Abstract
Aims
Prescribing errors are an important cause of patient safety incidents and are frequently caused by junior doctors. This might be because the prescribing competence of final‐year medical students is poor as a result of inadequate clinical pharmacology and therapeutic (CPT) education. We reviewed the literature to investigate which prescribing competencies medical students should have acquired in order to prescribe safely and effectively, and whether these have been attained by the time they graduate.
Methods
PubMed, EMBASE and ERIC databases were searched from the earliest dates up to and including January 2017, using the terms ‘prescribing’, ‘competence’ and ‘medical students’ in combination. Articles describing or evaluating essential prescribing competencies of final‐year medical students were included.
Results
Twenty‐five articles describing, and 47 articles evaluating, the prescribing competencies of final‐year students were included. Although there seems to be some agreement, we found no clear consensus among CPT teachers on which prescribing competencies medical students should have when they graduate. Studies showed that students had a general lack of preparedness, self‐confidence, knowledge and skills, specifically regarding general and antimicrobial prescribing and pharmacovigilance. However, the results should be interpreted with caution, given the heterogeneity and methodological weaknesses of the included studies.
Conclusions
There is considerable evidence that final‐year students have insufficient competencies to prescribe safely and effectively, although there is a need for a greater consensus among CPT teachers on the required competencies. Changes in undergraduate CPT education are urgently required in order to improve the prescribing of future doctors.
Keywords: clinical pharmacology, competence, medical curriculum, medical student, pharmacotherapy, prescribing, therapeutics
What is Already Known about this Subject
Prescribing errors can result in patient harm and high healthcare costs.
Junior doctors write many prescriptions in hospitals but one in 10 of their prescriptions may contain errors, in part because of poor prescribing competencies.
It is not clear whether medical students lack essential prescribing skills and competencies when they graduate.
What this Study Adds
There is a need for a greater consensus among clinical pharmacology and therapeutics teachers on the competencies that medical students should have in order to prescribe safely and effectively.
Despite the lack of a consensus, there is considerable evidence that final‐year medical students have not attained sufficient competencies for safe and effective prescribing as medical doctors, especially regarding general and antimicrobial prescribing and pharmacovigilance.
Changes in clinical pharmacology and therapeutics education during the undergraduate medical curriculum are urgently required, in order to improve the prescribing competencies of future doctors.
Introduction
Rational prescribing (i.e. effectively, safely and at low cost) is a challenging task for every medical doctor as it involves a mixture of knowledge, skills and attitudes integrated into the complex social context of the clinical workplace 1. Poor prescribing may result in prescribing errors and adverse drugs reactions, which could adversely affect patient outcomes, leading to hospitalization or even death 2, 3. There is considerable evidence that junior hospital doctors in the first 2 years of practice after graduation make relatively many prescribing errors (8–10% of prescriptions) and are more likely to make these errors than consultants 4, 5, 6. This is particularly worrying as junior doctors write a large proportion (68%) of hospital prescriptions 5.
Studies have identified a range of factors underlying the poor prescribing skills of junior doctors, including individual (e.g. lack of experience), environmental (e.g. high workload), organizational (e.g. lack of standardization) and patient (e.g. polypharmacy) factors 4, 7, 8. A lack of prescribing competencies (i.e. knowledge, skills and attitudes) among junior doctors is frequently mentioned 7, 9, which might be due to inadequate undergraduate education and training in clinical pharmacology and therapeutics (CPT). Indeed, a recent study showed that European final‐year medical students lacked essential prescribing competencies and felt that their medical curriculum had not adequately prepared them for safe prescribing 10. Another recent study showed that CPT education across Europe is still mainly based on traditional learning methods (e.g. lectures and written examinations), which seem to be associated with a lower level of prescribing knowledge and skills among final‐year students than problem‐based learning methods (e.g. patient simulation and real‐life prescribing) 11.
Although these findings are concerning, there is no comprehensive overview of the literature addressing the competencies that medical students should have acquired in order to prescribe safely and effectively as medical doctors, and whether these have been attained by the time they graduate. Previous literature reviews focused mainly on the prevalence and causes of prescribing errors made by junior doctors 12, 13. By shifting the focus to final‐year students rather than junior doctors, we aimed to identify possible shortcomings in undergraduate CPT education that could be improved in the future. To this end, we conducted a systematic search of the peer‐reviewed literature with the following two research questions: (i) which prescribing competencies should medical students have acquired in order to prescribe safely and effectively by the time they graduate?; and (ii) do final‐year medical students have sufficient prescribing competencies?
Methods
Data sources and literature search strategy
We performed a systematic search to identify descriptive or observational studies of the prescribing competencies of final‐year medical students. The review was conducted and performed according to the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) guidelines 14. The study protocol was registered in the PROSPERO database (registration number CRD42017067063). With the assistance of a medical information specialist (R.O.), we searched the PubMed, Excerpta Medica Database (EMBASE) and Education Resources Information Center (ERIC) databases systematically from the earliest dates up to 10 January 2017. PubMed was used as the standard medical research database, and the EMBASE and ERIC databases were used to detect articles published in more education‐orientated journals. For each database, the search terms used were variations of three key concepts: competence, prescribing and medical student. Full details of the search strategy in PubMed, EMBASE and ERIC are provided in Appendix S1. Duplicate articles were excluded and the remaining articles were screened for eligibility. Articles that were not available in digital form were retrieved from national university libraries or from the original author. The references of relevant articles were also screened using the forward and backward snowball method 15.
Study selection
First, two researchers (D.B. and S.G.) screened the titles and abstracts independently for eligibility. Disagreements were resolved by consensus with a third researcher (J.T.). Articles were included if they described prescribing competencies that medical graduates should have acquired or if they evaluated prescribing competencies of final‐year medical students. Prescribing competencies were defined as knowledge, skills or attitudes that are relevant to safe and effective prescribing. Final‐year medical students were defined as students who would graduate from medical school within 1 year or who had recently graduated but had not yet started working as a junior doctor (i.e. medical graduates). The following exclusion criteria were used: (i) outcome measure not related to prescribing competencies; (ii) intervention studies (e.g. evaluation of a specific educational intervention or teaching method); (iii) not including final‐year medical students (e.g. focusing only on lower‐grade medical students, junior doctors); (iv) non‐original research (i.e. reviews, editorials, letters to the editor, conference abstracts, symposium reports); (v) articles that only measure psychometric properties of assessments (e.g. validity, reliability); (vi) languages other than English, German or Dutch; and (vii) abstract not available. Reasons for exclusion were documented (Figure 1). In cases of doubt, the full‐text article was obtained and screened. Thereafter, the researchers screened the full‐text articles for eligibility, using the same inclusion and exclusion criteria as above, with the additional exclusion criterion of full‐text not available.
Figure 1.
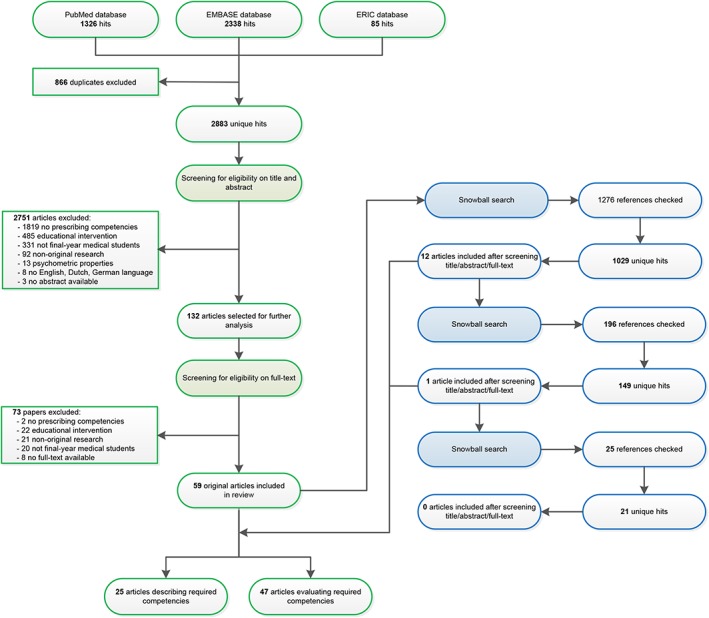
Flowchart of the systematic literature search
Data extraction and quality assessment
Data were extracted using the Best Evidence Medical Education (BEME) Collaboration coding sheet (Appendix S2) 16. The BEME coding items used were administrative, context, stated aim of study and documented performance. The Kirkpatrick model of hierarchy of evaluation, modified by Freeth, was used to evaluate the outcome level (Table 2) 17, 18. The main CPT topics were identified and the methodological quality of articles evaluating prescribing competencies was assessed using the Medical Education Research Quality Instrument (MERSQI) 19. It was not possible to use this instrument for articles describing competencies as almost all articles were based on expert opinion and did not provide quantitative data. The MERSQI instrument consists of six domains: study design, sampling, type of data, validation of evaluation instrument, data analysis and outcomes measured. The maximum score for each domain was 3, producing a maximum possible score of 18 and a potential range of 5–18. Although there is no defined cut‐off for high‐ or low‐quality study methods, a previous study used a MERSQI score of 14 or higher as a cut‐off for high quality 20. Two researchers (D.B. and S.G.) extracted data and assessed data quality independently, with a third author (J.T.) being involved, if necessary, to reach a consensus.
Data analysis
All descriptive analyses were performed in IBM SPSS version 22.0 (Chicago, IL). The total mean MERSQI score (accounting for ‘non‐applicable’ responses) was calculated. Moreover, the proportion of articles published in different years, on different continents and involving different health professions was calculated. Given the variety of study designs and outcomes studied, no quantitative analysis or additional analysis of risk for bias was performed.
Results
Search results
The initial search identified 3749 articles. The flowchart of the search, selection and review process is presented in Figure 1. Eleven articles could not be obtained from either the library or the corresponding authors, and were thus excluded. In total, 59 articles met the inclusion criteria; the 1276 references from these articles were snowball‐searched, which yielded 13 new articles. In total, 72 articles were included in the qualitative analysis, of which 25 described (Table 1) and 47 evaluated (Table 2) the competencies of final‐year medical students.
Table 1.
