Abstract
Objective
To investigate compliance with telephone helpline advice to attend an emergency department (ED) and the acuity of patients who presented to ED following a call.
Data Sources/Collection Methods
In New South Wales (NSW), Australia, 2009–2012, all (1.04 million) calls to a telephone triage service, ED presentations, hospital admissions and death registrations, linked using probabilistic data linkage.
Study Design
Population‐based, observational cohort study measuring ED presentations within 24 hours of a call in patients (1) with dispositions to attend ED (compliance) and (2) low‐urgency dispositions (self‐referral), triage categories on ED presentation.
Principal Findings
A total of 66.5 percent of patients were compliant with dispositions to attend an ED. A total of 6.2 percent of patients with low‐urgency dispositions self‐referred to the ED within 24 hours. After age adjustment, healthdirect compliant patients were significantly less likely (7.8 percent) to receive the least urgent ED triage category compared to the general NSW ED population (16.9 percent).
Conclusions
This large population‐based data linkage study provides precise estimates of ED attendance following calls to a telephone triage service and details the predictors of ED attendance. Patients who attend an ED compliant with a healthdirect helpline disposition are significantly less likely than the general ED population to receive the lowest urgency triage category on arrival.
Keywords: Administrative data uses; epidemiology; hospitals; referrals, referral networks
Over the last decade, many countries have experienced a large growth in telephone health advice and triage services (O'Connell et al. 2002; Sprivulis, Carey, and Rouse 2004; De Coster et al. 2010; Australian Medical Association 2014; Campbell et al. 2014). These services may be designed for patients of health care facilities (Hansen and Hunskaar 2011; Campbell et al. 2014), health maintenance organizations (O'Connell et al. 2002; Kempe et al. 2006; Navratil‐Strawn et al. 2014), or a whole population (De Coster et al. 2010) (Foster, Jessopp, and Chakraborti 2003; Labarere et al. 2003). The population of NSW, Australia, has access to the healthdirect helpline telephone triage service and publicly funded universal health care, and some may access private health care. Telephone triage services have been well received by the public (Hughes 2003; Ng et al. 2012), but they have been viewed cautiously by medical professionals, especially when services have been established for politically driven objectives not supported by evidence (Australian Medical Association 2014; Lind 2015), or when there is little information on compliance with, or appropriateness of, advice given. This study aims to provide high‐quality evidence regarding patient compliance with telephone triage advice to attend an ED, self‐referred attendance at an ED in calls given low‐urgency dispositions, and patient triage on arrival at the ED following a call.
Some of the existing research relies on self‐reporting to measure compliance (Kempe et al. 2001; Hansen and Hunskaar 2011; O'Cathain et al. 2014), which is subject to recall and social desirability biases. Using linked data minimizes these biases, although it is rarely performed for whole populations. A data linkage study from Calgary, Canada, reported that 52.3 percent of patients instructed to “go to ED” complied within 24 hours (De Coster et al. 2010), although the study was limited to one major city. Some American studies have reported compliance, but they are generally restricted to members of specific health maintenance organizations: 57.4 percent of patients attended ED as advised within 2 days (Navratil‐Strawn et al. 2014); 79.2 percent of patients attended hospital ED as advised within 2 days (O'Connell et al. 2002); and 74.0 percent of children attended hospital as advised within 4 hours (Kempe et al. 2006). Information on factors associated with compliance is patchy, even though such information could assist in improving telephone triage service delivery and illustrate particular barriers to health service access. Studies have shown that those patients more likely to comply with advice to attend emergency care are older (O'Connell et al. 2002; De Coster et al. 2010), have better background health, reside in middle‐ or high‐income neighborhoods (De Coster et al. 2010), or are younger children in the case of a pediatric study (Scarfone, Luberti, and Mistry 2004). Another study showed little impact of patient demographics (Niemann et al. 2004). Compliance is highest when the patient is satisfied with the disposition (Labarere et al. 2003; Lee et al. 2003) or when the patient's original intention is concordant with the call disposition (Munro et al. 2001; Niemann et al. 2004). The research on patients who attend an ED after telephone triage, despite not having been advised to do so, is sparse, and the definitions of what constitutes this form of “self‐referral” noncompliance are inconsistent. A small British study reported 2.4 percent of patients given non‐ED dispositions attended ED with the same presenting complaint as their telephone triage call. These subjects took significantly longer to attend ED than those who were advised to do so (Foster, Jessopp, and Chakraborti 2003). A Western Australian study of helpline callers residing within 2 km of a hospital showed that 9 percent of callers given a “nonurgent disposition” (disposition to seek care in 24 hours or later) presented at the ED within 24 hours (Sprivulis, Carey, and Rouse 2004).
In Australia, the “healthdirect helpline” telephone triage service aims to provide patients with trusted health professional advice about the appropriate care for their health issue and to help them find their closest appropriate and available local health service, regardless of the time of the call or the location of the caller (Healthdirect Australia 2015). This study used linked population‐based ED and hospital data to provide information on compliance with helpline advice to attend an ED and rates of self‐referral to ED. Under‐referral was investigated by quantifying hospitalizations, deaths, and more urgently triaged ED presentations in patients given low‐urgency dispositions, while over‐referral was examined by quantifying the least urgently triaged ED presentations in patients given dispositions to attend ED.
Methods
Setting
The healthdirect helpline is a telephone triage service that caters for six of eight Australian states and territories. It operates 24 hours a day, 7 days a week, and between 2009 and 2012, handled an average of 785,720 calls per year. Due to restricted funding, the service is minimally promoted, most commonly by word of mouth (personal communication, Healthdirect Australia). Calls are initially triaged by registered nurses, but since July 2011 some after‐hours calls are transferred on triage nurse discretion to an after‐hours GP for additional triage. Triage staff members assess health symptoms using a computerized clinical decision support system (CareEnhance Call Centre Software, Medibank Health Solutions Pty Ltd., Lane Cove, NSW, Australia). Prompted by the software, the triage staff member asks a series of questions designed to rule out important conditions and arrives at the condition that cannot be excluded (Graber et al. 2003). Triage staff have no access to a patient's medical history and assess a patient based on information reported in the telephone call. At the conclusion of the call, the triage staff member provides a “disposition”—a recommendation to follow a course of action. Dispositions include activating triple zero “000” (Australia‐wide phone number for an ambulance), attending an ED (public or private), attending a GP within a particular time frame, or appropriate guided self‐care. Calls triaged by nurses should only have one disposition, and calls referred to after‐hour GP triage should have one nurse‐triaged disposition with the value “speak to telephone GP” and one GP‐triaged disposition. At the conclusion of the call, callers are asked for their “original intention,” what they had intended to do if they had not called the healthdirect helpline. For reasons of data availability, the study was restricted to New South Wales (NSW), Australia's largest state, with a population of 7.29 million in 2012 (Australian Bureau of Statistics 2013), and to specific dispositions, described later.
On arrival at a hospital ED, patients undergo triage by a clinician, a process of prioritization based on clinical urgency, determined by patient condition and the potential for deterioration. This is described by the Australasian Triage Scale (ATS), a five‐point scale ranging from ATS 1 (medical attention immediately) to ATS 5 (medical attention within 2 hours)(Australasian College for Emergency Medicine 2013). It is not standard for ED clinicians to ask whether the patient has had prior contact with the healthdirect helpline.
