Abstract
Objective
To examine the impact of provider competition under global budgeting on the use of cesarean delivery in Taiwan.
Data Sources/Study Setting
(1) Quarterly inpatient claims data of all clinics and hospitals with birth‐related expenses from 2000 to 2008; (2) file of health facilities’ basic characteristics; and (3) regional quarterly point values (price conversion index) for clinics and hospitals, respectively, from the fourth quarter in 1999 to the third quarter in 2008, from the Statistics of the National Health Insurance Administration.
Study Design
Panel data of quarterly facility‐level cesarean delivery rates with provider characteristics, birth volumes, and regional point values are analyzed with the fractional response model to examine the effect of external price changes on provider behavior in birth delivery services.
Principal Findings
The decline in de facto prices of health services as a result of noncooperative competition under global budgeting is associated with an increase in cesarean delivery rates, with a high degree of response heterogeneity across different types of provider facilities.
Conclusions
While global budgeting is an effective cost containment tool, intensified financial pressures may lead to unintended consequences of compromised quality due to a shift in provider practice in pursuit of financial rewards.
Keywords: Cesarean delivery, global budgeting, quality of health care, provider behavior, reimbursement incentive
Health expenditures have increased drastically over the past decades in both developed and developing countries (Fan and Savedoff 2014). In the face of such continually rising costs of care, policy makers are more and more turning to payment policies to “bend the cost curve” (Cutler 2010). Among the array of interventions, global budgeting has been gaining popularity as it has been found to contain cost effectively (Wolfe and Moran 1992; Benstetter and Wambach 2006). Recent notable examples include the global budget‐based “Alternative Quality Contract” of Blue Cross Blue Shield (BCBS) Massachusetts (Song et al. 2012), the Maryland global budgeting hospital initiative in 2014 (Cornish and Hsu 2015), and Austria's 2013 reform to contain public health spending (Hofmarcher 2014).
If global budgeting achieves cost containment by improving efficiency and quality of care, then its appeal for sustainable health financing warrants consideration by all policy makers. However, in what manner global budgeting shapes the health service delivery remains largely an unanswered question. In fact, despite decades of various countries’ experiences, empirical evidence covering the impact of global budgeting on provider practices is still limited (Mathematica 2009; Moreno‐Serra 2014). Some recent studies have suggested that global budgeting could lead to changes in service volume, in terms of both total quantities and mix (Chang, Hsieh, and Myrtle 2011; Chen and Fan 2015). Nevertheless, the impact of global budgeting on quality is yet unclear.
This study contributes to the global budgeting literature by examining changes in facility‐level cesarean delivery rates as a result of provider competition under Taiwan's global budgeting scheme. The Taiwanese system enforces health expenditure limits by adjusting prices in accordance with volume changes. Specifically, on top of the fee‐for‐service (FFS) system, an ex post conversion factor, referred to as the “point value (PV),” is applied to equate the monetary value of actual services delivered to the set budget cap. The proportional price adjustment is applied uniformly to all services covered by the National Health Insurance (NHI). The expenditure cap with price adjustment generates a “tragedy‐of‐the‐commons” incentive—when the revenue for a specific provider is determined by its relative share, the “rational” behavior for every provider is to engage in volume expansion fueled by an increase in both inputs and investment, that is, noncooperative competition, ironically driving down de facto prices for all (Benstetter and Wambach 2006; Cheng, Chen, and Chang 2009). The important question for policy making is how the resulting price changes shape providers’ practices and service quality.
The use of cesarean delivery is an ideal candidate for exploring the aforementioned question. The literature has well documented that supply‐side factors could significantly influence clinical decisions for this procedure (Clark et al. 1998; Fuglenes, Øian, and Kristiansen 2009). For instance, it has been found that cesarean delivery use could be a manifestation of obstetricians’ practice of defensive medicine (Dubay, Kaestner, and Waidmann 1999; Fuglenes, Øian, and Kristiansen 2009). Studies have also presented that cesarean rates increase in response to income shock to obstetricians (Gruber and Owings 1996) or higher fee differentials between cesarean and normal deliveries (Gruber, Kim, and Mayzlin 1999). Specifically in Taiwan, qualitative evidence has demonstrated obstetricians’ preference toward cesarean delivery. For instance, the chief head of the department of obstetrics and gynecology at one medical center said in a newsletter that “normal delivery requires longer care‐giving time but is not better and reasonably reimbursed (than cesarean delivery). Scheduled cesarean delivery is a more time‐saving option and provides better life quality for health professionals” (Chou 2012).
While the costs and benefits of cesarean versus vaginal delivery are still a topic of debate in the medical community itself (Klein 2004; Lavender et al. 2012), the cesarean delivery rate is still on a steady rise in many parts of the world despite many containment efforts (Mazzoni et al. 2011). The economic and health implications for a large‐scale utilization of cesarean delivery make it an important public health issue (Declercq et al. 2007; Chen et al. 2014). As there exists determination for cost control across health systems, our investigation on the cesarean delivery rate in the context of noncooperative competition not only can inform policy makers about the potential trade‐offs, but also can shed light on how the rising cesarean delivery rate could be affected by cost containment measures.
Literature on the Impact of Global Budgeting Systems
Although global budgeting has been in use for decades with many new initiatives in the making, the literature unfortunately offers limited help in providing guidance on its impact. In a review of the latest evidence of cost control strategies, Moreno‐Serra (2014) concluded that there is still a lack of hard empirical evidence in the global budgeting literature as “most evidence (is) methodologically limited.” Existing observations note that global budgeting in general is associated with a lower rate of health expenditure growth (Yakoboski, Ratner, and Gross 1994; Schwartz, Glennerster, and Saltman 1997). Moreover, when an expenditure cap is imposed on top of the FFS system, service volume typically increases in both inpatient and outpatient settings (Chen et al. 2007; Chang, Hsieh, and Myrtle 2011; Hsu 2014). This is consistent with theoretical work that demonstrates the prisoners’ dilemma–like incentives to augment relative shares in such a design (Fan, Chen, and Kan 1998). However, most of the earlier empirical writings on global budgeting are descriptive in nature without an explicit comparison group and hence suffer from the issue of internal validity (Moreno‐Serra 2014; Chen and Fan 2015).
