Abstract
Background
Parental presence in the neonatal intensive care unit (NICU) is essential for families to participate in infant care and prepare them to transition from hospital to home. Nurses are the principal caregivers in the NICU. The nurse work environment may influence whether parents spend time with their hospitalized infants.
Purpose
To examine the relationship between the NICU work environment and parental presence in the NICU using a national data set.
Methods
We conducted a cross-sectional, observational study of a national sample of 104 NICUs, where 6060 nurses reported on 15,233 infants cared for. Secondary analysis was used to examine associations between the Practice Environment Scale of the Nursing Work Index (PES-NWI) (subscale items and with a composite measure) and the proportion of parents who were present during the nurses’ shift.
Results
Parents of 60% (SD = 9.7%) of infants were present during the nurses’ shift. The PES-NWI composite score and 2 domains—Nurse Participation in Hospital Affairs and Manager Leadership and Support—were significant predictors of parental presence. A 1 SD higher score in the composite or either subscale was associated with 2.5% more parents being present.
Implications for Practice
Parental presence in the NICU is significantly associated with better nurse work environments. NICU practices may be enhanced through enhanced leadership and professional opportunities for nurse managers and staff.
Implications for Research
Future work may benefit from qualitative work with parents to illuminate their experiences with nursing leaders and nurse-led interventions in the NICU and design and testing of interventions to improve the NICU work environment.
Keywords: infant, intensive care, neonatal, nurse staffing, nurse work environment, parental presence, Practice Environment Scale of the Nursing Work Index
Parental presence in the neonatal intensive care unit (NICU) is a building block of family-centered care (FCC), which has been associated with improved patient outcomes.1,2 Ensuring that families are partners in the healthcare of their family member is a priority of numerous national agencies and mandated by the Affordable Care Act.3 Families, especially mothers, may participate in crucial activities such as skin-to-skin care (SSC). Such care may be used to achieve thermoregulation in preterm infants and to initiate the production of human milk.4–6 There is a need for understanding the basis for parental presence to have successful FCC in the NICU.
For many new parents, the unexpected experience of their infant being admitted to the NICU invokes feelings of despair, powerlessness, and fear due to uncertainty of their infants’ condition.2,7–9 When parents, especially mothers, relinquish control of their infant to nurses and other healthcare providers in the NICU, they feel deeply disconnected and stressed because of their inability to alleviate any pain or discomfort from their infant.2,7,9,10 Given these challenges, parents still desire to be in the NICU so that they can participate in infant care, communicate with the healthcare team, and be present during clinical procedures.1,2,11–14
Since the 1960s, researchers have attempted to define necessary clinical conditions to achieve optimal FCC through parental presence in the NICU.2,15 During this period, significant medical, technical, and pharmaceutical advances have improved infant outcomes dramatically.16 This progress has resulted in a clinical environment where providers, especially nurses, have had to master the complexities of working in a NICU as “intensivists,” focusing on the safe utilization and interpretation of technology in addition to caring for infants and families.17–19 A shift toward FCC has evolved from a medical model to one where nurses are experts, act as gatekeepers, and attempt to integrate families into the care of their infant to leverage the strengths of families and support, empowerment, and communicate with parents as they learn to be the primary caregivers for their vulnerable infant while in the NICU.19
Nurses are the principal caregivers in the NICU. When parents are present, they are able to partner with nurses and actively participate in the care of their infant. A systematic review of the literature has shown that NICU nursing interventions that promote parental participation in infant care alleviate parental experiences of stress, anxiety, and loss of control.20 Parental presence during invasive procedures and routine healthcare rounds has several effects. It results in improved opportunities for communication with the healthcare team and improved reports of satisfaction for both parents and providers.21,22 Nurses are essential to guiding and empowering new parents toward successful transition as primary caregivers through family-integrated care, a model that operationalizes the principles of FCC. Outcomes have shown that parents who are able to directly partner with the multidisciplinary NICU team develop parenting skills and greater confidence and are better emotionally prepared to care for their infants when discharged home with their infant.23,24 A nurse–family relationship is important throughout the entire hospitalization to encourage support and learning in preparation for a smooth transition from hospital to home.
The organizational context within the NICU, specifically the work environment, may be a contributing factor to the establishment of the nurse–family relationship and whether parents spend time with their hospitalized infants. Evidence has linked the work environment to patient outcomes in infant populations.25–27 In addition, evidence that hospital systems and nursing delivery strategies affect neonatal outcomes has been established. NICU nurses bring to the clinical environment multiple qualities (eg, experience, leadership, NICU specialty certification, continued education, commitment, and caring); however, studies have linked level of education as an important characteristic of staff nurses on patient outcomes.
