Abstract
Objective
To determine whether observed patterns of physician interaction around shared patients are associated with higher levels of teamwork as perceived by physicians.
Data Sources/Study Setting
Michigan Medicare beneficiaries who underwent coronary artery bypass grafting (CABG) procedures at 24 hospitals in the state between 2008 and 2011.
Study Design
We assessed hospital teamwork using the teamwork climate scale in the Safety Attitudes Questionnaire. After aggregating across CABG discharges at these hospitals, we mapped the physician referral networks (including both surgeons and nonsurgeons) that served them and measured three network properties: (1) reinforcement, (2) clustering, and (3) density. We then used multilevel regression models to identify associations between network properties and teamwork at the hospitals on which the networks were anchored.
Principal Findings
In hospitals where physicians repeatedly cared for patients with the same colleagues, physicians perceived better teamwork (β‐reinforcement = 3.28, p = .003). When physicians who worked together also had other colleagues in common, the reported teamwork was stronger (β clustering = 1.71, p = .001). Reported teamwork did not change when physicians worked with a higher proportion of other physicians at the hospital (β density = −0.58, p = .64).
Conclusion
In networks with higher levels of reinforcement and clustering, physicians perceive stronger teamwork, perhaps because the strong ties between them create a shared understanding; however, sharing patients with more physicians overall (i.e., density) did not lead to stronger teamwork. Clinical and organizational leaders may consider designing the structure of clinical teams to increase interactions with known colleagues and repeated interactions between providers.
Keywords: Social network analysis, teamwork, cardiac care, physician teams
During a treatment episode, patients often see multiple physicians dispersed across care locations. Typically, these physicians are responsible for only one aspect of their patient's treatment. Consequently, they may be unable to see the full picture, fail to communicate all needed information, lack the power to take all appropriate actions given what they know, or even have incentives to shift costs onto others (Carthey, de Leval, and Reason 2001; Hashem, Chi, and Friedman 2003; Stange 2009). To reduce such fragmentation, policy makers have launched several delivery system reforms that are designed to foster a team‐based approach to patient care, most notably, patient‐centered medical homes and accountable care organizations (Jackson et al. 2013; Pham, Cohen, and Conway 2014). The hope is that these initiatives will increase the sense that providers are part of a coordinated team, improve communication between care team members, and facilitate coordinated patient care across providers, functions, and operating units (de Brantes, Rosenthal, and Painter 2009). However, the antecedents of high‐functioning care teams are poorly understood (Makary et al. 2006).
In health care, one important aspect of teamwork is the ongoing interaction between physicians as they provide care to their shared patients (Leonard, Graham, and Bonacum 2004; Wahr et al. 2013). Recent studies using social network analysis have demonstrated that the structure of providers' referral networks—which form the backbone of ongoing interaction between physicians—is associated with the quality of patient care; however, the mechanisms through which the network influences patient outcomes are unclear (Barnett et al. 2012; Casalino et al. 2015). Research on teams indicates that ongoing interaction may influence team performance by improving the collaboration between personnel—that is, teamwork (Weick and Roberts 1993; Huckman, Staats, and Upton 2009). In turn, teams with high‐quality teamwork may perform better because they more readily support one another, making it easier to provide input and to ask questions (Edmondson, Bohmer, and Pisano 2001; Smith‐Jentsch et al. 2009).
In this study, we use social network analysis to identify the patterns of interaction among physicians that may influence the quality of the team's work, focusing on two mechanisms. First, as physician team members work together repeatedly in cohesive groups, they may become more familiar with each other's preferences, personalities, strengths, and weaknesses (Uzzi 1996; Dahlander and McFarland 2013; Hollingsworth et al. 2015). This may make it easier to seek support and to resolve disagreements through mutual understanding and may help build shared routines that foster better communication and more successful patient care. Second, teams that are highly interconnected, in which physicians work with a higher proportion of other physicians on the team—rather than just a few partners—may be more willing to invest time and effort into communication, exhibit more trust, and share in a common purpose (Moody and White 2003; Reagans and McEvily 2003), making it easier to receive and react to others' input and to speak up when a problem is identified, thereby strengthening teamwork.
To test these two hypotheses, we analyzed the medical claims from Medicare beneficiaries and survey data from the Michigan Hospital Association. Specifically, we used network analytic tools to measure the patterns of interaction among physicians who provided care to beneficiaries undergoing coronary artery bypass grafting (CABG) in Michigan between 2008 and 2011. We then related these patterns of interaction to the quality of teamwork, measured by the physicians' reports of teamwork climate at the hospitals where these beneficiaries' procedures were performed. Findings from our study will help guide interventions that aim to alter physician interactions to improve health care providers' teamwork.
