Abstract
Background
Pediatric patients undergoing liver transplant are at significant risk for bleeding and thrombotic complications due to the complex nature of rebalanced hemostasis in patients with liver disease.
Methods/Objectives
We reviewed records of 92 pediatric liver and multivisceral transplant cases at Duke University Medical Center between January 2009 and December 2015. The goal was to define the nature and incidence of bleeding and thrombotic complications in this cohort and define potential risk factors.
Results
There were 24 major bleeding events in 19 transplants (incidence 20.7%) and 30 thrombotic events in 23 transplants (incidence 25%). Five of the 10 re-transplantations were for vascular thrombotic complications. Thirty-day mortality was 4.9%, and 3 of these 4 deaths were due to vascular thrombosis. No bleeding events led to re-transplantation or mortality. Prophylactic aspirin was associated with decreased risk of thrombosis without increased bleeding. Prophylactic heparin did not increase bleeding risk. Laboratory assays predicted events poorly, apparently failing to capture the nuanced and dynamic interplay between pro- and anti-coagulant factors in the post-transplant patient.
Conclusions
Both bleeding and thrombosis are frequent in this population, but only thrombotic complications contributed to re-transplantation and mortality. A standardized approach to coagulation testing and anti-thrombotic therapy may be useful in predicting and reducing adverse outcomes. Alternative approaches to monitoring hemostasis need to be prospectively investigated in this complex patient population.
Keywords: Bleeding, thrombosis, pediatric, liver transplant, hemostasis, anticoagulation
Introduction
Pediatric patients undergoing liver transplant are at risk for significant bleeding and thrombotic complications. Studies in both pediatric and adult cohorts estimate an incidence of thrombotic events in up to 26% of cases.1–9 Hepatic artery and portal vein thrombosis are reported at rates of 5–15% in pediatric cohorts, which is 3–4 times the incidence in adults.2,5–11 Bleeding estimates are harder to quantify given variability in the definition of major bleeding, but range from approximately 5–9%.12–14 The contribution of bleeding to morbidity is difficult to quantify, but thrombotic complications are known to reduce graft survival and contribute significantly to adverse outcomes, with mortality rates approaching 50% in those with hepatic artery thrombosis.6,9,15,16
The frequency and severity of bleeding and thrombotic complications in the liver transplant patient reflects the complicated balance of pro- and anti-coagulant factors in patients with liver disease. The liver plays a key role in hemostasis, because it synthesizes the majority of proteins involved in clot stabilization and fibrinolysis. Although many of these factors are altered by liver disease, under normal circumstances these pro- and anti-thrombotic factors roughly balance each other out, leading to a relatively stable hemostatic equilibrium. This concept has become known as “rebalanced hemostasis” in newly emerging literature on liver disease and transplantation.17–19
This precarious state of delicately balanced pro and anti-coagulant factors is easily perturbed. Any invasive procedure or insult can disrupt the equilibrium. The extraordinary changes in vascular integrity, blood flow, and perfusion that occur with liver transplant can tip the pendulum even further. These disturbances may lead either to bleeding or thrombosis, but the direction in which this balance tips is not well predicted by our current laboratory tools.20–23 Despite prolongation of standard coagulation assays, such as the prothrombin time (PT) and activated partial thromboplastin time (aPTT), there is growing evidence that a pro-thrombotic state exists in many pediatric patients for up to several weeks post-transplant.24–26
Due in part to a dearth of prognostic assays to accurately predict bleeding and thrombotic risk, there is no consensus on optimal post-transplant medical management.15,27 In addition to defining the incidence and nature of bleeding and thrombotic complications in pediatric patients undergoing liver and multivisceral transplant at Duke University Medical Center, this project also sought to identify patient, laboratory or management factors that were associated with an increase in these complications.
Methods
Study Design and Setting
We identified pediatric patients (birth to 18 years) who had undergone liver or multivisceral (combined liver, pancreas and small bowel) transplant at Duke University Medical Center between January 1st, 2009 and December 31st, 2015.
Using the electronic medical record (EMR), we abstracted information from 30 days pre- to 90 days post-transplant (defined as the peri-transplant period). EMR information was cross-referenced with documentation from the Organ Transplant Tracking Record and the UnetSM online database developed by UNOS (United Network for Organ Sharing). We collected clinical information including adverse outcomes. We also collected data on blood products and hemostatic agents given between 30 days pre- and 30 days post-transplant.
We recorded the following clinical lab values during the peri-transplant period: hemoglobin, platelet count, PT/INR, aPTT, fibrinogen, D-dimer, Anti-thrombin activity, Protein C activity, Protein S activity, rotational thromboelastometry (ROTEM), thromboelastography (TEG), creatinine, aspartate transaminase (AST), alanine transaminase (ALT), direct bilirubin, and indirect bilirubin. This study was approved by the Duke University Institutional Review Board (Pro00067233) with a waiver of informed consent and HIPAA authorization.
Outcomes and Definitions
Thrombotic events were defined as any documented thrombus by imaging or clinical diagnosis made by direct observation during a surgical procedure. This included both venous and arterial thromboembolic events. Patients were screened for hepatic thrombosis regularly with liver Doppler ultrasound during the first week post-operatively, with confirmatory imaging based on identified clinical or imaging concerns. Major bleeding events were defined as surgical bleeding requiring re-operation, central nervous system (CNS) bleeding, or anatomic bleeding (bleeding with identifiable hematoma requiring transfusion but not requiring surgical intervention). Intra-operative blood loss resulting in a >3g/dl drop in hemoglobin occurred in 78% of cases. Therefore, we did not include this definition as a major bleeding event for subsequent analyses.
Statistical Analysis
Data were entered into a RedCap Database and analyzed using a statistical software package (SAS, Cary, NC) with the assistance of statistical support from the Duke Clinical Research Institute. Categorical variables were summarized as counts and percentages and continuous variables as median with minimum and maximum. Potential predictive risk factors of interest for bleeding and thrombosis were similarly summarized by event (bleeding or thrombosis) or no event, and with odds ratios with 95% confidence intervals using univariable logistic regression. Due to the rarity of liver transplant in the pediatric population, the sample size used was the largest feasible and included all of the transplant cases during the defined time period. The sample size was not large enough to compensate for multiple comparisons in the analysis due to the limitations on sample size.
