Abstract
Objectives
The objectives of this study were to 1) determine if hypertensive patients with comorbid diabetes mellitus (DM) and/or chronic kidney disease (CKD) receiving a pharmacist intervention had a greater reduction in mean blood pressure (BP) and improved BP control at 9 months compared to those receiving usual care and 2) compare Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC-7) guideline and 2014 guideline (JNC-8) BP control rates in patients with DM and/or CKD.
Methods
This cluster, randomized trial included 32 medical offices in 15 states. Clinical pharmacists made treatment recommendations to physicians at intervention sites. This post-hoc analysis evaluated mean BP and BP control rates in the intervention and control groups.
Main results
The study included 335 patients (227 intervention, 108 control) when mean BP and control rates were evaluated by JNC-7 inclusion and control criteria. When JNC-8 inclusion and control criteria were applied, 241 patients (165 intervention, 76 control) remained and were included in the analysis. The pharmacist-intervention group had significantly greater mean SBP reduction compared to usual care at 9 months (8.64 mm Hg [95% Confidence interval (CI)= −12.8, −4.49, p<0.001]). The pharmacist-intervention group had significantly higher BP control at 9 months than usual care by either the JNC-7 or JNC-8 inclusion and control groups (adjusted odds ratio (OR) 1.97 [95% CI= 1.01, 3.86]; p=0.0470 and 2.16 [95%CI= 1.21, 3.85]; p=0.0102, respectively).
Principal conclusions
This study demonstrated that a physician-pharmacist collaborative intervention was effective in reducing mean systolic BP and improving BP control in patients with uncontrolled hypertension with DM and/or CKD, regardless of which BP guidelines were used.
Clinical Trial Registration Information
Keywords: team-based care, diabetes, chronic kidney disease, hypertension
Hypertension (HTN) affects roughly one out of every three adults in the United States and contributed to more than 400,000 deaths in 2014.1) In addition, hypertension increases the risk for cardiovascular disease, including myocardial infarction and stroke.2 Independently, diabetes mellitus (DM) and chronic kidney disease (CKD) are responsible for a high degree of cardiovascular complications.3–6 Hypertension with DM or CKD multiplies the risk for cardiovascular-related death, myocardial infarction (MI), angina pectoris, and stroke.7,8
Self-reported data found that 11.9% of individuals in the United States have either physician-diagnosed or undiagnosed DM.9 Among patients with both hypertension and DM, only 29.6% meet their blood pressure (BP) goal.10 Blood pressure control reduces cardiovascular complications in patients with both hypertension and DM.11,12 For each 10 mm Hg decrease in mean systolic BP (SBP) there is an associated 12% reduction in diabetic complications, 15% reduction in deaths related to DM, 11% reduction in myocardial infarction, and 13% reduction in microvascular complications.13
National Health and Nutrition Examination Survey data found that the prevalence of CKD in those with undiagnosed and diagnosed hypertension was 22.0% and 27.5%, respectively.14 Population-based data suggest that awareness, control, and adequate treatment of other cardiovascular complications are suboptimal in those with CKD. Studies have shown that even small elevations of BP place patients at increased risk for progression to end-stage renal disease.15, 16
Team-based care including pharmacists and nurses is a proven method to improve BP control.17–20 The physician-pharmacist collaborative management (PPCM) model involves close collaboration within primary care settings to optimize drug therapy and promote preventative health measures.21 Studies have shown that addition of pharmacists to the health care team improves BP in those with DM.22–24 Although there are examples of randomized controlled trials that have examined pharmacist contributions to BP outcomes in those with DM, many studies were conducted in community pharmacies, outside the United States, or with limited numbers of medical offices.25, 26
The Collaboration Among Pharmacists and Physicians To Improve Blood Pressure Now (CAPTION) study was a cluster-randomized implementation trial measuring the impact of PPCM on patients with uncontrolled hypertension in 32 medical offices across the United States.27 The primary end point in CAPTION did not achieve statistical significance; BP control was 43% in the intervention group and 34% in the control group at 9 months (adjusted odds ratio (OR) 1.57 [95% CI 0.99–2.50], p=0.059).27 The CAPTION trial defined BP control for those with DM and CKD as less than 130/80 mm Hg based on the, then current, Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC-7) guidelines.28 Additionally, the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial, which was published during the CAPTION trial, did not find evidence to support a goal SBP below 140 mm Hg in patients with diabetes.29 Some clinicians in the CAPTION trial anecdotally expressed discomfort with the JNC-7 goals.
The CAPTION investigators conducted a sensitivity analysis using the definitions from the newer 2014 evidence-based guidelines for the management of high BP in adults (JNC-8), which recommended higher BP goals (140/90 mm Hg) for patients who are older than 60 years of age and for patients who suffer from DM or CKD.30 When the higher goals were used, BP control was achieved in 61% of intervention patients and 45% of controls at 9 months (adjusted OR, 2.03 [95% CI 1.29–3.22], p=0.003). More than half of patients enrolled in CAPTION had either DM or CKD.27 Therefore, it was theorized that the lower BP control rates might be explained by providers who lowered BP to a point close to the JNC-7 BP goal in those with DM or CKD but may not have quite reached the aggressive less than 130/80-mm Hg threshold.
The aims of the present CAPTION substudy are to 1) determine if hypertensive patients with comorbid DM and/or CKD receiving a pharmacist intervention had improved BP control and greater reduction in mean BP at 9 months compared to those receiving usual care and 2) compare JNC-7 and JNC-8 BP control rates in CAPTION patients with DM and/or CKD.
Materials and Methods
The main study design, baseline data, and results have been previously published.27, 31 The CAPTION study included 32 medical offices from 15 U.S. states and was a prospective, cluster-randomized, multicenter clinical trial. Offices were stratified based on the level of pharmacy services provided and percent minority patients.31, 32 Offices were then randomized to one of the three study arms: (i) usual BP care; (ii) a 9-month BP intervention; or (iii) a sustained, 24-month intervention. The two intervention arms were designed to be the same for the first 9 months so they could be combined and compared to usual care. The analyses for the present substudy were planned post hoc and included mean BP reduction and BP control during the first 9 months of the intervention for patients with comorbid DM and/or CKD.