Identified articles (n = 25) describing the prescribing competencies of final‐year medical students
| Author | Country | Aim | CPT topic | Methods | Main results |
|---|---|---|---|---|---|
| Antman et al. (2016) 71 | USA | To define core competencies for the prevention and management of prescription drug misuse for medical education | Drug misuse | Evidence based on the opinion of a working group consisting of 4 deans and 2 leaders of medical societies in one country | 10 core competencies for the prevention and management of prescription drug misuse |
| Baker et al. (2011) 75 | UK | To develop a core list of 100 commonly prescribed drugs to support prescribing education | General prescribing | Evidence‐based retrospective analysis of prescribing data from primary and secondary care and a cross‐sectional survey among 148 FY1 doctors | A core list of 100 commonly prescribed drugs that is useful for teaching prescribing |
| Banna et al. (1994) 100 | United Arab Emirates | To present a core curriculum for the teaching of pharmacology and therapeutics for medical students | General prescribing | Evidence based on the opinion of 4 CPT teachers from one institution | 27 knowledge objectives and 21 skill objectives for pharmacology and therapeutics education |
| Borgeat et al. (1985) 72 | Canada | To describe specific learning objectives for the teaching therapeutic skills of a psychological nature to future physicians | Psychotherapy | Evidence based on the opinion of psychiatry teachers from one institution | 3 cognitive, 14 aptitudinal, and 5 attitudinal objectives for teaching therapeutics skill of a psychological nature |
| Davenport et al. (2005) 67 | UK; BSAC | To define learning outcomes for prudent antimicrobial prescribing to undergraduate medical students | Antimicrobial prescribing and resistance | Evidence based on the opinion of 2 working groups consisting of teachers from multiple institutions in one country | 12 learning objective domains for undergraduate education of prudent antibiotic prescribing |
| de Vries (1993) 63 | The Netherlands | To define a framework for the whole problem‐solving prescribing process and the learning objectives for medical education that can be derived from it | General prescribing | Evidence based on the opinion of general practitioners and clinical pharmacologists from multiple institutions in one country | 8 cognitive skills, 2 motor skills and 6 communication skills for CPT education |
| Donnenberg et al. (2016) 66 | USA; ACCP | To develop a comprehensive set of guidelines in clinical pharmacology for entering residency | General prescribing | Evidence based on the opinion of medical teachers from multiple institutions in one country | 8 topics for clinical pharmacology education |
| Flockhart et al. (2002) 65 | USA | To design and evaluate a core curriculum in CPT for final‐year medical students | General prescribing | Evidence based on a literature survey and the opinion of CPT teachers from 2 institutions in one country | 13 learning objectives for a core curriculum in CPT |
| Gitanjali & Shashindran (2006) 101 | India; IPS | To develop a draft curriculum for clinical pharmacology for medical undergraduates | General prescribing | Evidence based on a modified Delphi studya among pharmacologists of multiple institutions in one country | 13 knowledge, 3 psychomotor skills, 12 attitudes, and communication skills for clinical pharmacology education |
| Lum et al. (2013) 64 | Australia | To develop a set of national competencies for teaching safe and effective prescribing during the medical curriculum | General prescribing | Evidence based on the opinion of 3 teachers from 3 institutions in one country | 12 core competencies for safe and effective prescribing education |
| Mathur (2004) 102 | India | To describe a pharmacology curriculum for medical students | General prescribing | Evidence based on the opinion of 1 pharmacologist from one institution | 8 learning objectives for teaching pharmacology |
| Maxwell & Walley (2003) 60 | UK | To define national learning outcomes in CPT and to identify the minimum knowledge for medical graduates to prescribe safely and effectively | General prescribing | Evidence based on the opinion of 2 CPT teachers from 2 institutions in one country | 48 core knowledge and understanding, 35 core skill, 19 core attitude learning outcomes for CPT education. 201 core drugs and 148 core diseases that students should know about |
| Midlöv et al. (2015) 53 | Sweden | To identify the core competencies in basic and clinical pharmacology for medical students | General prescribing | Evidence based on a modified three‐round Delphi study involving 25 physicians of multiple institutions in one country | 40 core competencies for basic and clinical pharmacology education |
| Murison et al. (2013) 69 | USA; AAPM | To define learning outcomes for a new pain medicine curriculum for medical students | Pain medicine | Evidence based on a literature survey among 15 pain physicians of multiple institutions in one country | 27 recommended topics for pain medicine |
| Nierenberg (1990) 58 | USA; CMSECPT | To formulate an essential core curriculum for medical students in CPT | General prescribing | Evidence based on a consensus among 40 faculty members and council representatives of multiple institutions in one country | 17 core knowledge, 16 core skill and 5 core attitude learning outcomes for CPT education |
| O'Brien et al. (2009) 73 | USA | To describe the development and implementation of a pharmacogenomics course for health professional students | Pharmacogenomics | Evidence based on the opinion of a group of medical and health science teachers from 2 institutions in one country | 7 molecular knowledge, 8 pharmacology knowledge and 7 technical skill learning outcomes for pharmacogenomics education |
| Orme et al. (2002) 74 | EACPT | To develop a list of essential drugs and diseases for a core curriculum in CPT | General prescribing | Evidence based on the opinion of a working group of 9 CPT teachers from nine different European countries | A list of 120 drugs that students must know about, 47 drugs that students must be aware of; 67 diseases that students must know how to treat; 158 diseases that students must be able to diagnose; 36 diseases that students should be aware of |
| Birkett et al. (2010) 61 | IUPHAR | To present a model core curriculum for CPT and prescribing for medical students | General prescribing | Evidence based on the opinion of clinical pharmacologists from multiple countries | 63 core knowledge and understanding, 39 core skill, 19 core attitude learning outcomes for CPT and prescribing education |
| Pulcini & Gyssens (2013) 68 | France and the Netherlands | To review the education of prescribers of antibiotics, and analyse and discuss all relevant aspects | Antimicrobial prescribing and resistance | Evidence based on the opinion of 2 infectiologists from 2 countries | 34 learning objectives outcomes for prudent antibiotic prescribing, divided among 10 topics |
| Ross & Loke (2010) 55 | UK; BPS | To create a consensus on the required competencies for new graduates in the area of prescribing | General prescribing | Evidence based on a systematic review and modified two‐round Delphi study involving 21 experts in clinical pharmacology, pharmacy and medical education from multiple institutions in one country | 50 learning outcomes for prescribing education |
| Ross & Maxwell (2012) 62 | UK; BPS | To provide a clear statement of the learning outcomes in clinical pharmacology and prescribing, and to describe a curriculum that might enable medical students to achieve these outcomes | General prescribing | Evidence based on a previous Delphi study and opinion of 2 CPT teachers from 2 institutions in one country | 226 core knowledge and understanding and 58 core skill learning outcomes for teaching clinical pharmacology and prescribing. 98 drug classes and 125 therapeutic problems that students should be familiar with |
| Sice (1975) 57 | USA | To define the basic objectives for pharmacological education for preclinical students, clerks and residents | General prescribing | Evidence based on the opinion of 1 pharmacologist from 1 institution | 6 learning objectives for pharmacological education for preclinical medical students, 7 objectives for clerks and 5 objectives for residents |
| Taylor et al. (2016) 70 | Barbados | To create a summative document containing aims, objectives and methods that can be used for the training of healthcare professionals in ward‐based inpatient diabetes care | Diabetes care | Evidence based on the opinion of 55 final‐year medical students of 1 institution using a four‐stage approach | 13 aims, 29 learning objectives and 21 methods for the inpatient diabetes care |
| Turner & Weiner (2002) 56 | USA | To develop expert‐based guidelines for a medical curriculum on chronic pain evaluation and management in older adults | Pain medicine | Evidence based on a modified two‐round Delphi study involving 12 experts in pain management and medical education of multiple institutions in one country | 8 pain assessment knowledge, 7 pain management knowledge, 12 skills/abilities and 12 attitude items for chronic pain curriculum |
| Walley & Webb (1997) 54 | UK; BPS | To develop a national core curriculum in CPT for medical education | General prescribing | Evidence based on a four‐round Delphi study involving 8 senior clinical pharmacologists from 2 countries | 16 core knowledge and understanding, 14 core skill and 4 core attitude learning outcomes for teaching CPT |
AAPM, American Association of Physicists in Medicine; ACCP, American College of Clinical Pharmacy; BPS, British Pharmacological Society; BSAC, British Society for Antimicrobial Chemotherapy; CMSECPT, Council for Medical Student Education in Clinical Pharmacology and Therapeutics; CPT, clinical pharmacology and therapeutics; EACPT, European Association of Clinical Pharmacology and Therapeutics; FY1, foundation year 1; IPS, Indian Pharmacological Society; IUPHAR, International Union of Basic and Clinical Pharmacology
No reference or description of the Delhi process was provided
Table 2.
