Abstract
Objective
To test the impact of the dependent coverage expansion (DCE) on insurance disparities across race/ethnic groups.
Data Sources/Study Setting
Survey data from the National Survey of Drug Use and Health (NSDUH).
Study Design
Triple‐difference (DDD) models were applied to repeated cross‐sectional surveys of the U.S. adult population.
Data Collection/Extraction Methods
Data from 6 years (2008–2013) of the NSDUH were combined.
Principal Findings
Following the DCE, the relative odds of insurance increased 1.5 times (95 percent CI 1.1, 1.9) among whites compared to blacks and 1.4 times (95 percent CI 1.1, 1.8) among whites compared to Hispanics.
Conclusions
Health reform efforts, such as the DCE, can have negative effects on race/ethnic disparities, despite positive impacts in the general population.
Keywords: Health insurance coverage, health disparities, young adults
Improving access to care across the general population and reducing disparities in access to care across race and ethnic groups are complementary goals of public health policy (Williams and Jackson 2005; Koh, Graham, and Glied 2011). However, policies that aim to improve access to care may not affect these two goals in the same way (Mechanic 2002; Benach et al. 2011; Cerdá et al. 2014). In particular, researchers have raised the concern that preexisting social inequality could constrain benefits of some policies to relatively advantaged groups so that positive public health impacts are achieved at the same time as race and ethnic disparities are deepened (Phelan and Link 2005; Frohlich and Potvin 2008; Phelan, Link, and Tehranifar 2010). One potential example of this phenomenon is the dependent coverage expansion (DCE), which took effect in September 2010 as part of the Patient Protection and Affordable Care Act (ACA) and remains one of its most popular provisions (Blumenthal and Collins 2014). The DCE aimed to improve access to health insurance coverage for young adults, the age group with lowest prevalence of health insurance coverage (Collins, Garber, and Robertson 2011), by requiring private insurance policies that cover dependents to extend dependent coverage through age 25. Since the DCE only benefits individuals with privately insured parents or guardians, the potential divergence in its impact on population‐wide levels of coverage, on the one hand, and disparities in coverage, on the other, is a concern. Understanding the impact of the DCE on disparities in coverage is important for understanding the equity impact of health insurance reform.
Studies examining the impact of the DCE in the general population have consistently found that the policy increased insurance coverage among young adults (Wallace and Sommers 2015). However, evidence regarding differential effects across race and ethnic groups is mixed. Some studies have found no evidence of differential impact, suggesting that the gains in insurance coverage were evenly distributed across groups (Sommers et al. 2013; Kotagal et al. 2014; Shane and Ayyagari 2014). Other studies have found that the positive effect of the DCE on insurance coverage was greater among whites than among blacks and Hispanics (Akosa Antwi, Moriya, and Simon 2013; O'Hara and Brault 2013), a result which implies an increase in coverage disparities. Differences across these early studies may have been influenced by the early impacts of the DCE; all of the above studies used data through the end of 2011. A study using data through 2012 suggested that impacts of the DCE on insurance coverage among blacks and Hispanics may have been larger in that year compared with 2011 (Shane, Ayyagari, and Wehby 2016). Studies using data on a longer period following implementation of the DCE provide stronger evidence of differential impact. For instance, a study of insurance coverage among users of emergency rooms, which used data through 2012 from the National Trauma Data Bank, found that the DCE reduced the rate of uninsurance among patients by 17 percent for whites, 6 percent for blacks, and 4 percent for Hispanics (Scott et al. 2015a,b). One study using data through 2013 reported no heterogeneity in the effect of the DCE across race/ethnic groups (Barbaresco, Courtemanche, and Qi 2015), but no studies have examined the impact on disparities in coverage in detail. In this report, we directly test the impact of the DCE on disparities in insurance coverage among blacks and Hispanics relative to whites starting in the third quarter of 2010, when the ACA's DCE took effect, and continuing through the end of 2013, just before implementation of the ACA's Medicaid expansions and insurance exchanges.