Hospitals with better work environments, lower nurse-to-patient ratios, and higher proportions of nurses with a baccalaureate-level education or higher are associated with improved infant outcomes.25,26, 28,29 However, less is known about how NICU work environments may be linked to outcomes related to family/parent presence. The nurse–patient relationship is unique in the NICU because nursing care of the infant is shared between the parent and the nursing staff.
A Canadian study of 9 NICUs linked variations in the work environment to reduced nursing care activities, due to time constraints, and a lower nurse-assessed quality of care.30 NICU work environments, with sufficiently staffed and adequately trained nurses, are needed to optimize evidence-based practice and infant outcomes that depend on a family member’s presence in the NICU.13,31, 32 Nurses have been described as the gatekeepers of infant care in the NICU, and FCC is largely dependent on the ability of the nurse to have the time, training, and expertise to support families when they are present in the unit.1 The relationship between NICU nursing characteristics and parental presence has not been explored.
The authors advanced several hypotheses: (1) hospitals foster the optimal contribution of NICU nurses’ work by having better work environments; (2) higher acuity-adjusted nurse staffing ratios positively affect nurses’ contributions; and (3) exploration of the relationship of the nurse work environment with family presence in the NICU. The optimal nurse contribution was conceptualized as achieving a higher fraction of parents present in the NICU to create opportunities for nurses to prepare families for infant care and ultimate hospital discharge.
The objective of this study was to examine the associations between the NICU nurse work environment and nurse reports of parental presence utilizing novel data from a large national sample of NICUs in the United States. This study utilizes data on nurses’ actual activities with parents to determine whether certain NICU nursing characteristics foster parental presence. This body of work fits into the larger body of evidence linking organizational nursing factors to healthcare quality in the United States.
METHODS
The survey data originated from the parent study, “Acuity-Adjusted Staffing, Nurse Practice Environments and NICU Outcomes,” funded by the Robert Wood Johnson Foundation Interdisciplinary Nursing Quality Research Initiative program. Nurse survey data were collected in March 2008 from 104 NICUs nationally. All NICUs were members of the Vermont Oxford Network ([VON]; www.vtoxford.org), a voluntary collaborative dedicated to the quality and safety of care for newborns and their families. NICUs were recruited from all US VON NICUs. In 2008, the US VON contained 578 hospitals representing approximately 65% of NICUs and 80% of all very low birth-weight infants born in the United States.26 Institutional review board (IRB) approval was obtained for this project from the University of Pennsylvania. The parent study received IRB approval both from the University of Pennsylvania and the Rutgers University.
DESIGN
A cross-sectional study of secondary data was used to examine the outcomes of interest: the presence of parents in the NICU and the nurses’ work with parents.
SETTING AND PARTICIPANTS
A sample of 104 NICUs nationally participated in the parent study data.33 These NICUs were broadly representative of all US VON NICUs and represented 18% of the VON members in 2008. The sample had disproportionately more not-for-profit teaching hospitals and children’s hospitals than total VON members. Hospitals with Magnet designation comprised one-third of the study sample, compared with approximately a quarter of the VON. NICUs were classified into the 3 VON levels: level A (restriction to minor ventilation, no surgery); B (major surgery); and C (cardiac surgery and extracorporeal membrane oxygenation).34 These correspond to high level II, III, and IV units in the American Academy of Pediatrics classification.35
A Web survey of all registered nurses who worked at least 16 hours per week and had been employed at least 3 months was used to collect the parent data. The response rate was 77% (n = 6060 nurses reported on the care of 15,233 infants). In addition, nurse managers provided data about the size of each NICU (total nursing staff and number of beds).
MEASURES AND INSTRUMENTS
Organizational Nursing Factors
Practice Environment
The Practice Environment Scale of the Nursing Work Index (PES-NWI) was used to measure the degree to which certain aspects of a professional practice environment, including staffing, were present in the nurse’s current job.36,37 Multiple studies have demonstrated the predictive and discriminant validity of this 31-item, 4-point Likert-type instrument.36,38–40 Each item asks the nurses to indicate the extent to which the work environment characteristic is present in their job. The item response choices are “strongly disagree,” “disagree,” “agree,” and “strongly agree.” The PES-NWI items are categorized into 5 subscales that measure the following work environment domains: Nurse Participation in Hospital Affairs; Nursing Foundations for Quality of Care; Nurse Manager Ability, Leadership, and Support of Nurses; Staffing and Resource Adequacy; and Collegial Nurse–Physician Relations. A score of 2.5 is the midpoint between agree and disagree, and a score of 3 or greater indicates agreement that the element is present in the job.37 In addition to an analysis using subscales of the PES-NWI, the average of the subscale items was used as a composite measure and in regression models.