Patient Recruitment
The institutional review board (IRB) in each medical office approved this study. Patients were included if they: (i) were English- or Spanish-speaking males or females, over 18 years of age with diagnosed hypertension, (ii) had uncontrolled hypertension defined as a SBP 140 mm Hg or greater or diastolic BP (DBP) 90 mm Hg or greaterfor uncomplicated hypertension and a SBP of 130 mm Hg or greater or DBP 80 mm Hg or greater for patients with DM or CKD, and (iii) received care from one the participating medical clinics. A patient was classified as having DM/CKD if they had been diagnosed with either condition at baseline, as reported on the ‘Diagnosed Conditions’ electronic case report form. If neither condition was reported, a further examination of CKD was based on the calculated glomerular filtration rates from the patient’s two most recent creatinine tests at baseline. Glomerular filtration rate was calculated using the Modification of Diet in Renal Disease Study equation.33 In the present substudy, only patients with diagnosed DM, CKD, or both DM and CKD were included in the analysis. Patients could have either type 1 or type 2 DM. The study did not determine which type of DM these patients had, but the vast majority had type 2 DM.
Patients were excluded if they had (i) current signs of hypertensive emergency (acute angina, stroke, or renal failure); (ii) severe HTN (SBP >200 or DBP >114 mm Hg); (iii) history of MI, stroke, or unstable angina in prior 6 months; (iv) systolic dysfunction with left ventricular ejection fraction less than 35% determined by echocardiography, nuclear medication imaging, or ventriculography; (v) renal insufficiency as defined by GFR less than 20 mL/min or documented proteinuria greater than1 g/day; (vi) significant hepatic disease including cirrhosis, hepatitis B or C, or lab abnormalities (serum alanine transaminase or aspartate aminotransferase >2 upper limit of normal or total bilirubin >1.5 mg/dl) in the prior 6 months; (vii) pregnancy; (viii) diagnosis of pulmonary hypertension or sleep apnea; (ix) life expectancy estimated at less than 2 years; (x) residence in nursing home or diagnosis of dementia, and (xi) inability to give informed consent or impaired cognitive function (defined as ≥ 3 errors on the 10-item Pfeiffer).34
A study coordinator (generally a medical assistant or nurse) employed within each office recruited subjects and collected data. The study coordinator used billing records to identify patients with hypertension. Patient lists were then submitted to the biostatistician who randomized the list. The study coordinator then selected patients in order from the randomized list to avoid selection bias. All patients who agreed to participate signed written informed consent.
Data Collection
Study coordinators at all offices collected data at baseline, 9 and 24 months.31 Study coordinators were trained in Iowa City in the following areas: (i) ethical treatment of human subjects; (ii) informed consent documents; (iii) protocol methods; and (iv) BP measurement using the automated Omron HEM 907-XL device (Omron healthcare; Bannockburn, Illinois, United States). 35 Blood pressure was measured three times in the sitting position using appropriate technique. The first BP reading was not used. The second and third BP measurements were averaged, but if the SBP or DBP values varied by more than 4 mm Hg, a fourth measurement was taken and the two closest readings between the second, third, and fourth measurement were averaged. Study coordinators then collected information regarding demographics and past medical history, including DM and CKD, from both patient report and the medical record.
All data were uploaded into an encrypted, web-based data management system designed and managed by the Data Coordinating Center (DCC). The DCC conducted a centralized evaluation of data to minimize errors. Staff from the DCC visited each office to perform data monitoring procedures to compare the database with the medical record source documents.
Pharmacist Intervention
Pharmacists at each medical office in the intervention arm completed a patient interview including: (i) medication history of all prescription, nonprescription, and herbal medications; (ii) an assessment of health literacy including patient knowledge of BP medications, indication of each medication, goals of therapy, medication dosages and frequency, and potential side effects; (iii) contraindications to each medication; and (iv) issues related to adherence and monitoring.
Pharmacists were encouraged first to assess medication knowledge, and then educate the patient on hypertension and the importance of properly following the pharmacotherapy plan. Pharmacists also provided recommendations on lifestyle modification, a wallet card listing all current medications and doses, and pharmacist contact information. In certain patients warranting additional adherence aid, pharmacists encouraged the use of medication logs or medication boxes. The pharmacist then created an individualized care plan with BP goal and medication recommendations. Care plans were presented to the physician either verbally or, if preferred by the physician, by electronic communication. If the physician decided to make modifications, the pharmacist finalized the plan. The proposed intervention included scheduled face-to-face visits with the patient at baseline, 1, 2, 4, 6, and 8 months and a telephone call at 2 weeks. Additional telephone calls were added as needed for those with uncontrolled hypertension. Although there was a protocol that was suggested to implement the intervention, the study was designed as a more pragmatic, effectiveness trial. Thus, clinical pharmacists were free to modify the intervention based on their professional judgment including the frequency of visits with patients. There were no treatment protocols and clinical pharmacists were only instructed to follow the JNC-7 guidelines. Investigators tracked the number of visits with the pharmacists to determine how closely pharmacists adhered to the proposed intervention frequency.
Analysis
The analysis for the present study compared mean SBP and DBP for patients with DM and/or CKD receiving a pharmacist intervention to those receiving usual care. An additional analysis was performed comparing BP control in patients with DM and/or CKD receiving the pharmacist intervention to those receiving usual care with JNC-8 inclusion and control criteria. The CAPTION trial enrolled patients with uncontrolled hypertension, giving consideration to diagnoses of DM or CKD based on the JNC-7 criteria. If patients had a diagnosis of hypertension and DM and/or CKD, their BP goal was 130/80 mm Hg. In order to evaluate the effect of the intervention using JNC-8 criteria, 94 of the initial 335 subjects from the trial were excluded based on the higher BP goals (<140/90 mm Hg). For this reason, fewer original patients met the criteria for uncontrolled BP using the JNC-8 criteria. The analyses were secondary, post-hoc, and comparable to the main CAPTION analyses.27, 31
Mean SBP and DBP were analyzed using a linear mixed model with random effects for office and patient within office. The center random effects were assumed to be normally distributed and have a compound symmetric covariance structure, and the nested within subjects errors were assumed to have an AR(1) covariance structure. Blood pressure control was analyzed using a nonlinear mixed effects model with the logit link function. Like the linear models, the office random effects were assumed to be normally distributed with a compound symmetric covariance structure and the nested within subjects errors were assumed to have an AR(1) covariance structure. Potential confounding variables at baseline were examined, and sensitivity analyses was performed to adjust for any covariates that differed across treatment groups.27
Blood pressure was assumed to be uncontrolled if a BP value was missing at 9 months. This approach has been used in many trials and is a conservative method to recognize that if a patient missed the visit, BP was more likely to be uncontrolled than controlled.18, 36 No multiple imputation was used to account for missing BPs in the linear models. These same analyses were used for both the JNC-7 and JNC-8 analysis groups for mean BPs, the only difference being that patients in the original cohort with baseline BPs below the new threshold (<140/90 mm Hg) were not included in the JNC-8 cohort since those with controlled BP would not have met the original inclusion criteria for the study.