Data Linkage and Cleaning
This was an observational cohort study using the following linked data: healthdirect helpline call data (NSW, July 1, 2008 to December 31, 2012); presentations to EDs; hospital admissions; and death registrations in NSW for the same period. Hospital data include records of hospital separations (discharges, transfers, and deaths) in all public and private hospitals, while ED data capture approximately 96 percent of NSW public and private ED presentations, with some small rural EDs excluded (personal communication, NSW Department of Health). Probabilistic data linkage and the assignment of a “Project‐specific Person Number” (PPN) were performed by the Centre for Health Record Linkage (CHeReL). Data custodians matched PPNs with their respective clinical data and provided researchers with datasets containing PPN, demographic, and clinical variables. Researchers merged all the datasets using the PPN. Prior to analysis, all linked datasets were checked for inconsistencies, with exclusions listed in Figure 1.
Figure 1.
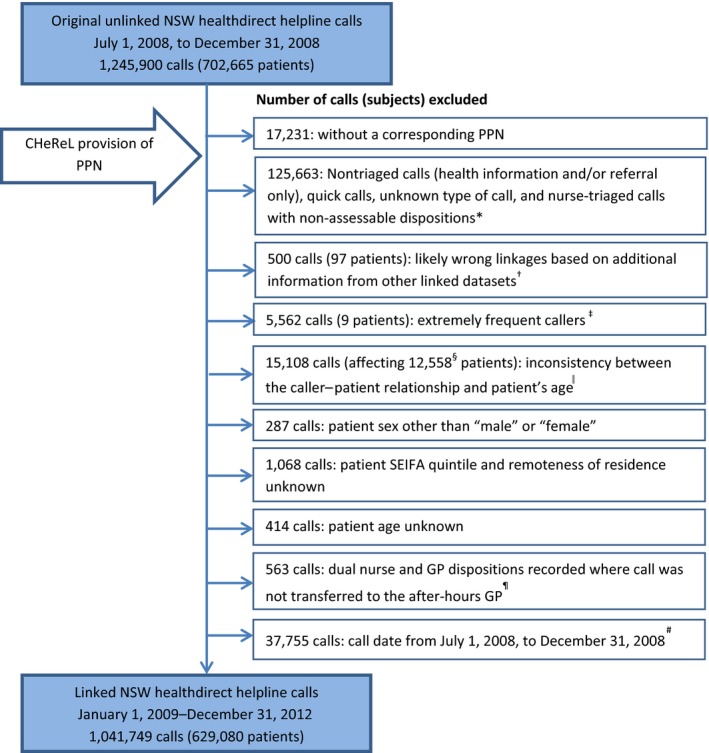
Flowchart of Call and Subject Exclusions Used for Descriptive Analysis and Compliance Rates [Color figure can be viewed at wileyonlinelibrary.com]
Notes. *Calls given nonassessable dispositions included dispositions such as a transfer to Sexual Assault Referral Centre or the Poisons Information Service. †Calls identified as likely wrong linkages included records of a healthdirect helpline call record occurring after a death record. ‡Subjects identified as “extremely frequent callers” were defined as callers with a series of 20 or more calls to the healthdirect helpline where the time between calls of the same series was less than or equal to 24 hours. §These 12,558 subjects had at least one call excluded due to an inconsistency between the caller–patient relationship and the patient's age. These included 3,743 subjects who had all their calls excluded. ‖Calls with inconsistent information between the caller–patient relationship and the patient's age included patients below 10 years calling for “self,” “grandchildren” calling for patients below 25 years, and “grandparents” calling for patients aged 60 years and older. ¶These were most likely the result of vulnerability in the data collection software and could be the result of a triage nurse attempting to triage two sets of symptoms in a single call (personal communication, Healthdirect Australia). #Note that calls dated between July 1, 2008, and December 31, 2008, were excluded from descriptive analysis and the calculation of compliance rates, but they were used to calculate the variable “calls to healthdirect in the last 6 months,” a covariate in regression models.
Outcome Measures and Definitions
This paper analyzes dispositions to attend an ED immediately and low‐urgency dispositions. Dispositions to attend an ED immediately included both nurse and GP dispositions of “ED immediately” and “ED immediately (GP not available).” Compliance with this disposition was defined as the presence of a linked record for an ED visit or hospital admission within 24 hours of the call to the healthdirect helpline. If the same patient was the subject of two or more calls with “Attend ED” dispositions within 24 hours, the patient was considered noncompliant with the earlier call/s and only the compliance to the final call in the 24‐hour period was assessed. Low‐urgency dispositions included dispositions for self‐care only; see a doctor within 72 hours or 2 weeks; see a dentist within 72 hours, 2 weeks, or when available; and see an appropriate health provider within 72 hours or 2 weeks. Self‐referral to an ED was defined as the presence of a linked record for an ED visit or hospital admission within 24 hours of the call to the healthdirect helpline, having received a low‐urgency disposition. Hospital admissions and deaths were confirmed by the presence of their respective linked records.
A call was considered “in‐hours” if it occurred during common NSW GP opening hours (8 a.m. to 6 p.m., Mondays to Fridays, 8 a.m. to 12 p.m., Saturdays). All other times or NSW public holidays were considered to be “after‐hours.”
Analyses
Summary statistics on call characteristics and demographics were calculated for all calls. Modeling of both the predictors of compliance and self‐referral was first conducted using hierarchical logistic regression modeling of multiple calls (level 1) nested within patients (level 2). However, as the majority of patients had only a single call in the dataset, modeling the higher level variation added very little information. Instead, final predictive models used a single‐level logistic regression using Proc Genmod (SAS). The factors included in the models were as follows: patient sex; age group; socioeconomic status (Socio‐Economic Indexes for Areas [SEIFA], mapped from patient postcode) (Australian Bureau of Statistics 2011); a composite variable of time of call and triage staff (nurse in‐hours, nurse after‐hours, and GP after‐hours); remoteness at time of call (ARIA+ [Australian Population and Migrations Research Centre 2015], mapped from patient postcode); caller's original intention; number of healthdirect helpline calls in the previous 6 months; the caller's relationship to the patient (self/other); and groups of clinical symptoms. Unadjusted (crude) and adjusted odds ratios (OR) and 95 percent confidence intervals (CI) were calculated.
Summary data of ED presentations by age group and ATS categories were obtained from the NSW Ministry of Health. The distribution of ATS categories in the healthdirect subjects was age‐standardized to the population of NSW ED presentations during the same time period. Calls with missing ATS information were excluded from the compliant attending (n = 1,819 of 102,999 excluded) and self‐referred groups (n = 610 of 19,211 excluded). Data analysis was performed using SAS version 9.3 (Cary, NC, USA), STATA/ MP Version 12.1 (College Station, TX, USA), MLwiN (University of Bristol, Bristol, UK), and Excel (Redmond, WA, USA).
Ethics Approvals
This study was approved by the NSW Population and Health Services Research Ethics Committee (No 2014/02/508) and all data custodians.
Results
Data Linkage and Cleaning
Between July 1, 2008, and December 31, 2012, 1,245,900 calls were made to the NSW healthdirect helpline regarding 702,665 patients. Call and subject exclusions are shown in Figure 1. After data cleaning, 1,041,749 calls from January 1, 2009, to December 31, 2012 (regarding 629,080 patients), were included in the descriptive analysis. The 97 patients excluded on the basis of likely false linkages (0.014 percent of patients) were consistent with the reported CHeReL false‐positive linkage rate of 0.4 percent.
Healthdirect Helpline Call and Patient Characteristics
The mean patient age at the time of the healthdirect helpline call was 24.6 years (SD 24.1), ranging from 0 to 109 years. Children younger than 5 years were the subject of the call (the patient) in 34.3 percent of calls, and 59.5 percent of calls regarded a female patient. Callers were most commonly calling regarding themselves (45.2 percent) or regarding their children (44.8 percent). Three‐quarters (75.2 percent) of the 1,041,749 calls were made after hours. Three‐quarters (74.9 percent) of the calls came from major cities, and 4.9 percent came from outer regional and more remote areas. Calls from areas in the middle SEIFA quintile made up the largest group (27.8 percent) of calls. Characteristics of calls are given in Table 1.