Results
Cohort Demographics
There were 92 transplants (in 82 patients) from January 2009 through December 2015. Patient demographics and indications for transplant are detailed in Table 1. Patients in the “Other” category included patients with acute hepatic failure or cirrhosis without identifiable etiology. Two patients were also included in the cohort who had been transplanted before the study period and required re-transplantation.
Table 1.
Cohort Demographics
| Characteristic | All Patients (N=82) |
|---|---|
|
| |
| Male Gender | 47 (57.3%) |
|
| |
| Race/Ethnicity | |
| White | 34/82 (41.5%) |
| Black or African American | 25/82 (30.5%) |
| Hispanic, Latino, or Spanish Origin | 13/82 (15.9%) |
| Asian | 4/82 (4.9%) |
| Other | 6/82 (7.3%) |
|
| |
| Age (months) | 15.5 (1.0–214.0)* |
|
| |
| Weight at Initial Transplant (kg) | 8.5 (3.2–100.2)* |
|
| |
| Height at Initial Transplant (cm) | 71.0 (45.0–175.3)* |
|
| |
| PELD Score** | 22.0 (4.0–44.0)* |
|
| |
| Indication for Initial Transplant | |
| Congenital/Primary Liver | 39/82 (47.6%) |
| Mechanical/Obstructive or due to Intestinal Failure | 12/82 (14.6%) |
| Malignant | 8/82 (9.8%) |
| Metabolic | 5/82 (6.1%) |
| Hematologic | 4/82 (4.9%) |
| Infectious | 4/82 (4.9%) |
| Other | 8/82 (9.8%) |
| Failure of Prior Transplant (pre-2009) | 2/82 (2.4%) |
= Median (range)
= Other than Status 1A or 1B. The PELD score stands for pediatric end stage liver disease score and is a numeric disease severity scoring system used for patients under age of 12 years. This takes into account the patient’s serum bilirubin, serum albumin, PT/INR, patient age < 12 months, and growth failure. The score is correlated with prognosis and likelihood of death within a certain time period. It is used by UNOS to allocate organs. The MELD score is similar but only uses serum bilirubin, serum creatinine and PT/INR. MELD score is used in patients > 12 years.
Transplant characteristics and outcomes
Transplant characteristics are given in Table 2. Just over 10% of cases were multivisceral transplants. Nearly a quarter of cases (22.8%) required a repeat operation for a bleeding or thrombotic complication. Within the follow-up period, there were 10 re-transplantations across 8 separate recipients, with 2 patients requiring a third transplant. Three additional patients were listed for re-transplantation but did not survive to receive a new organ. Five of these ten re-transplant procedures were for vascular thrombosis. All thrombotic events leading to re-transplantation were hepatic artery thrombosis or combined hepatic artery and portal vein thrombosis, and all occurred within 30 days of initial transplant (Table 2).
Table 2.
Transplant Characteristics and Outcomes
| Characteristic | All Transplants (N=92) |
|---|---|
| Type of Transplant | |
| Whole Liver | 45/92 (48.9%) |
| Partial Liver | 37/92 (40.2%) |
| Multivisceral | 10/92 (10.9%) |
|
| |
| Use of Conduit | 21/92 (22.8%) |
|
| |
| Donor to Recipient Weight Ratio | 1.5 (0.5–21.8)* |
|
| |
| Donor to Recipient Height Ratio | 1.2 (0.7–25.5)* |
|
| |
| Warm Ischemic Time (minutes) | 45.0 (20.0–82.0)* |
|
| |
| Cold Ischemic Time (minutes) | 347.5 (58.6–633.0)* |
|
| |
| Length of Hospitalization (days) | 21.5 (6.0–189.0)* |
|
| |
| Length of ICU Stay (days) | 8.0 (2.0–129.0)* |
|
| |
| Repeat Operation for Bleeding or Thrombotic Complication | 21/92 (22.8%) |
|
| |
| Listed for Re-Transplantation | 13/92 (14.1%) |
|
| |
| Survival to Re-Transplantation | 10/92 (10.9%) (2 were for 3rd transplant) |
|
| |
| Indication for Re-Transplantation | N = 10 |
|
| |
| Vascular Thrombosis** | 5/10 (50.0%) |
| Acute Rejection | 4/10 (40.0%) |
| Biliary Obstruction and Diffuse Strictures | 1/10 (10.0%) |
|
| |
| Mortality Data (30-day) | N = 82 Patients |
|
| |
| Deceased | 4/82 (4.9%) |
|
| |
| Mortality Due to Vascular Thrombosis | 3/82 (3.7%) |
= Median (range)
= All HAT or HAT+PVT, all isolated liver transplant recipients
HAT = Hepatic Artery Thrombosis
PVT = Portal Vein Thrombosis
Overall survival in the cohort was 90.2% with a median follow-up time of 3.6 years (0.67–7.42 years). Four patients died within 30 days of transplant, for a 30-day mortality of 4.9%. Three of these four transplant-related deaths were due to vascular thrombosis. All 3 patients had both hepatic artery and portal vein thromboses leading to graft failure and all died within 8 days of transplant. The fourth patient died from complications of adenoviral pneumonia. The remaining patient deaths beyond 30 days were from infection, anoxia, cardiorespiratory arrest, and recurrent hepatocellular carcinoma (Table 2).
Bleeding and Thrombotic Complications
Overall in our cohort, there were 24 bleeding events in 19 transplants (incidence of 20.7%) (Table 3). The majority of bleeding events were surgical (79.2%) requiring a repeat operation. There were 3 CNS bleeding events, and although these contributed to morbidity, none led directly to patient death. The majority of major bleeding events occurred within the first 7 days post-transplant (62.5%, N=15 events).
Table 3.