Methods
Sample
Data come from the National Survey of Drug Use and Health (NSDUH), an annual cross‐sectional survey conducted by the Substance Abuse and Mental Health Services Administration. The NSDUH sample is designed to be representative of the non‐Active Duty Military general population of the United States at the state level. Study procedures were approved by the RAND Human Subject Protection Committee.
Race/Ethnicity
Respondents self‐identified their race/ethnic identity as Hispanic or non‐Hispanic and white, black, Asian, Native American, or Other. Results are shown for comparisons on Non‐Hispanic whites (whites) with non‐Hispanic blacks (blacks), and Hispanics.
Outcome
Health insurance status is assessed by self‐report. The respondent or a proxy household member was asked whether they currently were covered by each of the following insurance types: Medicare, Medicaid/CHIP, Tricare/Champus/ChampVA/VA/Other Military, private insurance, or other insurance. Respondents were classified as having any insurance versus no insurance and those with any insurance classified as having private or public insurance. The primary outcome examined here is “any versus no insurance,” based on methodological research showing that respondents are more accurate in reporting any versus no coverage than in reporting specific types of coverage (Nelson et al. 2000; Call et al. 2013), particularly for public insurance (Hill 2007). Secondary analyses were conducted examining private and public insurance coverages.
Additional Covariates
Statistical adjustment is recommended in the literature to adjust for differences in group composition across time periods (Ryan, Burgess, and Dimick 2015). Models were specified with and without statistical controls for sex, educational attainment, income, and marital status.
Statistical Analysis
The impact of the DCE on disparities in insurance coverage was estimated using a triple‐difference (DDD) model, an extension of the difference‐in‐difference (DD) model frequently used in policy evaluation (Howell, Conway, and Rajkumar 2015). The DD model compares change over time in an intervention group with change over the same period of time in a control group unaffected by the policy in question. Change in the intervention group net of change in the control group is interpreted as an effect of the intervention. The DDD model extends the DD model to address the impact of the intervention on differences across subgroups, where the effect for each subgroup is estimated with a DD model. In this study, the DDD model is used to test whether the DCE affected the difference in insurance coverage between whites and blacks or Hispanics.
We applied a set of DDD analysis for the repeated cross‐sectional data from the NSDUH between the two age groups (19–25 and 26–34) using data from 2008 to 2013. In the equation below, let A, D, and R be binary indicators for age groups (A = 1 for 19–25 years old), time periods affected by DCE (D = 1 for the third quarter of 2010 and later periods), and race/ethnicity group (R = 1 for non‐Hispanic white and 0 for a reference minority group). The DDD approach was implemented by generalized linear models (GLM) taking the following form:
where E(Y it) is the mean of the outcome Y it (e.g., any insurance coverage), g() is a link function in GLM, X it γ is the effect of individual‐level coavariates (i.e., gender, education, marital status, and income), and is the fixed effect for time (quarter years, with most recent quarter omitted). The remaining seven terms model the covariate‐adjusted differences among the four subpopulations defined by age group and race/ethnicity. Specifically, the pre‐DCE differences between the two age groups are and + for the minority subpopulation and non‐Hispanic white subpopulation, respectively. The pre‐DCE difference among 26–34 years old between non‐Hispanic white and minority is represented by . The differences between pre‐ and post‐DCE periods are for minority aged 26–34 years old, for minority aged 19–25 years old, for non‐Hispanic white aged 26–34 years old, and for non‐Hispanic white aged 19–25 years old, respectively. The DD effect of the DCE is for the minority subpopulation and for non‐Hispanic white. The DDD effect for differential DCE effects between the two race/ethnicity groups is therefore the three‐way interaction , which is the main parameter of interest for inference. Models were estimated using logistic and identity links, with and without individual‐level covariates X it γ. All models were fitted in SAS 9.4 using survey adjusted procedures (PROC SURVEYREG and PROC SURVEYLOGISTIC) to adjust for the informative survey designs in NSDUH.