Methods
Primary Data Source and Study Population
For this study, we analyzed data from the Centers for Medicare & Medicaid Services. We used appropriate International Classification of Diseases, Ninth Revision, Clinical Modification procedure codes to identify beneficiaries older than 65 years in the Medicare Provider Analysis and Review (MedPAR) Research Identifiable Files (RIF) who underwent a CABG procedure in a Michigan hospital between January 1, 2008, and December 31, 2011. We limited our cohort to those beneficiaries with continuous enrollment in Medicare Parts A and B for 6 months before surgery and 60 days after hospital discharge. We also excluded Medicare Advantage patients because the health services provided to them are inconsistently captured in their claims.
We chose to focus on CABG care for three reasons: (1) It is commonly performed on older adults, (2) it occurs exclusively on an inpatient basis, allowing for ready identification in medical claims, and (3) CABG episodes often involve multiple specialists and occur over long periods of time, making it an interesting example of team interaction. For example, a typical CABG episode may begin with a referral from a primary care provider (PCP) to a cardiologist for diagnostic testing. The cardiologist may then refer the patient to an interventional cardiologist for additional testing. If the tests show that a procedure is needed, the CABG procedure itself will be performed by a cardiac surgeon, and during the following recovery, the patient will be monitored by an intensivist, the surgeon, and the cardiologist. Finally, after being discharged from the hospital, the patient returns to his PCP and surgeon for follow‐up visits. The CABG episode is likely to be a challenging environment for high‐level team performance due to the multiple specialties involved, each with distinct expertise and roles, and the long time period over which the episode occurs. Finally, the importance of information sharing, trust, help‐seeking, and team cohesiveness is likely to be particularly high in this setting.
Mapping Physician Teams
Next, we sought to define the physician teams that cared for these beneficiaries around their surgical episodes through a previously described algorithm (Hollingsworth et al. 2015). In brief, we used the MedPAR, Outpatient, and Carrier RIFs to identify all of the PCPs and medical and surgical specialists who billed for services rendered during a claims window beginning 30 days prior to a beneficiary's surgery and extending 60 days after hospital discharge. We excluded physicians who do not provide direct patient care (e.g., radiologists) or who have limited roles in perioperative management.
For each hospital in Michigan where CABG procedures were performed, we aggregated across all discharges in a given year to generate a bipartite (or two‐mode) network for that hospital, such that ties connected physicians to their patients, and physicians were indirectly connected to other physicians through their shared patients. To examine the patterns of interaction among physicians in teams caring for shared patients, we developed three descriptive characteristics based on these bipartite networks:
Reinforcement
We measured the extent to which physicians work together repeatedly using a network measure called reinforcement. Reinforcement quantifies how frequently physicians in a bipartite network provide care for the same patients. To calculate reinforcement, we created a ratio of the number of physician pairs that share at least two patients proportionate to the number of physician pairs that share at least one patient (Robins and Alexander 2004). Repeated interactions between actors in networks are likely to improve communication between partners (Dahlander and McFarland 2013). In consequence, high reinforcement may be associated with stronger teamwork by increasing physicians' familiarity with their partners, by increasing the extent to which past routines and shared knowledge inform patient care, and by reducing the chance of misunderstanding.
Clustering Coefficient
To capture the extent to which physicians work in cohesive groups, we measured each hospital's bipartite clustering coefficient. The bipartite clustering coefficient measures the tendency for physicians that share patients to have other colleagues in common. To calculate the clustering coefficient, we counted the number of closed loops in which three physicians were connected to one another through a shared patient and divided by the number of nonclosed paths in which a physician shared two partner physicians (regardless of whether those partners shared a patient with each other) (Opsahl 2013). A high clustering coefficient reflects a more cohesive team of physicians that work within a group of shared colleagues. In contrast, in networks with low clustering coefficients, physicians share more patients with physician partners that do not, themselves, work together. In hospitals with high clustering coefficients, patient care will more often occur in a “closed loop” in which members have a history of communicating. These closed relationships may enhance the work of the team by allowing for collective action among shared partners to facilitate and guide common behavior (Coleman 1988).
Density
We also assessed the interconnectedness—that is, the proportion of other physicians on the team that each physician works with—using the network density measure. We calculated the density of each network as the proportion of ties between physicians and patients that exist out of all of the possible ties that could exist. In a dense network, all physicians would be connected by a shared patient. Density is believed to be associated with a stronger shared culture or set of norms (Coleman 1988; Uzzi 1996). As a result, high density may foster stronger teamwork across the hospital. However, in networks with high density, physicians on average work with a greater number of other physicians than physicians in networks with lower density, potentially limiting the benefits from repeated interactions described above.