Results
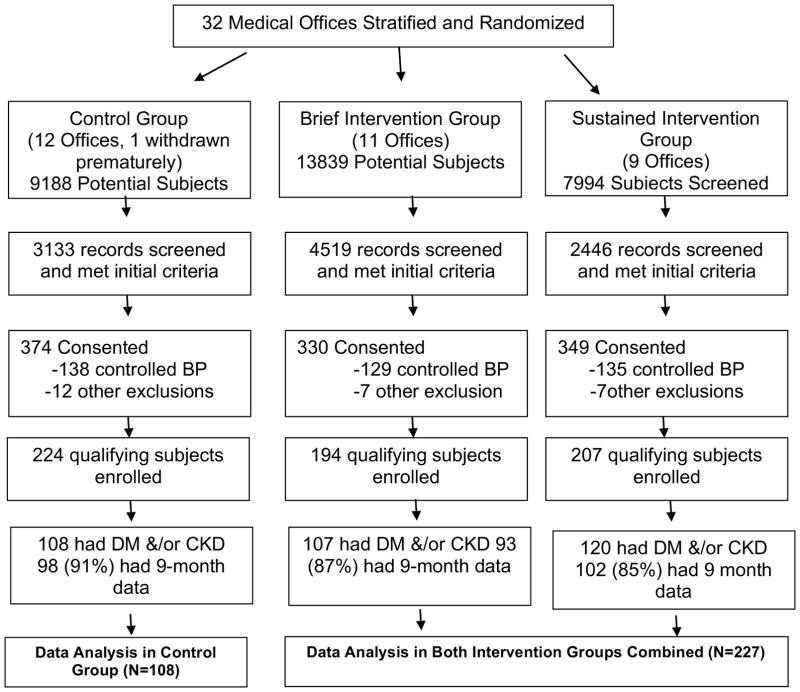
There were 335 patients included in this study; 242 had DM, 43 had CKD, and 50 had both. Patient recruitment began March 2010 and the last patient completed the trial in June 2013 (Figure 1). Therefore, the JNC-7 guidelines were in place throughout the entire study. There were no differences in the intervention effect related to sex. Baseline demographic information for the patients included in the present study is displayed in Table 1.
Figure 1.
CONSORT Statement of Clinic Randomization and Patient Participation
CONSORT: Consolidated Standards of Reporting Trials
BP: Blood pressure
DM: Diabetes mellitus
CKD: Chronic kidney disease
Table 1.
Demographic Characteristics at Baseline
| Variable | Control (N=108) N (%) |
Intervention (N=227) N (%) |
|---|---|---|
|
| ||
| Gender | ||
|
| ||
| Male | 37 (34.3%) | 84 (37.0%) |
| Female | 71 (65.7%) | 143 (63.0%) |
|
| ||
| Race/Ethnicity | ||
|
| ||
| Non-Hispanic Caucasian | 34 (31.5%) | 89 (39.2%) |
| Minority | 73 (67.6%) | 135 (59.5%) |
| Declined to answer/missing | 1 (0.9%) | 3 (1.3%) |
|
| ||
| Education | ||
|
| ||
| <= 12 Years | 65 (60.2%) | 137 (60.4%) |
| > 12 Years | 41 (38.0%) | 89 (39.2%) |
|
| ||
| Marital status | ||
|
| ||
| Married | 45 (41.7%) | 110 (48.5%) |
| Not married | 63 (58.3%) | 116 (51.1%) |
|
| ||
| Insurance coverage | ||
|
| ||
| Medicare | 40 (37.0%) | 77 (33.9%) |
| Private and Other | 41 (38.0%) | 75 (33.0%) |
| Medicaid | 19 (17.6%) | 37 (16.3%) |
| Free and None/Self-Pay | 8 (7.4%) | 38 (16.7%) |
|
| ||
| Annual income | ||
|
| ||
| < $25,000 | 60 (55.6%) | 129 (56.8%) |
| >= $25,000 | 48 (44.4%) | 97 (42.7%) |
|
| ||
| Smoking status | ||
|
| ||
| Current smoker | 14 (13.0%) | 43 (18.9%) |
| Former smoker | 33 (30.6%) | 76 (33.5%) |
| Never smoker | 60 (55.6%) | 106 (46.7%) |
|
| ||
| Duration of high BP | ||
|
| ||
| <= 3 years | 11 (10.2%) | 27 (11.9%) |
| > 3 – 10 years | 41 (38.0%) | 74 (32.6%) |
| > 10 years | 56 (51.9%) | 126 (55.5%) |
|
| ||
| Comorbidities | ||
|
| ||
| Diabetes | 75 (69.4%) | 167 (73.6%) |
| CKD | 15 (13.9%) | 28 (12.3%) |
| Diabetes and CKD | 18 (16.7%) | 32 (14.1%) |
| Hyperlipidemia | 81 (75.0%) | 158 (69.6%) |
| Arthritis/DJD/Chronic Pain | 60 (55.6%) | 88 (38.8%) |
| Depression or Anxiety | 29 (26.9%) | 68 (30.0%) |
| Asthma or COPD | 16 (14.8%) | 39 (17.2%) |
| Stroke or TIA | 8 (7.4%) | 18 (7.9%) |
| Coronary Artery Disease | 6 (5.6%) | 18 (7.9%) |
| Seizures/Other Neurologic Disorders | 9 (8.3%) | 10 (4.4%) |
| Heart Failure | 3 (2.8%) | 12 (5.3%) |
| Liver Disease | 2 (1.9%) | 3 (1.3%) |
| Peripheral Artery Disease | 0 (0.0%) | 4 (1.8%) |
|
| ||
| Number of Comorbidities | ||
|
| ||
| Mean (SD) | 3.0 (1.2) | 2.8 (1.4) |
|
| ||
| Age (years) | ||
|
| ||
| Mean (SD) | 63.1 (12.2) | 61.7 (11.6) |
| Min - Max | (28, 88) | (29, 93) |
|
| ||
| Baseline SBP (mm Hg) | ||
|
| ||
| Mean (SD) | 147.36 (16.26) | 147.00 (15.71) |
| Min - Max | (117, 197) | (106, 198) |
|
| ||
| Baseline DBP (mm Hg) | ||
|
| ||
| Mean (SD) | 80.70 (12.09) | 81.82 (11.65) |
| Min - Max | (53, 111) | (54, 114) |
|
| ||
| Weight (Kg) | ||
|
| ||
| Mean (SD) | 95.7 (25.2) | 98.5 (26.3) |
| Min - Max | (40, 188) | (42, 181) |
|
| ||
| BMI | ||
|
| ||
| Mean (SD) | 34.4 (8.0) | 35.3 (8.7) |
| Min - Max | (16, 61) | (19, 65) |
|
| ||
| Number of Antihypertensive Medications | ||
|
| ||
| Mean (SD) | 2.4 (1.2) | 2.3 (1.2) |
| Min - Max | (1, 6) | (1, 6) |
|
| ||
| Adverse Reaction Score | ||
|
| ||
| Mean (SD) | 34.5 (25.4) | 39.5 (30.0) |
| Min - Max | (1, 133) | (0, 142) |
BP: Blood pressure
SBP: Systolic blood pressure
DBP: Diastolic blood pressure
Min: minimum
Max: maximum
SD: standard deviation
CKD: Chronic Kidney Disease
BMI: Body mass index
COPD: chronic obstructive pulmonary disease
TIA: transient ischemic attack
DJD: degenerative joint disease
Table 2 shows mean BP at baseline and 9 months between patients receiving the pharmacist intervention and usual care. The pharmacist-intervention group achieved a model-adjusted SBP and DBP reduction of 8.64 (95% CI= −12.8, −4.49, p<0.001) and 2.90 (95% CI= −5.55, −0.25, p=0.0323) mm Hg greater than that of the control group, respectively.