Results
The sample includes a total of 118,110 respondents, 87,802 in the 19‐ to 25‐year‐old age group and 30.308 in the 26‐ to 34‐year‐old age group (Table 1). With respect to marital status, educational attainment and income, both blacks and Hispanics differ from whites before and after the DCE for both age groups. There is variation in the level of significance of differences in the sex composition of the groups, but the magnitude of the differences is small and the relative order of the proportions of male respondents is the same for all groups.
Table 1.
Sample Characteristics, National Survey of Drug Use and Health, 2008–2013, Ages 19–25 and Ages 26–24
| Characteristics | Age 19–25 | Age 26–34 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre‐DCE | Post‐DCE | Pre‐DCE | Post‐DCE | |||||||||
| White | Black† | Hispanic† | White | Black† | Hispanic† | White | Black† | Hispanic† | White | Black† | Hispanic† | |
| Sample size | 24,174 | 5,362 | 7,172 | 33,070 | 7,826 | 10,198 | 8,308 | 1,736 | 2,672 | 11,632 | 2,375 | 3,585 |
| Sex | ||||||||||||
| Male | 50.7 | 45.4*** | 51.9 | 49.7 | 47.3* | 52.2** | 49.5 | 45.8* | 55.0** | 49.7 | 45.2 | 51.9 |
| Marital status | ||||||||||||
| Married | 14.3 | 5.5*** | 17.8*** | 12.8 | 5.3*** | 14.2* | 53.3 | 28.9*** | 49.5** | 49.5 | 25.7*** | 46.7* |
| Widowed | 0.1 | 0.1 | 0.0 | 0.1 | 0.1 | 0.1 | 0.4 | 0.1 | 0.2 | 0.4 | 0.4 | 0.3 |
| Divorced or separated | 2.2 | 1.2 | 2.6 | 1.9 | 1.1 | 2.1 | 9.8 | 10.1 | 8.7 | 9.5 | 8.9 | 8.3 |
| Never been married | 83.5 | 93.3 | 79.6 | 85.2 | 93.5 | 83.5 | 36.5 | 60.8 | 41.5 | 40.6 | 65.0 | 44.7 |
| Education | ||||||||||||
| In school | 42.8 | 42.4*** | 32.5*** | 43.9 | 43.1*** | 38.3*** | 12.4 | 17.8*** | 8.8*** | 12.7 | 18.5*** | 9.9*** |
| Less than high school | 8.6 | 12.2 | 23.2 | 7.7 | 10.4 | 17.6 | 7.3 | 12.2 | 31.6 | 8.4 | 12.8 | 28.0 |
| High school graduate | 23.4 | 29.3 | 28.6 | 23.0 | 28.7 | 28.1 | 24.6 | 28.1 | 29.5 | 22.5 | 28.1 | 27.4 |
| Some college | 12.5 | 10.1 | 11.8 | 12.3 | 12.8 | 11.0 | 21.7 | 25.2 | 17.5 | 21.6 | 22.5 | 18.3 |
| College graduate | 12.8 | 6.0 | 3.9 | 13.1 | 5.0 | 4.9 | 33.9 | 16.7 | 12.5 | 34.8 | 18.1 | 16.3 |
| Income | ||||||||||||
| Less than $20,000 | 29.1 | 41.3*** | 28.5*** | 30.6 | 43.0*** | 30.6*** | 11.5 | 27.5*** | 23.0*** | 13.1 | 30.0*** | 25.7*** |
| $20,000–$49,999 | 33.0 | 36.3 | 42.7 | 31.3 | 35.6 | 41.9 | 33.4 | 39.8 | 47.3 | 33.6 | 39.5 | 42.6 |
| $50,000 – $74,999 | 15.3 | 10.8 | 12.9 | 14.5 | 10.1 | 13.3 | 22.6 | 15.9 | 13.4 | 20.8 | 14.8 | 14.7 |
| $75,000 or more | 22.5 | 11.6 | 16.0 | 23.6 | 11.2 | 14.2 | 32.5 | 16.8 | 16.3 | 32.4 | 15.6 | 17.0 |
Significance levels were marked as ***<.001, **<.01, *<.05.
†Rates were compared with whites of the same age group and during the same period.