Bleeding Complications
| All Transplants (N=92) | |||
|---|---|---|---|
|
| |||
| Total Number of Bleeding Events | 24 events (in 19 transplants) | ||
|
| |||
| Cases with Bleeding Event | 19/92 (20.7%) | ||
|
| |||
| Cases with > 1 Bleeding Event | 4/92 (4.3%) | ||
|
| |||
| Bleeding by Transplant Type | |||
| Whole Liver | 8/45 (17.8%) | ||
| Partial Liver | 8/37 (21.6%) | ||
| Multivisceral | 3/10 (30%) | ||
|
| |||
| Type of Bleeding Events | |||
| Surgical | 19/92 (20.7%) | ||
| CNS | 3/92 (3.3%) | ||
| Anatomic* | 2/92 (2.2%) | ||
| > 3g/dl hemoglobin drop** | 94 events in 72 transplants (excluded) | ||
|
| |||
| Timing of Bleeding | |||
|
| |||
| Type of Bleed | Days 0–7 Post-Op (N = 15 events) | Days 8– 30 Post-Op (N = 5 events) | 31+ Days Post-Op (N = 4 events) |
|
| |||
| Surgical | 11 events (5 W, 6 P) | 4 events (2 W, 1 P, 1 MV) | 4 events (1 P, 3 MV) |
|
| |||
| CNS | 3 events (1 W, 1 P, 1 MV) | 0 events | 0 events |
|
| |||
| Anatomic | 1 event (1 W) | 1 event (1 W) | 0 events |
= Anatomic signifies bleeding with identifiable hematoma requiring transfusion but not requiring surgical intervention
= All cases with drop in hemoglobin requiring transfusion but no other intervention. This was excluded in final analyses.
W = Whole Liver Transplant
P = Partial Liver Transplant
MV = Multivisceral Transplant
There were 30 thrombotic events in 23 transplants in our cohort (incidence of 25%) (Table 4). Hepatic artery thrombosis (HAT) was the most common thrombotic event (occurring in 12% of transplants) and portal vein thrombosis (PVT) was also frequent (occurring in 8.7% of transplants). There were 3 transplants in which both hepatic artery and portal vein thrombosis occurred (3.3%). Other events included six deep vein thromboses, 3 thromboses of the inferior vena cava, one hepatic vein thrombus, and one arterial thrombus related to a central line. There were no CNS thrombotic events. The majority of thrombotic events occurred within the first 7 days post-transplant (70%, N=20 events). Five percent of transplants had more than 1 bleeding or thrombotic event and 12 percent of transplants had both.
Table 4.
Thrombotic Complications
| All Transplants (N=92) | |||
|---|---|---|---|
|
| |||
| Total Number of Thrombotic Events | 30 events (in 23 transplants) | ||
|
| |||
| Cases with Thrombotic Event | 23/92 (25.0%) | ||
|
| |||
| Cases with > 1 Thrombotic Event | 5/92 (5.4%) | ||
|
| |||
| Thrombosis by Transplant Type | |||
| Whole Liver | 14/45 (31.1%) | ||
| Partial Liver | 6/37 (16.2%) | ||
| Multivisceral | 3/10 (30.0%) | ||
|
| |||
| Type of Thrombotic Events | |||
| Hepatic artery thrombosis | 11/92 (12%) | ||
| Portal vein thrombosis | 8/92 (8.7%) | ||
| Deep vein thrombosis | 6/92 (6.5%) | ||
| Other* | 5/92 (5.4%) | ||
|
| |||
| Timing of Thrombosis | |||
|
| |||
| Type of Thrombosis | Days 0–7 Post-Op (N = 21 events) | Days 8–30 Post-Op (N = 7 events) | 31+ Days Post-Op (N = 2 events) |
|
| |||
| Hepatic Artery Thrombosis | 11 events (7 W, 4 P) | 0 events | 0 events |
|
| |||
| Portal Vein Thrombosis | 6 events (4 W, 2 P) | 1 events (1 P) | 1 event (1 P) |
|
| |||
| Deep Vein Thrombosis | 1 event (1 W) | 4 events (4W) | 1 event (1 W) |
|
| |||
| Other* | 3 events (2W, 1 MV) | 2 events (1W, 1 MV) | |
= Other includes hepatic vein thrombosis, inferior vena cava thrombosis, and femoral artery thrombosis
W = Whole Liver Transplant
P = Partial Liver Transplant
MV = Multivisceral Transplant
Practices and Outcomes by Year
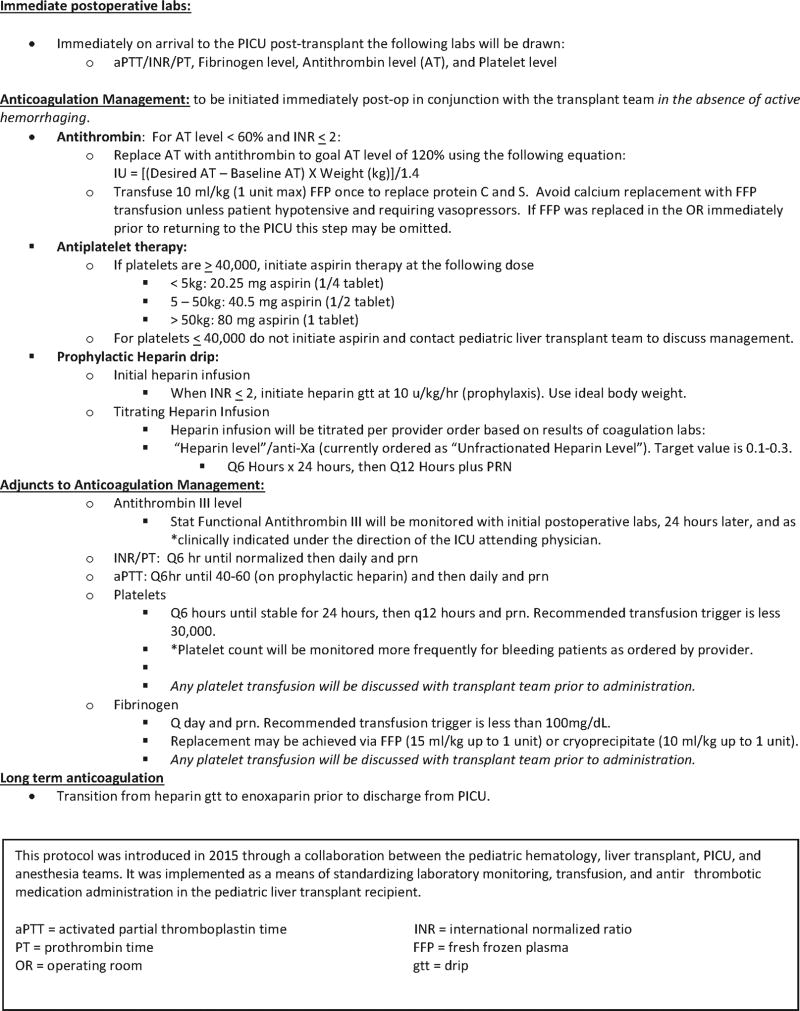
Differences in outcomes, cohort characteristics and anti-thrombotic management by year are shown in Supplemental Figure S1. Compared to earlier years, the cohort in more recent years is younger, there were more multivisceral transplants, and perhaps an overall sicker population, with a longer average ICU stay. Due to an increase in thrombotic events as well as re-transplantations related to thrombosis in 2013, clinical practice began to change to utilize increased heparin prophylaxis and antithrombin supplementation. This was officially adopted in a post-transplant hemostasis management protocol in 2015 (Figure 1).