Articles (n = 47) evaluating the prescribing competencies of final‐year medical students
| Author | Setting | Study design | Participants | CPT topic | Methods | Main results | Kirkpatrick level c | MERSQI‐score a |
|---|---|---|---|---|---|---|---|---|
| Abbo et al. (2013) 23 | USA; 3 medical schools | Single‐group, cross‐sectional descriptive | 317 final‐year (4th) medical students | Antimicrobial prescribing and resistance | 24‐point self‐administered electronic survey instrument about perceptions, knowledge and attitudes to antimicrobial use and resistance, including 11 clinical vignettes | 92% agreed that knowledge of antimicrobials is important. Mean correct knowledge score was low (51%; max. 100%). Only one‐third perceived their preparedness to be adequate in some fundamental principles of antimicrobial use. 90% wanted more education on appropriate use of antimicrobials | 1, 2b | 12 |
| Abubakar et al. (2015) 30 | Malaysia: one medical school | Multiple groups, cross‐sectional descriptive | 37 penultimate‐(4th) year and 50 final‐year (5th) medical students | Pharmacovigilance | 25‐point self‐administered written questionnaire about knowledge, attitudes and practices regarding ADRs and pharmacovigilance | 78% agreed that ADR reporting is a professional obligation. 59% recognized the right functions of pharmacovigilance. Only 21% knew the method used to report ADRs; 47% had never received any training in how to report ADRs | 1, 2b | 11 |
| Agrawal et al. (2013) 31 | India; one university | Multiple groups, cross‐sectional descriptive | 102 2nd‐year and 98 final‐year (5th) medical and dental students | Contraception | 55‐point self‐administered written questionnaire about knowledge, attitudes, and barriers to practice regarding oral contraceptive pills | Average knowledge score was low (16.7; max. 30); final‐year students had higher knowledge scores compared with 2nd year students. Most students had negative perceptions and attitudes to oral conceptive pills | 2b | 8.5 |
| Al‐Wadaani (2013) 87 | Saudi Arabia; one medical school | Single‐group, cross‐sectional descriptive | 73 final‐year (6th) medical students | Cardiovascular | 22‐point self‐administered written questionnaire about knowledge, attitudes and practices regarding diabetes and diabetic retinopathy | Overall knowledge, attitude and practice scores were moderate (64.8; max. 100). Students lacked knowledge about the follow‐up of diabetic patients for the screening of diabetic retinopathy. 90% of students did not know the proper angle of insulin injection | 2b | 10.5 |
| Awad et al. (2012) 32 | Kuwait; one university | Multiple groups, cross‐sectional descriptive | 54 junior and 68 senior (4th–7th‐year) medical and pharmacy students | Complementary and alternative medicines | Self‐administered written questionnaire about knowledge, perceived effectiveness and barriers to complementary and alternative medicine | Medical students had poor knowledge of complementary and alternative medicine. Over two‐thirds had positive attitudes. Lack of trained professionals and lack of scientific evidence were the most common perceived barriers | 2b | 9 |
| Azeem et al. (2010) 80 | Pakistan; one university hospital | Single‐group, cross‐sectional descriptive | 105 medical graduates | General prescribing | Self‐administered written questionnaire about perceptions regarding preparation and competency to prescribe as junior doctors | 19% considered themselves competent to prescribe at the time of graduation. <35% felt comfortable in providing information about treatment options to patients. The majority (59–95%) indicated a lack of formal teaching and practice at skills relating to drug therapy | 1, 2a | 6.5 |
| Beyhun et al. (2016) 85 | Turkey; one medical school | Single‐group, cross‐sectional descriptive | 148 final‐year (6th) medical students | Narcotics | Self‐administered written questionnaire about awareness of synthetic cannabinoids | Students’ mean awareness score was moderate (4.7; max. 9). Students lacked awareness of usage, illegal status and clinical effects of synthetic cannabinoids | 2b | 8.5 |
| Brinkman et al. (2017) 10 | Europe; 17 medical schools from 15 countries | Single‐group, cross‐sectional descriptive | 895 final‐year (5th–6th) medical students | General prescribing | Online assessment of prescribing knowledge (24 MCQs) and skills (5 patient cases). Self‐administered questionnaire about self‐reported confidence, perceived preparedness for prescribing, and received CPT education | Overall knowledge score was moderate (70%, max. 100%). 46% of the therapies were inappropriate and 55% of the prescriptions contained an error. Students lacked confidence in essential prescribing skills and felt not adequately prepared for prescribing responsibilities. >60% were not satisfied with the quantity and quality of undergraduate CPT education | 1, 2b | 13.5 |
| Brinkman et al. (2014) 27 | The Netherlands; one medical school | Single‐group; cross‐sectional descriptive | 483 final‐year (6th) medical students | General prescribing | Prescribing performance during 4 therapeutic consultations with real patients during clinical clerkship, self‐administered online questionnaire on self‐reported confidence in prescribing | Adequate performance score (7.93; max. 10). Majority (66–88%) lacked self‐reported confidence in essential prescribing skills | 2a, 3 | 9 |
| Cheng & Yu (2012) 33 | China; one medical school | Multiple groups; cross‐sectional descriptive | 103 penultimate‐year (6th) and 80 final‐year (7th) medical students, 59 clinical master degree candidates, 50 clinical doctors | Narcotics | 45‐point self‐administered written questionnaire about knowledge of cancer pain management | Senior medical students had a poor knowledge of cancer pain management, especially among non‐oncological medical students | 2b | 11.5 |
| Chuenchom et al. (2016) 76 | Thailand; three medical schools | Single‐group; cross‐sectional descriptive | 455 final‐year (6th) medical students | Antimicrobial prescribing and resistance | Self‐administered written questionnaire about perception, attitude and knowledge of antimicrobial resistance, appropriate antimicrobial use and infection control | Mean knowledge scores were low (1.61; max. 5). Nearly all participants had a positive attitude about antimicrobial resistance. >10% reported that they had never learned about antimicrobial resistance and appropriate antibiotic use. Nearly all students wanted more education about rational antimicrobial use | 1, 2b | 10 |
| Coombes et al. (2008) 81 | Australia; two teaching hospitals | Single‐group; cross‐sectional descriptive | 101 final‐year (4th) medical students | General prescribing | 21‐point self‐administered written questionnaire about students' perceptions of their readiness to prescribe, associated risks and outcome if involved in an error, as well as their perceptions of available support | 84% felt able to prescribe for simple complaints, whereas only 54% felt comfortable to prescribe warfarin and 66%to prescribe IV fluids. 99% were under the misapprehension that potentially harmful prescriptions would be safely administered. 79% perceived that they would be blamed if they made a prescribing error | 2a | 8.5 |
| Dyar et al. (2013) 35 | France; one medical school | Multiple groups; cross‐sectional descriptive | 34 penultimate‐year (5th) and 26 final‐year (6th) medical students | Antimicrobial prescribing and resistance | 41‐point self‐administered online questionnaire about knowledge, perceptions and beliefs about antibiotic resistance and prescribing | Final‐year students were highly aware of and concerned about the overuse of antibiotics. Areas of non‐confidence and gaps in knowledge were found. Students consistently overestimated the current burden of resistant bacteria and were unaware of success in reducing MRSA infections. 79% wanted more training in antibiotic selection | 1, 2b | 9.5 |
| Dyar et al. (2014) 77 | Europe; seven medical schools from seven countries | Single‐group; cross‐sectional descriptive | 338 final‐year (5th–6th) medical students | Antimicrobial prescribing and resistance | 41‐point self‐administered online questionnaire about knowledge, perceptions and beliefs about antibiotic resistance and prescribing | Students lacked confidence in combination therapy and dose selection of antibiotics. Students consistently overestimated the current burden of resistant bacteria and were unaware of success in reducing MRSA infections. 74% wanted more training in antibiotic selection | 1, 2b | 10.5 |
| Dyasanoor & Urooge (2016) 28 | India; one university hospital | Multiple groups; cross‐sectional descriptive | 52 undergraduates, 221 internsa, 227 postgraduates | General prescribing | Quality of 500 prescriptions dispensed by participants analysed according to 19 parameters | 39% of the prescriptions by interns were not adequate because important parameters were missing. Prescriptions written by undergraduates were better than those written by interns and postgraduates | 3 | 10 |
| Grossman & Sheidler (1985) 25 | USA; one university hospital | Multiple groups; pretest intervention | 4 2nd‐year, 12 penultimate‐year (3rd), 1 final‐year (4th) medical student, 68 house officers | Narcotics | 3 clinical vignettes about converting narcotic analgesic regimen in patients with pain | 2% of the answers of medical students were within the correct range. There were no significant differences between the responses among individuals at different education levels | 2b | 10 |
| Gyawali et al. (2016) 46 | Nepal; one university hospital | Multiple groups; cross‐sectional descriptive | 120 final‐year (5th) medical students, 117 internsa | Generic prescribing and substitution | Self‐administered written questionnaire about knowledge and perceptions of generic medicine and generic prescribing | Only 5% knew the correct regulatory limits for bioequivalence. 46% had the impression that brand‐name medicines were required to meet higher safety standards than were generic medicines. 17% had the impression that generic medicines caused more side effects and were less effective than brand‐name medicines | 2b | 12.5 |
| Haque et al. (2016) 36 | Malaysia; one medical school | Multiple groups; cross‐sectional descriptive | 41 3rd‐year, 55 penultimate‐year (4th) and 45 final‐year (5th) medical students | Antimicrobial prescribing and resistance | 21‐point self‐administered written questionnaire about knowledge, beliefs and practices regarding antibiotic resistance and prescribing | >50% of final‐year students lacked confidence in combination therapy and dose and duration selection of antibiotics. Students consistently overestimated the current burden of resistant bacteria. 88% wanted more training in rational antibiotic selection | 1, 2b | 12.5 |
| Harakeh et al. (2015) 37 | Saudi Arabia; two medical schools | Multiple groups; cross‐sectional descriptive | 1042 1st‐year to final‐year (6th) medical students | Antimicrobial prescribing and resistance | 20‐point self‐administered written questionnaire about knowledge, attitudes and practices regarding the use of antibiotics for upper respiratory tract infections | 93% of the final‐year medical students had adequate knowledge of antibiotic effectiveness. Similarly, most were aware of antibiotic abuse and development of drug resistance in bacteria | 2b | 9.5 |
| Hassali et al. (2007) 51 | Australia; 10 universities | Multiple groups; cross‐sectional descriptive | 400 final‐year (5th) medical students and 289 final‐year (5th) pharmacy pre‐registrants | Generic prescribing and substitution | 20‐point self‐administered online questionnaire about knowledge and perceptions of generic medicine, generic prescribing and generic substitution | Both groups scored poorly on the allowable bioequivalence limits, with pharmacy pre‐registrants scoring better. Both groups incorrectly believed that generic medicines met lower safety standards, were inferior in quality, less effective and produced more side effects than brand‐name medicines | 2b | 11.5 |
| Heaton et al. (2008) 82 | UK; 25 medical schools | Multiple groups; cross‐sectional descriptive | 2413 medical students graduating in 2006–2008 | General prescribing | 17‐point self‐administered online questionnaire about undergraduate training and assessment in pharmacology and therapeutics, the acquisition of prescribing skills and self‐reported confidence in prescribing | Only 38% felt confident about prescription writing and 35% had filled in a hospital prescription chart more than three times during training. 74% felt that there was (far) too little teaching and 56% disagreed that their assessment thoroughly tested knowledge and skills | 1, 2a | 10 |
| Hema et al. (2012) 47 | India; one university hospital | Multiple groups; cross‐sectional descriptive | 80 final‐year (5th) medical students, 88 internsb and 132 postgraduates | Pharmacovigilance | 25‐point self‐administered written questionnaire about awareness, knowledge and methods to apply pharmacovigilance | Compared with interns and postgraduates, final‐year students had a lower awareness score (2.5; max. 5), lower knowledge score (2.3; max. 8) and lower method of application score (5.8; max. 12) | 2b | 10 |
| Holstein et al. (2000) 38 | Germany; 21 academic teaching and university hospitals | Single‐group; cross‐sectional descriptive | 310 final‐year (6th) medical students | Cardiovascular | 20‐point self‐administered written questionnaire about clinically relevant diabetes treatment knowledge and experience | Marked gaps in manual experience and clinically relevant knowledge of diabetes, particularly in practical aspects of diabetes therapy. 45% had never injected insulin and 68% had no experience with the insulin pen. 81% were not satisfied with the diabetes teaching | 1, 2b | 10.5 |
