Abstract
Background:
There is no difference in the functional outcomes 6 months after total knee arthroplasty (TKA) for knee osteoarthritis between patellar resurfacing and non-resurfacing. Thus, we have performed this study to compare the short-term clinical outcomes of TKA performed with and without the patella resurfacing.
Methods:
A total of 50 patients with osteoarthritis of the knee (OAK) were randomized to receive patellar resurfacing (n=24; resurfaced group) or to retain their native patella (n=26; non-resurfaced group) based on envelope selection and provided informed consent. Disease specific outcomes including Knee Society Score (KSS), Knee Society Function Score (KSKS-F), Kujala Anterior Knee Pain Scale (AKPS), Western Ontario and McMaster Universities Arthritis Index (WOMAC), Short Form 36 (SF-36), and functional patella-related activities were measured within six months of follow-up.
Results:
There was no significant difference between the resurfaced and non-resurfaced groups in pre and post-operative improvement of range of motion (ROM) (P=0.421), KSS (P=0.782, P=0.553), KSKS-F (P=0.241, P=0.293), AKPS (P=0.128, P=0.443), WOMAC (P=0.700, P=0.282), and pain scores (P=0.120, P=0.508). There was no difference in ROM between resurfaced and non-resurfaced group pre (15.24° and 15.45°) and post-operative (18.48° and 18.74). No side effects related to patella was observed in any of the groups. Revision was required in none of the participants.
Conclusion:
The results showed no significant difference between patellar resurfacing and non-resurfacing in TKA for all outcome measures in a short term.
Level of evidence: I
Keywords: Non-resurfacing, Osteoarthritis, Patellar resurfacing, Total knee arthroplasty
Introduction
Total knee arthroplasty (TKA) is the gold standard treatment for knee osteoarthritis (OAK), which involves removing the damaged articular surfaces and replacing them with a tibial and femoral component (1-4). However, there is controversy as to whether the patella should be resurfaced or not during TKA (1). While TKA is commonly used in severe degenerative OA, surgeons are not certain about indications of patellar resurfacing (2). Some authors suggest that patellar resurfacing should be done simultaneously with TKA in order to relieve pain in the front of knee and eliminate the need for a second surgery (1, 3). However, others have observed that these two techniques are not different (5-7).
The advantages of patellar non-resurfacing include lower costs due to less dependence on equipment, reduced surgery time, decreased patello-femoral complications, and greater possibility to exert pressure on patello-femoral joint without the chance of prosthesis abrasion (5, 8, 9). However, patellar resurfacing during TKA is not performed by many surgeons worldwide due to its associated complications including patellar fracture, osteonecrosis, patellar polyethylene loosening, polyethylene abrasion, instability, patellar motion difficulties and problems in extensor mechanisms (10-13). Moreover, anterior knee pain is still a common complaint in patients undergoing patellar resurfacing and therefore patellar resurfacing has been suggested not be done routinely (14).
To date, no clinical trial and/or meta-analysis studies have been able to end the debate and find out a definitive answer (1, 15-19). In addition, to the best of our knowledge no results of patellar resurfacing or non-resurfacing in TKA has been reported in Iranian patients. Hence, considering the controversy whether to resurface the patella or not, a study on this contentious topic is needed. This study was designed to compare the short term results between patellar resurfacing and non-resurfacing in patients undergoing TKA.
Materials and Methods
Patients
A total of 50 patients with OAK at two university-affiliated teaching hospitals were recruited to the current study between January 2012 and November 2013. This study was approved by the ethics committees at Tehran University of Medical Sciences, Tehran, Iran. As the sample size in this study was within those of other studies on the same topic, no power analysis was done. The eligible subjects were patients under 70 years old with non-inflammatory arthritis and unsuccessful non-surgical treatment who were scheduled for TKA. Patients with inflammatory arthritis, history of patellectomy, high tibial osteotomy, patellar fracture, varus/valgus deformity of greater than 20 degrees, or flexion contracture more than 25 degrees and extensive bone defect were excluded from the study. Patients were randomized before surgery to receive patellar resurfacing (n = 24; resurfaced group) or to retain their native patella (n = 26; non-resurfaced group) based on envelope selection and provided informed consent. Evaluations were performed pre- and postoperatively by an evaluator who was blinded to group allocation. Patients were not blinded to group allocation.