Figure 1.
Duke Post-Transplant Hemostasis Management Protocol: This protocol was introduced in 2015 through a collaboration between the pediatric hematology, liver transplant, PICU, and anesthesia teams. It was implemented as a means of standardizing laboratory monitoring, transfusion, and anti-thrombotic medication administration in the pediatric liver transplant recipient.
Laboratory Testing
Complete blood count, fibrinogen and standard coagulation assays (PT/INR and aPTT) were measured frequently in all transplant recipients, with the majority having at least one measurement at each of the 12 time periods evaluated. Antithrombin activity was measured in 40.2% of transplants, with 95% of the measurements after 2012. Protein C and Protein S activity were only measured in 12% of transplants. Viscoelastic testing (with TEG or ROTEM) was performed in 26.1% of transplants and over half (14 cases, 58.3%) since 2013.
Transfusion
The median number of blood product transfusions (defined as 1 standard unit or 1 episode of weight-based transfusion) per transplant was 6.0 (0.0–43.0). The median estimated intra-operative blood loss per patient was 200ml (0–2600 ml) and the median estimated intra-operative blood loss as a percentage of total blood volume was 27.9% (range 0.0–391.0%). Since viscoelastic testing has been suggested to reduce transfusion requirements and improve outcomes in adult liver transplantation,28,29 we also looked separately at transfusions in the group that had this testing. The median number of transfusions per transplant (median 5.5 transfusions, range 1.0–42.0) and estimated intra-operative blood loss (255ml, range 0–2600ml) was similar, but blood loss as a percentage of total blood volume was higher at 57.0% (range 0.0–241.0%). By type of transplant, median number of transfusions was highest in the multivisceral group at 10.5 transfusions per transplant. This group also had the highest median number of pRBC transfusions post-operatively at 4.5 (compared to 1 in the whole liver and partial liver transplant groups).
Antithrombin supplementation was given in 17 cases (18.5%). All antithrombin supplementation was given within the first 72 hours of transplant. Recombinant Factor VIIa was given in 2 cases, one of whom received 14 separate doses prior to transplant for elevated INR. This patient had no bleeding or thrombotic complications before or after transplant. Cell saver was utilized in 2 cases.
Anti-Thrombotic Management
The majority of cases (92.4%) received post-operative anti-platelet prophylaxis with aspirin, typically for a period of about 3 months (Supplemental Table S1). Unfractionated heparin was used post-operatively in 48 transplants (52.2%), with 37 initiated for prophylaxis, and 11 for treatment after a pre- or post-transplant thrombotic event. Over 80% of patients were discharged on either an antiplatelet or anticoagulant medication, with aspirin utilized in most cases. Enoxaparin or warfarin, frequently in combination with aspirin, was used in some cases (Supplemental Table S1).
Factors Associated with Bleeding or Thrombosis
Univariable regression analysis was utilized to determine which clinical factors were associated with increased odds for bleeding or thrombosis (Table 5). We found several factors associated with increased odds for bleeding - including use of an arterial conduit for hepatic artery anastomosis, a history of prior gastrointestinal surgery, low platelet count and low fibrinogen. Lab values used for comparison were the minimum or maximum documented value during the pre-op, intra-op or post-operative periods. Somewhat counter intuitively, prophylactic aspirin was associated with a decreased risk of bleeding events (Table 5). This could be confounded that patients perceived to have increased risk for bleeding did not receive prophylactic aspirin. Factors associated with increased risk of thrombosis also included a history of prior gastrointestinal surgery and a low post-op fibrinogen. Use of prophylactic aspirin was associated with decreased thrombosis (Table 5). Stratification based on dose of aspirin was not performed, but all patients received weight-based dosing as outlined in Figure 1.
Table 5.
Factors Predictive of Bleeding or Thrombotic Complications
| Factors Associated with Bleeding | OR | p-value |
| Use of Arterial Conduit | 3.13 (1.05–9.34) | 0.0405 |
| Prior GI Surgery | 3.94 (1.05–14.69) | 0.0415 |
| Minimum Fibrinogen Post-Op (≤75mg/dl vs. >75mg/dl) | 7.96 (1.97–32.19) | 0.001 |
| Minimum Platelet Count Intra-Op (≤50k vs. >50k) | 4.51 (1.46–13.95) | 0.006 |
| Minimum Platelet Count Post-Op ((≤50k vs. >50k) | 8.01 (2.38–26.96) | 0.0002 |
| Use of Prophylactic Aspirin Post-Op | 0.04 (0.005– 0.37) | 0.0001 |
| Factors Associated with Thrombosis | OR | p-value |
| Minimum Fibrinogen Post-Op (≤75mg/dl vs. >75mg/dl) | 9.63 (2.24–41.39) | 0.0005 |
| Prior GI Surgery | 5.44 (1.48–20.01) | 0.0108 |
| Use of Prophylactic Aspirin Post-Op | 0.16 (0.03– 0.79) | 0.0131 |
Non-Predictive Factors for Bleeding or Thrombosis (all p > 0.05): Max INR (Pre, Intra, Post-Op), Minimum Antithrombin (<70%), EBL > 25% of Total Blood Volume, Intra-Op Transfusion, Use of Prophylactic Heparin Post-Op, Age, Weight, Transplant Type, Cold Ischemic Time, Donor to Recipient Weight Ratio
GI = gastrointestinal
Op = operative
EBL = estimated blood loss
We examined several other patient, surgical, and laboratory variables (Table 5) and found that none were predictive of bleeding or thrombosis. Intra-operative transfusions were not predictive of events and patients on prophylactic heparin were no more likely to require transfusion than those who were not anticoagulated (p = 0.531). However, the median number of transfusions given in the first 3 days post-transplant was higher in the transplants with bleeding (p < 0.001), those with thrombosis (p = 0.022), and in transplants with both types of event (p = 0.046).