| Hoque et al. (2016) 39 | Bangladesh; one medical school | Multiple groups; cross‐sectional descriptive | 40 3rd‐year, 33 penultimate‐year (4th) and 34 final‐year (5th) medical students | Antimicrobial prescribing and resistance | 21‐point self‐administered written questionnaire about knowledge, attitudes and perceptions about antimicrobial resistance and rational use of antimicrobials | Participants had an average level of confidence in the rational use of antimicrobials, with final‐year students being more confident than earlier‐year students. Students underestimated the prevalence rate of MRSA infection. 94% wanted more training in antibiotic selection | 1, 2b | 11.5 |
| Huang et al. (2013) 40 | China; three teaching hospitals | Multiple groups; cross‐sectional descriptive | 1236 medical students, including 241 final‐year (5th year) students, 852 nonmedical students | Antimicrobial prescribing and resistance | 30‐point self‐administered online questionnaire about knowledge, attitudes and perceptions about antibiotic use | Senior students had more knowledge of and positive attitudes to antibiotic use compared with junior students. No difference between penultimate‐year (4th) and final‐year (5th) students was observed. There was more excessive use of antibiotics among senior medical students | 2b | 12.5 |
| Humphreys et al. (2006) 78 | Ireland; three medical schools | Single‐group; cross‐sectional descriptive | 108 medical graduates | Antimicrobial prescribing and resistance | 19‐point self‐administered written questionnaire about knowledge and understanding of treatment and prevention of common infections | ±60% of the questions were answered correctly; questions regarding the rational use of antibiotics were poorly answered compared with other questions | 2b | 9 |
| Ibia et al. (2005) 24 | USA; 21 medical schools | Multiple groups; cross‐sectional descriptive | 30 penultimate‐year (3th) and 959 final‐year (4th) medical students | Antimicrobial prescribing and resistance | Six paediatric vignettes regarding clinical management of different upper respiratory tract infections | 99% were informed about the problems of antibiotic resistance. Majority of students 30–56%) prescribed antibiotics inappropriately for viral upper respiratory diseases. No subanalysis for done for study year | 2b | 11.5 |
| Iffat et al. (2014) 41 | Pakistan; multiple universities | Multiple groups; cross‐sectional descriptive | 78 3rd‐year, 212 penultimate‐year (4th) and 241 final‐year (5th) dental and medical students | Pharmacovigilance | 31‐point self‐administered written questionnaire about knowledge, attitudes and perceptions about ADR reporting | 88% had knowledge of ADRs. Medical students showed generally positive attitudes to ADR reporting. 55% did not know the definition of pharmacovigilance. Only 10% knew where to report ADRs. 72% indicated that they had not received any training in reporting ADRs | 2b | 12.5 |
| Ismail et al. (2015) 83 | Malaysia; one medical school | Single‐group; cross‐sectional descriptive | 23 final‐year (5th) medical students | Pharmacovigilance | Self‐administered written questionnaire about knowledge, attitudes and practice regarding ADRs and pharmacovigilance | 96% knew the term ADRs. 57% did not know the method for reporting ADRs, although 78% had observed ADRs during clinical clerkships. 87% had not received any training in ADR reporting during their medical training | 1, 2b | 10 |
| Jamshed et al. (2014) 52 | Malaysia; one medical school | Multiple groups; cross‐sectional descriptive | 72 final‐year (5th) medical students and 51 final‐year (5th) pharmacy students | Antimicrobial prescribing and resistance | Self‐administered written questionnaire about understanding of antibiotic use and antibiotic resistance | 94% showed adequate knowledge regarding the course content related to antibiotics. Only 30% were able to recognize penicillin and vancomycin‐resistant bacteria. Pharmacy students had better knowledge than medical students | 2b | 11 |
| Kaki (2011) 86 | Saudi Arabia; one medical school | Single‐group; cross‐sectional descriptive | 325 final‐year (6th) medical students | Narcotics | 18‐point self‐administered written questionnaire about knowledge, beliefs and attitudes to cancer pain management | 46% considered cancer pain as untreatable. 59% considered that the risk of addiction is high with opioid prescriptions. 68% limited opioid prescriptions to patients with poor prognosis. 63% indicated that they had received no education in pain medicine during their medical training | 1, 2b | 12 |
| Khan et al. (2013) 42 | India; one medical school | Multiple groups; cross‐sectional descriptive | 148 3rd‐year medical students and 130 medical graduates | General prescribing | Self‐administered written questionnaire about knowledge, attitudes and behaviour regarding safe prescribing, including one patient case | The knowledge and attitudes of medical graduates were satisfactory. 12% prescribed unnecessary antibiotics. Prescribing skills were generally inadequate as errors in written prescriptions were commonly found | 2b | 10.5 |
| Meher et al. (2015) 43 | India; one medical school | Single‐group; cross‐sectional descriptive | 60 2nd‐year, 60 penultimate‐year (4th), 60 final‐year (5th) medical students | Pharmacovigilance | 21‐point self‐administered written questionnaire about knowledge, attitudes and practice of pharmacovigilance | Mean knowledge and attitude scores for final‐year students were low (4.3; max. 7 and 1.7; max. 4, respectively). Penultimate‐year students had better knowledge and attitude scores than final and 2nd‐year students | 2b | 9.5 |
| Olakunle et al. (2014) 79 | Nigeria; three medical schools | Single‐group; cross‐sectional descriptive | 241 final‐year (6th) medical students | Antimicrobial prescribing and resistance | Self‐administered written questionnaire about knowledge of diagnosis and management of tuberculosis under DOTS | Only 46% correctly mentioned the various categories of the DOTS treatment regimen. 7% were able to identify the correct treatment duration for new tuberculosis | 2b | 10.5 |
| Oshikoya et al. (2008) 21 | Nigeria; one medical school | Single‐group; cross‐sectional descriptive | 34 final‐year (6th) medical students | General prescribing | Self‐administered written questionnaire about knowledge of principles of good prescribing and prescribing skills, including two clinical cases | 92% knew that rational prescribing involved prescribing correct dosage of an appropriate medicine formulation. Less than 50% of the prescriptions included name, case file number, age and gender of the patient | 2b | 10.5 |
| Ozoh et al. (2014) 89 | Nigeria; one medical school | Single‐group; cross‐sectional descriptive | 139 final‐year (6th) medical students | COPD | Self‐administered written questionnaire about knowledge of COPD diagnosis and treatment | 38% had good, 37% fair and 20% poor knowledge of COPD management. 55% were familiar with the GOLD guidelines. 28% correctly identified inhaled steroids and bronchodilators as therapy for stable COPD | 2b | 9.5 |
| Puchner & Zacharisen (2002) 48 | USA; two academic and two teaching hospitals | Multiple groups; cross‐sectional descriptive | 36 medical students (junior/senior), 342 medical specialists | Antimicrobial prescribing and resistance | Self‐administered written questionnaire about cephalosporin prescribing and knowledge of penicillin allergy | There was marked variation between study groups in the prescribing of cephalosporin and requesting penicillin skin testing. In general, medical specialists had a better knowledge of penicillin allergy than medical students | 2b | 8.5 |
| Rehman et al. (2011) 88 | USA; one medical school and four teaching hospitals | Multiple groups; cross‐sectional descriptive | 121 final‐year (4th) year medical students, 354 junior doctors | Cardiovascular | 11‐point self‐administered written questionnaire about knowledge of hypertension diagnosis and management | Only 8% answered the questions regarding hypertension treatment correctly. Mean number of correct answers given by final‐year students was low (5.2; max. 11), although they did better than junior doctors | 2b | 12.5 |
| Rothwell et al. (2012) 29 | UK; three medical schools | Single‐group; cross‐sectional descriptive | 65 medical graduates | General prescribing | Multiple methods, including face‐to‐face and telephone interviews, questionnaires and secondary data from prescribing safety assessment | 73–80% of the graduates felt generally underprepared for prescribing. Only 16–19% of the graduates passed the prescribing safety assessment at the first attempt | 2b | 11 |
| Scaioli et al. (2015) 44 | Italy; one medical school | Multiple groups; cross‐sectional descriptive | 465 1st year, 187 2nd‐year, 190 3rd‐year, 70 4th‐year, 79 penultimate‐year (5th), 59 final‐year (6th) healthcare students | Antimicrobial prescribing and resistance | 31‐point self‐administered written questionnaire about knowledge and attitude about antibiotic usage and antibiotic resistance | More than 90% answered all items correctly. However, 20% were not aware that antimicrobial drugs were not effective against viruses and that these drugs can cause secondary infections. However, no subanalysis by study year was performed | 2b | 11.5 |
| Schutte et al. (2017) 45 | The Netherlands; eight medical schools | Multiple groups; cross‐sectional descriptive | 354 3rd‐year, 92 4th‐year, 106 penultimate‐year (5th), 298 final‐year (6th) medical students | Pharmacovigilance | 10‐point self‐administered online questionnaire about pharmacovigilance awareness, skills and knowledge | Final‐year students had marginally better knowledge scores than 3rd‐year students (68% vs. 64%). Only 48% of the final‐year students felt sufficiently prepared to report ADRs in future practice, and a substantial proportion did not know the authority to which they should report ADRs | 1, 2b | 12.5 |
| Sharrad & Hassali (2011) 84 | Iraq; six medical schools | Single‐group; cross‐sectional descriptive | 546 final‐year (6th) medical students | Generic prescribing and substitution | 23‐point self‐administered written questionnaire about perception and knowledge of generic medicines and generic prescribing | >70% of the respondents did not possess sufficient knowledge about bioequivalence limits for generic medicines. >60% of the students thought that generic medicines were inferior, less effective and produced more side effects than brand‐name medicines | 2b | 13 |
| Thriemer et al. (2013) 49 | Democratic Republic of Congo; one medical school and multiple hospitals | Multiple groups; cross‐sectional descriptive | 106 final‐year (6th) medical students and 78 medical doctors | Antimicrobial prescribing and resistance | 23‐point self‐administered written questionnaire about knowledge, attitudes and practices regarding antibiotic prescribing | Mean knowledge scores were generally low (4.9; max. 9) and did not differ significantly between the groups. Students had high self‐confidence in antibiotic prescribing (86%), although this was lower than that of qualified doctors (95%) | 2b | 12.5 |
| Upadhyaya et al. (2012) 22 | India; one teaching hospital | Single‐group; cross‐sectional descriptive | 50 medical graduates | General prescribing | 22‐point self‐administered written questionnaire about self‐rated knowledge of the principles of good prescribing | 48% rated their prescribing knowledge as average, and 18% as (very) poor. 58% felt that their medical training did not prepare them for rational prescribing. 42% felt that they had some problems with writing a prescription during their internship | 1, 2a | 7 |
| Weber et al. (1986) 50 | Canada; one paediatric hospital | Multiple groups; cross‐sectional descriptive | 28 final‐year (4th) medical students, 21 paediatric residents, 22 paediatricians | General prescribing | Six paediatric patient cases about knowledge of the price of frequently prescribed medications | Students' estimations were adequate in 40% of the cases, which was lower than that of paediatric residents (52%) and paediatricians (62%) | 2b | 8 |
| Weinstein et al. (2000) 34 | USA; one medical school | Multiple groups; cross‐sectional descriptive | 88 1st‐year medical students, 180 final‐year (4th) medical students | Narcotics | 49‐point self‐administered written questionnaire about knowledge and attitudes on pain and the use of opioid analgesics | Senior medical students scored as well as, or better than, 1st‐year students on questions related to knowledge about pain. However, they had a more negative attitude to relieving chronic pain and seemed to have less understanding about the causes of pain in cancer patients | 2b | 10.5 |
| Wheeler et al. (2004) 26 | UK; one medical school | Multiple groups; cross‐sectional descriptive | 87 2nd‐year, 98 penultimate‐year (3rd), 78 final‐year (4th) medical students | General prescribing | Online multiple‐choice examination about dose‐calculating skills | The mean knowledge score for all students was low (1.2; max. 3), although final‐year students had significantly better knowledge scores than 1st‐year students | 2b | 9.5 |
ADR, adverse drug reactions; COPD, chronic obstructive pulmonary disease; CPT, clinical pharmacology and therapeutics; DOTS, directly observed treatment, short‐course; GOLD, Global Initiative for Chronic Obstructive Lung Disease; IV, intravenous; MCQ, multiple choice question; MERSQI, Medical Education Research Quality Instrument; MRSA, methicillin‐resistant Staphylococcus aureus
The MERSQI has a minimum score of 5 and a maximum score of 18.