Two recent studies addressed these methodological challenges and found robust evidence that provider competition under global budgeting with price adjustment does lead to growth in utilization as well as changes in service mix (Chang, Tsai, and Myrtle 2015; Chen and Fan 2015). Chang, Tsai, and Myrtle (2015) identified the effect of outpatient dialysis global budgeting by examining the changes in hypertension‐related outpatient visits and medications among hemodialysis patients before and after the global budget, compared with those changes among patients with hypertension who did not require hemodialysis. Chen and Fan (2015) took a different approach and used simulations to show that volume expansion will result in lower PV and de facto price cuts, triggering substitution favoring a more profitable service having higher price/cost ratios. This is in essence the manifestation of supplier‐induced demand well recognized in the health economics literature (McGuire and Pauly 1991).
Recent findings on practice pattern change raise concerns over health care quality under global budgeting. Song and colleagues (2012) investigated the impact of the “Alternative Quality Contract” in Massachusetts on quality, indicating that quality improves among providers under global budgeting compared to the control organizations, particularly in areas such as chronic care management and preventive care. However, in this specific program, provider payment is tied to performance in meeting predefined quality targets; that is, the improvement in quality most likely results from the binding quality requirements, rather than the global budgeting itself.
Health System and Utilization of Cesarean Delivery in Taiwan
Health System and Global Budgeting
Taiwan implemented its NHI in 1995. The enrollment is compulsory—but the enrollees enjoy a generous benefit package—most health services and medications provided by inpatient, outpatient, dental care, and Chinese medicine are covered with limited copayments. The improved access, coupled with the FFS reimbursement for providers, fueled a rapid growth in health expenditures during the following years (Cheng 2003). As the feasibility to significantly raise premiums was limited by political reasons, Taiwan's government quickly turned to global budgeting to ensure its financial sustainability.
To restrain health expenditure growth, NHI phased in global budgeting for different sectors, first starting with dental care in 1998, followed by Chinese medicine in 2000, clinics in 2001, hospitals in 2002, and finally a separate budget earmarked for outpatient dialysis care in 2003. As discussed, Taiwan's global budgeting is in essence an expenditure cap on top of the FFS system. The national expenditure budget is set by adjusting the budget for the preceding year with an inflation factor that is negotiated between provider and consumer representatives. The national cap is then divided up into six regional budgets based on demographics risk‐adjusted population. As health expenditures typically rise with income, a budget based on historical spending would thus favor populations with higher economic status. Even though not explicitly stated, the transition from FFS to population‐based budgeting has implications on cross‐region redistribution of resources away from the more economically developed regions. The regional budgets are allocated to providers according to their respective shares of total service volume in the region. That is, a hospital's revenue is determined by the following:
where B is the regional budget, q ij is the quantity of service j at hospital i, and p j represents the relative values of service j in points, similar to the set fees under FFS, as dictated by the payment schedule1 (Chen and Fan 2015). The revenue of hospital i is then a product of its service volume—point sum of all services (Q i), and the price conversion factor—PV, to equate the monetary value of the services delivered to the set budget cap. PV is calculated every quarter, when providers know retrospectively where they are positioned against others in the same region, as well as what the de facto prices are for the provided services. For instance, a total service volume in points 20 percent higher than the budget would entail a PV of 0.83 (1/1.2) and a 17 percent price cut on all services for all providers, which they only learn after the end of the quarter.
Utilization of Cesarean Delivery
Under NHI, expectant mothers are fully insured and do not bear the cost of delivery, with the only exception being elective cesarean deliveries on “maternal request,” that is, without medical indications, which accounts for only about 2 percent of births (Chen et al. 2014). Mothers can choose to deliver in hospitals (medical centers, regional or local hospitals) or obstetrics clinics with full operating room suites and beds for overnight stays. There is considerable variation in number of deliveries across obstetricians and health facilities (Figure S1). Prior to 2005, the reimbursement for vaginal delivery was typically 55–60 percent of that for cesarean delivery—U.S.$500–600 for the former and U.S.$900–1050 for the latter, depending on the facility type. In 2005, the Taiwan government raised the payment of vaginal delivery to equate the fees of the two procedures.
Since the inception of NHI, the cesarean delivery rates in Taiwan have been on a steady increase, from 25.4 percent in 1996 to 36.5 percent in 2011 and leveling off since then, making Taiwan one of the countries with the highest rates (Statistics Bureau 2010; Health Promotion Administration 2014). At the same time, there has been a large regional variation in cesarean delivery rates, with the difference exceeding 10 percentage points between regions with the highest and lowest rates (Chen 2015). Clinics also tend to have a much higher likelihood of performing cesarean deliveries than hospitals (Lin and Xirasagar 2004).
Methods
Research Design and Data
This study investigates how provider competition under global budgeting affects practice behavior, using the cesarean delivery rate as the indicator. The point value fluctuates depending on the regional service volume for a specific quarter. Therefore, we are able to leverage the significant variations in quarterly point values over time, across the six regions, and between clinics and hospitals.
We hypothesize that hospitals and clinics react to the price signals of the point values. Specifically, when the point value drops and the providers suffer a financial loss, they compensate by substituting toward cesarean delivery, as studies have indicated that this service is usually more profitable for providers, in terms of both observable reimbursement fees and nonobservable opportunity costs (Spetz, Smith, and Ennis 2001; Lo 2003; Grant 2009). Even with the parity in fees post‐2005, cesarean deliveries are still likely to be more economically favorable due to the shorter and scheduled care‐giving time and lower risks of malpractice litigation costs associated with cesarean deliveries (Han and Lien 2010). Moreover, providers earn more revenues with elective cesarean deliveries because they receive copayments in cash from patients and, unlike vaginal deliveries, only part of the actual reimbursements for elective cesarean deliveries is susceptible to price cuts by the point value adjustment (Chen et al. 2014).