Discussion
In our cohort of pediatric patients who underwent liver and multivisceral transplant, we observed a slightly higher incidence of both hepatic artery thrombosis (12%) and portal venous thrombosis (8.7%) compared to 1.35–16% in prior pediatric studies.2–6,8–13,30 The incidence of bleeding in our cohort was also higher than what has been reported previously (20.7% vs. 5–15%),11–13,30 but bleeding is reported inconsistently in prior cohorts and definitions vary, making the comparison difficult. Despite bleeding and thrombosis being similarly frequent events in our cohort, only thrombotic complications were associated with patient mortality. In contrast, bleeding tended to be more easily managed with transfusion or re-operation, with none requiring re-transplantation or resulting in patient death. Our 30-day survival rate was 95% and 1-year survival rate was 93%, which is in line with survival data from other studies.4,11,12,30,31 Of the four deaths within 30 days of transplant, three were due to vascular thrombosis.
Overall our cohort was similar to other recent studies in terms of demographics, surgical era, and indications for transplant, but there were some key differences that may account for our higher rates of thrombosis and bleeding (Supplemental Tables S2 and S3). Overall, our population was much younger, with a median age of 15.5 months vs. 1–7 years in most other groups.4,9,30,31 The smaller vessel sizes in our younger cohort might contribute to an increased thrombotic risk.4,5 Other pediatric cohorts included patients with similar transplant indications, but none we found included patients undergoing multivisceral transplant. Patients undergoing multivisceral transplant have often had multiple prior abdominal surgeries and other significant comorbidities, which may account for more complications post-operatively. Additionally, post-transplant medical management is highly variable,5,9,15,27,32 with most pediatric groups using some combination of anti-platelet and anticoagulant therapy but with different timing and length of therapy (Supplemental Table S3). These differences in cohort characteristics and management, as well as incomplete reporting of all thrombotic and bleeding complications, may account for some of the differences.
At our institution, there was an increase in vascular thrombotic complications that occurred in 2013, prompting an increase in use of post-operative anticoagulation. This ultimately became formalized in a post-transplant hemostasis management protocol adopted in early 2015 (Figure 1). This protocol defines transfusion parameters and laboratory monitoring. It also recommends routine use of unfractionated heparin prophylaxis and antithrombin supplementation. As might be anticipated, subsequent to an increase in use of post-transplant anticoagulation starting in 2013, there was an increase in bleeding events (from 10–30% to > 40%), but there were no re-transplantations or patient deaths related to bleeding. We have seen some decrease in major abdominal thrombosis (HAT and PVT), but have not seen a significant decrease in other thrombotic complications, possibly owing to a more complex and younger population. Along with the practice changes related to anticoagulation, there has been an introduction of alternative hemostasis testing with use of ROTEM and antithrombin activity testing. However, these tests are being utilized clinically without data to show that testing improves outcomes. In this cohort, these alternative tests were only used in a subset of the population, limiting our ability to comment on their utility. This highlights the importance of better understanding laboratory evaluation of coagulation in this population.
Along with this trend towards increased bleeding, we have seen an increase in transfusion. Transfusion during liver transplant in adults has been associated with many adverse outcomes and in general, many centers are moving towards minimizing transfusion in these patients.28,33–35 Multiple prior studies have shown negative consequences of excessive transfusion. Transfusion of pRBCs intra-operatively is a predictor of post-operative mortality in liver transplantation,35,36 transfusion of FFP has been associated with increased incidence of hepatic artery thrombosis,7,15 and platelet transfusion is also associated with poor outcomes.28 In this cohort, a higher median number of transfusions in the first 3 days post-operatively was associated with both bleeding and thrombotic complications. The best thresholds for transfusion are not known in this population, in part due to our inability to predict which patients will have bleeding. Improvements in our ability to predict patients at risk for thrombosis or bleeding may improve our ability to decrease transfusion exposure.
Our assessment of some of the commonly used coagulation assays, including PT/INR, aPTT, and fibrinogen levels, demonstrated that these tests were poorly predictive of adverse events. Abnormalities in the PT and aPTT reflect the deficiencies in procoagulant proteins’ production in patients with liver disease,22 but they do not take into account the delicate balance of pro- and anti-thrombotic factors seen in patients with liver disease23. The PT and INR do track with overall severity and prognosis of liver disease, but they do not necessarily predict adverse events.
Fibrinogen is an appealing marker to follow as a proxy for bleeding risk because patients with liver disease are known to have both hyperfibrinolysis37 and decreased fibrinolytic capacity.38 Optimal levels at which either bleeding risk or thrombotic risk increases are not known.22 In our cohort, a post-operative minimum fibrinogen of ≤ 75 mg/dL was associated with both increased bleeding and increased thrombosis. This makes it a poor predictive tool to distinguish risk of the 2 types of events. Additionally, the association of low fibrinogen with thrombosis may be due to confounding from transfusion to correct hypofibrinogenemia or it may simply be a reflection of a sicker patient population. It is also likely that these changes are dynamic with major differences in the fibrinolytic system during the anhepatic, reperfusion, and recovery phases of transplant.39
As might be expected in patients with severe thrombocytopenia, patients in our cohort with platelet counts < 50 × 10^9/L intra-operatively and post-operatively had more bleeding. Thrombocytopenia is multifactorial in patients with liver disease. Despite this quantitative platelet defect, patients in liver failure with platelet counts as low as 50 × 10^9/L have been shown to have adequate thrombin generation.40 This may offer some protection from spontaneous bleeding but may not be sufficient for major surgical intervention. The platelet count is only indicative of overall platelet numbers, but says nothing about platelet function or activity. Activation of platelets and release of endothelial factors may contribute significantly to at least local hypercoagulability, but we did not observe any relationship between the platelet counts and risk for thrombosis.