Interns in India and Malaysia have graduated from medical school but receive their full registration as a medical doctor after completion of the internship
Kirkpatrick's four levels of training evaluation are:
Level 1: Participation – covers learners' views on the learning experience, its organization, presentation, content, teaching methods and aspects of the instructional organization, materials and quality of instruction.
Level 2a: Modification of attitudes or perceptions – outcomes here relate to changes in the reciprocal attitudes or perceptions between participant groups towards intervention or simulation.
Level 2b: Modification of knowledge and skills – for knowledge, this relates to the acquisition of concepts, procedures and principles; for skills, this relates to the acquisition of thinking and problem solving, and psychomotor and social skills.
Level 3: Behavioural change – this documents the transfer of learning to the workplace or the willingness of learners to apply new knowledge and skills.
Level 4a: Change in organizational practice – this relates to wider changes in the organization or delivery of care, attributable to an educational programme.
Level 4b: Benefits to patients or clients – this relates to any improvement in the health or well‐being of patients and clients as a direct result of an educational programme.
Study characteristics
The number of articles evaluating prescribing competencies was found to have increased in the past two decades, from two articles in 2000 to eight in 2016; a similar trend was not seen for articles describing competencies (Figure 2). Of the 25 articles describing competencies, 12 came from Europe, 10 from North America, two from Asia and one from Australia. In terms of CPT topics, most articles (72%) described competencies in general prescribing. The vast majority of articles (96%) were based on expert opinion; only one used a cross‐sectional design.
Figure 2.
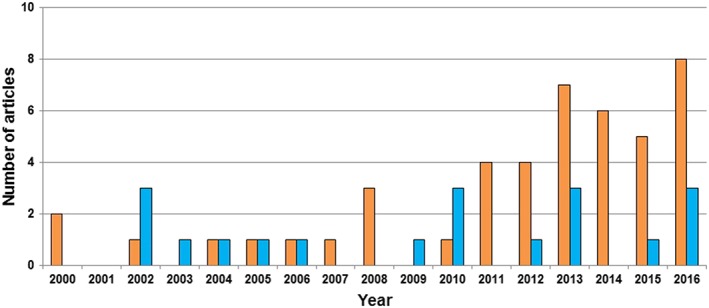
Identified articles describing prescribing competencies ( ) and evaluating prescribing competencies (
) and evaluating prescribing competencies ( ) per year. Articles published before 2000 (n = 8) were not included
) per year. Articles published before 2000 (n = 8) were not included
Of the 47 articles evaluating competencies, 22 were from Asia, 12 from Europe, seven from North America, four from Africa and two from Australia. In terms of CPT topics, most articles (32%) evaluated competencies in antimicrobial prescribing and resistance, and in general prescribing (26%). Most studies (85%) used a cross‐sectional survey as the primary evaluation method; other evaluation methods comprised clinical cases (n = 3) 10, 21, 22, clinical vignettes (n = 3) 23, 24, 25, multiple‐choice exams (n = 2) 10, 26, therapeutic consultations with patients in general practice (n = 1) 27, drug prescriptions during internship (n = 1) 28 and a mixture of quantitative and qualitative methods (n = 1) 29. In total, 10 339 final‐year medical students were involved. The median number of students per study was 104 (range 1–2413). Besides final‐year medical students, some studies also involved 1–5th year students (n = 20) 24, 25, 26, 28, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, junior doctors and residents (n = 8) 25, 28, 33, 46, 47, 48, 49, 50, medical specialists (n = 2) 48, 50, pharmacy students (n = 3) 32, 51, 52, dental students (n = 2) 31, 41 and nonhealthcare students (n = 1) 40.
Study quality
Of the 25 articles describing competencies, four articles (16%) were based on the opinion of experts from one institution, 16 (64%) on the opinion of experts from multiple institutions within one country (four used the Delphi method) and four (16%) on the opinion of experts from multiple countries (one used the Delphi method). Only four Delphi studies described how a consensus among experts was achieved 53, 54, 55, 56.
Of the 47 articles evaluating competencies, 27 (57%) had a single‐institution design, 45 (96%) reported objectively measured outcomes, and 21 (45%) had a response rate <50% or did not report it. Thirty‐two articles (68%) did not discuss the validity and reliability of the evaluation method used. Almost all articles (92%) used appropriate data analysis; however, only 30 (64%) used analytical methods other than descriptive analysis. The total MERSQI scores for the articles ranged from 6.5 to 13.5, with a mean (standard deviation) of 10.5 (1.6). Four (9%) articles measured students' perceptions or attitudes as the primary outcome (Kirkpatrick levels 1 and 2a), 41 (87%) measured students' knowledge or skills (Kirkpatrick level 2b), and two (4%) measured students' behaviour (Kirkpatrick level 3).
Which prescribing competencies should medical students have acquired by the time they graduate?
Regarding general prescribing, Sice was the first to define 13 competencies for undergraduate pharmacological education based on his own experience 57. In 1990, Nierenberg developed a more detailed list of 17 knowledge, 16 skills, and five attitude items relevant for general prescribing, based on a consensus among CPT teachers in the USA 58. Walley and Webb developed an almost identical list of 16 knowledge, 14 skills and four attitude items based on a Delphi study among clinical pharmacologists in the UK and Ireland 59. This Delphi study served as a basis for the 2003 British Pharmacological Society (BPS) core curriculum described by Maxwell and Walley 60, which includes 48 knowledge, 35 skills and 19 attitude items and which was largely taken over in an international paper by Birkett et al. 61. In 2012, Ross and Maxwell updated the BPS curriculum to 226 knowledge and 58 skills items 62, based on another Delphi study among CPT teachers in the UK 55. De Vries 63 and Lum et al. 64 described specific competencies related to the process of rational prescribing. Flockhart et al. 65 and Donnenberg et al. 66 used the principles formulated by Nierenberg to develop learning outcomes for a core CPT curriculum in the USA. More recently, Midlöv et al. defined 40 prescribing competencies based on a Delphi study among physicians in Sweden 53. Competencies mentioned in more than one study are listed in Appendix S3.
Besides general prescribing, Davenport et al. defined 12 competencies for prudent antimicrobial prescribing, based on a consensus between two UK working groups 67. This study served as a basis for the 34 learning outcomes for antimicrobial stewardship defined by Pulcini and Gyssens 68. Turner and Weiner used a Delphi study among pain specialists to develop 39 competencies for a chronic pain curriculum 56. Murinson et al. defined 27 learning objectives for general pain medicine, based on a survey among pain specialists 69. Other areas for which specific prescribing competencies have been described are diabetes care (n = 1) 70, drug misuse (n = 1) 71, psychotherapy (n = 1) 72 and pharmacogenomics (n = 1) 73.
Core drug lists
In 2002, Orme et al. was the first to describe a list of 120 ‘core drugs’ that students should know in detail, and 47 drugs that students should be familiar with but not required to know in any detail 74. Additionally, they provided a list of 67 ‘core diseases’ that students should know how to treat, 158 diseases that students should be able to diagnose and 36 diseases of which students should be aware. One year later, Maxwell and Walley described a more extensive list of 201 core drugs about which students should have an understanding of the mechanism of action, appropriate indications, appropriate routes of administration, and important contraindications and side effects 60. In addition, they reported 148 core diseases for which these drugs should be used. This list was further refined by Ross and Maxwell into 98 drug classes and 125 therapeutic problems that students should be familiar with 62. More recently, Baker et al. developed a validated list of 100 commonly prescribed drugs for use when teaching prescribing, based on a retrospective analysis of prescribing data from primary and secondary care combined with a survey among 148 foundation year 1 doctors 75.
Do final‐year medical students have sufficient prescribing competencies?
Fifteen articles evaluated students' attitudes to, and knowledge of, appropriate antimicrobial prescribing and resistance 23, 24, 35, 36, 37, 39, 40, 44, 48, 49, 52, 76, 77, 78, 79. Students generally had positive attitudes and perceptions about antimicrobial overuse and resistance 35, 49, 76, 77. However, they had poor knowledge of the local prevalence of resistant bacteria 35, 49, 77, 79 and of the treatment and prevention of common infections 24, 49, 78, 79. Additionally, they lacked self‐reported confidence in choosing the correct antibiotic, deciding when to use combination therapy, and choosing the correct dose and interval of administration 35, 36, 77. Only four studies reported a moderate‐to‐high level of knowledge about appropriate antimicrobial use among students 37, 40, 44, 52, and two described a moderate‐to‐high level of self‐reported confidence 39, 49. Most students (74–98%) wanted more training in rational antibiotic selection during medical training 23, 35, 36, 39, 76, 77.
Eleven studies examined students' competencies regarding general prescribing 10, 21, 22, 26, 27, 28, 42, 50, 80, 81, 82. Six studies, including a large study of 2413 UK students and graduates, reported that students felt that there was a lack of learning opportunities related to rational prescribing during their medical training, and that they felt underprepared for their prescribing responsibilities 10, 22, 29, 80, 81, 82. Two studies, including a large multicentre study involving 895 European students, showed that students lacked essential prescribing knowledge and skills for common therapeutic problems 10, 21. One study reported that students' knowledge and attitudes were satisfactory, although their prescribing skills for written patient cases were poor 42. Other studies reported that prescribing skills, such as estimating drug costs 50 and drug calculation skills 26, were deficient. Only two studies investigated students' behaviour in clinical practice. Dyasanoor and Urooge reported that many drug prescriptions written by students during their last internship were erroneous because information about important entries was missing 28. Conversely, Brinkman et al. showed that students were sufficiently skilled in conducting therapeutic consultations with real patients during the final internship of a context‐learning CPT curriculum 27.
Six studies showed that students had a positive attitude to pharmacovigilance but lacked knowledge about where and how to report adverse drug reactions 30, 41, 43, 45, 47, 83. Although many students (27–80%) had encountered an adverse drug reaction during clinical clerkships, very few (1–18%) had reported one 30, 43. Three studies reported that students (72–94%) received no or little training in reporting adverse drug reactions during medical training 30, 41, 83.
Three studies showed that students generally had poor knowledge of, and negative perceptions about, prescribing generic medicines 46, 51, 84. They were generally under the misapprehension that generic medicines were inferior in quality, less effective and produced more side effects than brand‐name medicines 46, 51, 84. They generally lacked knowledge of synthetic cannabinoids 85, cancer pain management 33, 86 and conversion of narcotic analgesic regimens 25, although the latter study included only one final‐year student. Moreover, senior students were more negative about relieving chronic pain and seemed to have less understanding than first‐year students of the causes of pain in cancer patients 34.