Table 2.
Mean blood pressure at Baseline and 9 months
| Baseline | 9-months | |||||
|---|---|---|---|---|---|---|
| Control (N=108) | Intervention (N=227) | Control (N=108) | Intervention (N=227) | Model Based Difference (95% CI) | p-values | |
| SBP (mm Hg) | ||||||
| Mean (SD) | 147.36 (16.26) | 147.00 (15.71) | 139.29 (20.52) | 130.65 (16.67) | −8.64 (−12.8, −4.49) | <0.001 |
| DBP (mm Hg) | ||||||
| Mean (SD) | 80.70 (12.09) | 81.82 (11.65) | 76.16 (16.09) | 74.23 (10.64) | −2.90 (−5.55, −0.25) | 0.0323 |
SBP: Systolic blood pressure
DBP: Diastolic blood pressure
SD: Standard deviation
CI: Confidence interval
Table 3 shows BP control rates at 9 months between patients receiving the pharmacist intervention and those receiving usual care for both JNC-7 and JNC-8 BP goals. The pharmacist intervention, regardless of BP goal, was able to reach significant BP control compared to usual care in both the JNC-7 analysis (adjusted OR, 1.97 [95% CI=1.01, 3.86]; p=0.0470) and the JNC-8 analysis (adjusted OR, 2.16 [95% CI=1.21, 3.85]; p=0.0102).
Table 3.
Blood pressure Control Rates With Pharmacist Intervention versus Usual Care at 9 months
| BP Guideline | Control (N=108) | Intervention (N=227) | Adjusted Odds-Ratio (95% CI) | p-values |
|---|---|---|---|---|
| JNC-7 (130/80 mm Hg) | 23 (21.3%; n=108) | 77 (33.9%; n=227) | 1.97 (1.01, 3.86) | 0.0470 |
| JNC-8 (140/90 mm Hg) | 31 (40.8%; n=76) | 96 (58.2%; n=165) | 2.16 (1.21, 3.85) | 0.0102 |
BP: Blood pressure
JNC: Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure.
The numbers and types of pharmacist recommendations and the medications used in the CAPTION trial were previously published.37 There were no differences in medication classes used between intervention and control groups following the intervention with the exception that there was greater use of diuretics and aldosterone antagonists in the intervention group.
Discussion
This study demonstrated that a pharmacist intervention significantly reduced mean SBP in patients with uncontrolled hypertension and DM and/or CKD compared to usual care. Most importantly, the pharmacist-intervention group had significantly higher BP control at 9 months compared to usual care, regardless of which BP goal was used. The level of significance was higher in the JNC-8 analysis compared to that of the JNC-7 analysis. Findings based on race, income, education, and insurance status were previously published.38 The pharmacist intervention had similar effects in these subgroups as with the entire study population including those previously taking three or more antihypertensive medications at baseline.39 As anticipated, a considerable difference in control rates was found between pharmacist intervention and usual care when JNC-7 and JNC-8 BP goals were applied since JNC-8 relaxed goals for DM and CKD. We theorize that the pharmacist intervention was successful in getting most patients close to their 130/80-mm Hg threshold. However, because the ACCORD trial and other commentaries published during our study questioned these lower goals, some clinicians may have not felt comfortable lowering BP to these levels.29
In previous studies, PPCM has been shown to both reduce mean BP and increase BP control.17 In the original CAPTION trial, the difference in mean BP between the pharmacist intervention and usual care for all study patients was−-6.1/−2.9 mm Hg (p<0.001 and p=0.003, respectively) at 9 months.27 However, the primary outcome was BP control, and this did not quite achieve statistical significance (p=0.059), in part, due to greater interclinic variability than originally expected.27 Newer studies and the most recent hypertension 2017 guidelines supported by multiple professional organizations recommend a BP of less than 130/80 mm Hg in almost all individuals with hypertension.40, 41 These new goals will be difficult to achieve especially in patients with comorbidities and socioeconomic disadvantages.