Because of the inability of standard coagulation assays to give an accurate picture of the rebalanced hemostasis present in patients with liver disease, there is a need for alternative assays to help guide management. Alternative and global hemostasis assays are being utilized with increasing frequency in the transplant setting to try to better capture the rebalanced hemostasis present in patients with liver disease.17,18,41–43 Recently, there have been several studies showing decreased transfusion requirements using viscoelastic testing during transplantation in adult patients undergoing liver transplant,29,44 which may justify addition of these laboratory assays to standard of care protocols or their use in determining which patients may require transfusion. Although global hemostasis assays may have the advantage of showing a more accurate picture of multiple components of hemostasis,22,45 these assays have not been validated in a pediatric population and we did not observe a benefit of this testing in our patients. Given that use of viscoelastic testing in our cohort was limited to single time testing intra-operatively in only a quarter of patients, we could not correlate abnormalities in these tests with bleeding or thrombotic events. Our retrospective review is limited in its ability to determine the predictive capability of different laboratory assays given the differences in timing and frequency of measurement, and given that the types of assays utilized has changed over time. Prospective studies validating the use of these tests in a pediatric population and in a pediatric transplant population are necessary to confirming their validity and applicability.
The complex nature of coagulation in pediatric liver transplant and the high stakes for patient outcomes motivate further inquiry into optimal post-transplant laboratory monitoring, anti-thrombotic, and hemostasis management. The complex balance and significant variation over time of pro- and anti-coagulant factors in these patients makes prediction and prevention of bleeding and thrombotic events difficult. This is consistent with the concept of rebalanced hemostasis, which stands in contrast to prior conceptions of increased bleeding risk in patients with abnormal routine coagulation studies.17–19 Hypercoagulability and thrombosis appear to be of even greater concern than bleeding, especially in pediatric recipients, because thrombosis can lead to significant morbidity and mortality. The apparent failure of standard coagulation assays to predict thrombotic events presents an important clinical challenge. Initiation of anticoagulation or antiplatelet therapy—or cessation of measures that might increase thrombotic risk—requires surveillance of the patient’s hemostatic state. An effective strategy for monitoring patients’ hemostatic state remains elusive.
Supplementary Material
Acknowledgments
Dr. Borst is supported by a Training Grant (T32 HL007057) from the NHLBI. Thank you to Tracy G. Spears, MS, RN and Lawrence H, Muhlbaier, PhD for their statistical support.
Abbreviations
- ALT
alanine transaminase
- aPTT
activated partial thromboplastin time
- AST
aspartate transaminase
- CNS
central nervous system
- EMR
electronic medical record
- FFP
fresh frozen plasma
- HAT
hepatic artery thrombosis
- INR
international normalized ratio
- MELD
model for end-stage liver disease
- PELD
pediatric end-stage liver disease
- pRBC
packed red blood cells
- PT
prothrombin time
- PVT
portal vein thrombosis
- ROTEM
rotational thromboelastometry
- TEG
thromboelastography
- UNOS
United Network for Organ Sharing
Footnotes
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Contribution: A.J. Borst designed the research, performed the research, analyzed the data and wrote the paper. D.L. Sudan contributed vital intellectual information and helped to write and edit the paper. L.A. Wang helped perform the research and helped to write and edit the paper. M.J. Neuss helped perform the research and helped to write and edit the paper. J.A. Rothman helped to write and edit the paper. T.L. Ortel helped to design the research, analyze the data, write and edit the paper.
- -
- -
- -
- -
References
- 1.Alexander BR, Antigua AD, Rosenberg AF, Caruso LJ, Voils SA, LeClaire AC. Chemoprophylaxis Use and Risk of Venous Thromboembolism and Death in Adult Patients following Orthotopic Liver Transplantation. J Pharm Pract. 2015:1–6. doi: 10.1177/0897190014566304. [DOI] [PubMed] [Google Scholar]
- 2.Ayala R, Martínez-López J, Cedena T, Bustelos R, Jimenez C, Moreno E, Ribera C. Recipient and donor thrombophilia and the risk of portal venous thrombosis and hepatic artery thrombosis in liver recipients. BMC Gastroenterol. 2011;11:130. doi: 10.1186/1471-230X-11-130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bustelos R, Ayala R, Martinez J, Martin MA, Toledo T, Grande S, Garfia C, Moreno A, Perez B, Meneu JC, Moreno E, Ribera C. Living donor liver transplantation: usefulness of hemostatic and prothrombotic screening in potential donors. Transplant Proc. 2009;41:3791–5. doi: 10.1016/j.transproceed.2009.06.214. [DOI] [PubMed] [Google Scholar]
- 4.Goss JA, Shackleton CR, McDiarmid SV, Maggard M, Swenson K, Seu P, Vargas J, Martin M, Ament M, Brill J, Harrison R, Busuttil RW. Long-term results of pediatric liver transplantation: an analysis of 569 transplants. Ann Surg. 1998;228:411–20. doi: 10.1097/00000658-199809000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Heffron TG, Pillen T, Welch D, Smallwood GA, Redd D, Romero R. Hepatic artery thrombosis in pediatric liver transplantation. Transplant Proc. 2003;35:1447–8. doi: 10.1016/s0041-1345(03)00459-7. [DOI] [PubMed] [Google Scholar]