We choose the cesarean delivery rate as our dependent variable of interest, because even though obstetricians are less likely to induce the quantities of births, they do have influence over the choice of cesarean delivery in their practices. The volume of birth‐related health services is miniscule compared with the total sectoral quantity. For each obstetrician, it is reasonable to expect that any shift in his or her practice in birth delivery would not have a meaningful impact on the point value, and hence, we treat changes in point values as extrinsic. Because the point value is derived ex post at the end of each quarter, the most relevant information for providers would be the point value in the preceding quarter.
We assembled our data from three sources. The principal one is the inpatient claims from the National Health Research Institute (NHRI) database in Taiwan, from which we identified all birth deliveries from 2000 to 2008. The inpatient claims include deliveries in both hospitals and obstetric clinics, because of their overnight stays. Given the single‐payer system and universal coverage, our analysis is less susceptible to issues commonly seen in complex U.S. multi‐payer systems, such as selection bias. As we are interested in the organization behavior of provider facilities, we restructured the data by regrouping patient claims based on a scrambled but unique health facility identifier and then estimated the cesarean delivery rates based on the frequency of normal and cesarean deliveries in each facility every quarter.
The second data source is a file on health facilities’ basic characteristics, also from NHRI, that provides information on each facility's ownership, accreditation status, and geographical region. Information on facility characteristics was then extracted and linked with the claims file via the unique facility identifier. Lastly, we extracted quarterly point values for clinics and hospitals, respectively, for each region from the Statistics of the National Health Insurance Administration. For quarters when global budgeting was not implemented, point values are defined as 1, as providers are fully reimbursed for each dollar of services provided. Because our study investigated the relationship between cesarean delivery rates and the respective point values in the preceding quarters, the point values extracted are from the fourth quarter in 1999 to the third quarter in 2008.
Statistical Analysis
Our dependent variable of interest, cesarean delivery rate, is a fractional outcome, bounded between 0 and 1. The functional form issues associated with such a type of outcome cannot be satisfactorily addressed by traditional log‐odds transformation. Considering our unbalanced panel data given the market entry and exit of health facilities, we followed recommendations by Williams (2015) and estimated the point value's effect on the cesarean delivery rate, using the fractional response model (FRM).2 As noted by Wooldridge (2011), the generalized linear model (GLM) with binomial distribution and probit link function can also be applied to analyze proportions, and it yields essentially the same results as FRM.
Our estimation is performed with the following empirical specification:
Here, CS ijt indicates the cesarean delivery rate of provider i in region j and at time t; PV jt‐1 indicates the point value of region j in the preceding time period t−1; and X i is a set of dummies of time‐invariant provider facility characteristics, including accreditation level (clinic, local hospital, regional hospital, and medical center) and ownership (private versus public). As the literature has found that different types of providers exhibit differential strategic behavior in competition under global budgeting due to institutional constraints (Chen and Fan 2015), we also include in our final models interaction terms between the point value and time‐invariant characteristics. Estimators for the point value, β, and for the interaction terms, δ, are our main estimators of interest. We include birth delivery volume for provider i at time t (Xvolit), because of the potential association between delivery volume and cesarean rate observed empirically in the literature (McKenzie and Stephenson 1993; Lin and Xirasagar 2004; Clark et al. 2007). More important, following Papke and Wooldridge (2008), we also add the time averages of birth volume of provider i, Avg(Xvoli), to control for the unobserved provider effects correlated over time. To control for any effects of market consolidation in respective regions, we also introduce a market concentration index (MCI) of birth delivery, defined as the sum of squares of birth volume shares of the health facilities in a region during a quarter. MCI of birth delivery is similar to the Herfindahl–Hirschman Index for measuring changes in market structure. Finally, η j are region fixed effects, ω t are time dummies, and ε ijt are error terms. We model two types of time dummies separately: year and quarter fixed effects. The former account for unobservable year‐specific factors that could correlate with point values and cesarean delivery rates, such as policy impact or an increase in birth rates due to the cultural preferences for being born under a certain Chinese zodiac (Tang et al. 2006). The latter, on the other hand, address potential biases caused by some unobserved seasonal factors.
We also perform a number of sensitivity analyses. A provider behavioral response to price changes could differ across pregnancies of different risk profiles. Therefore, we conduct subgroup analyses—specifically among mothers 40 years and older, whose pregnancies are significantly riskier, and lower risk ones between 20 and 30 years old, respectively. We also perform sensitivity analyses with different timeframes and facility delivery volumes to ensure that our results are robust to various specifications.
Results
Descriptive Statistics
Table 1 presents the descriptive statistics of the health facilities in Taiwan that provide birth delivery services and that are examined in our study. It shows a significant reduction in the number of health facilities, particularly among local hospitals (46.86 percent) and clinics (35.26 percent). On average, the annual birth delivery volumes decrease across different facilities, except for local hospitals where market consolidation is most prominent. The total segment volume of births delivered also declines substantially. The decline affects local hospitals and clinics the most, where it falls by at least one‐third.
Table 1.