Three studies investigated students' knowledge of the treatment of cardiovascular diseases 38, 87, 88. Two studies reported deficiencies in students' knowledge of diabetes mellitus therapy – specifically, diabetic retinopathy and insulin treatment 38, 87. Rehman et al. found that students lacked knowledge of the first‐line treatment of uncomplicated arterial hypertension 88. Awad et al. investigated students' knowledge of, and attitude to, alternative and complementary medicines 32. Although students were positive about complementary and alternative therapies, their self‐reported knowledge was poor. Agrawal et al. reported that while students had good‐to‐excellent knowledge of oral contraceptive pills, they lacked a positive attitude in practice 31. Ozoh et al. found that students' general knowledge of chronic pulmonary obstructive disease treatment was modest, and that they were not familiar with international guidelines on optimal treatment 89.
Discussion
This was the first systematic review to investigate which prescribing competencies are required for safe and effective prescribing, and whether these have been attained by medical students by the time they graduate. We identified 25 studies that described a variety of prescribing competencies covering several CPT topics. The vast majority of these studies (72%) reported competencies regarding general prescribing and were based primarily on the early work of Nierenberg 58 and Walley and Webb 54. Although there seems to be some agreement about specific competencies (e.g. taking drug history, writing prescriptions; Appendix S3), we found no clear consensus among CPT teachers on which prescribing competencies are required before medical students/graduates are allowed to prescribe. A clear definition of competencies is important to steer curricular content – specifically, assessment – and students' approach to learning 90. A lack of agreement on the required competencies of students has also been identified in other areas of medical education – for example, global health 91 and nutritional medicine 92. It was not within the scope of the present review to determine why there is a lack of a consensus. One possibility is that most studies (64%) were focused on the local setting in a specific country – mainly the UK and USA. Authors might have chosen this local approach owing to structural differences in medical education between countries. Another possibility is that competencies were rarely the main focus of the retrieved articles, and thus provided little information on which to draw conclusions. Although studies were mainly based on expert opinion, few described how a consensus between experts was achieved. Additionally, most studies did not describe competencies in detail, which makes it difficult to implement relevant changes in the undergraduate CPT programme. Taken together, there is a need for a greater consensus among CPT teachers on detailed requirements for safe prescribing, to ensure that students are exposed to similar basic levels of training. This is becoming more important, given the increased cross‐border mobility of medical students and junior doctors 93.
Notwithstanding the lack of a consensus on essential competencies, we identified 47 articles reporting a general lack of students' preparedness, self‐confidence, (self‐reported) knowledge and skills, specifically regarding general prescribing, antimicrobial prescribing and pharmacovigilance. These findings are in line with previous literature reviews reporting that medical graduates feel particularly unprepared for prescribing relative to their preparedness for other clinical competencies (e.g. history taking and physical examination) 94, 95. This lack of competence could at least partly explain the relatively high number of prescribing errors made by junior doctors, and is probably due to inadequate CPT education during the undergraduate medical curriculum. Indeed, recent studies have reported that CPT education is still based mainly on traditional learning methods (e.g. lectures and oral exams) 11, and is often not taught and assessed separately because the subject is integrated into broader course designs 62.
What can be done? To improve CPT education in undergraduate European medical curricula, we recently formulated a list of recommendations that could also be useful elsewhere (e.g. the USA) 11. More emphasis should be given to training medical students in clinical practice, preferably as early as possible during medical training, with students being responsible for patient care under the supervision of a senior clinician 96. Moreover, prudent antibiotic prescribing and pharmacovigilance should be given more attention as many studies reported that students felt that there was a lack of training in these two subjects. However, as prescribing errors are caused by multiple factors, changing undergraduate CPT education is only part of the solution, and multifaceted interventions in clinical practice are needed that address the different aspects of the prescribing process 97.
Although our findings are worrying, the results should be interpreted with caution, given the heterogeneity and methodological weaknesses of the included studies. Studies were generally of a single‐institution design and of low‐to‐moderate quality (mean MERSQI score 10.5), and different evaluation methods were used without their validity and reliability being reported. Moreover, as the vast majority of studies (96%) measured ‘soft endpoints’ (Kirkpatrick levels 1 and 2) in a controlled setting, it can be questioned whether the same results would be found in clinical practice. It is unlikely that competence in this context would be better, given the high workload, stress and distractions on hospital wards. Taken together, we conclude that there is considerable evidence that final‐year medical students lack the prescribing competencies required for safe prescribing.
Our review had a number of limitations. First, articles may have been missed, although we attempted to minimize the likelihood of this by searching three databases and using a snowball strategy. Second, one recent important study was not included because the search was terminated before its publication. The latter study describes the delivery of a national prescribing assessment to 7343 UK final‐year medical students in 2016 98. Although there was significant variation in performance between final‐year medical students studying in different UK medical schools, their overall performance was good (95% passed the test). The study shows that the introduction of a valid and reliable national prescribing assessment is a powerful tool to emphasize CPT in the medical curriculum, and to evaluate and improve the essential prescribing competencies of future doctors. More countries should consider implementing a similar national prescribing assessment. Third, the cross‐sectional studies were small and had low response rates. Fourth, a number of potentially relevant studies were excluded because they did not mention students’ year of training. Fifth, the prescribing competencies of students might have been underestimated as a result of publication bias that favoured negative outcomes.
Conclusion
Taking these limitations into consideration, there is considerable evidence that final‐year medical students have insufficient prescribing competencies, which suggests that changes in undergraduate CPT education are required urgently. Moreover, there is a need for a greater consensus among CPT teachers on the competencies that are essential to ensure that medical students prescribe safely and effectively. Steps are being taken to build a European consensus among CPT experts. The Education Working Group of the European Association of Clinical Pharmacology and Therapeutics is conducting a new Delphi study to achieve a consensus on learning outcomes that should be common to all European undergraduate CPT curricula. Future studies should investigate valid and reliable methods for assessing students' prescribing competencies in clinical practice, especially as current studies lack quality and mainly evaluate competencies in a controlled environment. To develop evidence‐based CPT education, further studies of educational interventions with Kirkpatrick's highest level of outcome are needed, preferably with a multicentre design, a large number of participants and a long follow‐up. Student‐run clinics may be useful for this purpose as they offer students early prescribing experience, with real responsibility for patient care under the supervision of a senior clinician 99.
Competing Interests
There are no competing interests to declare. The authors alone are responsible for the content and writing of this article. This study was carried out as part of our routine work. No funds were received.
All authors declare that this work has not been, and will not be, published, in whole or part, in any other journal, and agree to the contents of the manuscript in its submitted form.
Supporting information
Appendix S1 Search strategy performed in PubMed, Excerpta Medica Database (EMBASE) and Education Resources Information Center (ERIC) databases on 10 January 2017
Appendix S2 Best Evidence Medical Education (BEME) Collaboration coding sheet
Appendix S3 General prescribing competencies mentioned by more than one study
Brinkman, D. J. , Tichelaar, J. , Graaf, S. , Otten, R. H. J. , Richir, M. C. , and van Agtmael, M. A. (2018) Do final‐year medical students have sufficient prescribing competencies? A systematic literature review. Br J Clin Pharmacol, 84: 615–635. doi: 10.1111/bcp.13491.
References
- 1. McLellan L, Tully MP, Dornan T. How could undergraduate education prepare new graduates to be safer prescribers? Br J Clin Pharmacol 2012; 74: 605–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Dean B, Schachter M, Vincent C, Barber N. Causes of prescribing errors in hospital inpatients: a prospective study. Lancet 2002; 359: 1373–1378. [DOI] [PubMed] [Google Scholar]
- 3. Leendertse AJ, Egberts AC, Stoker LJ, van den Bemt PM, HARM Study Group . Frequency of and risk factors for preventable medication‐related hospital admissions in the Netherlands. Arch Intern Med 2008; 168: 1890–1896. [DOI] [PubMed] [Google Scholar]
- 4. Ryan C, Ross S, Davey P, Duncan EM, Francis JJ, Fielding S, et al Prevalence and causes of prescribing errors: the PRescribing Outcomes for Trainee Doctors Engaged in Clinical Training (PROTECT) study. PLoS One 2014; 9: e79802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Dornan T, Ashcroft D, Heathfield H, Lewis P, Miles J, Taylor D, et al An in depth investigation into fauses of prescribing errors by foundation trainees in relation to their medical education ‐ EQUIP Study. London: General Medical Council, 2009. Available at http://www.gmc-uk.org/FINAL_Report_prevalence_and_causes_of_prescribing_errors.pdf_28935150.pdf (last accessed 5 December 2017).
- 6. Ashcroft DM, Lewis PJ, Tully MP, Farragher TM, Taylor D, Wass V, et al Prevalence, nature, severity and risk factors for prescribing errors in hospital inpatients: prospective study in 20 UK hospitals. Drug Saf 2015; 38: 833–843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ross S, Ryan C, Duncan EM, Francis JJ, Johnston M, Ker JS, et al Perceived causes of prescribing errors by junior doctors in hospital inpatients: a study from the PROTECT programme. BMJ Qual Saf 2013; 22: 97–102. [DOI] [PubMed] [Google Scholar]
- 8. Lewis PJ, Ashcroft DM, Dornan T, Taylor D, Wass V, Tully MP. Exploring the causes of junior doctors' prescribing mistakes: a qualitative study. Br J Clin Pharmacol 2014; 78: 310–319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lesar TS, Briceland L, Stein DS. Factors related to errors in medication prescribing. JAMA 1997; 277: 312–317. [PubMed] [Google Scholar]
- 10. Brinkman DJ, Tichelaar J, Schutte T, Benemei S, Böttiger Y, Chamontin B, et al Essential competencies in prescribing: a first European cross‐sectional study among 895 final‐year medical students. Clin Pharmacol Ther 2017; 101: 281–289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Brinkman DJ, Tichelaar J, Okorie M, Bissell L, Christiaens T, Likic R, et al Pharmacology and therapeutics education in the European Union needs harmonization and modernization: a cross‐sectional survey among 185 medical schools in 27 countries. Clin Pharmacol Ther 2017; 102: 815–822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ross S, Bond C, Rothnie H, Thomas S, Macleod MJ. What is the scale of prescribing errors committed by junior doctors? A systematic review. Br J Clin Pharmacol 2009; 67: 629–640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lewis PJ, Dornan T, Taylor D, Tully MP, Wass V, Ashcroft DM. Prevalence, incidence and nature of prescribing errors in hospital inpatients: a systematic review. Drug Saf 2009; 32: 379–389. [DOI] [PubMed] [Google Scholar]
- 14. Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group . Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. BMJ 2009; 339: b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wohlin C. Guidelines for snowballing in systematic literature studies and a replication in software engineering [online]. Available at https://dl.acm.org/citation.cfm?id=2601268 (last accessed 26 September 2017).