Parental Presence and Care Activities Measures
Parental presence was measured using the nurse respondents’ answer “Yes” to the question “Were parents of this infant(s) present on your last shift?” Nurse responses that indicated that parents were present “less than half the shift” and “more than half the shift” were combined into a single variable indicating that parents were present at some time during the nurse’s last shift worked. Hence, the numerator was the total number of infants on the unit whose parents were present at any time during the nurse’s shift. The denominator was the total number of infants who were assigned to all nurses on the unit.
In the survey, nurses also identified activities performed with parents that required nursing care “beyond what would have been required had the family not been present.” Care needs that nurses and parents worked on together to address were identified. However, examples of care activities were not defined for all items in the survey and were left open to the interpretation by the individual nurse respondent. Nurses categorized these care activities into the following 8 categories: special language or cultural needs, complex social situations (eg, drug use or addiction, housing), limited parenting skills, breast-feeding support, emotional support related to infant’s rapid deterioration or termination of life support, routine beside teaching and communicating, parent teaching beyond routine bedside teaching, and formal teaching or training session (eg, cardiopulmonary resuscitation, monitors).
Data Analysis
Descriptive statistics were used to describe the hospital sample and NICU nursing characteristics, parental presence, and care activities with parents. Bivariate relationships were assessed between the independent variables—nurse practice environment subscales and composite, and the dependent variable—parental presence. Independent variables with correlation with the dependent variable at P < .05 were analyzed in a bivariate linear regression model. The dependent variable was the percentage of infants whose parents were present in each NICU. Continuous practice environment variables were standardized for ease of interpretation. To explore the possibility that less stressful environments in lower-level NICUs may account for the comfort of parents being in the NICU, we tested NICU level as a control variable in the regression model. Two dummy variables were included. NICU level B was the reference category. The statistical significance level was P < .05 for a 2-tailed test. Analyses were conducted using Stata version 14.0.41
RESULTS
The majority of NICUs (57%) in the sample provided midlevel care (level B) (Table 1). The sample had a larger proportion of higher-level (level C) NICUs and fewer low-level (level A) NICUs than all US VON NICUs. The sample units were larger than average US NICUs (mean = 41 vs 22 beds); comparisons with US distribution are not shown in the tabular form. The average staff size was 75 full-time registered nurses. In terms of staffing, each nurse cared for an average of 2 infants per shift. Most infants were lower acuity; 62% were level 1 or 2. The hospital characteristics of the sample have been published previously.5 The majority of nurse survey respondents (69%) worked their last shift on a weekday.
TABLE 1.
NICU and Infant Sample Characteristics
| NICU (N = 104)a | % |
|---|---|
| NICU level of careb | |
| A | 14 |
| B | 57 |
| C | 29 |
| Number of beds, mean (SD) | 41 (20) |
| Registered nurses, mean (SD) | 75 (42) |
| Infant acuity distribution (n = 15,191)c | |
| Level 1 continuing care | 33 |
| Level 2 requiring intermediate care | 29 |
| Level 3 requiring intensive care | 26 |
| Level 4 requiring multisystem support | 8 |
| Level 5 requiring complex critical care | 4 |
Abbreviation: NICU, neonatal intensive care unit.
Results have been reported in Hallowell et al.5
Level refers to level of clinical care: A, minor ventilation only; B, minor surgery; C, cardiac surgery and extracorporeal membrane oxygenation.
Results have been reported in Rogowski et al.42
This table was reproduced with permission from the rightsholders. © 2015 Wiley Periodicals Inc.
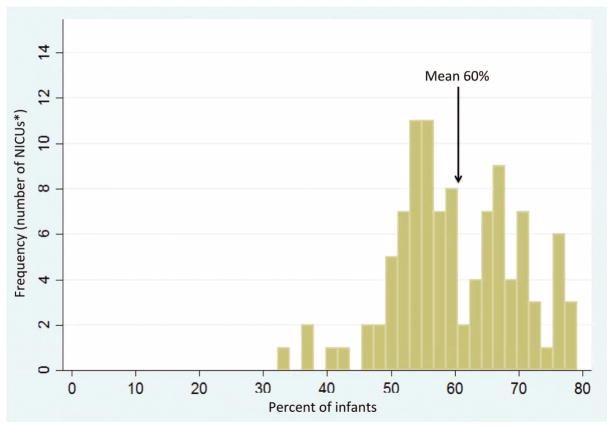
On average, 60% of infants’ parents were present during the shift (SD = 9.7%). This ranged from 33% to 79% across units (Figure 1). The percentage of parents present was similar across days, nights, and weekends shifts. Parents of 46% of infants required additional time from the nurse (Table 2). At least 1 additional nursing care activity was provided to parents of 40% of the infant sample, 35% of parents present required 2 activities, and 26% of required 3 or more activities.