Time trends in insurance coverage for 19‐ to 25‐year‐olds, the age group targeted by the DCE, and 26‐ to 34‐year‐olds, the control group, are shown in Figure 1 for blacks, Hispanics, and whites. For all three groups, the proportion with any insurance is lower among 19‐ to 25‐year‐olds than among 26‐ to 34‐year‐olds for the entire pre‐DCE period, which ended close to the end of 2010. After that point in time, the differences between the age groups narrow, and, among whites but not blacks or Hispanics, the age‐group difference reverses, with the younger group reaching higher levels of coverage than the older group.
Figure 1.
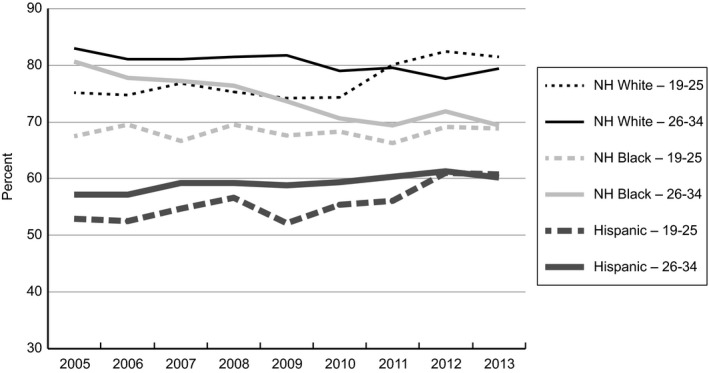
Age Group Trends in Insurance Coverage by Race/Ethnic Group, 2005–2013
Results from the DDD analysis of the impact of the DCE on disparities in insurance coverage between whites and blacks and between whites and Hispanics are presented in Table 2. Estimates from two logistic regression models for each comparison are shown, one with no adjustment for covariates and one with statistical adjustment for sex, marital status, income, and education.
Table 2.
DDD Estimates of the Impact of the DCE on Race/Ethnic Disparities in Health Insurance Coverage, NSDUH 2008–2013
| Contrast | Unadjusted | Adjusted† | ||||||
|---|---|---|---|---|---|---|---|---|
| Estimate | Lower Limit | Upper Limit | p‐Value | Estimate | Lower Limit | Upper Limit | p‐Value | |
| White–black comparison | ||||||||
| Difference prior to DCE, age 19–25 | 1.4 | 1.2 | 1.5 | <.0001 | 1.1 | 0.9 | 1.2 | .3047 |
| Difference after DCE, age 19–25 | 1.9 | 1.8 | 2.1 | <.0001 | 1.5 | 1.4 | 1.7 | <.0001 |
| Difference in difference, age 19–25 | 1.4 | 1.2 | 1.6 | <.0001 | 1.4 | 1.3 | 1.7 | <.0001 |
| Difference prior to DCE, age 26–34 | 1.6 | 1.3 | 1.9 | <.0001 | 1.1 | 0.9 | 1.3 | .4729 |
| Difference after DCE, age 26–34 | 1.5 | 1.3 | 1.8 | <.0001 | 1.1 | 0.9 | 1.2 | .5422 |
| Difference in difference, age 26–34 | 1.0 | 0.8 | 1.2 | .8579 | 1.0 | 0.8 | 1.2 | .9039 |
| DDD across age groups | 1.4 | 1.1 | 1.8 | .0026 | 1.5 | 1.1 | 1.9 | .0072 |
| White–Hispanic comparison | ||||||||
| Difference prior to DCE, age 19–25 | 2.4 | 2.2 | 2.7 | <.0001 | 1.9 | 1.7 | 2.1 | <.0001 |
| Difference after DCE, age 19–25 | 2.9 | 2.7 | 3.1 | <.0001 | 2.4 | 2.2 | 2.6 | <.0001 |
| Difference in difference, age 19–25 | 1.2 | 1.1 | 1.4 | .0025 | 1.3 | 1.1 | 1.4 | .0001 |
| Difference prior to DCE, age 26–34 | 3.0 | 2.7 | 3.3 | <.0001 | 1.8 | 1.6 | 2.1 | <.0001 |
| Difference after DCE, age 26–34 | 2.4 | 2.2 | 2.8 | <.0001 | 1.6 | 1.4 | 1.9 | <.0001 |
| Difference in difference, age 26–34 | 0.8 | 0.7 | 1.0 | .0181 | 0.9 | 0.8 | 1.1 | .2103 |
| DDD across age groups | 1.5 | 1.2 | 1.8 | <.0001 | 1.4 | 1.1 | 1.8 | .0013 |
†Covariate adjusted models include control for sex, marital status, income, and education.