Descriptive Statistics of Health Facilities Providing Birth Delivery Services
| 2000 | 2002 | 2004 | 2006 | 2008 | |
|---|---|---|---|---|---|
| Medical centers | |||||
| N | 17 | 17 | 17 | 19 | 19 |
| Avg. annual delivery volume, count per facility | 2,404 | 2,148 | 1,892 | 1,788 | 1,781 |
| Total delivery volume, segment total | 40,865 | 36,521 | 32,159 | 33,980 | 33,848 |
| Avg cesarean section rate, % | 36.53 | 36.48 | 35.16 | 35.03 | 36.05 |
| Regional hospitals | |||||
| N | 61 | 68 | 69 | 63 | 68 |
| Avg. annual delivery volume, count per facility | 1,078 | 862 | 770 | 750 | 743 |
| Total delivery volume, segment total | 65,764 | 58,635 | 53,148 | 47,230 | 50,555 |
| Avg cesarean section rate, % | 35.87 | 34.99 | 33.05 | 35.22 | 35.39 |
| Local hospitals | |||||
| N | 175 | 133 | 113 | 98 | 93 |
| Avg. annual delivery volume, count per facility | 435 | 449 | 498 | 536 | 522 |
| Total delivery volume, segment total | 76,096 | 59,687 | 56,221 | 52,527 | 48,561 |
| Avg cesarean section rate, % | 35.07 | 33.88 | 32.13 | 34.41 | 35.79 |
| Clinics | |||||
| N | 397 | 357 | 324 | 301 | 257 |
| Avg. annual delivery volume, count per facility | 244 | 216 | 213 | 216 | 224 |
| Total delivery volume, segment total | 96,961 | 77,158 | 69,005 | 64,950 | 57,449 |
| Avg cesarean section rate, % | 30.97 | 32.90 | 31.70 | 32.68 | 34.07 |
Cesarean delivery rates in Taiwan on average are well above 30 percent. In 2000, there is a substantial difference in cesarean delivery rates between clinics and hospitals, with a 5.56 percentage point difference between clinics and medical centers. The difference drops over time, as medical centers’ rate is consistently above 35 percent, while clinics have seen their average rates increase from 30.97 percent in 2000 to 34.07 percent in 2008. Despite the high average rates, there is a wide variation in cesarean delivery rates across facilities. For instance, for the last quarter in 2008, the first and third quartile rates among clinics are 22.2 and 46.1 percent, respectively.
There is also a significant temporal variation in point values. On average, the variation is larger among clinics than among hospitals—clinics’ point values fluctuate between 0.7 and 1.3, while those for hospitals stay between 0.8 and 1.1. Across the six regions, point values also vary greatly. As an example, Figure 1 presents regional point values for the hospital sector from 2002 to 2008. Overall, after the implementation of global budgeting, we see a decline in point values, particularly in 2004 and 2005, after which point values rise back, albeit to levels still <1. Nevertheless, except for the last two quarters in 2002, when the scheme was being phased in with the national point values applied across regions, point values diverge cross‐regionally and move independently over time without any clear recognizable relationship among one another.
Figure 1.
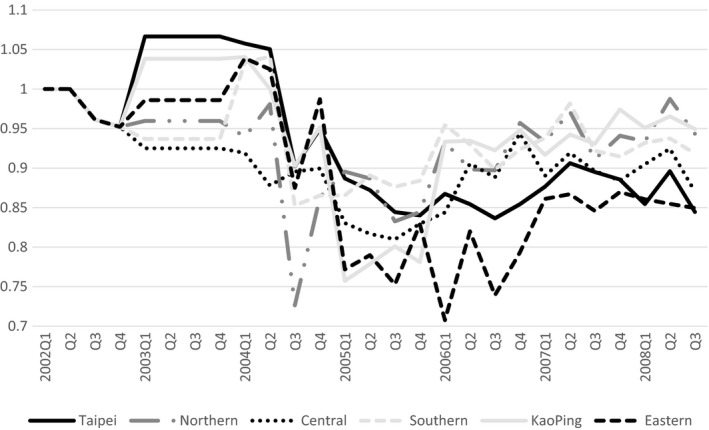
- Note. Hospital sector includes medical centers, regional hospitals, and local hospitals, which compete for revenues from the same pool of global budgeting in the respective regions.
Fractional Response Model Analyses
Table 2 presents the results of our FRM estimation. In Model (1), we examine the average treatment effects of point values across all health facilities. The impact estimate of point values suggests a negative effect, but the magnitude is not statistically different from zero. Allowing for differential effects of the point value in Models (2) and (3) shows a significant variation in how different types of health facilities respond to point value changes. Overall, the point value has a negative and statistically significant impact on cesarean rates, with the exception in medical centers: While the estimated effect for medical centers (coefficient for PV, as the reference category) is statistically insignificant, all the interaction terms yield negative and statistically significant results. The negative impacts of the point value on cesarean delivery rates have the largest magnitude among regional hospitals and clinics, followed by local hospitals. There is a significant interaction between the point value and ownership, with the positive sign indicating an effect that counteracts the negative impact of the point value on cesarean delivery rates. In other words, private facilities might react to changes in the point value less so than their public counterparts. The deployment of different time dummies—year fixed effects in Model 2 and quarter fixed effects in Model 3—yields consistent and very similar results.
Table 2.
Results from Fraction Response Model
| (1)† | (2)† | (3)‡ | |
|---|---|---|---|
| Point value (reference: medical centers) | −0.09 | 0.08 | 0.09 |
| (0.06) | (0.16) | (0.17) | |
| Point value × regional hospitals | −0.58*** | −0.58*** | |
| (0.14) | (0.14) | ||
| Point value × local hospitals | −0.50*** | −0.50*** | |
| (0.15) | (0.15) | ||
| Point value × clinics | −0.56*** | −0.54*** | |
| (0.13) | (0.13) | ||
| Point value × private | 0.40* | 0.40* | |
| (0.18) | (0.18) | ||
| Regional hospitals | −0.03* | 0.52*** | 0.53*** |
| (0.01) | (0.13) | (0.13) | |
| Local hospitals | −0.04** | 0.44** | 0.43** |
| (0.01) | (0.14) | (0.14) | |
| Clinics | −0.08*** | 0.44*** | 0.43*** |
| (0.01) | (0.12) | (0.13) | |
| Private ownership | −0.05*** | −0.43* | −0.43* |
| (0.01) | (0.18) | (0.18) | |
| Total birth volume (‘00) | −0.01 | −0.01* | −0.01* |
| (0.01) | (0.01) | (0.01) | |
| Birth volume time average (‘00) | 0.01 | 0.01 | 0.01 |
| (0.01) | (0.01) | (0.01) | |
| Market concentration index | −0.20 | −0.25 | −0.32 |
| (0.62) | (0.62) | (0.63) | |
| Northern region | −0.11*** | −0.11*** | −0.11*** |
| (0.02) | (0.02) | (0.02) | |
| Central region | −0.23*** | −0.24*** | −0.24*** |
| (0.01) | (0.01) | (0.01) | |
| Southern region | −0.10*** | −0.10*** | −0.10*** |
| (0.01) | (0.01) | (0.01) | |
| KaoPing region | −0.04** | −0.04** | −0.04** |
| (0.01) | (0.01) | (0.01) | |
| Eastern region | −0.23** | −0.23* | −0.22* |
| (0.09) | (0.09) | (0.09) | |
| Observations (facilities) | 876 | 876 | 876 |
Notes. Robust standard errors in parentheses ***p < .001, **p < .01, *p < .05.