FIGURE 1.
Percentage of infants whose parents were present during the nurses’ shift.
TABLE 2.
Frequency of Parental Presence and Nursing Care Activities Provided With Parents
| Infants (N = 15,233) | n (%) |
|---|---|
| Parents were present at least half the nurses’ shift or more | 8989 (59) |
| Parents who were present and required extra nursing care | 6828 (45) |
| Nursing care activities provided with parentsa | |
| Routine beside teaching and communicating with families | 5509 (36) |
| Breastfeeding support | 2004 (13) |
| Parent teaching beyond routine bedside teaching | 1602 (11) |
| Parents have limited parenting skills | 1421 (9) |
| A complex social situation (eg, drug use or addiction, housing) | 837 (5) |
| Parents have special language or cultural needs | 823 (5) |
| Emotional support to parents due to infant’s rapid deterioration or termination of life support | 458 (3) |
| Needs formal teaching or training session | 292 (2) |
Activities performed with infants whose parents were reported to require extra nursing care. Adapted with permission from Hallowell et al., Characteristics of the NICU Work Environment Associated with Breastfeeding Support. Advances in Neonatal Nursing, Vol. 14, Iss. 4. Copyright © 2014 by The National Association of Neonatal Nurses.
One-third of the parents (36%) present required the nurse to provide routine bedside teaching and communication. Nonroutine teaching (11%) and special training sessions (2%) were activities that also required additional nursing time. As reported in prior studies, breastfeeding support was provided to 13% of parents present.5 Nine percent of parents required additional time with nurses due to limited parenting skills. Language, cultural needs, and complex social situations each required additional nursing time for 5% of the infants.
The practice environment was highly rated in the NICU sample, where the average PES-NWI composite score was more than 3.0 (mean = 3.06), with a range of 2.42 to 3.97.
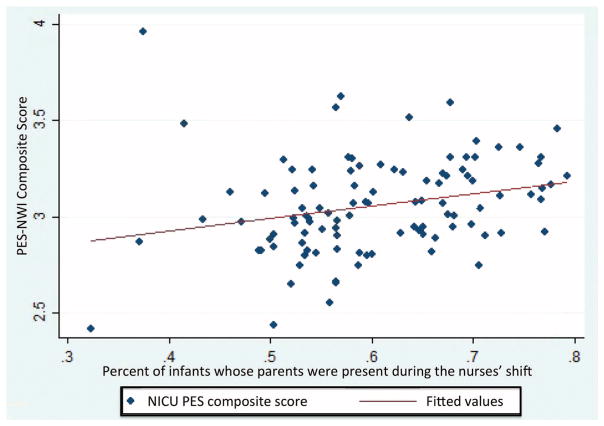
Modest correlations were observed between parental presence and the PES-NWI subscales “Nurse Participation in Hospital Affairs” (r = 0.24; P < .02) and “Nurse Manager Ability, Leadership, and Support of Nurses” (r = 0.23; P < .02), as well as the composite PES-NWI (r = 0.25; P < .01). The latter relationship is depicted in the scatterplot, in which the correlation between the composite PES-NWI and parental presence is shown by the upward sloping line in the scatterplot (Figure 2). A significant correlation was also observed between parental presence and level A NICUs (r = 0.21; P < .03).
FIGURE 2.
Scatterplot of the PES-NWI composite score and infants whose parents were present during the nurses’ shift. NICU indicates neonatal intensive care unit; PES-NWI, Practice Environment Scale of the Nursing Work Index.