- 6.Yilmaz A, Arikan C, Tumgor G, Kilic M, Aydogdu S. Vascular complications in living-related and deceased donation pediatric liver transplantation: single center’s experience from Turkey. Pediatr Transplant. 2007;11:160–4. doi: 10.1111/j.1399-3046.2006.00601.x. [DOI] [PubMed] [Google Scholar]
- 7.Hatano E, Terajima H, Yabe S, Asonuma K, Egawa H, Kiuchi T, Uemoto S, Inomata Y, Tanaka K, Yamaoka Y. Hepatic artery thrombosis in living related liver transplantation. Transplantation. 1997;64:1443–6. doi: 10.1097/00007890-199711270-00012. [DOI] [PubMed] [Google Scholar]
- 8.Duffy JP, Hong JC, Farmer DG, Ghobrial RM, Yersiz H, Hiatt JR, Busuttil RW. Vascular complications of orthotopic liver transplantation: experience in more than 4,200 patients. J Am Coll Surg. 2009;208:896–903. doi: 10.1016/j.jamcollsurg.2008.12.032. [DOI] [PubMed] [Google Scholar]
- 9.Ooi CY, Brandão LR, Zolpys L, De Angelis M, Drew W, Jones N, Ling SC, Fecteau A, Ng VL. Thrombotic events after pediatric liver transplantation. Pediatr Transplant. 2010;14:476–82. doi: 10.1111/j.1399-3046.2009.01252.x. [DOI] [PubMed] [Google Scholar]
- 10.Millis JM, Seaman DS, Piper JB, Alonso EM, Kelly S, Hackworth CA, Newell KA, Bruce DS, Woodle ES, Thistlethwaite JR, Whitington PF. Portal vein thrombosis and stenosis in pediatric liver transplantation. Transplantation. 1996;62:748–54. doi: 10.1097/00007890-199609270-00008. [DOI] [PubMed] [Google Scholar]
- 11.Moray G, Tezcaner T, Akdur A, Özçay F, Sezgin A, Kırnap M, Yıldırım S, Arslan G, Haberal M. Results of pediatric liver transplant: a single-center experience. Exp Clin Transplant Off J Middle East Soc Organ Transplant. 2015;13:59–63. [PubMed] [Google Scholar]
- 12.Broering DC, Kim J-S, Mueller T, Fischer L, Ganschow R, Bicak T, Mueller L, Hillert C, Wilms C, Hinrichs B, Helmke K, Pothmann W, Burdelski M, Rogiers X. One hundred thirty-two consecutive pediatric liver transplants without hospital mortality: lessons learned and outlook for the future. Ann Surg. 2004;240:1002–1012. doi: 10.1097/01.sla.0000146148.01586.72. discussion 1012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sanchez SE, Javid PJ, Lao OB, Dick AA, Perkins JD, Reyes JD, Horslen SP, Healey PJ, Sawin R. Hepatic artery thrombosis and liver malignancy in pediatric liver transplantation. J Pediatr Surg. 2012;47:1255–60. doi: 10.1016/j.jpedsurg.2012.03.035. [DOI] [PubMed] [Google Scholar]
- 14.Kaneko J, Sugawara Y, Tamura S, Togashi J, Matsui Y, Akamatsu N, Kishi Y, Makuuchi M. Coagulation and fibrinolytic profiles and appropriate use of heparin after living-donor liver transplantation. Clin Transplant. 2005;19:804–9. doi: 10.1111/j.1399-0012.2005.00425.x. [DOI] [PubMed] [Google Scholar]
- 15.Algarni AA, Mourad MM, Bramhall SR. Anticoagulation and antiplatelets as prophylaxis for hepatic artery thrombosis after liver transplantation. World J Hepatol. 2015;7:1238–43. doi: 10.4254/wjh.v7.i9.1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bekker J, Ploem S, de Jong KP. Early hepatic artery thrombosis after liver transplantation: a systematic review of the incidence, outcome and risk factors. Am J Transplant Off J Am Soc Transplant Am Soc Transpl Surg. 2009;9:746–57. doi: 10.1111/j.1600-6143.2008.02541.x. [DOI] [PubMed] [Google Scholar]
- 17.Lisman T, Porte RJ. Rebalanced hemostasis in patients with liver disease: evidence and clinical consequences. Blood. 2010;116:878–85. doi: 10.1182/blood-2010-02-261891. [DOI] [PubMed] [Google Scholar]
- 18.Raffini L, Witmer C. Pediatric transplantation: managing bleeding. J Thromb Haemost JTH. 2015;13:S362–369. doi: 10.1111/jth.12913. [DOI] [PubMed] [Google Scholar]
- 19.Saner FH, Gieseler RK, Akiz H, Canbay A, Görlinger K. Delicate Balance of Bleeding and Thrombosis in End-Stage Liver Disease and Liver Transplantation. Digestion. 2013;88:135–44. doi: 10.1159/000354400. [DOI] [PubMed] [Google Scholar]
- 20.Arshad F, Lisman T, Porte RJ. Hypercoagulability as a contributor to thrombotic complications in the liver transplant recipient. Liver Int Off J Int Assoc Study Liver. 2013;33:820–7. doi: 10.1111/liv.12140. [DOI] [PubMed] [Google Scholar]
- 21.Caldwell SH, Hoffman M, Lisman T, Macik BG, Northup PG, Reddy KR, Tripodi A, Sanyal AJ. Coagulation in Liver Disease Group. Coagulation disorders and hemostasis in liver disease: pathophysiology and critical assessment of current management. Hepatol. 2006;44:1039–46. doi: 10.1002/hep.21303. [DOI] [PubMed] [Google Scholar]
- 22.Northup PG, Caldwell SH. Coagulation in Liver Disease: A Guide for the Clinician. Clin Gastroenterol Hepatol. 2013;11:1064–74. doi: 10.1016/j.cgh.2013.02.026. [DOI] [PubMed] [Google Scholar]
- 23.Weeder PD, Porte RJ, Lisman T. Hemostasis in Liver Disease: Implications of New Concepts for Perioperative Management. Transfus Med Rev. 2014;28:107–13. doi: 10.1016/j.tmrv.2014.03.002. [DOI] [PubMed] [Google Scholar]
- 24.Mimuro J, Mizuta K, Kawano Y, Hishikawa S, Hamano A, Kashiwakura Y, Ishiwata A, Ohmori T, Madoiwa S, Kawarasaki H, Sakata Y. Impact of acute cellular rejection on coagulation and fibrinolysis biomarkers within the immediate post-operative period in pediatric liver transplantation. Pediatr Transplant. 2010;14:369–76. doi: 10.1111/j.1399-3046.2009.01248.x. [DOI] [PubMed] [Google Scholar]
- 25.Feltracco P, Barbieri S, Cillo U, Zanus G, Senzolo M, Ori C. Perioperative thrombotic complications in liver transplantation. World J Gastroenterol. 2015;21:8004–13. doi: 10.3748/wjg.v21.i26.8004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stine JG, Northup PG. Coagulopathy Before and After Liver Transplantation: From the Hepatic to the Systemic Circulatory Systems. Clin Liver Dis. 2017;21:253–74. doi: 10.1016/j.cld.2016.12.003. [DOI] [PubMed] [Google Scholar]