(‘00): in hundreds.
†Model is adjusted for year fixed effects (8‐year dummies).
‡Model is adjusted for quarter fixed effects (35 quarter dummies).
To facilitate our understanding of the effect magnitude of a change in the point value on cesarean delivery rates, Figure 2 shows the marginal effects of a 10 percentage point drop in PV for different types of facilities based upon Model (2). As an example, a 10 percentage point decline leads to a 1.90 percentage point increase in cesarean delivery rates in the next quarter among public regional hospitals. One thing of note in this set of estimates is that for private medical centers, there is a significantly positive effect of the point value; that is, a drop in the point value leads to a further decline in cesarean delivery rates in these institutions.
Figure 2.
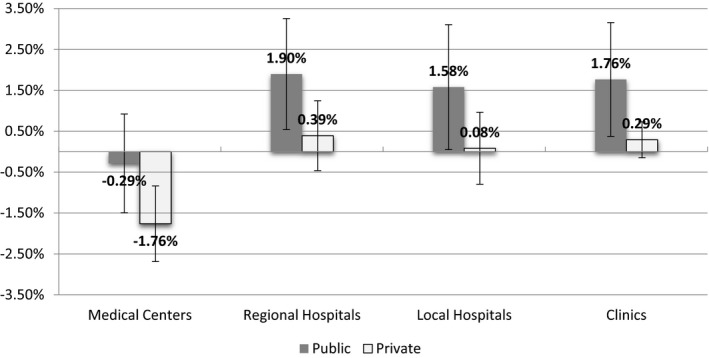
- Note. Error bars show 95% confidence interval.
Subgroup analyses of different maternal age groups in Table 3 show that the difference in the cesarean rate associated with point value change is larger among mothers in their 20s; for example, the coefficient for the point value impact among regional hospitals is −0.80 versus −0.58 for the entire sample. On the other hand, there is no statistically significant effect among mothers of advanced ages (40 years and older). Finally, results from sensitivity analyses with different timeframes are consistent with the main results, and so are ones limited to facilities with higher delivery volumes.
Table 3.
Sensitivity Analyses
| Sample Restriction | Timeframe (Year) | Maternal Age | Delivery Volume (Quarter) | ||||
|---|---|---|---|---|---|---|---|
| 1998–2008 | 2002–2008 | 2000–2006 | Age ≥40 | 30 > Age ≥20 | >50 | >100 | |
| Point value (reference: medical centers) | 0.14 | 0.02 | −0.09 | −0.31 | 0.03 | 0.11 | 0.22 |
| (0.16) | (0.17) | (0.18) | (0.47) | (0.18) | (0.12) | (0.13) | |
| Point value × regional hospitals | −0.54*** | −0.62*** | −0.49*** | 0.02 | −0.80*** | −0.59*** | −0.38** |
| (0.13) | (0.15) | (0.15) | (0.43) | (0.16) | (0.11) | (0.12) | |
| Point value × local hospitals | −0.41** | −0.60*** | −0.25 | −0.02 | −0.59*** | −0.56*** | −0.34** |
| (0.14) | (0.16) | (0.16) | (0.45) | (0.17) | (0.11) | (0.12) | |
| Point value × clinics | −0.62*** | −0.50*** | −0.34* | −0.38 | −0.68*** | −0.50*** | −0.45*** |
| (0.12) | (0.14) | (0.13) | (0.40) | (0.15) | (0.11) | (0.11) | |
| Point value × private | 0.38* | 0.40* | 0.33 | 0.42 | 0.55** | 0.29* | 0.13 |
| (0.17) | (0.20) | (0.20) | (0.47) | (0.20) | (0.11) | (0.13) | |
Notes. All models are adjusted for hospital accreditation, ownership, total birth volume, birth volume time averages, region and year fixed effects.
Robust standard errors in parentheses ***p < .001, **p < .01, *p < .05.
Discussion and Conclusion
The economic pressures confronting health systems around the world have prompted many to explore payment interventions, including global budgeting, in order to contain ever‐increasing health care costs. Despite cumulative experiences, our knowledge on how global budgeting shapes provider practice and care quality is limited. In this study, we look into how changes in point value, as a result of provider competition under an expenditure cap, affect cesarean delivery rates.
Our study offers two main contributions to the global budgeting literature. First, we find that cost containment by global budgeting may come at the expense of compromised quality, as providers strategically change their service mix in response to the financial incentives. Second, except for medical centers, clinics and different types of hospitals respond to these external price signals differently—a drop in the point value leads to an increase in cesarean delivery rates among clinics and regional hospitals, and slightly less so in local hospitals. At the same time, behavioral changes induced by point value variations are more prominent among public hospitals versus private hospitals, as well as among pregnancies of young mothers, who are at lower risks medically than those with advanced ages.
The negative effect of point values on cesarean delivery is consistent with our expectations based upon prior theoretical works on provider behavior. McGuire and Pauly (1991) argued that when there are strong income effects from fee changes, providers seek out target income. In our case, the fee cuts due to a point value drop lead health facilities to shift toward cesarean deliveries to compensate for lost income.
The unique impact of point values on cesarean delivery rates in private medical centers is very much intriguing. One may posit that the corresponding drop in cesarean delivery rates with point value declines could hypothetically result from smaller facilities limiting their quantities of normal deliveries and directing mothers to medical centers at the end of the referral chain. Nevertheless, when we test for the point value impact on cesarean delivery quantities, the results do not support such a hypothesis—point value changes do not have any discernible effect on the number of cesarean deliveries (Table S1). An alternative explanation, also based upon McGuire and Pauly (1991), could be that the fee cut has only a limited income effect, and given the much wider array of health services that private medical centers provide, providers could exhibit profit maximization behavior, which entails a relative decline in cesarean delivery rates given the larger absolute reduction in profits for this procedure relative to vaginal delivery.