In bivariate regression models, a 1 SD higher PES-NWI “Nurse Participation in Hospital Affairs” sub-scale score was associated with 2.3% higher percentage of parents present (P < .02). A 1 SD higher PES-NWI “Nurse Manager Ability, Leadership, and Support of Nurses” subscale score was associated with a 2.2% higher percentage of parents present (P < .02), and the PES-NWI composite score was associated with a 2.5% higher percentage of parents present (P < .01). A 1 SD higher proportion of level A NICUs was associated with a 2% higher percentage of parents present (P < .03). A multiple linear model was used to test the association with the level A NICU variable and the PES-NWI composite score; significance was associated only with the PES-NWI composite and a 2.1% higher percentage of parental presence (P < .03). A 1 SD higher PES-NWI “Staffing and Resource Adequacy” subscale score was associated with a 1.8% increase in parental presence; however, this was marginally significant (P < .06). The addition of NICU level to the regression model did not change the results. The NICU-level dummy variables were not significant.
DISCUSSION
The motivation for this study was to examine the extent to which parents are present in the NICU and to understand characteristics of this clinical setting that may have facilitated parental presence at the infant bedside. Admission of an infant to the NICU is traumatic for many parents, who often feel overwhelmed. Parents may encounter conditions that hamper their ability to have access to their infants during all phases of the NICU admission (acute critical phase, stabilizing and discharge phases).43 Multiple barriers exist that may limit parental visitation in the NICU. These barriers may be physical and related to hospital or unit design (eg, a long distance between the NICU and maternity wards), related to the physical design of the NICUs (eg, open bay/multiple crib room design may jeopardize confidentiality of patient information), health related (eg, mother recovering from childbirth), related to other responsibilities (eg, need to care of the home), or related to poor socioeconomic situations (eg, inability to access transportation).2,14 In addition, NICU characteristics such as a nonwelcoming or family-friendly environment (eg, noisy with alarms, staff, other visitors, lack of privacy), lack of information from providers, and poor treatment from nursing staff (eg, having to ask permission to care for their child) have been described to deter parental presence.14
Nurses are the main caregivers in the NICU and are in the best position to foster parental presence, which is essential for the provision of FCC. We found that most NICU infants’ parents are present, but this varies considerably across NICUs. Given the desirability of parental presence, one question is how to foster a greater parental presence in units with few parents present. We found that NICUs with positive nurse work environments had higher numbers of parents present. The elements of the work environment that seem most important to fostering the presence of parents are having an effective nurse manager and sufficient staff and resources. An effective manager can communicate and emphasize the importance of FCC, which requires the parent’s presence.
With sufficient staff, the nurses have time to work with parents, respond to their concerns, and explain the infant’s health status and care needs. Three-fourths of parents required additional nursing time to complete a range of activities. The principal activity was routine bedside teaching, required by 4 of 5 parents, followed by breastfeeding support, needed by a third of parents, and nonroutine bedside teaching, required by a quarter of parents. Our results suggest that additional nursing time was primarily devoted to helping parents learn basic parenting skills (eg, SSC/holding of their infant, diapering, and feeding) necessary to achieve competency, foster parental well-being, facilitate independence, and instill confidence as caretakers.43 These concepts are vitally important when nurses prepare families for the infant’s discharge to home.
How can better work environments be achieved? One way is through Magnet accreditation of the institution based on meeting standards for nursing excellence. Empirical evidence has demonstrated that Magnet hospitals have better work environments, that becoming a Magnet hospital improves work environments, and that very low birth-weight infants have better health outcomes in Magnet hospital NICU.26 The evidence suggests that in Magnet hospitals, the possibility of FCC with all of its advantages is enhanced. If leadership is the basis for Magnet success, our study identified this effect via the work environment at the nursing unit level.
The NICU work environment is necessarily focused on nursing care that is technology focused and oriented to efficiency.44 Nurses in our study reported that basic bedside teaching accounted for the majority of additional nursing time spent with parents. Our results, showing that parents are present consistently across day, night, and weekend shifts, indicate that nurses have opportunities to work with them across the breadth of daily care activities. Nurse managers may consider an open-door visitation policy and unrestricted access to the NICU as a strategy to foster full parent participation and partnerships with nurses and clinical staff.45 A shift in the NICU culture toward partnerships with parents would allow parents to participate in many daily activities, which contributes to the development of daily care routines for the infant and also includes parents in clinical rounds, nursing reports, infant admission, and infant emergencies.2
Summary of Recommendations for Practice and Research.
| What we know: |
|
| What needs to be studied: |
|
| What we can do today: |
|
LIMITATIONS
The use of secondary data limits causal inference. Future research could test an intervention that improves the work environment to determine whether this increases parental presence. The results from this sample may not generalize to all NICUs. The nominal categories provided on the survey to report parent activities may have limited capturing the true range of activities that nurses do with parents. This study did not examine variations in parental presence by hospital Magnet status or the length of time parents spent in the NICU. Magnet status, a hospital-wide designation, may influence our outcome of interest, but the emphasis here was the nursing unit environment. Time is an essential element of nurse–parent support and rapport. Future studies may focus on these topics.