Table 1.
Characteristics of Calls to the NSW Healthdirect Helpline January 1, 2009, to December 31, 2012: All Healthdirect Calls, Calls with Dispositions to Attend an ED Immediately, and Calls with “Low‐Urgency” Dispositions
| All Healthdirect Calls (%) | Attend ED Immediately Dispositions (%) | Low‐Urgency Dispositions (%) | |
|---|---|---|---|
| Patient age | |||
| 0–4 years | 357,690 (34.34) | 50,882 (32.87) | 160,334 (52.09) |
| 5–9 years | 73,004 (7.01) | 13,995 (9.04) | 25,239 (8.20) |
| 10–14 years | 35,715 (3.43) | 8,409 (5.43) | 10,187 (3.31) |
| 15–17 years | 22,398 (2.15) | 4,187 (2.70) | 4,151 (1.35) |
| 18–34 years | 225,521 (21.65) | 34,186 (22.09) | 41,665 (13.54) |
| 35–44 years | 108,743 (10.44) | 14,239 (9.20) | 19,764 (6.42) |
| 45–54 years | 71,665 (6.88) | 9,756 (6.30) | 14,269 (4.64) |
| 55–64 years | 58,165 (5.58) | 7,506 (4.85) | 12,695 (4.12) |
| 65–74 years | 44,401 (4.26) | 5,769 (3.73) | 9,765 (3.17) |
| 75+ years | 44,447 (4.27) | 5,859 (3.79) | 9,756 (3.17) |
| Sex | |||
| Females | 619,422 (59.46) | 87,978 (56.84) | 171,813 (55.82) |
| Males | 422,327 (40.54) | 66,810 (43.16) | 136,012 (44.18) |
| Caller relationship to patient | |||
| Self | 471,249 (45.24) | 61,367 (39.65) | 94,787 (30.79) |
| Parent | 466,850 (44.81) | 74,101 (47.87) | 190,465 (61.87) |
| Carer | 4,117 (0.40) | 519 (0.34) | 1,486 (0.48) |
| Child | 17,903 (1.72) | 3,080 (1.99) | 2,784 (0.90) |
| Spouse, partner | 41,335 (3.97) | 8,369 (5.41) | 6,274 (2.04) |
| Grandparent | 6,966 (0.67) | 1,134 (0.73) | 2,729 (0.89) |
| Grandchild | 863 (0.08) | 153 (0.10) | 136 (0.04) |
| Other | 15,911 (1.53) | 3,332 (2.15) | 3,896 (1.27) |
| Unknown | 16,555 (1.59) | 2,733 (1.77) | 5,268 (1.71) |
| Triage staff and call time | |||
| Nurse in‐hours | 258,251 (24.79) | 30,373 (19.62) | 80,073 (26.01) |
| Nurse after‐hours | 687,898 (66.03) | 103,045 (66.57) | 219,293 (71.23) |
| GP after‐hours | 95,600 (9.18) | 21,370 (13.81) | 8,484 (2.76) |
| Original intention | |||
| Call 000 | 23,473 (2.25) | 5,772 (3.73) | 3,385 (1.10) |
| Attend ED | 193,022 (18.53) | 51,376 (33.19) | 44,611 (14.49) |
| Contact Doctor | 260,760 (25.03) | 28,097 (18.15) | 80,045 (26.00) |
| Home, self‐care | 132,919 (12.76) | 18,562 (11.99) | 51,658 (16.78) |
| Did not know what to do | 294,856 (28.30) | 42,744 (27.61) | 97,429 (31.65) |
| Nonprofessional advice | 7,452 (0.72) | 956 (0.62) | 3,282 (1.07) |
| Missing intention | 129,267 (12.41) | 7,281 (4.70) | 27,415 (8.91) |
| Healthdirect calls in past 6 months | |||
| 0 calls | 783,354 (75.20) | 121,630 (78.58) | 217,072 (70.52) |
| 1 call | 143,602 (13.78) | 19,613 (12.67) | 48,211 (15.66) |
| 2–3 calls | 70,662 (6.78) | 8,799 (5.68) | 26,575 (8.63) |
| 4–9 calls | 29,172 (2.80) | 3,213 (2.08) | 11,227 (3.65) |
| 10–19 calls | 6,967 (0.67) | 729 (0.47) | 2,338 (0.76) |
| 20 or more calls | 7,992 (0.77) | 804 (0.52) | 2,402 (0.78) |
| SEIFA | |||
| Quintile 1 (lower SES) | 157,417 (15.11) | 25,184 (16.27) | 44,525 (14.46) |
| Quintile 2 | 191,077 (18.34) | 29,895 (19.31) | 51,329 (16.67) |
| Quintile 3 | 289,133 (27.75) | 42,478 (27.44) | 78,545 (25.52) |
| Quintile 4 | 198,628 (19.07) | 28,170 (18.20) | 62,730 (20.38) |
| Quintile 5 (higher SES) | 205,494 (19.73) | 29,061 (18.77) | 70,696 (22.97) |
| Remoteness | |||
| Major city | 780,361 (74.91) | 112,078 (72.41) | 237,506 (77.16) |
| Inner regional | 210,488 (20.21) | 34,562 (22.33) | 56,394 (18.32) |
| Outer regional | 48,591 (4.66) | 7,831 (5.06) | 13,234 (4.30) |
| Remote or very remote | 2,309 (0.22) | 317 (0.20) | 691 (0.22) |
| Disposition (nurse or GP) | |||
| Activate 000 | 37,365 (3.59) | ||
| Attend ED immediately | 154,788 (14.86) | 154,788 (100) | |
| See doctor immediately | 96,747 (9.29) | ||
| See doctor within 4 hours | 125,729 (12.07) | ||
| See doctor within 24 hours, self‐care | 201,866 (19.38) | ||
| See doctor within 72 hours/2 weeks | 53,012 (5.09) | 53,012 (17.22) | |
| Self‐care only | 238,627 (22.91) | 238,627 (77.52) | |
| See mental health immediately/ within 4 hours | 1,631 (0.16) | ||
| Call Poisons Information Centre immediately | 11,922 (1.14) | ||
| See other provider within 24 hours, self‐care | 39,491 (3.79) | ||
| See other provider within 72 hours/2 weeks | 14,806 (1.42) | 14,806 (4.81) | |
| See dentist in 4 hours/24 hours | 2,893 (0.28) | ||
| See dentist in 72 hours/2 weeks/ when available | 1,380 (0.13) | 1,380 (0.45) | |
| Call terminated before completion | 33,197 (3.19) | ||
| Unknown disposition, missing, not applicable | 28,295 (2.73) | ||
| Clinical guideline groups | |||
| Skin, wounds, exposure to external agents | 128,285 (12.31) | 16,327 (10.55) | 44,519 (14.46) |
| Respiratory symptoms | 77,267 (7.42) | 18,573 (12.00) | 17,989 (5.84) |
| Head, neck, face symptoms | 100,147 (9.61) | 17,519 (11.32) | 31,149 (10.12) |
| Limb symptoms | 46,320 (4.45) | 8,980 (5.80) | 7,818 (2.54) |
| Neurological, headache, seizure | 49,592 (4.76) | 9,220 (5.96) | 5,997 (1.95) |
| Abdominal, pelvic, back symptoms | 58,272 (5.59) | 17,660 (11.41) | 8,579 (2.79) |
| Fever, cold/flu, other infectious disease | 90,552 (8.69) | 8,972 (5.80) | 39,001 (12.67) |
| Chest pain, irregular heartbeat, hypertension | 39,900 (3.83) | 9,779 (6.32) | 4,847 (1.57) |
| Bleeding, immunity, immune response | 46,832 (4.50) | 5,878 (3.80) | 13,255 (4.31) |
| GI, reproductive system, urinary system | 80,293 (7.71) | 8,240 (5.32) | 29,778 (9.67) |
| Pregnancy and neonate specific | 46,347 (4.45) | 10,780 (6.96) | 8,825 (2.87) |
| Mental health, other symptoms | 101,492 (9.74) | 19,190 (12.40) | 43,368 (14.09) |
| Seen provider earlier, general healthdirect | 176,450 (16.94) | 3,670 (2.37) | 52,700 (17.12) |
| Total calls by group | 1,041,749 (100) | 154,788 (100) | 307,825 (100) |
SEIFA, socio‐economic indexes for areas; SES, socioeconomic status.