The differential responses by different types of provider facilities are likely driven by a number of factors. First, compared with large medical centers, clinics and smaller hospitals are more likely to be managed by physicians, and their responses to price changes are likely to be more in alignment with financial considerations given the closely tied incentive structure. Second, medical centers face more bureaucratic and professional constraints. In other words, any change in practice might be internally restrained by physicians subscribing to strict clinical standards and being externally monitored by the NHI administration (Chen 2011). Third, given the smaller birth delivery volumes and large number of facilities among clinics and smaller hospitals, their actions are also more “noncooperative” and economically driven toward shifting to more profitable items (Olson 1965; Chen and Fan 2015).
Fourth and lastly, the results show a much milder response among private hospitals. Because public hospitals are often assumed to be less responsive to financial incentives, this finding is seemingly counterintuitive, but it can be understood through the institutional background in Taiwan. In response to criticism directed at inefficiency among public facilities, these entities have been increasingly required to finance their own operations since the 1990s. They began to set up funds to reward physicians with bonuses tied to earned profits. Furthermore, physicians in public facilities typically have a lower base salary due to legal restrictions, and hence, a larger portion of their income could in fact come from profit‐based bonuses when compared to their counterparts in private facilities (Chen 2011). Because the data on the presence of profit‐based bonuses are private and unavailable, we cannot directly investigate their role in provider behavior. However, the findings herein suggest that provider behavior may be driven more by the internal incentive structure set up by managers, rather than the traditional typology of facility ownership.
Our study has a number of limitations. The claims‐based panel data of delivery by facility enable us to investigate how providers respond to changes in point values. However, as with any observational study using time‐series data, the possibility of effects from unobserved concurrent factors cannot be completely excluded. We do employ a number of measures to minimize endogeneity, including the use of time dummies, region fixed effects, and time averages of facility‐level characteristics. Following Papke and Wooldridge (2008), we also choose a probit response function over logit in our estimation, as the former is known to be superior with potentially endogenous variables. As our findings are robust to alternative timeframe specifications and subgroups, any effect from unobserved factors should be minimal if any.
Another limitation of our study is the use of the cesarean delivery rate as the quality indicator. Although it is a widely recognized quality indicator tracked by many, including AHRQ (2011), it is admittedly a utilization and process measurement. We do not have adequate information, due to data limitations, to answer the important question of whether the shift in provider practice has an adverse impact on maternal or fetal health outcomes. This would be an important input into future considerations and revisions of global budgeting schemes and should be explored in future studies.
Finally, not all global budgeting systems are the same (Long and Marquis 1994; Chen and Fan 2016). The expenditure limit could be enforced by either volume control or price adjustment. The global budgeting impact we have identified on provider practice and quality might be specific to the price adjustment design, which has been applied in countries such as Germany, Canada, and Taiwan. Global budgeting systems that contain costs through setting individual provider budgets may face a different set of issues for inefficiency, access, and quality.
Because of these limitations, one should be cautious in making general inferences of our findings. Nevertheless, the consistent findings across different model specifications provide assurance as to the validity of our results. Our study highlights the importance of examining the potential trade‐offs in quality of cost control interventions. It is also important to consider the different institutional constraints faced by different providers, as well as any differences exhibited in how they respond to policy interventions. A blunt imposition of an expenditure cap, despite its effectiveness in cost containment, could lead to issues in health care quality and compromise the ultimate objectives of health systems to improve people's health.
Supporting information
Appendix SA1: Author Matrix.
Appendix SA2:
Figure S1: Distribution in the Number of Total Annual Deliveries among Taiwanese Obstetricians, 2004.
Table S1: Negative Binomial Model to Investigate the Relationship between Point Value and Number of Cesarean Deliveries in Health Facilities.
Acknowledgments
Joint Acknowledgement/Disclosure Statement: This work was supported by the Ministry of Science and Technology in Taiwan through grants MOST 104‐2410‐H‐010‐021 and MOST 104‐2410‐H‐305‐057‐MY3 and is based on data from the National Health Insurance Research Database (NHIRD) in Taiwan. The MOST financial support and the NHIRD data provision are gratefully acknowledged.
Disclosures: None.
Disclaimers: None.
Notes
The “point schedule” is inherited from the fee schedule under FFS and has been only revised twice in 2004 and 2013 based on suggestions by professional societies. Values for new services are set by the Pharmaceutical Benefit and Reimbursement Scheme Joint Committee through reference pricing and negotiation.