Other investigators have examined the impact of team-based care in the treatment of multiple chronic conditions. The Fremantle Diabetes Study demonstrated positive BP control outcomes (p=0.043), but it should be noted that the investigators defined BP control as <135/85 mm Hg.42 A group of investigators showed improved mean BP with a pharmacist intervention in North Carolina internal medicine offices.24 The pharmacist-intervention group in this study had a mean BP reduction of 7 mm Hg over the course of 12 months, whereas the control group had a mean BP increase of 2 mm Hg, making the difference 9 mm Hg between groups. In contrast, the patient group receiving pharmacist intervention in the present study had a mean BP reduction of about 16 mm Hg, with the usual-care group achieving an 8 mm Hg reduction. A randomized study conducted in a community health center found a significant difference in mean BP after a 9-month pharmacist intervention, but baseline SBP for both intervention and control was already quite low (130.0 mm Hg and 130.7 mm Hg, respectively).25 A study conducted with patients from 14 community pharmacies in Edmonton, Alberta, Canada, found that care from pharmacist-nurse teams significantly improved BP control and reduced mean BP in those with hypertension and DM.26 By comparison, the patient population in the Canadian study had lower mean BP at baseline and considerably less BP reduction (5.6 mm Hg) than the present study. Several studies have found that the addition of a pharmacist to a primary care team was effective in reducing mean BP and meeting BP targets.22, 23 Although patients in one of the studies achieved significantly improve BP control (p=0.02), the difference in mean BP between intervention and control groups was modest (4.9 mm Hg).22
The present study is unique because it was a cluster, randomized-controlled trial in patients enrolled from 32 medical offices across 15 U.S. states. One strength of the CAPTION trial was that it was designed as a more pragmatic, effectiveness trial. A standard practice, protocol, medications, or method of communication with physicians was not required. Some pharmacists used collaborative practice agreements to initiate and adjust therapy, whereas others had all medication changes approved by the physician. The only goal established for the pharmacist was to achieve BP control using JNC-7 criteria. Fifty-four percent of patients were from under-represented minority groups, with 71% being African American, 26% Hispanic, and 3% other.27 Additionally, 49% had income less than $25,000/year and 25% used Medicaid, self-pay, or no insurance for their health care payment.38 Finally, 27% of patients met the definition of treatment-resistant hypertension.39 The intervention was as effective, or nearly as effective, for all these groups despite the challenges of achieving BP control in these patient groups. In this regard, the findings are generalizable to a broad range of practices and patient populations.
The most likely reason for improved BP in the intervention group was intensification of suboptimal regimens. There were significantly more medication changes (4.9 ± 5.1 vs 1.1 ± 1.6, p=0.0003) and medications added or doses increased (3.2 ±3.2 vs 0.7 ± 1.1, p=0.0002) in the intervention group compared to the control group, respectively.37 The intervention group was treated with significantly more diuretics and aldosterone antagonists, the latter likely being used for patients with treatment-resistant hypertension.
The disadvantage of efficacy trials without compulsory treatment and care protocols is that the intervention may not be completely implemented and there may be significant variability across sites. For instance, BP control rates ranged from 20% to 71% in the 20 intervention offices, and there was no clear indication that higher numbers of patients from minority groups, with lower income, no insurance, less education, or with diabetes or CKD explained these variable results.43 These findings suggest, but cannot prove, that variability in pharmacist practice styles may have contributed to the differences in BP control across sites.44
There are important limitations to this study. Fifteen percent of patients did not complete the 9-month visit, but this rate of missing data was actually lower than expected. A conservative approach was used to analyze missing data, which is a strength of the study. Additionally, this was a post-hoc analysis. However, the general findings in these patients with DM and/or CKD were similar to the overall study population that were prospectively enrolled. Despite these limitations, the addition of a pharmacist to the care team improved BP outcomes in groups at high cardiovascular risk who often have poor BP control.45
Conclusion
This study demonstrated that an intervention utilizing pharmacists embedded within medical offices who were members of the care team reduced mean SBP in those with uncontrolled hypertension and comorbid DM and/or CKD. Additionally, regardless of which guideline criteria were used to specify BP control, the pharmacist intervention improved patient BP control. Additional studies are warranted to support the effectiveness of PPCM in patients with hypertension, especially in light of the new hypertension guidelines that again suggest lower BP goals in patients with DM and CKD similar to the JNC-7 guidelines. Our findings suggest that a team-based care model including pharmacists can be implemented to improve BP control and reduce mean BP in patients with uncontrolled hypertension and DM and/or CKD.