A total of 95,600 calls (9.2 percent) received a nurse disposition of “speak to telephone GP” and were analyzed according to the GP disposition, with the remaining calls analyzed according to their nurse disposition. A total of 428 different guidelines were used for patient triage. The five most common individual guidelines were pediatric vomiting (4.3 percent), medication questions in an adult (3.7 percent), pediatric fever (3.0 percent), abdominal pain or discomfort (2.9 percent), and “seen doctor/health care provider” (2.6 percent). This last is a guideline reserved for patients who had had a recent visit to a doctor or health care provider concerning the same symptoms as the call.
The patients of the healthdirect helpline are younger and are more likely to be female than the NSW general population. Patients below 5 years made up 28.3 percent of healthdirect patients (vs. 6.5 percent NSW general population 2012), while patients 65 years and older made up 9.6 percent of healthdirect patients (vs. 14.9 percent NSW general population 2012). The ratio of males to females among healthdirect patients was 0.71 compared to 0.98 in the NSW general population. Just over 2 percent of the NSW population were patients of the healthdirect telephone triage service in a given year, ranging from 2.0 percent in 2010 to 2.5 percent in 2012 (Australian Bureau of Statistics 2012).
Rates and Predictors of Compliance in Those Given Dispositions to Attend ED Immediately
A total of 154,788 calls regarding 136,147 patients (14.9 percent of calls) between January 1, 2009, and December 31, 2012, received a disposition to attend ED immediately and were used to model the predictors of compliance (see Table 2). A total of 605 calls with “Attend ED” dispositions were followed by another call with the same disposition within 24 hours and were assumed to be noncompliant.
Table 2.
Factors Associated with Compliance with Dispositions to Attend ED Immediately (n = 154,788)
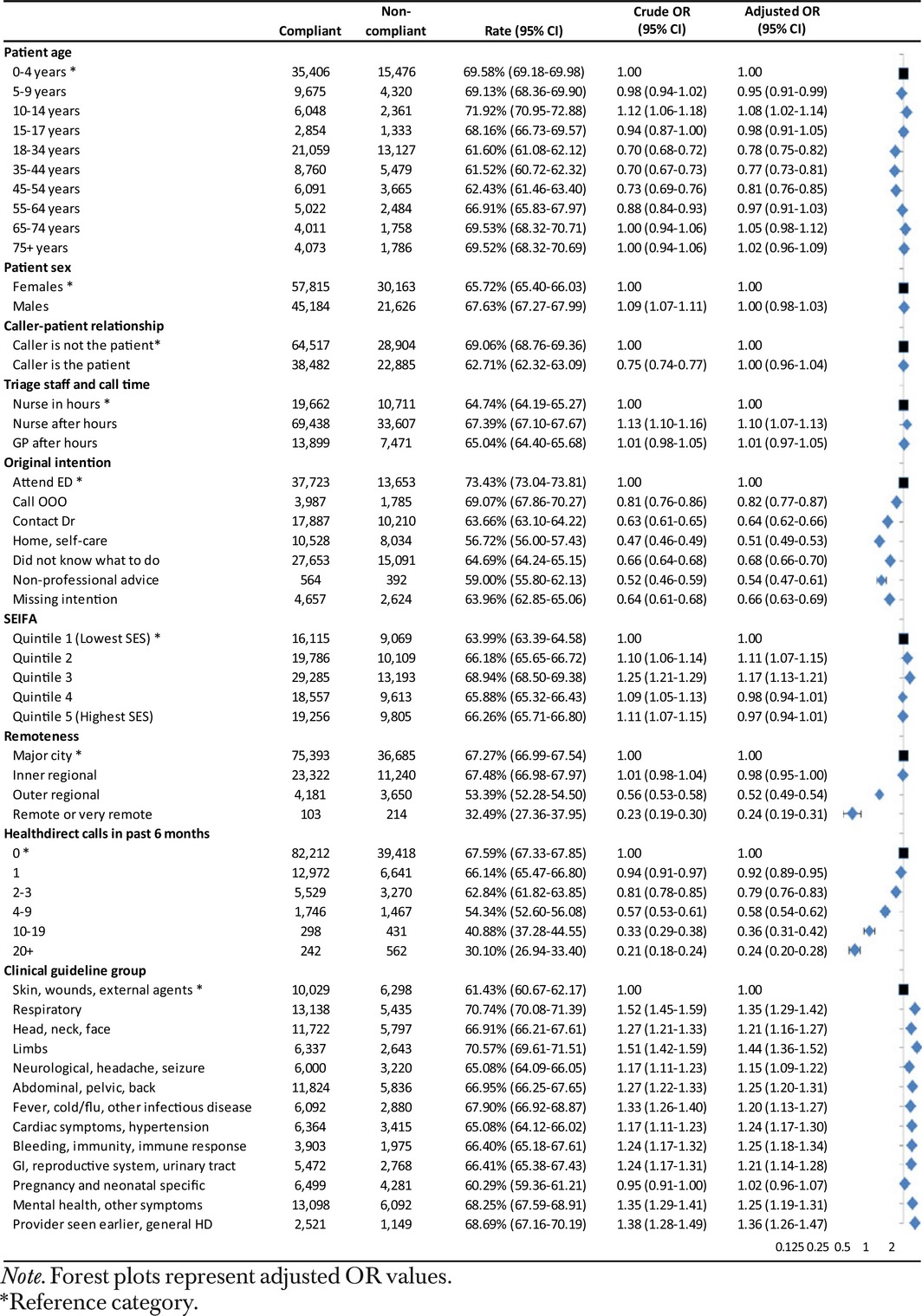
In calls given dispositions to attend ED immediately, the patient was compliant in 66.5 percent (95 percent CI 66.3 to 66.8) of calls. Compliance was identified by an ED presentation record in 98.3 percent of calls, and the remainder of compliant calls had a hospital admission record within 24 hours of the call without a preceding ED presentation record.
Controlling for other factors in the model, patients aged 10–14 years were the most compliant, while those aged from 18 to 34 years and 35 to 44 years were least compliant. Compliance was highest in those living in an area in the middle quintile of socioeconomic status. There was no significant difference by patient sex or caller–patient relationship. Compared to nurse‐triaged calls in‐hours, nurse‐triaged calls after‐hours had significantly higher compliance with dispositions to attend ED immediately, but compliance with GP‐triaged after‐hours calls was significantly lower than with nurse‐triaged calls after‐hours. Calls from outer regional and more remote areas had significantly lower compliance than calls from major cities and inner regional areas, with the lowest compliance in the most remote areas. Callers whose original intention was to attend an ED were more likely to be compliant with dispositions to attend ED immediately, compared to callers with other intentions. The more times a caller had contacted the healthdirect helpline in the previous 6 months, the less likely it was that the patient was compliant. Clinical guidelines with lower compliance included those relating to neurological, headache or seizure, and pregnancy or neonatal‐specific guidelines.