FRM can be implemented in Stata with the user‐written routine, fracglm, downloadable at http://www3.nd.edu/~rwilliam/stata
References
- AHRQ . 2011. “Cesarean Delivery Rate: Inpatient Quality Indicators #21” [accessed on November 22, 2015]. Available at http://www.qualityindicators.ahrq.gov/Downloads/Modules/IQI/V43/TechSpecs/IQI%2021%20Cesarean%20Delivery%20Rate.pdf
- Benstetter, F. , and Wambach A.. 2006. “The Treadmill Effect in a Fixed Budget System.” Journal of Health Economics 25 (1): 146–69. [DOI] [PubMed] [Google Scholar]
- Chang, R.‐E. , Hsieh C.‐J., and Myrtle R. C.. 2011. “The Effect of Outpatient Dialysis Global Budget Cap on Healthcare Utilization by End‐Stage Renal Disease Patients.” Social Science & Medicine 73 (1): 153–9. [DOI] [PubMed] [Google Scholar]
- Chang, R.‐E. , Tsai Y.‐H., and Myrtle R. C.. 2015. “Assessing the Impact of Budget Controls on the Prescribing Behaviours of Physicians Treating Dialysis‐Dependent Patients.” Health Policy and Planning 30 (9): 1142–51. [DOI] [PubMed] [Google Scholar]
- Chen, Y.‐T. 2011. Strategic Provider Behavior under Global Budget Payment. Boston: Harvard University. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen, G.‐D. 2015. Area Variations of Cesarean Section Rates, Factors Influencing Physician's Cesarean Section Rates and Association between Cesarean Section Rates and Perinatal Morbidity. Taipei, Taiwan: National Taiwan University. [Google Scholar]
- Chen, B. , and Fan V. Y.. 2015. “Strategic Provider Behavior under Global Budget Payment with Price Adjustment in Taiwan.” Health Economics 24 (11): 1422–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen, B. , and Fan V. Y.. 2016. “Global Budget Payment: Proposing the CAP Framework.” INQUIRY: The Journal of Health Care Organization, Provision, and Financing 53: 1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen, F.‐J. , Laditka J. N., Laditka S. B., and Xirasagar S.. 2007. “Providers’ Responses to Global Budgeting in Taiwan: What Were the Initial Effects?” Health Services Management Research 20 (2): 113–20. [DOI] [PubMed] [Google Scholar]
- Chen, C.‐S. , Liu T.‐C., Chen B., and Lin C.‐L.. 2014. “The Failure of Financial Incentive? The Seemingly Inexorable Rise of Cesarean Section.” Social Science & Medicine 101: 47–51. [DOI] [PubMed] [Google Scholar]
- Cheng, T.‐M. 2003. “Taiwan's New National Health Insurance Program: Genesis and Experience So Far.” Health Affairs 22 (3): 61–76. [DOI] [PubMed] [Google Scholar]
- Cheng, S.‐H. , Chen C.‐C., and Chang W.‐L.. 2009. “Hospital Response to a Global Budget Program under Universal Health Insurance in Taiwan.” Health Policy 92 (2–3): 158–64. [DOI] [PubMed] [Google Scholar]
- Chou, M.‐M. 2012. “Rising Cesarean Section Rate—A Serious and Complex Public Health Issue.” Taichung Veterans General Hospital Journal 174: 6–7. [Google Scholar]
- Clark, S. L. , Xu W., Porter T. F., and Love D.. 1998. “Institutional Influences on the Primary Cesarean Section Rate in Utah, 1992 to 1995.” American Journal of Obstetrics and Gynecology 179 (4): 841–5. [DOI] [PubMed] [Google Scholar]
- Clark, S. L. , Belfort M. A., Hankins G. D. V., Meyers J. A., and Houser F. M.. 2007. “Variation in the Rates of Operative Delivery in the United States.” American Journal of Obstetrics and Gynecology 196 (6): 526. e1‐526.e5. [DOI] [PubMed] [Google Scholar]
- Cornish, A. , and Hsu A.. 2015. “In Maryland, A Change In How Hospitals Are Paid Boosts Public Health” NPR.org [accessed on October 28, 2015]. Available at http://www.npr.org/sections/health-shots/2015/10/23/451212483/in-maryland-a-change-in-how-hospitals-are-paid-boosts-public-health
- Cutler, D. 2010. “Analysis & Commentary How Health Care Reform Must Bend the Cost Curve.” Health Affairs 29 (6): 1131–5. [DOI] [PubMed] [Google Scholar]
- Declercq, E. , Barger M., Cabral H. J., Evans S. R., Kotelchuck M., Simon C., Weiss J., and Heffner L. J.. 2007. “Maternal Outcomes Associated with Planned Primary Cesarean Births Compared with Planned Vaginal Births.” Obstetrics & Gynecology 109 (3): 669–77. [DOI] [PubMed] [Google Scholar]
- Dubay, L. , Kaestner R., and Waidmann T.. 1999. “The Impact of Malpractice Fears on Cesarean Section Rates.” Journal of Health Economics 18 (4): 491–522. [DOI] [PubMed] [Google Scholar]
- Fan, C.‐P. , Chen K.‐P., and Kan K.. 1998. “The Design of Payment Systems for Physicians under Global Budget – An Experimental Study.” Journal of Economic Behavior & Organization 34 (2): 295–311. [Google Scholar]
- Fan, V. Y. , and Savedoff W. D.. 2014. “The Health Financing Transition: A Conceptual Framework and Empirical Evidence.” Social Science & Medicine 105: 112–21. [DOI] [PubMed] [Google Scholar]
- Fuglenes, D. , Øian P., and Kristiansen I. S.. 2009. “Obstetricians’ Choice of Cesarean Delivery in Ambiguous Cases: Is It Influenced by Risk Attitude or Fear of Complaints and Litigation?” American Journal of Obstetrics and Gynecology 200 (1): 48. e1‐48.e8. [DOI] [PubMed] [Google Scholar]
- Grant, D. 2009. “Physician Financial Incentives and Cesarean Delivery: New Conclusions From the Healthcare Cost and Utilization Project.” Journal of Health Economics 28 (1): 244–50. [DOI] [PubMed] [Google Scholar]
- Gruber, J. , Kim J., and Mayzlin D.. 1999. “Physician Fees and Procedure Intensity: The Case of Cesarean Delivery.” Journal of Health Economics 18 (4): 473–90. [DOI] [PubMed] [Google Scholar]
- Gruber, J. , and Owings M.. 1996. “Physician Financial Incentives and Cesarean Section Delivery.” RAND Journal of Economics 27 (1): 99–123. [PubMed] [Google Scholar]