Examples of bipartite physician–patient networks associated with two hospitals are presented in Figure 1. These networks were chosen because, although they are relatively similar in size, they differ notably on the three focal network characteristics.
Figure 1.
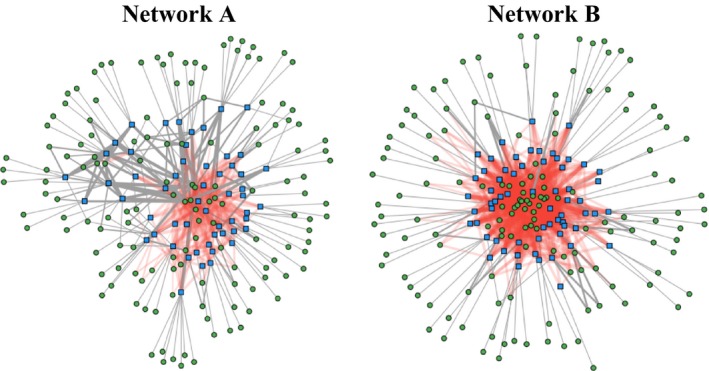
- Notes. Bipartite projection of physician–patient CABG care in two networks. In these figures, each green circle represents a physician and each blue square represents a patient. Each tie represents a treatment relationship between physician and patient, the thickness of each tie represents the log of the reinforcement of that relationship, and ties are colored red when more than half of the relationships they are part of are closed clusters. Although the two networks are of similar sizes, with 143 physicians and 55 patients in network A and 144 physicians and 63 patients in network B, network A has a reinforcement of 0.18, a clustering coefficient of 0.39, and a density of 0.06 while network B has a reinforcement of 0.31, a clustering coefficient of 0.71, and a density of 0.08. [Color figure can be viewed at wileyonlinelibrary.com]
Measuring Hospital Teamwork
Measuring teamwork is challenging, and no gold standard currently exists for capturing all dimensions of teamwork (Valentine, Nembhard, and Edmondson 2015). We chose to use the teamwork climate section of the Safety Attitudes Questionnaire (SAQ) because this scale captures dimensions of teamwork, including communication, coordination, and collaboration, that are likely to be particularly important to successful CABG care. Moreover, it is reliable, valid, and relates to patient outcomes (Sexton et al. 2006; Davenport et al. 2007; Valentine, Nembhard, and Edmondson 2015). The SAQ includes six items to assess respondents' perceptions of teamwork climate in their hospital. Each item is a statement that respondents are asked to assess using a five‐item Likert‐like scale, ranging from disagree strongly to agree strongly. The six statements are as follows: (1) Nurse input is well received in this work setting; (2) in this work setting, it is difficult to speak up if I perceive a problem with patient care (reverse coded); (3) disagreements in this work setting are resolved appropriately (i.e., not who is right, but what is best for the patient); (4) I have the support I need from others in this work setting to care for patients; (5) it is easy for personnel here to ask questions when there is something that they do not understand; and (6) the physicians and nurses here work together as a well‐coordinated team. We chose to use the full teamwork climate scale as the dependent variable in our main analyses because it has been previously validated; however, in robustness tests, we ensured that the pattern of results remained consistent when the first item, which relates specifically to nursing input and not the physician teams studied here, was removed. Responses to these six items are correlated, producing an overall Cronbach's alpha of 0.82, so we combined them into a single scale. In some cases, respondents skipped one or more questions. To account for this, we averaged respondents' score by the number of questions that they responded to.
Statistical Analysis
For our initial analytic step, we summarized the characteristics of individual respondents, the hospitals that they worked in, and the counties that the hospital served. Individual characteristics included the physician's age, gender, tenure, and job role (coded as attending, fellow, or resident); these may relate both to the structure of the team and the individual's perception of teamwork. We derived several hospital‐level characteristics from the American Hospital Association Annual Survey including the number of physicians and patients in the network, size (small [<100 beds], medium [100–399 beds] or large [400+ beds]), location (urban or rural), teaching status (none, minor, or major), ownership (for‐profit, nonprofit, or government), affiliation (independent, system, network, both system and network), the number of nurses per 1,000 inpatient days, and the percent of inpatient days for Medicaid and Medicare. In addition, we derived information about the county served by the hospital from the Area Health Resource File, including information about the population (the percent of individuals older than 25 years with a college education in the hospital's county, the percent living in an urban area, income per capita, proportion black, Hispanic, or older than 65 years) and the supply of health care (surgical specialists, PCPs, and hospital beds per 1,000 people). Hospital and geographic characteristics may be related to teamwork by influencing the resources available to the hospital and, by association, the stress placed on hospital staff and support available to them. In addition, geographic properties have been shown to correlate with several network properties (Hollingsworth et al. 2015).