CONCLUSION
Nursing can play an important role in fostering the presence of parents in NICUs, which is important for FCC. Positive nurse work environments are an essential foundation for a welcoming milieu in the NICU. The prominent elements of these environments are effective nurse leaders and sufficient staffing. Nurses are perfectly positioned to foster the bond between parents and infants.
What this study adds.
Highlights how positive nurse work environments are an essential foundation for a welcoming milieu in the NICU.
Effective nurse leaders and nursing leadership in the NICU are essential to improvements in family outcomes.
Acknowledgments
Supported in part by the 2014 Sigma Theta Tau International Small Grants Award, which has been completed (Hallowell, PI; Lake, Mentor). This study was initiated during the primary author’s postdoctoral study, which was funded by the National Institute of Nursing Research of the National Institutes of Health award number T32NR007104 “Advanced Training in Nursing Outcomes Research” (Aiken, PI) at the Center for Health Outcomes and Policy Research, University of Pennsylvania. The primary data used in the data set were funded through the Robert Wood Johnson Foundation Interdisciplinary Nursing Quality Research Initiative grant “Acuity-Adjusted Staffing, Nurse Practice Environments and NICU Outcomes” (Lake, PI).
Footnotes
Institution where the work occurred: Center for Health Outcomes and Policy Research, University of Pennsylvania School of Nursing, and Villanova University College of Nursing.
The authors declare no conflicts of interest.
References
- 1.Gooding JS, Cooper LG, Blaine AI, Franck LS, Howse JL, Berns SD. Family support and family-centered care in the neonatal intensive care unit: origins, advances, impact. Semin Perinatol. 2011;35(1):20–28. doi: 10.1053/j.semperi.2010.10.004. [DOI] [PubMed] [Google Scholar]
- 2.Griffin T. A family-centered “visitation” policy in the neonatal intensive care unit that welcomes parents as partners. J Perinat Neonatal Nurs. 2013;27(2):160–165. doi: 10.1097/JPN.0b013e3182907f26. quiz 166–167. [DOI] [PubMed] [Google Scholar]
- 3.National Quality Forum. [Accessed July 18, 2016];Person- and family-centered care. http://www.qualityforum.org/Topics/Person-_and_Family-Centered_Care.aspx.
- 4.Charpak N, Ruiz JG, Zupan J, et al. Kangaroo mother care: 25 years after. Acta Paediatr. 2005;94(5):514–522. doi: 10.1111/j.1651-2227.2005.tb01930.x. [DOI] [PubMed] [Google Scholar]
- 5.Hallowell SG, Spatz DL, Hanlon AL, Rogowski JA, Lake ET. Characteristics of the NICU work environment associated with breastfeeding support [published online ahead of print July 31, 2014] Adv Neonatal Care. 2014;14(4):290–300. doi: 10.1097/ANC.0000000000000102. doi:10.1097-ANC.0000000000000102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Spatz DL. Ten steps for promoting and protecting breastfeeding for vulnerable infants. J Perinat Neonatal Nurs. 2004;18(4):385–396. doi: 10.1097/00005237-200410000-00009. [DOI] [PubMed] [Google Scholar]
- 7.Bernaix LW, Schmidt CA, Jamerson PA, Seiter L, Smith J. The NICU experience of lactation and its relationship to family management style. MCN Am J Matern Child Nurs. 2006;31(2):95–100. doi: 10.1097/00005721-200603000-00008. [DOI] [PubMed] [Google Scholar]
- 8.Galarza-Winton ME, Dicky T, O’Leary L, Lee SK, O’Brien K. Implementing family-integrated care in the NICU: educating nurses. Adv Neonatal Care. 2013;13(5):335–340. doi: 10.1097/ANC.0b013e3182a14cde. [DOI] [PubMed] [Google Scholar]
- 9.Thomas LM. The changing role of parents in neonatal care: a historical review. Neonatal Netw. 2008;27(2):91–100. doi: 10.1891/0730-0832.27.2.91. [DOI] [PubMed] [Google Scholar]
- 10.Boucher CA, Brazal PM, Graham-Certosini C, Carnaghan-Sherrard K. Mothers’ breastfeeding experiences in the NICU. Neonatal Netw. 2011;30(1):21–28. doi: 10.1891/0730-0832.30.1.21. [DOI] [PubMed] [Google Scholar]