- 16. Hammick M, Dornan T, Steinert Y. Conducting a best evidence systematic review. Part 1: From idea to data coding. BEME Guide No. 13. Med Teach 2010; 32: 3–15. [DOI] [PubMed] [Google Scholar]
- 17. Steinert Y, Mann K, Centeno A, Dolmans D, Spencer J, Gelula M, et al A systematic review of faculty development initiatives designed to improve teaching effectiveness in medical education: BEME Guide No. 8. Med Teach 2006; 28: 497–526. [DOI] [PubMed] [Google Scholar]
- 18. Freeth D, Hammick M, Koppel I, Reeves S, Barr H. A Critical Review of Evaluations of Interprofessional Education. London: Learning & Teaching Support Network for Health Sciences and Practice, 2002. [Google Scholar]
- 19. Reed DA, Cook DA, Beckman TJ, Levine RB, Kern DE, Wright SM. Association between funding and quality of published medical education research. JAMA 2007; 298: 1002–1009. [DOI] [PubMed] [Google Scholar]
- 20. Lin H, Lin E, Auditore S, Fanning J. A narrative review of high‐quality literature on the effects of resident duty hours reforms. Acad Med 2016; 91: 140–150. [DOI] [PubMed] [Google Scholar]
- 21. Oshikoya KA, Bello JA, Ayorinde EO. Prescribing knowledge and skills of final year medical students in Nigeria. Indian J Pharmacol 2008; 40: 251–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Upadhyaya P, Seth V, Sharma M, Ahmed M, Moghe VV, Khan ZY. Prescribing knowledge in the light of undergraduate clinical pharmacology and therapeutics teaching in India: views of first‐year postgraduate students. Adv Med Educ Pract 2012; 3: 47–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Abbo LM, Cosgrove SE, Pottinger PS, Pereyra M, Sinkowitz‐Cochran R, Srinivasan A, et al Medical students' perceptions and knowledge about antimicrobial stewardship: how are we educating our future prescribers? Clin Infect Dis 2013; 57: 631–638. [DOI] [PubMed] [Google Scholar]
- 24. Ibia E, Sheridan M, Schwartz R. Knowledge of the principles of judicious antibiotic use for upper respiratory infections: a survey of senior medical students. South Med J 2005; 98: 889–895. [DOI] [PubMed] [Google Scholar]
- 25. Grossman SA, Sheidler VR. Skills of medical students and house officers in prescribing narcotic medications. J Med Educ 1985; 60: 552–557. [DOI] [PubMed] [Google Scholar]
- 26. Wheeler DW, Remoundos DD, Whittlestone KD, House TP, Menon DK. Calculation of doses of drugs in solution: are medical students confused by different means of expressing drug concentrations? Drug Saf 2004; 27: 729–734. [DOI] [PubMed] [Google Scholar]
- 27. Brinkman DJ, Tichelaar J, van Agtmael MA, Schotsman R, de Vries TP, Richir MC. The prescribing performance and confidence of final‐year medical students. Clin Pharmacol Ther 2014; 96: 531–533. [DOI] [PubMed] [Google Scholar]
- 28. Dyasanoor S, Urooge A. Insight into quality of prescription writing – an institutional study. J Clin Diagn Res 2016; 10: 61–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Rothwell C, Burford B, Morrison J, Morrow G, Allen M, Davies C, et al Junior doctors prescribing: enhancing their learning in practice. Br J Clin Pharmacol 2012; 73: 194–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Abubakar AR, Simbak NB, Haque M. Pharmacovigilance study: awareness among medical students of a new medical school of Malaysia. Int J Pharm Res 2015; 7: 83–88. [Google Scholar]
- 31. Agrawal PS, Sadadia M, Date S, Trivedi C. Knowledge, attitude and practice of oral contraceptives among undergraduate medical and dental students at SBKS MI & RC, Piparia, Vadodara. Int J Pharm Sci Rev Res 2013; 22: 139–143. [Google Scholar]
- 32. Awad AI, Al‐Ajmi S, Waheedi MA. Knowledge, perceptions and attitudes toward complementary and alternative therapies among Kuwaiti medical and pharmacy students. Med Princ Pract 2012; 21: 350–354. [DOI] [PubMed] [Google Scholar]
- 33. Cheng Y, Yu S. A survey of advanced medical students' knowledge towards cancer pain management. Chin‐Ger J Clin Oncol 2012; 11: 533–538. [Google Scholar]
- 34. Weinstein SM, Laux LF, Thornby JI, Lorimor RJ, Hill CS Jr, Thorpe DM, et al Medical students' attitudes toward pain and the use of opioid analgesics: implications for changing medical school curriculum. South Med J 2000; 93: 472–478. [PubMed] [Google Scholar]
- 35. Dyar OJ, Howard P, Nathwani D, Pulcini C. Knowledge, attitudes, and beliefs of French medical students about antibiotic prescribing and resistance. Med Mal Infect 2013; 43: 423–430. [DOI] [PubMed] [Google Scholar]
- 36. Haque M, Rahman NIA, Zulkifli Z, Ismail S. Antibiotic prescribing and resistance: knowledge level of medical students of clinical years of university Sultan Zainal Abidin, Malaysia. Ther Clin Risk Manag 2016; 12: 413–426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Harakeh S, Almatrafi M, Ungapen H, Hammad R, Olayan F, Hakim R, et al Perceptions of medical students towards antibiotic prescribing for upper respiratory tract infections in Saudi Arabia. BMJ Open Respir Res 2015; 2: e000078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Holstein A, Widjaja A, Nahrwold D, Egberts EH. Clinically relevant diabetes knowledge and experience amongst final year medical students. Pract Diabetes Int 2000; 17: 3–8. [Google Scholar]
- 39. Hoque R, Mostafa A, Haque M. Insight of medical students of clinical years to antimicrobials prescribing and resistance in private medical school, Chittagong, Bangladesh. J Young Pharm 2016; 8: 447–455. [Google Scholar]
- 40. Huang Y, Gu J, Zhang M, Ren Z, Yang W, Chen Y, et al Knowledge, attitude and practice of antibiotics: a questionnaire study among 2500 Chinese students. BMC Med Educ 2013; 13: 163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Iffat W, Shakeel S, Naseem S, Imam S, Khan M. Attitudinal survey to assess medical and dental students' belief of ADR reporting in Pakistan. Int J Pharm Sci 2014; 6: 279–283. [Google Scholar]
- 42. Khan AKA, Rashed MR, Muneersha TKM, Rahiman OMF. Assessment of the prescribing knowledge, attitude and skills of medical students and interns in a large teaching hospital of southern India. Biomed Pharmacol J 2013; 6: 63–69. [Google Scholar]
- 43. Meher BR, Joshua N, Asha B, Mukherji D. A questionnaire based study to assess knowledge, attitude and practice of pharmacovigilance among undergraduate medical students in a tertiary care teaching hospital of South India. Perspect Clin Res 2015; 6: 217–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Scaioli G, Gualano MR, Gili R, Masucci S, Bert F, Siliquini R. Antibiotic use: a cross‐sectional survey assessing the knowledge, attitudes and practices amongst students of a school of medicine in Italy. PLoS One 2015; 10: e0122476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Schutte T, Tichelaar J, Reumerman MO, van Eekeren R, Rissmann R, Kramers C, et al Pharmacovigilance skills, knowledge and attitudes in our future doctors – A nationwide study in the Netherlands. Basic Clin Pharmacol Toxicol 2017; 120: 475–481. [DOI] [PubMed] [Google Scholar]
- 46. Gyawali S, Hassali MA, Saha A. A survey exploring the knowledge and perceptions of senior medical students in Nepal toward generic medicines. SAGE Open Med 2016; 4: 2050312116662570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Hema NG, Bhuvana KB, Sangeetha K. Pharmacovigilance: the extent of awareness among the final year students, interns and postgraduates in a government teaching hospital. J Clin Diagn Res 2012; 6: 1248–1253. [Google Scholar]
- 48. Puchner TC Jr, Zacharisen MC. A survey of antibiotic prescribing and knowledge of penicillin allergy. Ann Allergy Asthma Immunol 2002; 88: 24–29. [DOI] [PubMed] [Google Scholar]
- 49. Thriemer K, Katuala Y, Batoko B, Alworonga JP, Devlieger H, Van Geet C, et al Antibiotic prescribing in DR Congo: a knowledge, attitude and practice survey among medical doctors and students. PLoS One 2013; 8: e55495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Weber ML, Auger C, Cleroux R. Knowledge of medical students, pediatric residents, and pediatricians about the cost of some medications. Pediatr Pharmacol 1986; 5: 281–285. [PubMed] [Google Scholar]
- 51. Hassali MA, Kong DCM, Stewart K. A comparison between senior medical students' and pharmacy pre‐registrants' knowledge and perceptions of generic medicines. Med Educ 2007; 41: 703–710. [DOI] [PubMed] [Google Scholar]
- 52. Jamshed SQ, Elkalmi R, Rajiah K, Al‐Shami AK, Shamsudin SH, Siddiqui MJA, et al Understanding of antibiotic use and resistance among final‐year pharmacy and medical students: a pilot study. J Infect Dev Ctries 2014; 8: 780–785. [DOI] [PubMed] [Google Scholar]
- 53. Midlöv P, Höglund P, Eriksson T, Diehl A, Edgren G. Developing a competency‐based curriculum in basic and clinical pharmacology – a Delphi study among physicians. Basic Clin Pharmacol Toxicol 2015; 117: 413–420. [DOI] [PubMed] [Google Scholar]
- 54. Walley T, Webb DJ. Developing a core curriculum in clinical pharmacology and therapeutics: a Delphi study. Br J Clin Pharmacol 1997; 44: 167–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Ross S, Loke YK. Development of learning outcomes for an undergraduate prescribing curriculum (British Pharmacological Society prescribing initiative). Br J Clin Pharmacol 2010; 70: 604–608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Turner GH, Weiner DK. Essential components of a medical student curriculum on chronic pain management in older adults: results of a modified Delphi process. Pain Med 2002; 3: 240–252. [DOI] [PubMed] [Google Scholar]
- 57. Sice J. Objectives of pharmacological education. J Med Educ 1975; 50: 773–778. [PubMed] [Google Scholar]
- 58. Nierenberg DW. A core curriculum for medical students in clinical pharmacology and therapeutics. The Council for Medical Student Education in Clinical Pharmacology and Therapeutics. Clin Pharmacol Ther 1990; 48: 606–610. [DOI] [PubMed] [Google Scholar]
- 59. Walley T, Webb DJ. Core content of a course in clinical pharmacology. Br J Clin Pharmacol 1997; 44: 171–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Maxwell S, Walley T. Teaching safe and effective prescribing in UK medical schools: a core curriculum for tomorrow's doctors. Br J Clin Pharmacol 2003; 55: 496–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Birkett D, Brosen K, Cascorbi I, Gustafsson LL, Maxwell S, Rago L, et al Clinical pharmacology in research, teaching and health care: Considerations by IUPHAR, the International Union of Basic and Clinical Pharmacology. Basic Clin Pharmacol Toxicol 2010; 107: 531–559. [DOI] [PubMed] [Google Scholar]