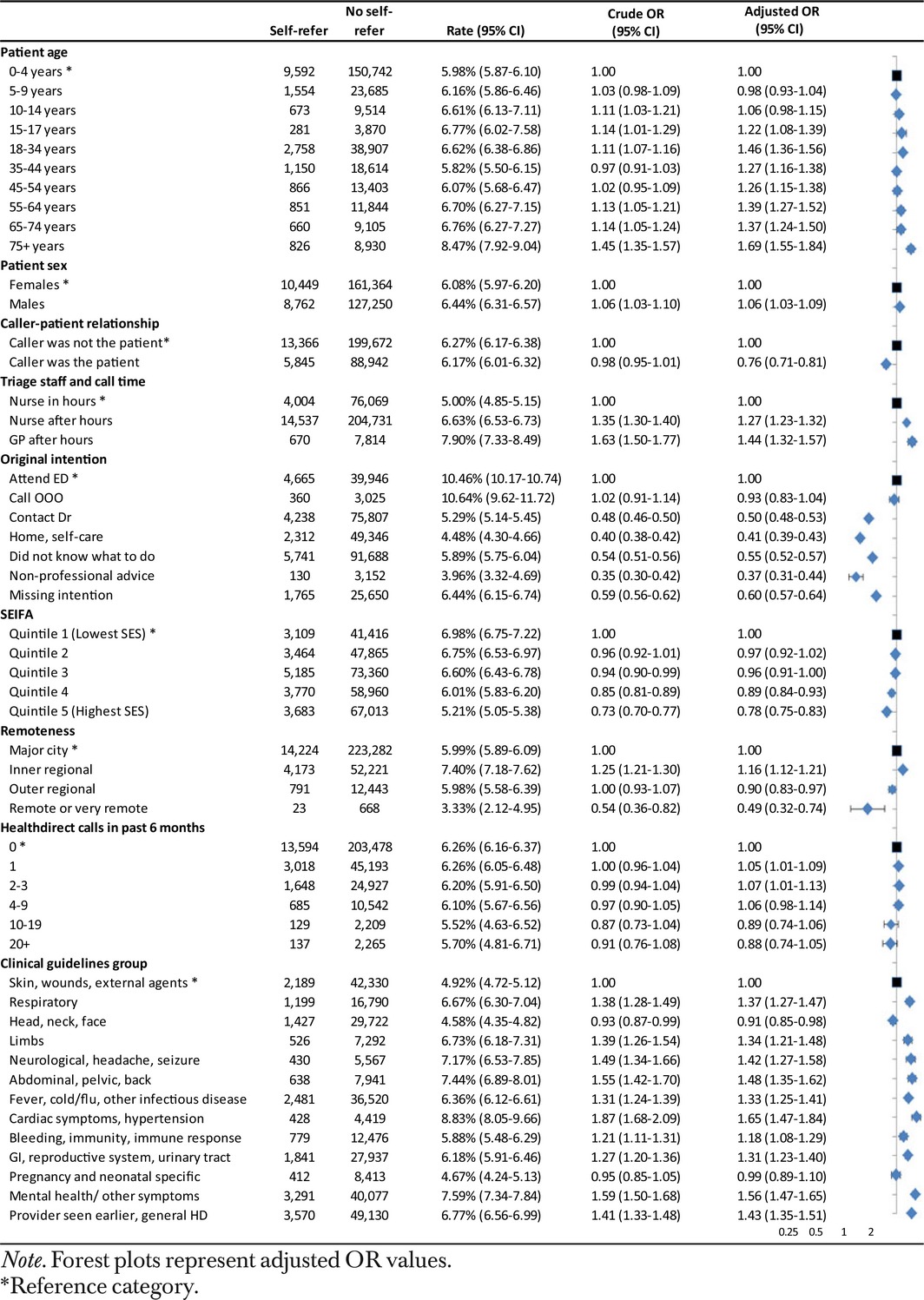
Rates and Predictors of Self‐Referral to the ED in Those Given a Low‐Urgency Disposition
A total of 307,825 NSW healthdirect helpline calls between January 1, 2009, and December 31, 2012 (regarding 216,749 unique patients), received a low‐urgency disposition, comprising 29.5 percent of all NSW calls. Following 19,211 of these calls, the patient attended an ED or hospital within 24 hours, a rate of 6.2 percent (95 percent CI 6.2 to 6.3).
Controlling for other factors in the model, patients significantly more likely to self‐refer to the ED within 24 hours of a low‐urgency disposition included males and adult patients (patients aged 18 to 34 years and 55 years and older). Those living in areas of high socioeconomic status were less likely to self‐refer than those in the lowest socioeconomic status areas, and self‐referral was also less likely if the caller was the patient rather than another person. After‐hours calls were significantly more likely to result in a self‐referral than calls made in‐hours. Calls from inner regional areas were significantly more likely, and calls from outer regional, remote, or very remote areas significantly less likely, to self‐refer compared to calls from major cities. Callers whose original intention was to attend ED were more likely to self‐refer. Clinical guidelines relating to respiratory symptoms, cardiac or hypertensive symptoms, and mental health/other symptoms had higher rates of self‐referral. Predictors of self‐referral are listed in Table 3.
Table 3.
Factors Associated with Self‐Referral to the ED within Twenty‐Four Hours in Patients Given Low‐Urgency Dispositions (n = 307,825)
Time to ED Presentation and ED Triage Category on Arrival
In patients compliant with dispositions to attend ED immediately, 94.2 percent (95 percent CI 94.1 to 94.4 percent) presented at the ED within 4 hours of the call, compared to 46.6 percent (95 percent CI 45.9 to 47.3 percent) of those who self‐referred after low‐urgency dispositions. More ED self‐referrals (30.0 percent, 95 percent CI 29.3 to 30.6 percent) occurred between 12 and 24 hours after the call, compared to 2.7 percent (95 percent CI 2.6 to 2.8) of compliant attendances. There was no evidence of difference in time to ED presentation by ATS triage level in self‐referrals to the ED, as is shown in Figure S1.
There were significant differences in the age‐adjusted distribution of ATS categories on ED presentations between healthdirect‐compliant patients, healthdirect self‐referred patients, and general NSW ED attendants. Significantly fewer compliant healthdirect patients were triaged as ATS 5 (medical attention within 120 minutes) (7.8 percent, 95 percent CI 7.6 to 7.9 percent), compared to general NSW ED attendants (16.9 percent, 95 percent CI 16.9 to 17.0 percent). By contrast, the proportion of ATS 5 among healthdirect self‐referred patients (16.9 percent, 95 percent CI 16.4 to 17.4 percent) was not significantly different from general NSW ED attendants.
Differences were also noted in triage to ATS 2 (medical attention within 10 minutes). Significantly fewer healthdirect patients who self‐referred after low‐urgency dispositions were triaged as ATS 2 (4.0 percent, 95 percent CI 3.8 to 4.3 percent) compared to the general population (8.4 percent, 95 percent CI 8.3 to 8.4 percent) and healthdirect‐compliant patients (7.0 percent, 95 percent CI 6.9 to 7.2 percent, Table 4).
Table 4.