DCE, dependent coverage expansion; DDD, difference in difference in difference; NSDUH, National Survey of Drug Use and Health; upper and lower limits shown for the 95% confidence interval.
The unadjusted models for the white–black comparison show that among the 19‐ to 25‐year‐old age group, whites were significantly more likely to have insurance before the DCE (OR = 1.4, 95 percent CI 1.2–15) and that the disparity in insurance coverage was larger after the DCE (OR = 1.9, 95 percent CI 1.8–2.1). The increase in disparity between the two time periods was statistically significant in this age group (OR = 1.4, 95 percent CI 1.2–1.6). In contrast, among the 26‐ to 34‐year‐old age group, the disparity was significant in both time periods (PRE: OR = 1.6, 95 percent CI 1.3–1.9; POST: OR = 1.5, 95 percent CI 1.3–1.8), but there was no change in this disparity between the time periods (OR = 1.0, 95 percent CI 0.8–1.2). The DDD estimate, which compares the temporal change in disparities between the two age groups, is statistically significant (OR = 1.4, 95 percent CI 1.1–1.8). In the model adjusting for covariates, the estimates of disparities between whites and blacks are reduced, but the DDD estimate indicating a relative increase in disparities among the younger than the older age group remains statistically significant (OR = 1.5, 95 percent CI 1.1–1.9). The magnitude of the impact of the DCE on disparities between whites and blacks was estimated using a linear regression model; the model indicates that the DCE increased disparities between whites and blacks by 5 percent.
Results for the comparison between whites and Hispanics differ in some respects from that between whites and blacks. Disparities between whites and Hispanics are larger in magnitude than those between whites and blacks for both age groups before and after the DCE. In addition, in the unadjusted model, there is a statistically significant decrease in disparities between whites and Hispanics among the 26‐ to 34‐year‐old age group between the pre‐ and post‐DCE periods (OR = 0.8, 95 percent CI 0.7–1.0). However, the DDD estimate of the impact of the DCE on disparities is similar; the DDD estimates of the DCE impact on disparities are significant in both the unadjusted model (OR = 1.5, 95 percent CI 1.2–1.8) and the adjusted model (OR = 1.4, 95 percent CI 1.1–1.8). Linear regression indicates that the DCE increased disparities between whites and Hispanics by 4 percent.
Secondary analyses were conducted examining private and public insurance coverage. For private insurance coverage, the unadjusted DDD estimate of the impact of the DCE on disparities is smaller than observed for any insurance, but statistically significant for disparities between whites and blacks (OR = 1.2, 95 percent CI 1.0–1.4) and disparities between whites and Hispanics (OR = 1.2, 95 percent CI 1.0–1.4). In adjusted models, the impact on disparities between whites and blacks remains statistically significant (OR = 1.2, 95 percent CI 1.0–1.5), while the impact on disparities between whites and Hispanics is no longer statistically significant (OR = 1.1, 95 percent CI 0.9–1.4). For public insurance, none of the models find DDD estimates approaching statistical significance (p‐values range from .317 to .570).
The robustness of the results was tested using two methods suggested in the literature. (Results available from authors.) First, following Slusky (2015), we tested for placebo effects, that is, significant DDD results using time points prior to the DCE at which no policy impacts were expected. Tests using 2006 and 2008 as cutpoints found no statistically significant DDD contrasts for either disparity, suggesting that the trends prior to the DCE were parallel. Second, to account for early implementation of the DCE prior to September 2010 (Busch, Golberstein, and Meara 2014), we reran the analyses excluding the 2010 survey year, as some prior studies have done (Chua and Sommers 2014; Scott et al. 2015a,b). Results excluding data from 2010 were similar to those reported in Table 2.