Our data exhibit a multilevel structure wherein the individual providers that respond to the survey are nested within the hospitals in which they work. We used multilevel regression models to account for this nested structure. The dependent variable in these models was individual perceptions of teamwork. The independent variables were reinforcement, clustering, and density. In addition, to test whether the relationship between greater interconnectedness and teamwork depends on the level of reinforcement, we created a fourth model in which we interacted connectedness and reinforcement after de‐meaning each variable to reduce multicollinearity and facilitate interpretation (Aiken, West, and Reno 1991). In each model, we controlled for respondent, hospital, and region characteristics.
We present marginal effect estimates derived from these regression models to help interpret our results. To create these estimates, we first standardized the teamwork measure, so that one unit was equal to one standard deviation (SD). Next, holding all covariates at the mean, we varied each network measure from a low level (the 25th percentile) to a high level (the 75th percentile) and observed the change in standardized teamwork.
We performed our analyses using Stata IC 14. All tests were two‐tailed, and we set the probability of a type 1 error at 0.05. Our Institutional Review Board deemed that this study using de‐identified data was exempt from its oversight.
Results
Our sample included survey responses from 1,108 physicians practicing in the surgical and intensive care units of 24 hospitals (Table 1). Most respondents agreed with statements indicating that the quality of teamwork in their unit was high (average of 4.2 for physicians). There were no hospitals with fewer than 100 beds in our sample, likely because hospitals that size usually do not perform CABG. The majority of respondents practiced in not‐for‐profit teaching hospitals, and most practiced in hospitals that were part of a multihospital system.
Table 1.
Descriptive Statistics of Respondents, Providers, and Region
| Providers | |
| Physicians (n = 1,108) | |
| Teamwork climate | 4.2 |
| Tenure | 5.6 |
| Female | 16.5% |
| Hospitals | Average |
| Reinforcement of ties | 0.23 |
| Clustering coefficient | 0.48 |
| Density | 0.06 |
| Size | |
| Small | – |
| Medium | 45% |
| Large | 55% |
| Location | |
| Urban | 87.4% |
| Rural | 12.6% |
| Teaching status | |
| None | 17.9% |
| Minor | 32.7% |
| Major | 49.3% |
| Ownership | |
| For‐profit | 1.01% |
| Nonprofit | 98.9% |
| Government | – |
| Affiliation | |
| Independent | 24.4% |
| System | 26.1% |
| Network | – |
| System and network | 51.7% |
| Hospitals—continuous variables | |
| Nurses per thousand inpatient days | 8 |
| Percent Medicaid inpatient days | 13.4% |
| Percent Medicare inpatient days | 55.2% |
| Region | |
| College educated | 31.5% |
| Live in urban area | 83.8% |
| Income per capita | 38,793 |
| Specialty physicians per 1k | 1.34 |
| Surgeons per 1k | 0.74 |
| Primary care providers per 1k | 1.06 |
| Beds per 1k | 3.2 |
| Proportion black | 15.7% |
| Proportion Hispanic | 4.08% |
| Proportion older than 65 years | 13.1% |
We first investigated whether the structure of physicians' interactions influenced physicians' perceptions of teamwork. We found that both reinforcement, which measured the frequency of repeated interaction between physicians, and clustering, which measured the extent to which physicians shared the same colleagues, were associated with higher levels of reported teamwork after controlling for observed individual and hospital characteristics (p = .006 and p = .004, respectively [Table 2]).
Table 2.
Relationship between Teamwork Climate and Network Characteristics: Multilevel Random Effect Regressions
| Teamwork Climate | (1) | (2) | (3) | (4) |
|---|---|---|---|---|
| Reinforcement | 3.12*** (1.13) | 4.952*** (1.375) | ||
| Clustering coefficient | 1.69*** (0.58) | |||
| Network density | −0.58 (2.18) | −6.996** (3.012) | ||
| Reinforcement*density | 33.02 (23.92) | |||
| Observations | 1,108 | 1,108 | 1,108 | |
| Number of groups | 24 | 24 | 24 |
Standard errors in parentheses ***p < .01, **p < .05, *p < .1.
Our measure of interconnectedness across the unit, density, was generated by physicians working with a high proportion of other physicians at the hospital. We found that density was not directly associated with higher teamwork (p = .641). However, when density and reinforcement were interacted, we found that density was associated with lower teamwork (p = .020) at the average level of reinforcement and that the interaction between density and reinforcement was positive and trending toward statistical significance (p = .16), suggesting that greater interconnectedness may have a negative effect at low levels of reinforcement, but the negative effect may become smaller at higher levels of reinforcement. All patterns of results remained consistent in a robustness test excluding one item from the teamwork scale (Table S2).