- Han, H.‐W. , and Lien H.‐M.. 2010. “Can Doubling the Payment for Vaginal Delivery Lower the Cesarean Section Rate in Taiwan?” Taiwan Journal of Public Health 29 (3): 218–27. [Google Scholar]
- Health Promotion Administration . 2014. “2014 Annual Report of Birth Registry Statistics” Available at http://www.hpa.gov.tw/Bhpnet/Web/HealthTopic/TopicArticle.aspx?No=201508170001&parentid=201109200006
- Hofmarcher, M. M. 2014. “The Austrian Health Reform 2013 Is Promising but Requires Continuous Political Ambition.” Health Policy 118 (1): 8–13. [DOI] [PubMed] [Google Scholar]
- Hsu, P.‐F. 2014. “Does a Global Budget Superimposed on Fee‐for‐Service Payments Mitigate Hospitals’ Medical Claims in Taiwan?” International Journal of Health Care Finance and Economics 14 (4): 369–84. [DOI] [PubMed] [Google Scholar]
- Klein, M. C. 2004. “Quick Fix Culture: The Cesarean‐Section‐on‐Demand Debate.” Birth 31 (3): 161–4. [DOI] [PubMed] [Google Scholar]
- Lavender, T. , Hofmeyr G. J., Neilson J. P., Kingdon C., and Gyte G. M.. 2012. “Caesarean Section for Non‐Medical Reasons at Term” In Cochrane Database of Systematic Reviews. Hoboken, NJ: John Wiley & Sons. [DOI] [PubMed] [Google Scholar]
- Lin, H.‐C. , and Xirasagar S.. 2004. “Institutional Factors in Cesarean Delivery Rates: Policy and Research Implications.” Obstetrics & Gynecology 103 (1). Available at http://journals.lww.com/greenjournal/Fulltext/2004/01000/Institutional_Factors_in_Cesarean_Delivery_Rates_22.aspx [DOI] [PubMed] [Google Scholar]
- Lo, J. C. 2003. “Patients’ Attitudes vs. Physicians’ Determination: Implications for Cesarean Sections.” Social Science & Medicine 57 (1): 91–6. [DOI] [PubMed] [Google Scholar]
- Long, S. H. , and Marquis M. S.. 1994. “Toward a Global Budget for the U.S. Health System: Implementation Issues and Information Needs,” Rand Issue Papers IP‐143 [accessed on November 22, 2015]. Available at http://www.rand.org/pubs/issue_papers/IP143/index2.html
- Mathematica . 2009. “Recommendations of the Special Commission on the Health Care Payment System,” 9‐197‐NaN‐1 Policy Brief to Massachusetts Special Commission on the Health Care Payment System, Commonwealth of Massachusetts, Division of Health Care Finance and Policy [accessed on November 18, 2015]. Available at http://archives.lib.state.ma.us/handle/2452/41295
- Mazzoni, A. , Althabe F., Liu N., Bonotti A., Gibbons L., Sánchez A., and Belizán J.. 2011. “Women's Preference for Caesarean Section: A Systematic Review and Meta‐Analysis of Observational Studies.” BJOG: An International Journal of Obstetrics & Gynaecology 118 (4): 391–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGuire, T. G. , and Pauly M. V.. 1991. “Physician Response to Fee Changes with Multiple Payers.” Journal of Health Economics 10 (4): 385–410. [DOI] [PubMed] [Google Scholar]
- McKenzie, L. , and Stephenson P. A.. 1993. “Variation in Cesarean Section Rates Among Hospitals in Washington State.” American Journal of Public Health 83 (8): 1109–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moreno‐Serra, R. 2014. “The Impact of Cost‐Containment Policies on Health Expenditure.” OECD Journal on Budgeting 13 (3): 1–29. [Google Scholar]
- Olson, M. 1965. The Logic of Collective Action. Cambridge, MA: Harvard University Press. [Google Scholar]
- Papke, L. E. , and Wooldridge J. M.. 2008. “Panel Data Methods for Fractional Response Variables with an Application to Test Pass Rates.” Journal of Econometrics 145 (1–2): 121–33. [Google Scholar]
- Schwartz, F. W. , Glennerster H., and Saltman R. B.. 1997. Fixing Health Budgets: Experience From Europe and North America. Hoboken, NJ: John Wiley & Sons. [Google Scholar]
- Song, Z. , Safran D. G., Landon B. E., Landrum M. B., He Y., Mechanic R. E., Day M. P., and Chernew M. E.. 2012. “The ‘Alternative Quality Contract’, Based on a Global Budget, Lowered Medical Spending and Improved Quality.” Health Affairs 31 (8): 1885–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spetz, J. , Smith M. W., and Ennis S. F.. 2001. “Physician Incentives and the Timing of Cesarean Sections: Evidence from California.” Medical Care 39 (6): 536–50. [DOI] [PubMed] [Google Scholar]
- Statistics Bureau . 2010. “Social Indicators 2009” [accessed on November 21, 2015]. Available at http://eng.stat.gov.tw/lp.asp?ctNode=3480&CtUnit=1344&BaseDSD=7&mp=5
- Tang, C.‐H. , Wu M.‐P., Liu J.‐T., Lin H.‐C., and Hsu C.‐C.. 2006. “Delayed Parenthood and the Risk of Cesarean Delivery—Is Paternal Age an Independent Risk Factor?” Birth 33 (1): 18–26. [DOI] [PubMed] [Google Scholar]
- Williams, R. 2015. “Analyzing Proportions: Fractional Response and Zero One Inflated Beta Models” [accessed on November 21, 2015]. Available at https://www3.nd.edu/~rwilliam/stats3/FractionalResponseModels.pdf
- Wolfe, P. R. , and Moran D. W.. 1992. “Global Budgeting in the OECD Countries.” Health Care Financing Review 14 (3): 55–76. [PMC free article] [PubMed] [Google Scholar]
- Wooldridge, J. M. 2011. “Fractional Response Models With Endogenous Explanatory Variables and Heterogeneity” [accessed on November 21, 2015]. Available at http://www.stata.com/meeting/chicago11/materials/chi11_wooldridge.pdf
- Yakoboski, P. J. , Ratner J., and Gross D. J.. 1994. “The Effectiveness of Budget Targets and Caps in the German Ambulatory Care Sector.” Benefits Quarterly 10 (3): 31. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix SA1: Author Matrix.
Appendix SA2:
Figure S1: Distribution in the Number of Total Annual Deliveries among Taiwanese Obstetricians, 2004.
Table S1: Negative Binomial Model to Investigate the Relationship between Point Value and Number of Cesarean Deliveries in Health Facilities.