Discussion
Prior studies provide strong evidence that the DCE has had a positive impact on health insurance coverage among young adults, the age group that historically has been least likely to be covered (Collins et al. 2012; Sommers et al. 2013; Blumenthal and Collins 2014). However, the evidence to date regarding the equity effect of the DCE, specifically its impact on race/ethnic disparities, has not been clear, perhaps due to the short follow‐up period examined in prior studies. In this study, which used data from a large national survey through the end of 2013, preceding the ACAs Medicaid expansions and health insurance marketplaces, the evidence is clear that the DCE widened race/ethnic disparities in insurance coverage for both blacks and Hispanics relative to whites. The impact of the DCE on disparities in insurance coverage is particularly important because of the potential influence of disparities in coverage on disparities in health care utilization and health status. A growing literature suggests that the DCE has had some positive downstream impacts (Barbaresco, Courtemanche, and Qi 2015). Although evidence to date does not suggest that the DCE has impacted utilization in general (Shane, Ayyagari, and Wehby 2016), there is evidence that it has increased utilization of behavioral health care services (Saloner and Le Cook 2014; Breslau et al. in press). Disparities in the impact of the DCE could result in widening disparities in these downstream outcomes.
Secondary analyses that examined the impact of the DCE on disparities on private and public insurance coverage separately confirm the direction of impact and the specificity of the impact on private versus public insurance sources, but also suggest that the effects were smaller in magnitude. These results should be interpreted in light of evidence that respondents report whether they have any insurance more accurately than they report specific sources of coverage (Nelson et al. 2000).
A strength of this study is that it covers the entire period during which the DCE was likely to be the dominant policy influence on disparities in health insurance coverage in this age group, from the initial implementation through the Medicaid expansion in 2014, which is likely to have had distinct effects. Although some states expanded Medicaid prior to 2014, studies of those early expansion states show larger increases in coverage among the older compared to younger adults (Sommers, Kenney, and Epstein 2014). Early expansion of Medicaid may have influenced results of this and other studies of the DCE, but it is likely to have reduced the apparent impact of the DCE on coverage and on disparities in coverage.
Perhaps most important, this finding highlights the need to examine contemporary as well as historical causes of health disparities and acknowledge the complex challenges of achieving a more equitable health system through health policy (Alegría et al. 2016). Unintended adverse effects on health equity can occur if relatively advantaged individuals among the target population are better able to take advantage of new opportunities. In this case, the DCE offered a benefit only to those whose parents or guardians were privately insured, a group that is likely to be relatively advantaged not only with respect to access to care but also with respect to socioeconomic status, since private coverage is more common among those with higher incomes (Smith and Medalia 2015).
Supporting information
Appendix SA1: Author Matrix.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: This research was supported by a grant from the National Institute on Minority Health and Health Disparities (R01 MD010274).
Disclosures: None.
Disclaimers: None.