To help interpret these results and provide a sense of magnitude, we produced marginal estimates of these relationships using a standardized measure of teamwork (Figure 2). Moving from low to high reinforcement was associated with an increase in teamwork of 50 percent of an SD. An increase in clustering was associated with a change of 59 percent of an SD for physicians.
Figure 2.
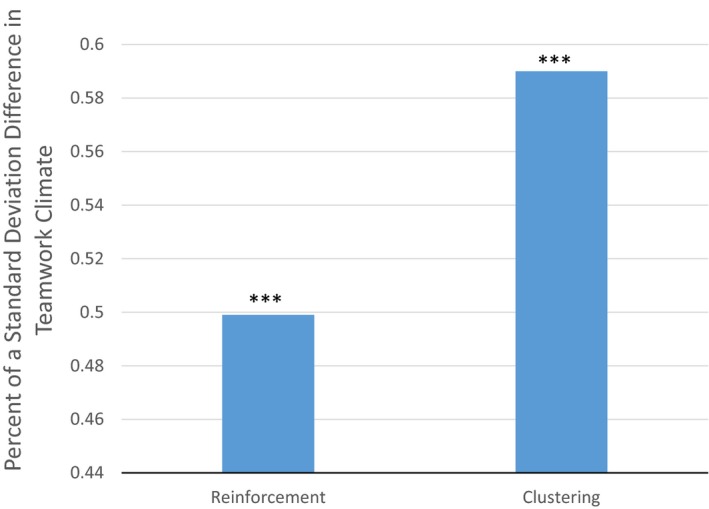
Difference in Teamwork Climate between Hospitals at 25th and 75th Percentile of Three Network Measures [Color figure can be viewed at wileyonlinelibrary.com]
We found that when reinforcement was set 1 SD below the mean, a change from −1 to 1 SD in density was associated with a change in teamwork equivalent to 77 percent of an SD, whereas when reinforcement was set 1 SD above the mean, a change from 1 SD below to 1 SD above the mean was associated with a smaller decrease of 40 percent of an SD. In Figure S1, we show the marginal effects of the interaction between density and reinforcement.
Discussion
In this study, we sought to understand how the patterns of physician interaction around shared patients during CABG episodes were related to physicians' perception of teamwork in the surgical units and intensive care units where these patients were treated. Drawing from network theory and the literature on team familiarity, we hypothesized that repeated and cohesive small group interactions may be associated with stronger teamwork by facilitating the development of familiarity and shared routines and that networks where physicians were connected to many other physicians might also be associated with stronger teamwork by creating shared norms and trust across the entire network. While we found support for our first hypothesis, we did not find that greater hospital‐wide interconnectedness created by physicians working with more other physicians was associated with stronger teamwork. Instead, we found that greater interconnectedness was associated with weaker teamwork when it was accompanied by a low level of reinforcement. This suggests that the specific patterns of physician interaction in patient care provide a basis for learning and the development of helpful communication practices.
Guidelines for CABG surgery highlight the importance of building successful interdisciplinary teams made up of cardiac surgeons, cardiologists, and PCPs to facilitate shared and balanced decision making (Group et al. 2012; Holmes et al. 2013). As providers and organizations work to build interdisciplinary teams, they should consider not only the expertise possessed by each team member but also how proposed changes might best alter physician interaction to create a basis for collaborative teams providing improved patient care. Our findings indicate that these interdisciplinary teams may work together most successfully when members have experience working with one another as a relatively stable team, and when multiple team members have worked with one another in the care of shared partners, rather than when team composition is more fluid.
Our findings contribute to the literature on team familiarity by further investigating the implications of the structure of interactions between individuals. Existing studies largely measure team familiarity using aggregate measures of a group's past experience working together, such as the average number of times each pair of members on a team have worked together in the past, or the number of times that the team as a whole has previously worked together (Reagans, Argote, and Brooks 2005; Espinosa et al. 2007; Huckman and Staats 2011; Xu et al. 2013). While useful, this approach does not offer insight into the relevance of the structure or pattern of the team's past experience working together. Our finding of an association between reinforcement, clustering, and teamwork, but not density and teamwork, offers suggestive evidence that network closure may be helpful to promoting productive teams. In contrast, simply having a large proportion of ties present in the network may inhibit the work of the team when it is not grounded in a sufficient number of reinforced ties.