Acknowledgments
Funding: Supported by the National Heart, Lung, and Blood Institute, RO1HL091841 and RO1HL091843
Site investigators for intervention offices in the CAPTION study:
Mark Jones, Pharm.D., Katherine M. Brasch, LPN, Andrew Andresen, MD, Genesis Family Medical Center, Davenport, IA; Lucinda Buys, Pharm.D., Maureen Huff, RN, Kurt Rosenkrans, M.D., Siouxland Medical Education Foundation, Sioux City, IA; Eric MacLaughlin, Pharm.D., Debbie Hermes, LPN, Rodney Young, MD, Texas Tech Center for Community and Family Medicine, Amarillo, TX; John Gums, Pharm.D; Eric Dietrich, Pharm.D., Steven Smith, Pharm.D., Delores Buffington, RN, Danielle Poulton, LPN, Karen Hall, MD, University of Florida Family Practice, Gainesville, FL; James Hoehns, Pharm.D., Pamela Trenkamp, RN, CCRP, James Poock, MD, Northeast Iowa Family Practice Center, Waterloo, IA; Timothy Ives, Pharm.D; Betsy Bryant-Shilliday, Pharm.D; Robb Malone, Pharm.D., Kate Gerrald, Pharm.D., Natalie Phillips, William Garneau, James Joyner, Paul Chelminski, M.D., University of North Carolina Enhanced Care Clinic, Chapel Hill, NC; Rex Force, PharmD, John Holmes, PharmD, Mary Macdonald, LPN, Loni Chacon, LPN, Brandon Mickelsen, D.O., Pocatello Family Medicine Clinic, Pocatello, ID; Oralia Bazaldua, Pharm.D; John Tovar, Pharm.D., Bryan Bayles, Ph.D., Inez Cruz, Ph.D., LMSW, Ramin Poursani, MD, University of Texas Health Science Center, San Antonio, TX; Carrie Stoltenberg, R.Ph., Jody Pankow, BSN, RN, Kate Judge, MSSW, Louis Sanner, MD, Northeast Family Practice, Madison, WI; Casey Gallimore, Pharm.D., Connie Kraus, Pharm.D; Anna Legreid Dopp, Pharm.D; Jeff Freud, Pharm.D., Jessica Wolf, Pharm.D., Terri Carufel-Wert, RN, Kate Judge, MSSW, Beth Potter, MD, Wingra Family Medical Center, Madison, WI; Elizabeth Buckley, Pharm.D., Victoria Mertins, RN, Karin Dinda, Nancy Kojis, RN, Jesse DeGroat, MD, Wheaton Franciscan Medical Group, Racine, WI;Karen Gunning, PharmD, Crystal Ecker, RN, Karly Pippitt, MD, University of Utah, Salt Lake City, UT; Nima Patel, Pharm.D., Gillian Pianka, MPA, Sandy Amoroso, RN, BSM, CNN, April Grant, Anuradha Paranjape, M.D., MPH, FACP, Lawrence Ward, M.D., MPH, Temple University, Philadelphia, PA; Christie Schumacher, PharmD,, Mary Ann Kliethermes, Pharm.D., Midwestern University, and Golbarg Moaddab, MD, Advocate Medical Group, Chicago, IL; Eric Jackson, Pharm.D., Evelyn Pianko, MA, Alan Cementina, MD, Family Medicine Center at Asylum Hill, Hartford, CT; Angela Wisniewski, Pharm.D., Meredith Snyder, BA, MPH, Jeanette Figueroa, MD, Jefferson Family Medicine Clinic, Buffalo, NY; Roberta Farrah, Pharm.D., Patricia Klatt, Pharm.D; M. Maggie Folan, PhD, Sandra Sauereisen, MD, University of Pittsburgh Medical Center St. Margaret Family Medicine, Pittsburg, PA; Kelly Ragucci, Pharm.D; Sarah Shrader, Pharm.D., Allison McCutcheon, MPH, Eric Matheson, MD, MS, Medical University of South Carolina Department of Family Medicine Clinic, Charleston, SC; Lori Dickerson, Pharm.D; Allison McCutcheon, MPH, Peter Carek, MD, MS, Trident Family Medicine, Charleston, SC; Adrienne Z. Ables, Pharm.D., Lynda Lowe, RN, I.S. Simon, MD, Spartanburg Family Medicine, Spartanburg, SC; Kevin Sneed, Pharm.D., H. Glenn Whelan, Pharm.D., Kymia Love Jackson, BBA, Eduardo Gonzalez, MD, University of South Florida Department of Family Medicine, Tampa, FL; CoraLynn Trewet, Pharm.D., Mary Froehle, BS, CHES, Rhonda Foley, LPN, Larry Severidt, MD, Broadlawns Family Health Center, Des Moines, IA; Jennifer Goldman-Levine, Pharm.D., Sandy Cogliano, MA, Greg Sawin, MD, Tufts University Family Medicine, Malden, MA; Philip Rodgers, Pharm.D; Tracie Rothrock-Christian, Pharm.D., Angela Braswell, LPN, Duke University Medical Center, Lynn Bowlby, MD, Durham, NC; Karen Oles, Pharm.D., Rebecca Edwards, Pharm.D., Geraldine Zurek, MEd, CCRP, David Townsend, MD, Northwest Area Health Education Center, Wake Forest University, Winston Salem, NC; Jeri Sias, Pharm.D, Jose Rodriguez, CPHT, CCRP, Marco Diaz, MD, Texas Tech Community Partnership Clinics, El Paso, TX; Margie Perez-Padilla, Pharm.D., Jose Rodriguez, CPHT, CCRP, Brenda Silva, PA-C, Jose Luna, Jr., MD, University of Texas, Centro San Vicente, El Paso, TX; Julie Adkison, Pharm.D., Dianne Torres, MA, Michael Crouch, MD, Memorial Family Medicine Program, Sugar Land, TX; Sarah McBane, Pharm.D., Grace Kuo, Pharm.D., Alice Blaj, Heather Hutchinson, Sara Ramirez, MA, Carlos Rojas, MD, Fourth & Lewis Family Medicine, San Diego, CA; Grace Kuo, Pharm.D., MPH, Nathan Painter, Pharm.D., Alita Newsome, MA, Alice Blaj, Heather Hutchinson, Marie Williams, MA, Dustin Lillie, MD, Scripps Ranch Family Medicine, San Diego, CA.
Footnotes
Conflict of interest: Authors of this paper have nothing to disclose concerning possible financial or personal relationships with commercial entities that may have a direct or indirect interest in the subject matter of this manuscript.
References
- 1.High Blood Pressure Fact Sheet. Centers for Disease Control and Prevention; [Accessed on December 20, 2017]. [cited 2016 July 14]. Available from: http://www.cdc.gov/dhdsp/data_statistics/fact_sheets/fs_bloodpressure.htm. [Google Scholar]
- 2.Centers for Disease Control and Prevention, National Center for Health Statistics. Underlying Cause of Death 1999–2013 on CDC WONDER Online Database, released 2015. [Accessed on December 20, 2017];Data are from the Multiple Cause of Death Files, 1999–2013, as compiled from data provided by the 57 vital statistics jurisdictions through the Vital Statistics Cooperative Program. http://wonder.cdc.gov/ucd-icd10.html.