References
- Akosa Antwi, Y. , Moriya A. S., and Simon K.. 2013. “Effects of Federal Policy to Insure Young Adults: Evidence from the 2010 Affordable Care Act's Dependent‐Coverage Mandate.” American Economic Journal: Economic Policy 5 (4): 1–28. [Google Scholar]
- Alegría, M. , Alvarez K., Ishikawa R. Z., DiMarzio K., and McPeck S.. 2016. “Removing Obstacles to Eliminating Racial and Ethnic Disparities in Behavioral Health Care.” Health Affairs 35 (6): 991–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barbaresco, S. , Courtemanche C. J., and Qi Y. L.. 2015. “Impacts of the Affordable Care Act Dependent Coverage Provision on Health‐Related Outcomes of Young Adults.” Journal of Health Economics 40: 54–68. [DOI] [PubMed] [Google Scholar]
- Benach, J. , Malmusi D., Yasui Y., Martínez J. M., and Muntaner C.. 2011. “Beyond Rose's Strategies: A Typology of Scenarios of Policy Impact on Population Health and Health Inequalities.” International Journal of Health Services 41 (1): 1–9. [DOI] [PubMed] [Google Scholar]
- Blumenthal, D. , and Collins S. R.. 2014. “Health Care Coverage under the Affordable Care Act—a Progress Report.” New England Journal of Medicine 371 (3): 275–81. [DOI] [PubMed] [Google Scholar]
- Breslau, J. , Stein B. D., Han B., Shelton S., and Yu H. 2017. “Impact of the Affordable Care Act's Dependent Coverage Expansion on the Health Care and Health Status of Young Adults: What Do We Know So Far?” Medical Care Research and Review, DOI: 10.1177/1077558716682171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Busch, S. H. , Golberstein E., and Meara E.. 2014. “ACA Dependent Coverage Provision Reduced High Out‐of‐Pocket Health Care Spending for Young Adults.” Health Affairs (Millwood) 33 (8): 1361–6. [DOI] [PubMed] [Google Scholar]
- Call, K. T. , Davern M. E., Klerman J. A., and Lynch V.. 2013. “Comparing Errors in Medicaid Reporting across Surveys: Evidence to Date.” Health Services Research 48(2 pt 1): 652–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cerdá, M. , Tracy M., Ahern J., and Galea S.. 2014. “Addressing Population Health and Health Inequalities: The Role of Fundamental Causes.” American Journal of Public Health 104 (S4): S609–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chua, K. , and Sommers B. D.. 2014. “Changes in Health and Medical Spending among Young Adults under Health Reform.” JAMA 311 (23): 2437–9. [DOI] [PubMed] [Google Scholar]
- Collins, S. R. , Garber T., and Robertson R.. 2011. “Realizing Health Reform's Potential: How the Affordable Care Act Is Helping Young Adults Stay Covered.” Issue Brief (Commonwealth Fund) 5: 1–26. [PubMed] [Google Scholar]
- Collins, S. R. , Robertson R., Garber T., and Doty M. M.. 2012. “Young, Uninsured, and in Debt: Why Young Adults Lack Health Insurance and How the Affordable Care Act Is Helping: Findings from the Commonwealth Fund Health Insurance Tracking Survey of Young Adults, 2011.” Issue Brief (Commonw Fund) 14: 1–24. [PubMed] [Google Scholar]
- Frohlich, K. L. , and Potvin L.. 2008. “Transcending the Known in Public Health Practice.” American Journal of Public Health 98 (2): 216–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill, S. C. 2007. “The Accuracy of Reported Insurance Status in the MEPS.” Inquiry 44 (4): 443–68. [DOI] [PubMed] [Google Scholar]
- Howell, B. L. , Conway P. H., and Rajkumar R.. 2015. “Guiding Principles for Center for Medicare and Medicaid Innovation Model Evaluations.” JAMA 313 (23): 2317–8. [DOI] [PubMed] [Google Scholar]
- Koh, H. K. , Graham G., and Glied S. A.. 2011. “Reducing Racial and Ethnic Disparities: The Action Plan from the Department of Health and Human Services.” Health Affairs (Millwood) 30 (10): 1822–9. [DOI] [PubMed] [Google Scholar]
- Kotagal, M. , Carle A. C., Kessler L. G., and Flum D. R.. 2014. “Limited Impact on Health and Access to Care for 19‐ to 25‐year‐olds Following the Patient Protection and Affordable Care Act.” JAMA Pediatr 168 (11): 1023–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mechanic, D. 2002. “Disadvantage, Inequality, and Social Policy.” Health Affairs 21 (2): 48–59. [DOI] [PubMed] [Google Scholar]