Our study also has implications for the mechanisms by which physician referral networks are associated with patient outcomes. Prior research has focused on the relationship between network membership or network structure and outcomes (Barnett et al. 2012; Pollack et al. 2014; Casalino et al. 2015). Our findings suggest that network structure may help by improving the team's ability to work together. Future research directly testing a mediation model, in which the impact of network structure on outcomes is driven by its effect on teamwork, is needed to better understand the mechanisms we investigate here.
This study has several limitations. First, we used a cross‐sectional design that allows for the identification of associations, but not for causal identification of the link between patterns of physician interaction and teamwork. It is also possible that hospitals with successful teamwork facilitate the creation of reinforced, clustered networks, so that the direction of causality is the reverse of our models. Second, our outcome is the perceived quality of teamwork. We do not directly measure the successful functioning of teams or patient outcomes. We hypothesized that different patterns of physician interaction would be more proximately associated with the quality of teamwork than with other measures of quality and therefore easier to measure given a restricted sample. Further, teamwork quality may act as a key mechanism through which these patterns of physician interaction influence patient outcomes. However, it may also be that patterns of interaction are associated more with perception than reality, and the available data do not allow us to separate these. Third, we examined the relationship between one surgical procedure (CABG) and teamwork in the operating room and intensive care unit, but other procedures with their own networks are undertaken in these areas and might also relate to the overall work of the team. In subsequent analyses, we noted that the structure of hospitals' physician–patient CABG network was closely correlated with hospitals' physician–patient networks for two other diverse procedures (colectomy and total hip replacement). As a result, we view CABG as an important case in its own right and a tracer for the networks of other procedures at the hospitals studied. Fourth, our measure of reinforcement, drawn from the network literature, only accounts for whether two physicians shared more than one patient, but it does not capture the number of patients shared beyond two (Robins and Alexander 2004; Opsahl 2013). It may be that higher levels of repeated interactions provide additional benefit. However, in our data, only 11 percent of physician pairs shared more than two patients a year, indicating that our measure characterizes the majority of repeat interactions. Finally, we examine only a small subset of hospitals and it is possible that there is something unique about the subset of hospitals for which we have teamwork data that limits the generalizability of this study to other hospitals that perform CABG.
Despite these limitations, we find suggestive evidence that the patterns of physician interaction relate to the quality of the team's work. This study represents an early effort to understand this potentially important relationship, and there is a great deal more to learn about how physician interaction influences the functioning of teams in health care. As such, our findings suggest several next steps. While there is a growing literature on the relationship between physician networks and outcomes (Barnett et al. 2012; Casalino et al. 2015), more attention to the intermediary mechanisms, such as teamwork, patient safety culture, and provider communication habits, may be essential to understanding how network patterns influence patient outcomes. It will also be important to assess whether our results are consistent in other surgical and nonsurgical episodes of care comprised of different types of care teams, including different combinations of specialties and different types of coordination. We have selected key network characteristics that seemed most likely to influence teamwork functioning; however, future studies might consider the impact of additional network characteristics. Finally, as policies and organizational initiatives are implemented to alter the effectiveness of care teams, it will be essential to include an assessment of how these initiatives change the patterns of interaction among providers in ways that either foster or disrupt provider interactions that lead to strong teamwork and beneficial patient outcomes.
Supporting information
Appendix SA1: Author Matrix.
Table S1. Full Random Effects Regression Models.
Table S2. Random Effects Model Omitting Nursing Input Component of Teamwork.
Figure S1. Marginal Effect of the Interaction between Reinforcement and Density.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: The Michigan Health & Hospital Association provided data from the Safety Attitude Questionnaire. This study was funded, in part, by Agency for Healthcare Research and Quality (grant 1 R01HS024525 01A1 and 1 R01 HS024728 01 to John M. Hollingsworth). Brahmajee Nallamothu has received honoraria from the Cardiac Advisory Board of UnitedHealthcare (past), American College of Cardiology (past), and the American Heart Association (present).
Disclosures: None.
Disclaimer: None.