- 3.Vinik A, Flemmer M. Diabetes and macrovascular disease. Journal of diabetes and its complications. 2002;16(3):235–45. doi: 10.1016/s1056-8727(01)00212-4. [DOI] [PubMed] [Google Scholar]
- 4.Klein R, Klein BE, Moss SE. Relation of glycemic control to diabetic microvascular complications in diabetes mellitus. Annals of internal medicine. 1996;124(1 Pt 2):90–6. doi: 10.7326/0003-4819-124-1_part_2-199601011-00003. [DOI] [PubMed] [Google Scholar]
- 5.Daly C. Is early chronic kidney disease an important risk factor for cardiovascular disease? A background paper prepared for the UK Consensus Conference on early chronic kidney disease. Nephrology, dialysis, transplantation : official publication of the European Dialysis and Transplant Association - European Renal Association. 2007;22(Suppl 9):ix19–25. doi: 10.1093/ndt/gfm445. [DOI] [PubMed] [Google Scholar]
- 6.Keith DS, Nichols GA, Gullion CM, Brown JB, Smith DH. Longitudinal follow-up and outcomes among a population with chronic kidney disease in a large managed care organization. Archives of internal medicine. 2004;164(6):659–63. doi: 10.1001/archinte.164.6.659. [DOI] [PubMed] [Google Scholar]
- 7.Hypertension in Diabetes Study (HDS): II. Increased risk of cardiovascular complications in hypertensive type 2 diabetic patients. Journal of hypertension. 1993;11(3):319–25. doi: 10.1097/00004872-199303000-00013. [DOI] [PubMed] [Google Scholar]
- 8.Shulman NB, Ford CE, Hall WD, et al. Prognostic value of serum creatinine and effect of treatment of hypertension on renal function. Results from the hypertension detection and follow-up program. The Hypertension Detection and Follow-up Program Cooperative Group. Hypertension. 1989;13(5 Suppl):I80–93. doi: 10.1161/01.hyp.13.5_suppl.i80. [DOI] [PubMed] [Google Scholar]
- 9.National Center for Health Statistics. Health, United States, 2015: With Special Feature on Racial and Ethnic Health Disparities. Hyattsville, MD: 2016. [PubMed] [Google Scholar]
- 10.Suh DC, Kim CM, Choi IS, Plauschinat CA, Barone JA. Trends in blood pressure control and treatment among type 2 diabetes with comorbid hypertension in the United States: 1988–2004. Journal of hypertension. 2009;27(9):1908–16. doi: 10.1097/HJH.0b013e32832d4aee. [DOI] [PubMed] [Google Scholar]
- 11.Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. UK Prospective Diabetes Study Group. BMJ (Clinical research ed) 1998;317(7160):703–13. [PMC free article] [PubMed] [Google Scholar]
- 12.Efficacy of atenolol and captopril in reducing risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 39. UK Prospective Diabetes Study Group. BMJ (Clinical research ed) 1998;317(7160):713–20. [PMC free article] [PubMed] [Google Scholar]
- 13.Effects of ramipril on cardiovascular and microvascular outcomes in people with diabetes mellitus: results of the HOPE study and MICRO-HOPE substudy. Heart Outcomes Prevention Evaluation Study Investigators. Lancet (London, England) 2000;355(9200):253–9. [PubMed] [Google Scholar]
- 14.Cutler JA, Sorlie PD, Wolz M, Thom T, Fields LE, Roccella EJ. Trends in hypertension prevalence, awareness, treatment, and control rates in United States adults between 1988–1994 and 1999–2004. Hypertension. 2008;52(5):818–27. doi: 10.1161/HYPERTENSIONAHA.108.113357. [DOI] [PubMed] [Google Scholar]
- 15.Snyder JJ, Collins AJ. KDOQI hypertension, dyslipidemia, and diabetes care guidelines and current care patterns in the United States CKD population: National Health and Nutrition Examination Survey 1999–2004. American journal of nephrology. 2009;30(1):44–54. doi: 10.1159/000201014. [DOI] [PubMed] [Google Scholar]
- 16.Sarafidis PA, Li S, Chen SC, et al. Hypertension awareness, treatment, and control in chronic kidney disease. The American journal of medicine. 2008;121(4):332–40. doi: 10.1016/j.amjmed.2007.11.025. [DOI] [PubMed] [Google Scholar]
- 17.Proia KK, Thota AB, Njie GJ, et al. Team-based care and improved blood pressure control: a community guide systematic review. American journal of preventive medicine. 2014;47(1):86–99. doi: 10.1016/j.amepre.2014.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Carter BL, Ardery G, Dawson JD, et al. Physician and pharmacist collaboration to improve blood pressure control. Archives of internal medicine. 2009;169(21):1996–2002. doi: 10.1001/archinternmed.2009.358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Santschi V, Chiolero A, Colosimo AL, et al. Improving blood pressure control through pharmacist interventions: a meta-analysis of randomized controlled trials. Journal of the American Heart Association. 2014;3(2):e000718. doi: 10.1161/JAHA.113.000718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bove AA, Santamore WP, Homko C, et al. Reducing cardiovascular disease risk in medically underserved urban and rural communities. American heart journal. 2011;161(2):351–9. doi: 10.1016/j.ahj.2010.11.008. [DOI] [PubMed] [Google Scholar]
- 21.Von Muenster SJ, Carter BL, Weber CA, et al. Description of pharmacist interventions during physician-pharmacist co-management of hypertension. Pharmacy world & science : PWS. 2008;30(1):128–35. doi: 10.1007/s11096-007-9155-6. [DOI] [PubMed] [Google Scholar]
- 22.Simpson SH, Majumdar SR, Tsuyuki RT, Lewanczuk RZ, Spooner R, Johnson JA. Effect of adding pharmacists to primary care teams on blood pressure control in patients with type 2 diabetes: a randomized controlled trial. Diabetes care. 2011;34(1):20–6. doi: 10.2337/dc10-1294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Edelman D, Fredrickson SK, Melnyk SD, et al. Medical clinics versus usual care for patients with both diabetes and hypertension: a randomized trial. Annals of internal medicine. 2010;152(11):689–96. doi: 10.7326/0003-4819-152-11-201006010-00001. [DOI] [PubMed] [Google Scholar]