- 11.Bailey SM, Hendricks-Muñoz KD, Mally P. Parental influence on clinical management during neonatal intensive care: a survey of US neo-natologists. J Matern Fetal Neonatal Med. 2013;26(12):1239–1244. doi: 10.3109/14767058.2013.776531. [DOI] [PubMed] [Google Scholar]
- 12.Beesley SJ, Hopkins RO, Francis L, et al. Let them in: family presence during intensive care unit procedures. Ann Am Thoracic Soc. 2016;13(7):1155–1159. doi: 10.1513/AnnalsATS.201511-754OI. [DOI] [PubMed] [Google Scholar]
- 13.Cooper LG, Gooding JS, Gallagher J, Sternesky L, Ledsky R, Berns SD. Impact of a family-centered care initiative on NICU care, staff and families. J Perinatol. 2007;27(S2):S32–S37. doi: 10.1038/sj.jp.7211840. [DOI] [PubMed] [Google Scholar]
- 14.Wigert H, Berg M, Hellström A-L. Parental presence when their child is in neonatal intensive care. Scand J Caring Sci. 2010;24(1):139–146. doi: 10.1111/j.1471-6712.2009.00697.x. [DOI] [PubMed] [Google Scholar]
- 15.Maree C, Downes F. Trends in family-centered care in neonatal intensive care. J Perinat Neonatal Nurs. 2016;30(3):265–269. doi: 10.1097/JPN.0000000000000202. [DOI] [PubMed] [Google Scholar]
- 16.Horbar JD, Edwards EM, Greenberg LT, et al. Variation in performance of neonatal intensive care units in the United States. JAMA Pediatr. 2017;171(3):e164396. doi: 10.1001/jamapediatrics.2016.4396. [DOI] [PubMed] [Google Scholar]
- 17.Cricco-Lizza R. The need to nurse the nurse: emotional labor in neonatal intensive care. Qual Health Res. 2014;24(5):615–628. doi: 10.1177/1049732314528810. [DOI] [PubMed] [Google Scholar]
- 18.Cricco-Lizza R. Rooting for the breast: breastfeeding promotion in the NICU. MCN Am J Matern Child Nurs. 2009;34(6):356–364. doi: 10.1097/01.NMC.0000363684.43186.fe. [DOI] [PubMed] [Google Scholar]
- 19.Nyqvist KH, Engvall G. Parents as their infant’s primary caregivers in a neonatal intensive care unit. J Pediatr Nurs. 2009;24(2):153–163. doi: 10.1016/j.pedn.2008.07.006. [DOI] [PubMed] [Google Scholar]
- 20.Obeidat HM, Bond EA, Callister LC. The parental experience of having an infant in the newborn intensive care unit. J Perinat Educ. 2009;18(3):23–29. doi: 10.1624/105812409X461199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Duran CR, Oman KS, Abel JJ, Koziel VM, Szymanski D. Attitudes toward and beliefs about family presence: a survey of healthcare providers, patients’ families, and patients. Am J Crit Care. 2007;16(3):270–279. quiz 280; discussion 281–282. [PubMed] [Google Scholar]
- 22.Grzyb MJ, Coo H, Rühland L, Dow K. Views of parents and health-care providers regarding parental presence at bedside rounds in a neonatal intensive care unit. J Perinatol. 2014;34(2):143–148. doi: 10.1038/jp.2013.144. [DOI] [PubMed] [Google Scholar]
- 23.Bracht M, O’Leary L, Lee SK, O’Brien K. Implementing family-integrated care in the NICU: a parent education and support program. Adv Neonatal Care. 2013;13(2):115–126. doi: 10.1097/ANC.0b013e318285fb5b. [DOI] [PubMed] [Google Scholar]
- 24.O’Brien K, Bracht M, Macdonell K, et al. A pilot cohort analytic study of family integrated care in a Canadian neonatal intensive care unit. BMC Pregnancy Childbirth. 2013;13(1):S12. doi: 10.1186/1471-2393-13-S1-S12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hallowell S, Rogowski JA, Spatz DL, Hanlon AL, Kenny M, Lake ET. Factors associated with infant feeding of human milk at discharge from neonatal intensive care: cross-sectional analysis of nurse survey and infant outcomes data. Int J Nurs Stud. 2016;53:190–203. doi: 10.1016/j.ijnurstu.2015.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lake ET, Staiger D, Horbar J, et al. Association between hospital recognition for nursing excellence and outcomes of very low-birth-weight infants. JAMA. 2012;307(16):1709–1716. doi: 10.1001/jama.2012.504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rogowski JA, Staiger D, Patrick T, Horbar J, Kenny M, Lake ET. Nurse staffing and NICU infection rates. JAMA Pediatr. 2013;167(5):444–450. doi: 10.1001/jamapediatrics.2013.