References
- Aiken, L. S. , West S. G., and Reno R. R.. 1991. Multiple Regression: Testing and Interpreting Interactions. Thousand Oaks, CA: Sage. [Google Scholar]
- Barnett, M. L. , Christakis N. A., O'Malley A. J., Onnela J.‐P., Keating N. L., and Landon B. E.. 2012. “Physician Patient‐Sharing Networks and the Cost and Intensity of Care in US Hospitals.” Medical Care 50 (2): 152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Brantes, F. , Rosenthal M. B., and Painter M.. 2009. “Building a Bridge from Fragmentation to Accountability—The Prometheus Payment Model.” New England Journal of Medicine 361 (11): 1033–6. [DOI] [PubMed] [Google Scholar]
- Carthey, J. , de Leval M. R., and Reason J. T.. 2001. “The Human Factor in Cardiac Surgery: Errors and Near Misses in a High Technology Medical Domain.” Annals of Thoracic Surgery 72 (1): 300–5. [DOI] [PubMed] [Google Scholar]
- Casalino, L. P. , Pesko M. F., Ryan A. M., Nyweide D. J., Iwashyna T. J., Sun X., Mendelsohn J., and Moody J.. 2015. “Physician Networks and Ambulatory Care‐Sensitive Admissions.” Medical Care 53 (6): 534–41. [DOI] [PubMed] [Google Scholar]
- Coleman, J. S. 1988. “Social Capital in the Creation of Human Capital.” American Journal of Sociology 00: S95–120. [Google Scholar]
- Dahlander, L. , and McFarland D. A.. 2013. “Ties That Last Tie Formation and Persistence in Research Collaborations over Time.” Administrative Science Quarterly 58 (1): 69–110. [Google Scholar]
- Davenport, D. L. , Henderson W. G., Mosca C. L., Khuri S. F., and Mentzer R. M.. 2007. “Risk‐Adjusted Morbidity in Teaching Hospitals Correlates with Reported Levels of Communication and Collaboration on Surgical Teams but Not with Scale Measures of Teamwork Climate, Safety Climate, or Working Conditions.” Journal of the American College of Surgeons 205 (6): 778–84. [DOI] [PubMed] [Google Scholar]
- Edmondson, A. C. , Bohmer R. M., and Pisano G. P.. 2001. “Disrupted Routines: Team Learning and New Technology Implementation in Hospitals.” Administrative Science Quarterly 46 (4): 685–716. [Google Scholar]
- Espinosa, J. A. , Slaughter S. A., Kraut R. E., and Herbsleb J. D.. 2007. “Team Knowledge and Coordination in Geographically Distributed Software Development.” Journal of Management Information Systems 24 (1): 135–69. [Google Scholar]
- Group, C. R. W. , Patel M. R., Dehmer G. J., Hirshfeld J. W., Smith P. K., Spertus J. A., Panel T., Masoudi F. A., Chambers C. E., and Ferguson T. B.. 2012. “ACCF/SCAI/STS/AATS/AHA/ASNC/HFSA/SCCT 2012 Appropriate Use Criteria for Coronary Revascularization Focused Update: A Report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, Society for Cardiovascular Angiography and Interventions, Society of Thoracic Surgeons, American Association for Thoracic Surgery, American Heart Association, American Society of Nuclear Cardiology, and the Society of Cardiovascular Computed Tomography.” Journal of Thoracic and Cardiovascular Surgery 143 (4): 780–803. [DOI] [PubMed] [Google Scholar]
- Hashem, A. , Chi M. T., and Friedman C. P.. 2003. “Medical Errors as a Result of Specialization.” Journal of Biomedical Informatics 36 (1): 61–9. [DOI] [PubMed] [Google Scholar]
- Hollingsworth, J. M. , Funk R. J., Garrison S. A., Owen‐Smith J., Kaufman S. R., Landon B. E., and Birkmeyer J. D.. 2015. “Differences Between Physician Social Networks for Cardiac Surgery Serving Communities with High Versus Low Proportions of Black Residents.” Medical Care 53 (2): 160–7. [DOI] [PubMed] [Google Scholar]
- Holmes, D. R. , Rich J. B., Zoghbi W. A., and Mack M. J.. 2013. “The Heart Team of Cardiovascular Care.” Journal of the American College of Cardiology 61 (9): 903–7. [DOI] [PubMed] [Google Scholar]
- Huckman, R. S. , and Staats B. R.. 2011. “Fluid Tasks and Fluid Teams: The Impact of Diversity in Experience and Team Familiarity on Team Performance.” Manufacturing & Service Operations Management 13 (3): 310–28. [Google Scholar]
- Huckman, R. S. , Staats B. R., and Upton D. M.. 2009. “Team Familiarity, Role Experience, and Performance: Evidence from Indian Software Services.” Management Science 55 (1): 85–100. [Google Scholar]
- Jackson, G. L. , Powers B. J., Chatterjee R., Bettger J. P., Kemper A. R., Hasselblad V., Dolor R. J., Irvine R. J., Heidenfelder B. L., and Kendrick A. S.. 2013. “The Patient‐Centered Medical Home: A Systematic Review.” Annals of Internal Medicine 158 (3): 169–78. [DOI] [PubMed] [Google Scholar]