- 62. Ross S, Maxwell S. Prescribing and the core curriculum for tomorrow's doctors: BPS curriculum in clinical pharmacology and prescribing for medical students. Br J Clin Pharmacol 2012; 74: 644–661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. de Vries TP. Presenting clinical pharmacology and therapeutics: a problem based approach for choosing and prescribing drugs. Br J Clin Pharmacol 1993; 35: 581–586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Lum E, Mitchell C, Coombes I. The competent prescriber: 12 core competencies for safe prescribing. Aust Prescr 2013; 36: 13–16. [Google Scholar]
- 65. Flockhart DA, Yasuda SU, Pezzullo JC, Knollmann BC. Teaching rational prescribing: a new clinical pharmacology curriculum for medical schools. Naunyn Schmiedebergs Arch Pharmacol 2002; 366: 33–43. [DOI] [PubMed] [Google Scholar]
- 66. Donnenberg VS, Burris JF, Wiernik PH, Cohen LJ, Korth‐Bradley JM. How to fix the dangerous lack of clinical pharmacology education in the medical profession: the generation of core entrustable professional activities in clinical pharmacology for entering residency. J Clin Pharmacol 2016; 56: 1177–1179. [DOI] [PubMed] [Google Scholar]
- 67. Davenport LAP, Davey PG, Ker JS, BSAC Undergraduate Education Working Party . An outcome‐based approach for teaching prudent antimicrobial prescribing to undergraduate medical students: report of a Working Party of the British Society for Antimicrobial Chemotherapy. J Antimicrob Chemother 2005; 56: 196–203. [DOI] [PubMed] [Google Scholar]
- 68. Pulcini C, Gyssens IC. How to educate prescribers in antimicrobial stewardship practices. Virulence 2013; 4: 192–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Murinson BB, Gordin V, Flynn S, Driver LC, Gallagher RM, Grabois M. Recommendations for a new curriculum in pain medicine for medical students: toward a career distinguished by competence and compassion. Pain Med 2013; 14: 345–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Taylor CG Jr, Atherley A, Murphy MM. Towards an inpatient diabetes curriculum: medical student‐generated aims, objectives and methods for ward‐based learning of non‐critical, non‐perioperative inpatient diabetes care. Diabet Med 2016; 33: 827–834. [DOI] [PubMed] [Google Scholar]
- 71. Antman KH, Berman HA, Flotte TR, Flier J, Dimitri DM, Bharel M. Developing core competencies for the prevention and management of prescription drug misuse: a medical education collaboration in Massachusetts. Acad Med 2016; 91: 1348–1351. [DOI] [PubMed] [Google Scholar]
- 72. Borgeat F, Gagnon J, Hudon M, Lalonde P, Reid W. Teaching therapeutic skills of a psychological nature to future physicians. Can J Psychiatry 1985; 30: 445–449. [DOI] [PubMed] [Google Scholar]
- 73. O'Brien TJ, Goodsaid F, Plack M, Harralson A, Harrouk W, Hales TG, et al Development of an undergraduate pharmacogenomics curriculum. Pharmacogenomics 2009; 10: 1979–1986. [DOI] [PubMed] [Google Scholar]
- 74. Orme M, Frolich J, Vrhovac B. Towards a core curriculum in clinical pharmacology for undergraduate medical students in Europe. Eur J Clin Pharmacol 2002; 58: 635–640. [DOI] [PubMed] [Google Scholar]
- 75. Baker E, Roberts AP, Wilde K, Walton H, Suri S, Rull G, et al Development of a core drug list towards improving prescribing education and reducing errors in the UK. Br J Clin Pharmacol 2011; 71: 190–198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Chuenchom N, Thamlikitkul V, Chaiwarith R, Deoisares R, Rattanaumpawan P. Perception, attitude, and knowledge regarding antimicrobial resistance, appropriate antimicrobial use, and infection control among future medical practitioners: a multicenter study. Infect Control Hosp Epidemiol 2016; 37: 603–605. [DOI] [PubMed] [Google Scholar]
- 77. Dyar OJ, Pulcini C, Howard P, Nathwani D, Beovic B, Harbarth S, et al European medical students: a first multicentre study of knowledge, attitudes and perceptions of antibiotic prescribing and antibiotic resistance. J Antimicrob Chemother 2014; 69: 842–846. [DOI] [PubMed] [Google Scholar]
- 78. Humphreys H, Dillane T, O'Connell B, Luke LC. Survey of recent medical graduates' knowledge and understanding of the treatment and prevention of infection. Ir Med J 2006; 99: 58–59. [PubMed] [Google Scholar]
- 79. Olakunle OS, Oladimeji O, Olalekan AW, Olugbenga‐Bello A, Akinleye C, Oluwatoyin OA. Knowledge of tuberculosis management using directly observed treatment short course therapy among final year medical students in South Western Nigeria. Pan Afr Med J 2014; 18: 32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Azeem M, Bhutta AR, Bashir A, Pervez A, Samee U, Raza A. Are King Edward Medical University graduates adequately trained to prescribe medicine at the point of graduation? Views of house officers. Pak J Med Sci 2010; 4: 210–214. [Google Scholar]
- 81. Coombes ID, Mitchell CA, Stowasser DA. Safe medication practice: attitudes of medical students about to begin their intern year. Med Educ 2008; 42: 427–431. [DOI] [PubMed] [Google Scholar]
- 82. Heaton A, Webb DJ, Maxwell SRJ. Undergraduate preparation for prescribing: the views of 2413 UK medical students and recent graduates. Br J Clin Pharmacol 2008; 66: 128–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Ismail SB, Rahman NIA, Anantrao NH, Dali WPEW, Umar BU, Haque M. Awareness of pharmacovigilance among future house officers; a study among first batch of final year medical students of UniSZA, Malaysia. Int J Pharm Res 2015; 7: 96–101. [Google Scholar]
- 84. Sharrad AK, Hassali MA. Knowledge and perceptions of final year medical students in Iraqi universities about generic medicines. J Bioequiv Availab 2011; 3: 86–91. [Google Scholar]
- 85. Beyhun NE, Can G, Topbas M, Cankaya S, Ketenci HC. Are the last grade medical students aware of the danger of synthetic cannabinoids? J Forensic Leg Med 2016; 38: 1–5. [DOI] [PubMed] [Google Scholar]
- 86. Kaki AM. Medical students' knowledge and attitude toward cancer pain management in Saudi Arabia. Saudi Med J 2011; 32: 628–632. [PubMed] [Google Scholar]
- 87. Al‐Wadaani FA. The knowledge attitude and practice regarding diabetes and diabetic retinopathy among the final year medical students of King Faisal University Medical College of Al Hasa region of Saudi Arabia: a cross sectional survey. Niger J Clin Pract 2013; 16: 164–168. [DOI] [PubMed] [Google Scholar]
- 88. Rehman A, Rehman T, Shaikh MA, Naqvi SA. Awareness of hypertension among the medical students and junior doctors – a multicenter study from Pakistan. J Pak Med Assoc 2011; 61: 1153–1157. [PubMed] [Google Scholar]
- 89. Ozoh OB, Awokola T, Buist SA. Medical students' knowledge about the management of chronic obstructive pulmonary disease in Nigeria. Int J Tuberc Lung Dis 2014; 18: 117–121. [DOI] [PubMed] [Google Scholar]
- 90. Harden RM, Crosby JR, Davis MH, Friedman M. AMEE Guide No. 14: Outcome‐based education: Part 5 – From competency to meta‐competency: a model for the specification of learning outcomes. Med Teach 1999; 21: 546–552. [DOI] [PubMed] [Google Scholar]
- 91. Battat R, Seidman G, Chadi N, Chanda MY, Nehme J, Hulme J, et al Global health competencies and approaches in medical education: a literature review. BMC Med Educ 2010; 10: 94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Adams KM, Kohlmeier M, Powell M, Zeisel SH. Nutrition in medicine: nutrition education for medical students and residents. Nutr Clin Pract 2010; 25: 471–480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Costigliola V. Mobility of medical doctors in cross‐border healthcare. EPMA J 2011; 2: 333–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Monrouxe LV, Grundy L, Mann M, John Z, Panagoulas E, Bullock A, et al How prepared are UK medical graduates for practice? A rapid review of the literature 2009‐2014. BMJ Open 2017; 7: e013656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Alexander C, Millar J, Szmidt N, Hanlon K, Cleland J. Can new doctors be prepared for practice? A review. Clin Teach 2014; 11: 188–192. [DOI] [PubMed] [Google Scholar]
- 96. Tichelaar J, van Kan C, van Unen RJ, Schneider AJ, van Agtmael MA, de Vries TP, et al The effect of different levels of realism of context learning on the prescribing competencies of medical students during the clinical clerkship in internal medicine: an exploratory study. Eur J Clin Pharmacol 2015; 71: 237–242. [DOI] [PubMed] [Google Scholar]
- 97. Tully MP, Ashcroft DM, Dornan T, Lewis PJ, Taylor D, Wass V. The causes of and factors associated with prescribing errors in hospital inpatients: a systematic review. Drug Saf 2009; 32: 819–836. [DOI] [PubMed] [Google Scholar]
- 98. Maxwell SR, Coleman JJ, Bollington L, Taylor C, Webb DJ. Prescribing Safety Assessment 2016: delivery of a national prescribing assessment to 7343 UK final‐year medical students. Br J Clin Pharmacol 2017; 83: 2249–2258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Dekker RS, Schutte T, Tichelaar J, Thijs A, van Agtmael MA, de Vries TP, et al A novel approach to teaching pharmacotherapeutics – feasibility of the learner‐centered student‐run clinic. Eur J Clin Pharmacol 2015; 71: 1381–1387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Banna NR, Boyd EJS, Harron DWG. Pharmacology teaching: developing an integrated core curriculum in pharmacology and therapeutics. Int Pharm J 1994; 8: 63–67. [Google Scholar]
- 101. Gitanjali B, Shashindran CH. Curriculum in clinical pharmacology for medical undergraduates of India. Indian J Pharmacol 2006; 38: S108–SS14. [Google Scholar]
- 102. Mathur VS. Towards a more meaningful teaching of pharmacology. Indian J Pharmacol 2004; 36: 259–261. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1 Search strategy performed in PubMed, Excerpta Medica Database (EMBASE) and Education Resources Information Center (ERIC) databases on 10 January 2017
Appendix S2 Best Evidence Medical Education (BEME) Collaboration coding sheet
Appendix S3 General prescribing competencies mentioned by more than one study