Australasian Triage Scale Categories on ED Presentation within Twenty‐Four Hours of the Healthdirect Helpline Call for Compliant Attenders and Self‐Referred Attenders Compared to the NSW General Population of ED Attenders
| ED Triage | Healthdirect‐Compliant Attenders (Jan. 1, 2009–Dec. 31, 2012) | Healthdirect Self‐Referred Attenders (Jan. 1, 2009–Dec. 31, 2012) | NSW Population ED Attenders (July 1, 2008–June 30 2012) | |||||
|---|---|---|---|---|---|---|---|---|
| N (obs) | N (exp) | Standardized Ratea (95% CI) | N (obs) | N (exp) | Standardized Ratea (95% CI) | N (obs.) | Rate (95% CI) | |
| ATS1 | 77 | 91 | 0.09% (0.07–0.11) | 21 | 19 | 0.10% (0.06–0.16) | 51,120 | 0.60% (0.59–0.60) |
| ATS2 | 6,323 | 7,126 | 7.04% (6.89–7.20) | 675 | 751 | 4.04% (3.76–4.33) | 715,482 | 8.35% (8.34–8.37) |
| ATS3 | 37,551 | 37,402 | 36.97% (36.67–37.26) | 5,663 | 5,123 | 27.54% (26.90–28.19) | 2,564,502 | 29.95% (29.92–29.98) |
| ATS4 | 48,742 | 48,723 | 48.15% (47.85–48.46) | 9,517 | 9,568 | 51.44% (50.72–52.16) | 3,782,094 | 44.16% (44.13–44.20) |
| ATS5 | 8,487 | 7,837 | 7.75% (7.58–7.91) | 2,725 | 3,140 | 16.88% (16.35–17.43) | 1,450,417 | 16.94% (16.91–16.96) |
| Total | 101,180 | 101,180 | 18,601 | 18,601 | 8,563,615 | |||
Both healthdirect populations have been age‐standardized to the NSW population of ED attendances (July 2008–June 30 2012).
Hospital Admissions and Deaths within Twenty‐Four Hours of the Call
In the 24 hours following the healthdirect call, 21.7 percent (95 percent CI 21.5–22.0) of patients presenting at an ED in accordance with a healthdirect disposition were admitted to hospital, significantly higher than the 18.6 percent (95 percent CI 18.0–19.2) of self‐referred patients who presented to an ED. As shown in Table 5, rates of hospitalization by ATS level on ED arrival did not significantly differ between compliant attenders and self‐referred groups, except for patients triaged as ATS 5, who were significantly more likely to be hospitalized in the compliant attender group (5.7 percent, 95 percent CI 5.2–6.2) than in the self‐referred group (4.0 percent, 95 percent CI 3.3–4.8).
Table 5.
Hospital Admission Records with Twenty‐Four Hours of the Healthdirect Helpline Call for Compliant Attenders and Self‐Referred Attenders, by Australasian Triage Scale on ED Presentation
| ED Triage | Healthdirect‐Compliant Attenders (Jan. 1, 2009–Dec. 31, 2012) | Healthdirect Self‐Referred Attenders (Jan. 1, 2009–Dec. 31, 2012) | ||
|---|---|---|---|---|
| N Attended ED | N Admitted (%) | N Attended ED | N Admitted (%) | |
| ATS1 | 77 | 58 (75.3%, 95% CI 64.2–84.4)) | 21 | 17 (81.0%, 95% CI 58.1–94.6) |
| ATS2 | 6,323 | 3,268 (51.7%, 95% CI 50.4–52.9) | 675 | 377 (55.9%, 95% CI 52.0–59.6) |
| ATS3 | 37,551 | 11,406 (30.4%, 95% CI 29.9–30.8) | 5,663 | 1,709 (30.2%, 95% CI 29.0–31.4) |
| ATS4 | 48,742 | 6,789 (13.9%, 95% CI 13.6–14.2) | 9,517 | 1,245 (13.1%, 95% CI 12.4–13.8) |
| ATS5 | 8,487 | 482 (5.7%, 95% CI 5.2–6.2) | 2,725 | 110 (4.0%, 95% CI 3.3–4.8) |
| Total | 101,180 | 22,003 (21.7%, 95% CI 21.5–22.0) | 18,601 | 3,458 (18.6%, 95% CI 18.0–19.2) |
There were a total of 15 deaths (0.015 percent) recorded in compliant attenders in the 24 hours following a healthdirect call, with 80 percent of these in patients aged 50 and above. Fewer than five deaths (<0.027 percent) were recorded in patients who self‐referred to the ED, all of which were in patients aged 50 and above. Further details concerning deaths cannot be provided due to privacy considerations.
Discussion
Principal Findings
In this population‐based data linkage study, we found that just over two‐thirds (66.5 percent) of patients were compliant with dispositions to attend ED immediately given by the healthdirect telephone triage service. The great majority (94.2 percent) of these compliant patients attended within 4 hours of the call. The telephone triage disposition received is only one factor in a patient's decision to attend ED. Controlling for other patient and call‐related factors, there was a significantly lower likelihood of compliance where the caller resided in a remote area or had made a greater number of calls to the helpline in the previous 6 months. Among patients receiving a low‐urgency disposition, 6.2 percent self‐referred to the ED within 24 hours, with 46.6 percent of these presenting at an ED within 4 hours of the call. Residents in more remote areas were significantly less likely to self‐refer, and significantly more self‐referrals occurred in patients who reported their original intention was to attend ED, or calls where another person was calling on behalf of the patient. Patients aged 18 to 34 years were less likely to comply with a disposition to attend ED immediately and more likely to self‐refer to ED when compared to the youngest patients. After age adjustment, healthdirect‐compliant patients who attended ED included a significantly lower proportion of the least urgent (ATS 5) triage category (7.8 percent), and a significantly higher proportion of presentations triaged as ATS 3 (medical attention within 30 minutes) than the general NSW ED patient population. The proportion of ATS 5 presentations in the self‐referred group (16.9 percent) did not differ from the general NSW ED population. While 4.0 percent of the self‐referred group were triaged as ATS 2 on arrival, this was significantly lower than the 8.4 percent of the NSW ED population who were triaged as ATS 2. Hospitalization rates within 24 hours of the call were significantly lower in self‐referred attenders (18.6 percent) than those who attended compliant with healthdirect dispositions (21.7 percent).
Strengths and Limitations
This study of an entire population permitted precise calculation of rates and estimation of predictors of compliance and self‐referral, although the predictors were limited to those contained in the administrative datasets. Interpretation of the caller's “original intention” should be treated with caution as this information could have been influenced by the disposition given. The question could have been asked either before or after the disposition had been stated, in a nonstandardized way. We do not know whether a prior healthdirect call was reported on presentation at ED or whether the report of this information may have influenced the resulting ATS level. The study only examined compliance and self‐referral in relation to EDs. Linkage of GP and other service data is required to assess compliance with helpline advice to self‐care or see a GP. False‐positive links (estimated at <0.1 percent) would have a minimal impact on the findings. However, some small rural EDs do not contribute data to the NSW ED data collection. The use of hospital inpatient as well as ED data to identify patients partially addressed this issue; however, some NSW callers, particularly those residing near state borders, may have attended interstate EDs that would not have been captured by the NSW dataset. These factors may have resulted in an underestimation of compliance and self‐referral rates in outer regional and more remote areas.
After‐hours GP triage commenced in mid‐2011, and there was no significant impact (p = .33) of year of call on compliance with dispositions to attend an ED. We know little about what prompts a referral from the after‐hours nurse to GP triage worker, but the clinical symptoms group were included in the regression models to control for varying likelihood of after‐hours GP referral based on clinical symptoms.