- Leonard, M. , Graham S., and Bonacum D.. 2004. “The Human Factor: The Critical Importance of Effective Teamwork and Communication in Providing Safe Care.” Quality and Safety in Health Care 13 (suppl 1): i85–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Makary, M. A. , Sexton J. B., Freischlag J. A., Holzmueller C. G., Millman E. A., Rowen L., and Pronovost P. J.. 2006. “Operating Room Teamwork among Physicians and Nurses: Teamwork in the Eye of the Beholder.” Journal of the American College of Surgeons 202 (5): 746–52. [DOI] [PubMed] [Google Scholar]
- Moody, J. , and White D. R.. 2003. “Structural Cohesion and Embeddedness: A Hierarchical Concept of Social Groups.” American Sociological Review 68 (1):103–27. [Google Scholar]
- Opsahl, T. 2013. “Triadic Closure in Two‐Mode Networks: Redefining the Global and Local Clustering Coefficients.” Social Networks 35 (2): 159–67. [Google Scholar]
- Pham, H. H. , Cohen M., and Conway P. H.. 2014. “The Pioneer Accountable Care Organization Model: Improving Quality and Lowering Costs.” Journal of the American Medical Association 312 (16): 1635–6. [DOI] [PubMed] [Google Scholar]
- Pollack, C. E. , Wang H., Bekelman J. E., Weissman G., Epstein A. J., Liao K., Dugoff E. H., and Armstrong K.. 2014. “Physician Social Networks and Variation in Rates of Complications after Radical Prostatectomy.” Value in Health 17 (5): 611–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reagans, R. , Argote L., and Brooks D.. 2005. “Individual Experience and Experience Working Together: Predicting Learning Rates from Knowing Who Knows What and Knowing How to Work Together.” Management Science 51 (6): 869–81. [Google Scholar]
- Reagans, R. , and McEvily B.. 2003. “Network Structure and Knowledge Transfer: The Effects of Cohesion and Range.” Administrative Science Quarterly 48 (2): 240–67. [Google Scholar]
- Robins, G. , and Alexander M.. 2004. “Small Worlds among Interlocking Directors: Network Structure and Distance in Bipartite Graphs.” Computational & Mathematical Organization Theory 10 (1): 69–94. [Google Scholar]
- Sexton, J. B. , Makary M. A., Tersigni A. R., Pryor D., Hendrich A., Thomas E. J., Holzmueller C. G., Knight A. P., Wu Y., and Pronovost P. J.. 2006. “Teamwork in the Operating RoomFrontline Perspectives among Hospitals and Operating Room Personnel.” Journal of the American Society of Anesthesiologists 105 (5): 877–84. [DOI] [PubMed] [Google Scholar]
- Smith‐Jentsch, K. A. , Kraiger K., Cannon‐Bowers J. A., and Salas E.. 2009. “Do Familiar Teammates Request and Accept More Backup? Transactive Memory in Air Traffic Control.” Human Factors: The Journal of the Human Factors and Ergonomics Society 51 (2): 181–92. [DOI] [PubMed] [Google Scholar]
- Stange, K. C. 2009. “The Problem of Fragmentation and the Need for Integrative Solutions.” Annals of Family Medicine 7 (2): 100–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uzzi, B. 1996. “The Sources and Consequences of Embeddedness for the Economic Performance of Organizations: The Network Effect.” American Sociological Review 674–98. [Google Scholar]
- Valentine, M. A. , Nembhard I. M., and Edmondson A. C.. 2015. “Measuring Teamwork in Health Care Settings: A Review of Survey Instruments.” Medical Care 53 (4): e16–30. [DOI] [PubMed] [Google Scholar]
- Wahr, J. A. , Prager R. L., Abernathy J., Martinez E. A., Salas E., Seifert P. C., Groom R. C., Spiess B. D., Searles B. E., and Sundt T. M.. 2013. “Patient Safety in the Cardiac Operating Room: Human Factors and Teamwork: A Scientific Statement from the American Heart Association.” Circulation 128 (10): 1139–69. [DOI] [PubMed] [Google Scholar]
- Weick, K. E. , and Roberts K. H.. 1993. “Collective Mind in Organizations: Heedful Interrelating on Flight Decks.” Administrative Science Quarterly 38 (3):357–81. [Google Scholar]
- Xu, R. , Carty M. J., Orgill D. P., Lipsitz S. R., and Duclos A.. 2013. “The Teaming Curve: A Longitudinal Study of the Influence of Surgical Team Familiarity on Operative Time.” Annals of Surgery 258 (6): 953–7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix SA1: Author Matrix.
Table S1. Full Random Effects Regression Models.
Table S2. Random Effects Model Omitting Nursing Input Component of Teamwork.
Figure S1. Marginal Effect of the Interaction between Reinforcement and Density.