- Nelson, D. E. , Thompson B. L., Davenport N. J., and Penaloza L. J.. 2000. “What People Really Know about Their Health Insurance: A Comparison of Information Obtained from Individuals and Their Insurers.” American Journal of Public Health 90 (6): 924–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Hara, B. , and Brault M. W.. 2013. “The Disparate Impact of the ACA‐Dependent Expansion across Population Subgroups.” Health Services Research 48 (5): 1581–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phelan, J. C. , and Link B. G.. 2005. “Controlling Disease and Creating Disparities: A Fundamental Cause Perspective.” The Journals of Gerontology Series B: Psychological Sciences and Social Sciences 60 (Special Issue 2): S27–33. [DOI] [PubMed] [Google Scholar]
- Phelan, J. C. , Link B. G., and Tehranifar P.. 2010. “Social Conditions as Fundamental Causes of Health Inequalities: Theory, Evidence, and Policy Implications.” Journal of Health and Social Behavior 51 (1 suppl): S28–40. [DOI] [PubMed] [Google Scholar]
- Ryan, A. M. , Burgess J. F. Jr, and Dimick J. B.. 2015. “Why We Should Not Be Indifferent to Specification Choices for Difference‐in‐Differences.” Health Services Research 50 (4): 1211–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saloner, B. , and Le Cook B.. 2014. “An ACA Provision Increased Treatment for Young Adults with Possible Mental Illnesses Relative to Comparison Group.” Health Aff (Millwood) 33 (8): 1425–34. [DOI] [PubMed] [Google Scholar]
- Scott, J. W. , Salim A., Sommers B. D., Tsai T. C., Scott K. W., and Song Z. R.. 2015a. “Racial and Regional Disparities in the Effect of the Affordable Care Act's Dependent Coverage Provision on Young Adult Trauma Patients.” Journal of the American College of Surgeons 221 (2): 495–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott, J. W. , Sommers B. D., Tsai T. C., Scott K. W., Schwartz A. L., and Song Z.. 2015b. “Dependent Coverage Provision Led to Uneven Insurance Gains and Unchanged Mortality Rates in Young Adult Trauma Patients.” Health Affairs 34 (1): 124–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shane, D. M. , and Ayyagari P.. 2014. “Will Health Care Reform Reduce Disparities in Insurance Coverage?: Evidence from the Dependent Coverage Mandate.” Medical Care 52 (6): 528–34. [DOI] [PubMed] [Google Scholar]
- Shane, D. M. , Ayyagari P., and Wehby G.. 2016. “Continued Gains in Health Insurance but Few Signs of Increased Utilization: An Update on the ACA's Dependent Coverage Mandate.” Medical Care Research and Review: MCRR 73 (4): 478–92. [DOI] [PubMed] [Google Scholar]
- Slusky, D. J. . 2015. “Significant Placebo Results in Difference‐in‐Differences Analysis: The Case of the ACA's Parental Mandate.” Eastern Economic Journal, DOI: 10.1057/eej.2015.49. [Google Scholar]
- Smith, J. C. , and Medalia C.. 2015. Health Insurance Coverage in the United States, 2014. Current Population Reports. Washington, DC: U.S. Census Bureau. P60‐253. [Google Scholar]
- Sommers, B. D. , Kenney G. M., and Epstein A. M.. 2014. “New Evidence on the Affordable Care Act: Coverage Impacts of Early Medicaid Expansions.” Health Affairs 33 (1): 78–87. [DOI] [PubMed] [Google Scholar]
- Sommers, B. D. , Buchmueller T., Decker S. L., Carey C., and Kronick R.. 2013. “The Affordable Care Act Has Led to Significant Gains in Health Insurance and Access to Care for Young Adults.” Health Affairs 32 (1): 165–74. [DOI] [PubMed] [Google Scholar]
- Wallace, J. , and Sommers B. D.. 2015. “Effect of Dependent Coverage Expansion of the Affordable Care Act on Health and Access to Care for Young Adults.” JAMA Pediatr 169 (5): 495–7. [DOI] [PubMed] [Google Scholar]
- Williams, D. R. , and Jackson P. B.. 2005. “Social Sources of Racial Disparities in Health.” Health Affairs (Millwood) 24 (2): 325–34. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix SA1: Author Matrix.