Comparisons with Other Studies
This study examined more than 1 million calls to the healthdirect helpline across an entire Australian state, including urban, rural, and remote locations. The next largest comparable study examined approximately 96,000 telephone triage calls, in the Calgary Health Region, Canada (De Coster et al. 2010). The 67.3 percent compliance with dispositions to attend ED immediately observed in major NSW cities is greater than the 52.3 percent compliance with a recommendation to “Go to ED” observed in Calgary (De Coster et al. 2010). Both studies used linked data methods and had the same definition of compliance.
In the current study, 9.2 percent of calls were referred to the after‐hours GP, and after controlling for other factors, compliance with an ED disposition given by an after‐hours nurse was marginally higher (67.4 percent) than the compliance with ED dispositions advised by an after‐hours GP (65.0 percent). In a U.S. study, compliance with pediatrician or nurse advice to seek emergency care was not significantly different (Lee et al. 2003); however, in the current study GP triage staff were only available after‐hours. Self‐referral rates in patients given low‐urgency dispositions after‐hours did not significantly differ between nurse and after‐hours GP triage staff.
In terms of patient factors, this study showed that children were most likely to comply with attend ED disposition, adults aged 18–44 years were least compliant, and adults over 55 years were more compliant than younger adults. This was consistent with a U.S. study that reported that patients over 45 years were more likely to comply with attend ED dispositions than younger adults (O'Connell et al. 2002). The same U.S. study found that patients with more than one call to the triage service were less likely to have hospital or physician records following a call, consistent with the current finding that a patient was less likely to be compliant if he or she was the subject of many prior calls. The finding that compliance is significantly more likely where the caller's initial intention matches the call disposition is expected, and it has been shown in previous studies (Munro et al. 2001; Niemann et al. 2004).
This study also confirmed previous research that self‐referrals present later to the ED than those given a disposition to attend (Foster, Jessopp, and Chakraborti 2003; Stewart et al. 2006). The rate of self‐referral (6.2 percent) in patients given low‐urgency dispositions in this study was lower than the 9.0 percent self‐referral rate reported at a single hospital in Western Australia (Sprivulis, Carey, and Rouse 2004), although in that study “nonurgent dispositions” were defined as those where medical care should be sought on the next day or later. In the current study, where “nonurgent dispositions” were defined as dispositions to seek care in 72 hours or later, the proportion of self‐referred patients triaged in the ED as the least urgent ATS 5 category (16.9 percent) was identical to the general population attending the ED.
Implications for Clinicians and Policymakers
This study provided evidence which can be used to assess the appropriateness of telephone triage dispositions. Patients who attended ED after being advised to do so were less than half as likely as the general population of ED attenders to be triaged to the least urgent category (ATS 5) and were significantly more likely to be classified into the more urgent categories ATS 3 and 4, implying low rates of over‐referral in healthdirect patients. The small percentage of healthdirect self‐referred patients who received higher ATS ratings on ED presentation may suggest a degree of under‐referral. However, not all of these patients would have been under‐referred; telephone triage dispositions are based only on reported symptoms, and symptom change over time is possible, particularly for the 30 percent of self‐referrals who presented between 12 and 24 hours after the call.
Two small Western Australian studies concluded that healthdirect helpline patients had similar levels of ED referral appropriateness as nonhealthdirect patients (Sprivulis, Carey, and Rouse 2004; Ng et al. 2012), and both were based in a single urban hospital. One study based its judgement of appropriateness on the similar distributions of triage categories between helpline callers who attended ED within 24 hours and ED attenders who had not called the helpline (Sprivulis, Carey, and Rouse 2004), thus failing to discriminate between healthdirect callers who were compliant with a disposition to attend ED and those who self‐referred after a low‐urgency disposition. The second study (Ng et al. 2012) defined appropriateness of referral to ED on the basis of subsequent patient management or outcomes (e.g., hospital admission, tests and procedures, death) and reported similar levels of appropriateness (~73 percent) in patients who self‐reported that they had been referred to ED by the healthdirect helpline and those who did not report referral by healthdirect or a GP. However, in the Ng et al. study, only around three‐quarters of patients who self‐reported a helpline referral could be identified in the healthdirect call data after data linkage, nor were the estimates age‐adjusted despite substantial age differences in the populations. In the present study, ATS triage category on ED presentation was used as the primary measure of helpline disposition appropriateness, as this outcome occurs closest in time to the telephone triage, and would be most relevant to the symptoms reported in that call. Patients who are untreated or not admitted do not necessary represent inappropriate ED presentations. However, administrative data have limited information on which to assess appropriateness, and application of different methods, such as simulated patient scenarios, may be better able to assess the appropriateness of telephone triage dispositions.
Future Research and Conclusions
This study did not assess the potential impact of the telephone triage helpline on ED overcrowding, a contentious issue in Australia (Nagree et al. 2013; Australian Medical Association 2014) and elsewhere (Lind 2015). Current evidence implicates access block (difficulty transferring admitted patients to inpatient beds), not a deluge of low‐urgency patients, as the main cause of ED overcrowding (Hughes 2003; Forero, McCarthy, and Hillman 2011). As only 5.9 percent of the 1,733,732 presentations made to NSW EDs during the study period (source: NSW ED data) were made in accordance with healthdirect helpline dispositions, and the helpline being accessed by just over 2 percent of the NSW population in a given year, the helpline has a limited impact on ED activity, when compared with the growth of general population attendances. However, this does not preclude other beneficial impacts of these services, such as referral to needed services; provision of reassurance, comfort and peace of mind to patients and their carers; and improved patient outcomes. Such benefits may be particularly important for people with limited access to health care, such as those living in rural and remote areas, who experience financial or other barriers to accessing health care, or who experience health emergencies out of hours where immediate medical or nursing advice is not otherwise available. Further analyses of linked data incorporating investigation of patient trajectories of care and outcomes, and analyses according to geography and indicators of disadvantage, will help to elucidate these issues.
Supporting information
Appendix SA1: Author Matrix.
Figure S1. Time from Healthdirect Helpline Call to Self‐Referred ED Presentation, by Australasian Triage Scale Categories on ED Presentation.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: The authors would like to thank all members of the Project Steering Group for their contributions. Thanks also to the Centre for Health Record Linkage for conducting the data linkage and the data custodians for providing the administrative data sets. The authors declare that (1) the organization that employs Louisa Jorm, Amy Gibson, Duong Tran, Deborah Randall and Alys Havard, (Centre for Big Data Research in Health, UNSW Australia) received a grant from Healthdirect Australia in order to conduct the analysis for the submitted work; (2) Amy Gibson, Deborah Randall, Duong Tran, Alys Havard and Louisa Jorm had no financial relationship with Healthdirect Australia outside of the submitted work in the 36 months prior to publication. Mary Byrne and Maureen Robinson are employees of Healthdirect Australia, and Anthony Lawler is a director of Healthdirect Australia. Mary Byrne, Maureen Robinson, and Anthony Lawler provided expert advice on the healthdirect helpline service and data, but they did not participate in data cleaning, data analysis, or selection of findings for publication; (3) the spouses, partners, or children of the authors have no financial relationships that may be relevant to the submitted work; and (4) during the course of this study, Anthony Lawler commenced the role of President of the Australasian College for Emergency Medicine, and this includes the role of chair of that organization's Board. An earlier version of the main findings of this paper has been presented at an international conference.
Disclaimer: None.
