed] [Google Scholar]
- 8. Bakleh M, Wold LE, Mandrekar JN, Harmsen WS, Dimashkieh HH, Baddour LM. Correlation of histopathologic findings with clinical outcome in necrotizing fasciitis. Clin Inefct Dis. 2005;40:410–4. [DOI] [PubMed] [Google Scholar]