- 24.Rothman RL, Malone R, Bryant B, et al. A randomized trial of a primary care-based disease management program to improve cardiovascular risk factors and glycated hemoglobin levels in patients with diabetes. The American journal of medicine. 2005;118(3):276–84. doi: 10.1016/j.amjmed.2004.09.017. [DOI] [PubMed] [Google Scholar]
- 25.Scott DM, Boyd ST, Stephan M, Augustine SC, Reardon TP. Outcomes of pharmacist-managed diabetes care services in a community health center. American journal of health-system pharmacy : AJHP : official journal of the American Society of Health-System Pharmacists. 2006;63(21):2116–22. doi: 10.2146/ajhp060040. [DOI] [PubMed] [Google Scholar]
- 26.McLean DL, McAlister FA, Johnson JA, et al. A randomized trial of the effect of community pharmacist and nurse care on improving blood pressure management in patients with diabetes mellitus: study of cardiovascular risk intervention by pharmacists-hypertension (SCRIP-HTN) Archives of internal medicine. 2008;168(21):2355–61. doi: 10.1001/archinte.168.21.2355. [DOI] [PubMed] [Google Scholar]
- 27.Carter BL, Coffey CS, Ardery G, et al. Cluster-randomized trial of a physician/pharmacist collaborative model to improve blood pressure control. Circulation Cardiovascular quality and outcomes. 2015;8(3):235–43. doi: 10.1161/CIRCOUTCOMES.114.001283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chobanian AV, Bakris GL, Black HR, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. Jama. 2003;289(19):2560–72. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 29.Gerstein HC, Miller ME, Byington RP, et al. Effects of intensive glucose lowering in type 2 diabetes. The New England journal of medicine. 2008;358(24):2545–59. doi: 10.1056/NEJMoa0802743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8) Jama. 2014;311(5):507–20. doi: 10.1001/jama.2013.284427. [DOI] [PubMed] [Google Scholar]
- 31.Carter BL, Clarke W, Ardery G, et al. A cluster-randomized effectiveness trial of a physician-pharmacist collaborative model to improve blood pressure control. Circulation Cardiovascular quality and outcomes. 2010;3(4):418–23. doi: 10.1161/CIRCOUTCOMES.109.908038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Billups SJ, Okano G, Malone D, et al. Assessing the structure and process for providing pharmaceutical care in Veterans Affairs medical centers. American journal of health-system pharmacy : AJHP : official journal of the American Society of Health-System Pharmacists. 2000;57(1):29–39. doi: 10.1093/ajhp/57.1.29. [DOI] [PubMed] [Google Scholar]
- 33.Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Annals of internal medicine. 1999;130(6):461–70. doi: 10.7326/0003-4819-130-6-199903160-00002. [DOI] [PubMed] [Google Scholar]
- 34.Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. Journal of the American Geriatrics Society. 1975;23(10):433–41. doi: 10.1111/j.1532-5415.1975.tb00927.x. [DOI] [PubMed] [Google Scholar]
- 35.Pickering TG, Hall JE, Appel LJ, et al. Recommendations for blood pressure measurement in humans and experimental animals: Part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Hypertension. 2005;45(1):142–61. doi: 10.1161/01.HYP.0000150859.47929.8e. [DOI] [PubMed] [Google Scholar]
- 36.Carter BL, Bergus GR, Dawson JD, et al. A cluster randomized trial to evaluate physician/pharmacist collaboration to improve blood pressure control. Journal of clinical hypertension (Greenwich, Conn) 2008;10(4):260–71. doi: 10.1111/j.1751-7176.2008.07434.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gums TH, Uribe L, Vander Weg MW, James P, Coffey C, Carter BL. Pharmacist intervention for blood pressure control: medication intensification and adherence. Journal of the American Society of Hypertension : JASH. 2015;9(7):569–78. doi: 10.1016/j.jash.2015.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Anderegg MD, Gums TH, Uribe L, Coffey CS, James PA, Carter BL. Physician-Pharmacist Collaborative Management: Narrowing the Socioeconomic Blood Pressure Gap. Hypertension. 2016;68(5):1314–20. doi: 10.1161/HYPERTENSIONAHA.116.08043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Smith SM, Carris NW, Dietrich E, et al. Physician-pharmacist collaboration versus usual care for treatment-resistant hypertension. Journal of the American Society of Hypertension. 2016;10(4):307–17. doi: 10.1016/j.jash.2016.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Williamson JD, Supiano MA, Applegate WB, et al. Intensive vs Standard Blood Pressure Control and Cardiovascular Disease Outcomes in Adults Aged >/=75 Years: A Randomized Clinical Trial. JAMA. 2016;315(24):2673–82. doi: 10.1001/jama.2016.7050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults. Hypertension. Journal of the American College of Cardiology. 2017 doi: 10.1016/j.jacc.2017.11.006. [DOI] [Google Scholar]
- 42.Clifford RM, Davis WA, Batty KT, Davis TM. Effect of a pharmaceutical care program on vascular risk factors in type 2 diabetes: the Fremantle Diabetes Study. Diabetes care. 2005;28(4):771–6. doi: 10.2337/diacare.28.4.771. [DOI] [PubMed] [Google Scholar]
- 43.Carter BL. Primary Care Physician-Pharmacist Collaborative Care Model: Strategies for Implementation. Pharmacotherapy. 2016;36(4):363–73. doi: 10.1002/phar.1732. [DOI] [PubMed] [Google Scholar]
- 44.Isetts BJ, Buffington DE, Carter BL, Smith M, Polgreen LA, James PA. Evaluation of Pharmacists’ Work in a Physician-Pharmacist Collaborative Model for the Management of Hypertension. Pharmacotherapy. 2016;36(4):374–84. doi: 10.1002/phar.1727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.McLean DL, Simpson SH, McAlister FA, Tsuyuki RT. Treatment and blood pressure control in 47,964 people with diabetes and hypertension: a systematic review of observational studies. The Canadian journal of cardiology. 2006;22(10):855–60. doi: 10.1016/s0828-282x(06)70304-x. [DOI] [PMC free article] [PubMed] [Google Scholar]