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cimiotti JP, Haas J, Saiman L, Larson EL. Impact of staffing on bloodstream infections in the neonatal intensive care unit. Arch Pediatr Adolescent Med. 2006;160(8):832–836. doi: 10.1001/archpedi.160.8.832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lake ET, Staiger D, Horbar J, Kenny MJ, Patrick T, Rogowski JA. Disparities in perinatal quality outcomes for very low birth weight infants in neonatal intensive care. Health Serv Res. 2015;50(2):374–397. doi: 10.1111/1475-6773.12225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rochefort CM, Clarke SP. Nurses’ work environments, care rationing, job outcomes, and quality of care on neonatal units. J Adv Nurs. 2010;66(10):2213–2224. doi: 10.1111/j.1365-2648.2010.05376.x. [DOI] [PubMed] [Google Scholar]
- 31.Cockcroft S. How can family centred care be improved to meet the needs of parents with a premature baby in neonatal intensive care? J Neonatal Nurs. 2012;18(3):105–110. [Google Scholar]
- 32.Higman W, Shaw K. Nurses’ understanding about the delivery of family centered care in the neonatal unit. J Neonatal Nurs. 2008;14(6):193–198. [Google Scholar]
- 33.Lake ET, Patrick T, Rogowski J, et al. The three Es: how neonatal staff nurses’ education, experience, and environments affect infant outcomes. J Obstet Gynecol Neonatal Nurs. 2010;39(suppl):S97–S98. [Google Scholar]
- 34.Vermont Oxford Network. Vermont Oxford Network Database Manual of Operations for Infants Born in 2008. Burlington, VT: Vermont Oxford Network; 2008. Release 12.1. [Google Scholar]
- 35.American Academy of Pediatrics Committee on Fetus and Newborn. Levels of neonatal care. Pediatrics. 2012;130(3):587–597. doi: 10.1542/peds.2012-1999. [DOI] [PubMed] [Google Scholar]
- 36.Friese CR, Lake ET, Aiken LH, Silber JH, Sochalski J. Hospital nurse practice environments and outcomes for surgical oncology patients. Health Serv Res. 2008;43(4):1145–1163. doi: 10.1111/j.1475-6773.2007.00825.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lake ET. Development of the Practice Environment Scale of the Nursing Work Index. Res Nurs Health. 2002;25(3):176–188. doi: 10.1002/nur.10032. [DOI] [PubMed] [Google Scholar]
- 38.Aiken LH, Clarke SP, Sloane DM, Lake ET, Cheny T. Effects of hospital care environment on patient mortality and nurse outcomes. J Nurs Adm. 2008;38(5):223–229. doi: 10.1097/01.NNA.0000312773.42352.d7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kutney-Lee A, Lake ET, Aiken LH. Development of the hospital nurse surveillance capacity profile. Res Nurs Health. 2009;32(32):217–228. doi: 10.1002/nur.20316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lake ET, Friese CR. Variations in nursing practice environments: relation to staffing and hospital characteristics. Nurs Res. 2006;55(1):1–9. doi: 10.1097/00006199-200601000-00001. [DOI] [PubMed] [Google Scholar]
- 41.StataCorp. Stata Statistical Software. College Station, TX: StataCorp LP; 2015. Release 14. [Google Scholar]
- 42.Rogowski J, Staiger D, Patrick T, Horbar J, Kenny M, Lake E. Nurse staffing in neonatal intensive care units in the United States. Res Nurs Health. 2015;38:333–341. doi: 10.1002/nur.21674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fegran L, Fagermoen MS, Helseth S. Development of parent–nurse relationships in neonatal intensive care units—from closeness to detachment. J Adv Nurs. 2008;64(4):363–371. doi: 10.1111/j.1365-2648.2008.04777.x. [DOI] [PubMed] [Google Scholar]
- 44.Cricco-Lizza R. Everyday nursing practice values in the NICU and their reflection on breastfeeding promotion. Qual Health Res. 2011;21(3):339–409. doi: 10.1177/1049732310379239. [DOI] [PubMed] [Google Scholar]
- 45.Moore KAC, Coker K, DuBuisson AB, Swett B, Edwards WH. Implementing potentially better practices for improving family-centered care in neonatal intensive care units: successes and challenges. Pediatrics. 2003;111(suppl E1):e450–e460. [PubMed] [Google Scholar]