References
- Australasian College for Emergency Medicine . 2013. Policy on the Australasian Triage Scale. Melbourne: Australasian College for Emergency Medicine. [Google Scholar]
- Australian Bureau of Statistics . 2011. Socio‐Economic Indexes for Areas (SEIFA). B. Pink. Canberra: Commonwealth of Australia. [Google Scholar]
- Australian Bureau of Statistics . 2012. Australian Demographic Statistics, June 2012. Canberra: Australian Bureau of Statistics. [Google Scholar]
- Australian Bureau of Statistics . 2013. Regional Population Growth, Australia 2011–12. Canberra: Australian Bureau of Statistics. [Google Scholar]
- Australian Medical Association . 2014. AMA Position Statement: Call Centre Triage and Advice Services 2004. Revised 2014. Sydney: Australian Medical Association. [Google Scholar]
- Australian Population and Migrations Research Centre . 2015. ARIA (Accessibility/Remoteness Index of Australia). Adelaide: University of Adelaide. [Google Scholar]
- Campbell, J. L. , Fletcher E., Britten N., Green C., Holt T. A., Lattimer V., Richards D. A., Richards S. H., Salisbury C., Calitri R., Bowyer V., Chaplin K., Kandiyali R., Murdoch J., Roscoe J., Varley A., Warren F. C., and Taylor R. S.. 2014. “Telephone Triage for Management of Same‐Day Consultation Request in General Practice (the ESTEEM Trial): A Cluster‐Randomised Controlled Trial and Cost‐Consequence Analysis.” Lancet 384: 1859–68. [DOI] [PubMed] [Google Scholar]
- De Coster, C. , Quan H., Elford R., Li B., Mazzei L., and Zimmer S.. 2010. “Follow‐Through after Calling a Nurse Telephone Advice Line: A Population‐Based Study.” Family Practice 27: 271–78. [DOI] [PubMed] [Google Scholar]
- Forero, R. , McCarthy S. M., and Hillman K.. 2011. “Access Block and Emergency Department Overcrowding.” Critical Care 15: 216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foster, J. , Jessopp L., and Chakraborti S.. 2003. “Do Callers to NHS Direct Follow the Advice to Attend an Accident and Emergency Department?” Emergency Medicine Journal 20: 285–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graber, D. , Ardagh M., O'Donovan P., and St George I.. 2003. “A Telephone Advice Line Does Not Decrease the Number of Presentations to Christchurch Emergency Department, but Does Decrease the Number of Phone Callers Seeking Advice.” New Zealand Medical Journal 116 (1177): U495. [PubMed] [Google Scholar]
- Hansen, E. H. , and Hunskaar S.. 2011. “Understanding of and Adherence to Advice after Telephone Counselling by Nurse: A Survey among Callers to a Primary Emergency Out‐of‐Hours Service in Norway.” Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine 19 (48). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Healthdirect Australia . 2015. Annual Report‐ Business Highlights 2014–2015. Sydney: Healthdirect Australia. [Google Scholar]
- Hughes, G. 2003. “Giving Emergency Advice Over the Telephone: It Can Be Done Safely and Consistently.” New Zealand Medical Journal 116 (1177): U495. [PubMed] [Google Scholar]
- Kempe, A. , Luberti A. A., Hertz A. R., Sherman H. B., Amin D., Dempsey C., Chandramouli V., MacKenzie T., and Hegarty T. W.. 2001. “Delivery of Pediatric After‐Hours Care by Call Centers: A Multicentre Study of Parental Perceptions and Compliance.” Pediatrics 108 (6). [DOI] [PubMed] [Google Scholar]
- Kempe, A. , Bunik M., Ellis J., Magid D., Hegarty T., Dickinson L. M., and Steiner J. F.. 2006. “How Safe Is Triage by an After‐Hours Telephone Call Center?” Pediatrics 118 (2): 457–63. [DOI] [PubMed] [Google Scholar]
- Labarere, J. , Torres J. P., Francois P., Fourny M., Argento P., Gensburger X., and Methonnex P.. 2003. “Patient Compliance with Medical Advice Given by Telephone.” American Journal of Emergency Medicine 21: 288–92. [DOI] [PubMed] [Google Scholar]
- Lee, T. J. , Baraff L. J., Wall S. P., Guzy J., Johnson D., and Woo H.. 2003. “Parental Compliance with After Hours Telephone Triage Advice: Nurse Advice Service Versus on‐Call Pediatricians.” Clinical Pediatrics 42: 613–19. [DOI] [PubMed] [Google Scholar]
- Lind, S. 2015. Rise in A&E Attendances Caused by NHS 111, Emergency Medicine Leader Claims. Pulse London: Cogora Limited. [Google Scholar]
- Munro, J. , Nicholl J., O'Cathain A., Knowles E., and Morgan A.. 2001. Evaluation of NHS Direct First Wave Sites: Final Report of the Phase 1 Research. Sheffield: University of Sheffield. [Google Scholar]
- Nagree, Y. , Camarda V. J., Fatovich D. M., Cameron P. A., Dey I., Gosbell A. D., McCarthy S. M., and Mountain D.. 2013. “Quantifying the Proportion of General Practice and Low‐Acuity Patients in the Emergency Department.” Medical Journal of Australia 198: 612–15. [DOI] [PubMed] [Google Scholar]
- Navratil‐Strawn, J. L. , Hawkins K., Wells T. S., Ozminkowki R. J., Hawkins‐Koch J., Chan H., Hartley S. K., Migliori R. J., and Yeh C. S.. 2014. “Listening to the Nurse Pays off: An Integrated Nurse HealthLine Programme Was Associated with Significant Cost Savings.” Journal of Nursing Management 22: 837–47. [DOI] [PubMed] [Google Scholar]
- Ng, J. Y. , Fatovich D. M., Turner V. F., Wurmel J. A., Skevington S. A., and Phillips M. R.. 2012. “Appropriateness of Healthdirect Referrals to the Emergency Department Compared with Self‐Referrals and GP Referrals.” Medical Journal of Australia 197: 498–502. [DOI] [PubMed] [Google Scholar]
- Niemann, S. , Meer A., Simonin C., and Abel T.. 2004. “Medical Telephone Triage and Subsequent Patient Behaviour: How Do They Compare?” Swiss Medical Weekly 134: 126–31. [DOI] [PubMed] [Google Scholar]
- O'Cathain, A. , Knowles E., Turner J., and Nicholl J.. 2014. “Acceptability of NHS 111 the Telephone Service for Urgent Health Care: Cross Sectional Postal Survey of Users’ Views.” Family Practice 31 (2): 193–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Connell, J. M. , Towles W., Yin M., and Malakar C. L.. 2002. “Patient Decision Making: Use of and Adherence to Telephone‐Based Nurse Triage Recommendations.” Medical Decision Making 22: 309–17. [DOI] [PubMed] [Google Scholar]
- Scarfone, R. J. , Luberti A. A., and Mistry R. D.. 2004. “Outcomes of Children Referred to an Emergency Department by an After‐Hours Call Centre.” Pediatric Emergency Care 20 (6): 367–72. [DOI] [PubMed] [Google Scholar]
- Sprivulis, P. , Carey M., and Rouse I.. 2004. “Compliance with Advice and Appropriateness of Emergency Presentation Following Contact with the HealthDirect Telephone Triage Service.” Emergency Medicine Australasia 16: 35–40. [DOI] [PubMed] [Google Scholar]
- Stewart, B. , Fairhurst R., Markland J., and Marzouk O.. 2006. “Review of Calls to NHS Direct Related to Attendance in the Paediatric Emergency Department.” Emergency Medicine Journal 23: 911–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix SA1: Author Matrix.
Figure S1. Time from Healthdirect Helpline Call to Self‐Referred ED Presentation, by Australasian Triage Scale Categories on ED Presentation.