- 27.McLin VA, Rimensberger P, Belli DC, Wildhaber BE. Anticoagulation following pediatric liver transplantation reduces early thrombotic events. Pediatr Transplant. 2011;15:117–8. doi: 10.1111/j.1399-3046.2010.01426.x. [DOI] [PubMed] [Google Scholar]
- 28.Guo C-B, Pu C-L, Li Y-C, Zhang M-M, Deng Y, Yan L-N, Kang Q, Jin X-Q. Thirty-five consecutive pediatric living donor liver transplantation: experiences and lessons learned from a single center. Hepatogastroenterology. 2014;61:391–7. [PubMed] [Google Scholar]
- 29.Kanmaz T, Yankol Y, Mecit N, Durmaz O, Acarli K, Kalayoğlu M. Pediatric liver transplant: a single-center study of 100 consecutive patients. Exp Clin Transplant Off J Middle East Soc Organ Transplant. 2014;12:41–5. doi: 10.6002/ect.2013.0016. [DOI] [PubMed] [Google Scholar]
- 30.Nacoti M, Cazzaniga S, Lorusso F, Naldi L, Brambillasca P, Benigni A, Corno V, Colledan M, Bonanomi E, Vedovati S, Buoro S, Falanga A, Lussana F, Barbui T, Sonzogni V. The impact of perioperative transfusion of blood products on survival after pediatric liver transplantation. Pediatr Transplant. 2012;16:357–66. doi: 10.1111/j.1399-3046.2012.01674.x. [DOI] [PubMed] [Google Scholar]
- 31.Donohue CI. Reducing transfusion requirements in liver transplantation. World J Transplant. 2015;5:165. doi: 10.5500/wjt.v5.i4.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Leon-Justel A, Noval-Padillo JA, Alvarez-Rios AI, Mellado P, Gomez-Bravo MA, Álamo JM, Porras M, Barrero L, Hinojosa R, Carmona M, Vilches-Arenas A, Guerrero JM. Point-of-care haemostasis monitoring during liver transplantation reduces transfusion requirements and improves patient outcome. Clin Chim Acta Int J Clin Chem. 2015;446:277–83. doi: 10.1016/j.cca.2015.04.022. [DOI] [PubMed] [Google Scholar]
- 33.Shay R, Taber D, Pilch N, Meadows H, Tischer S, McGillicuddy J, Bratton C, Baliga P, Chavin K. Early aspirin therapy may reduce hepatic artery thrombosis in liver transplantation. Transplant Proc. 2013;45:330–4. doi: 10.1016/j.transproceed.2012.05.075. [DOI] [PubMed] [Google Scholar]
- 34.De Pietri L, Bianchini M, Montalti R, De Maria N, Di Maira T, Begliomini B, Gerunda GE, di Benedetto F, Garcia-Tsao G, Villa E. Thrombelastography-guided blood product use before invasive procedures in cirrhosis with severe coagulopathy: A randomized, controlled trial. Hepatol. 2016;63:566–73. doi: 10.1002/hep.28148. [DOI] [PubMed] [Google Scholar]
- 35.Nacoti M, Corbella D, Fazzi F, Rapido F, Bonanomi E. Coagulopathy and transfusion therapy in pediatric liver transplantation. World J Gastroenterol. 2016;22:2005–23. doi: 10.3748/wjg.v22.i6.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Clevenger B, Mallett SV. Transfusion and coagulation management in liver transplantation. World J Gastroenterol. 2014;20:6146–58. doi: 10.3748/wjg.v20.i20.6146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rana A, Petrowsky H, Hong JC, Agopian VG, Kaldas FM, Farmer D, Yersiz H, Hiatt JR, Busuttil RW. Blood transfusion requirement during liver transplantation is an important risk factor for mortality. J Am Coll Surg. 2013;216:902–7. doi: 10.1016/j.jamcollsurg.2012.12.047. [DOI] [PubMed] [Google Scholar]
- 38.Rijken DC, Kock EL, Guimarães AHC, Talens S, Darwish Murad S, Janssen HLA, Leebeek FWG. Evidence for an enhanced fibrinolytic capacity in cirrhosis as measured with two different global fibrinolysis tests. J Thromb Haemost JTH. 2012;10:2116–22. doi: 10.1111/j.1538-7836.2012.04901.x. [DOI] [PubMed] [Google Scholar]
- 39.Lisman T, Bakhtiari K, Adelmeijer J, Meijers JCM, Porte RJ, Stravitz RT. Intact thrombin generation and decreased fibrinolytic capacity in patients with acute liver injury or acute liver failure. J Thromb Haemost JTH. 2012;10:1312–9. doi: 10.1111/j.1538-7836.2012.04770.x. [DOI] [PubMed] [Google Scholar]
- 40.Hartmann M, Szalai C, Saner FH. Hemostasis in liver transplantation: Pathophysiology, monitoring, and treatment. World J Gastroenterol. 2016;22:1541–50. doi: 10.3748/wjg.v22.i4.1541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tripodi A, Primignani M, Chantarangkul V, Clerici M, Dell’Era A, Fabris F, Salerno F, Mannucci PM. Thrombin generation in patients with cirrhosis: the role of platelets. Hepatol. 2006;44:440–5. doi: 10.1002/hep.21266. [DOI] [PubMed] [Google Scholar]
- 42.Porte RJ. Coagulation and fibrinolysis in orthotopic liver transplantation: current views and insights. Semin Thromb Hemost. 1993;19:191–6. doi: 10.1055/s-2007-994025. [DOI] [PubMed] [Google Scholar]
- 43.Dargaud Y, Sorensen B, Shima M, Hayward C, Srivastava A, Negrier C. Global haemostasis and point of care testing. Haemoph Off J World Fed Hemoph. 2012;18:81–8. doi: 10.1111/j.1365-2516.2012.02855.x. [DOI] [PubMed] [Google Scholar]
- 44.Benes J, Zatloukal J, Kletecka J. Viscoelastic Methods of Blood Clotting Assessment – A Multidisciplinary Review. [cited 2016 Oct 31];Front Med [Internet] 2015 Sep 14;2 doi: 10.3389/fmed.2015.00062. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4568412/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wang S-C, Shieh J-F, Chang K-Y, Chu Y-C, Liu C-S, Loong C-C, Chan K-H, Mandell S, Tsou M-Y. Thromboelastography-Guided Transfusion Decreases Intraoperative Blood Transfusion During Orthotopic Liver Transplantation: Randomized Clinical Trial. Transplant Proc. 2010;42:2590–3. doi: 10.1016/j.transproceed.2010.05.144. [DOI] [PubMed] [Google Scholar]
- 46.Tripodi A, Primignani M, Chantarangkul V, Viscardi Y, Dell’Era A, Fabris FM, Mannucci PM. The coagulopathy of cirrhosis assessed by thromboelastometry and its correlation with conventional coagulation parameters. Thromb Res. 2009;124:132–6. doi: 10.1016/j.thromres.2008.11.008. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.