Operative technique
One of three experienced surgeons or their trainees under supervision performed the surgery. Patients were allocated into the PR and PNR groups after tibial and femoral cut. Standard surgical technique including a midline incision and medial parapatellar exposure was utilized in all patients. All surgeries were done under tourniquet pressure. The Profix™ Total Knee System, a posterior cruciate sacrificing, fixed bearing prosthesis manufactured by Zimmer Inc. was used in all subjects with cemented components. In cases where both knees needed surgery, each knee was randomized independently. PR was performed using all-polyethylene prosthesis, and PNR was achieved with osteophyte removal, electro-cauterization in the 5mm edge of the patella, and fibrillated cartilage smoothing. A standardized clinical pathway was followed ensuring all subjects received similar preoperative, perioperative and postoperative care; early mobilization was encouraged starting the first postoperative day.
Evaluations
The following clinical, functional and radiologic scores were assessed pre and postoperatively for 6 months after surgery: Knee range of motion (ROM), Knee Society Knee score (KSKS), Knee Society Function Score (KSKS-F), Western Ontario and McMaster Universities Arthritis Index (WOMAC), 36-Item Short Form Health Survey (SF-36), Kujala Anterior Knee Pain Scale (AKPS) and Visual Analogue Scale (VAS) for pain. Alignment was evaluated using knee society radiographic evaluation system in which α and β are defined as angles of femoral and tibial components in coronal section and γ and δ are defined as angles of femoral and tibial components in sagittal section. In addition, the patients’ radiographic images were scored based on the Kellgren-Lawrence six commonly used systems in both PR and PNR groups. Patients’ comorbidities, post-surgical complications, need for a second surgery, and the surgery to release lateral retinaculum were carefully documented. Other parameters such as age, gender, height, weight, and patella thickness were assessed as independent factors.
Statistical Analysis
Statistical analysis was performed using SPSS software, version 18.0 (Chicago, IL, USA). The data are presented as mean ± standard deviation. The Kolmogorov- Smirnov test was performed for normal distribution of the data. The Wilcoxon and Mann-Whitney U tests were used to compare the continuous variables. The paired t-test was used to compare the quantitative variables before and after the surgery. A P<0.05 was considered as statistically significant.
Results
A total of 50 subjects (42 women and 8 men, aged 64.8 ± 7.8 years) were randomly allocated into resurfaced (n=24) and non-resurfaced (n=26) groups. There were 11 cases of right side osteoarthritis in PR, and 13 in PNR groups; and in the left knee the number was 13 in both groups. Both PR and PNR groups showed improved ROM and other functional tests after surgery, (P≤0.001) [Table 1; Figure 1]. No significant difference were seen between the resurfaced and non-resurfaced groups in pre and post-operative improvement of ROM (P=0.421), KSKS (P=0.782, P=0.553), KSKS-F (P=0.241, P=0.293), AKPS (P=0.128, P=0.443), WOMAC (P=0.700, P=0.282), and pain scores (P=0.120, P=0.508) [Table 1]. Moreover, The mean angles evaluated by knee society radiographic evaluation system did not show any significant difference between the two groups (Table 1, T-test, P>0.05). No significant differences were seen in the baseline characteristics between the resurfaced and non-resurfaced groups, including age (P=0.92), gender (P=1.00), BMI (P=0.57) and patella thickness (P=0.46), except for the SF-36, where the NPR group showed a lower preoperative. Surgical complications were not observed during the 6-month follow-up. None of the patients in either group needed a revision surgery or lateral retinaculum release. The differences in co-morbidities between the two groups were statistically non-significant.
Table 1.
The knee function and radiographic scores
| Resurfaced Mean (SD) | Non-Resurfaced Mean (SD) | P value | ||
|---|---|---|---|---|
| KSKS score | Preop. | 26.97 (13.2) | 25.73 (13.7) | 0.782 |
| Postop. | 84.75 (6.2) | 83.46 (8.7) | 0.553 | |
| KSKS-F score | Preop. | 28.87 (21.3) | 22.08 (19.3) | 0.241 |
| Postop. | 83.75 (13.4) | 87.73 (19.2) | 0.293 | |
| AKPS score | Preop. | 34.67 (12.4) | 29.58 (10.9) | 0.128 |
| Postop. | 75.33 (11) | 72.85 (11.7) | 0.443 | |
| WOMAC score | Preop. | 70.22 (13.3) | 68.6 (15.8) | 0.700 |
| Postop. | 23.80 (16.7) | 18.79 (15.7) | 0.282 | |
| SF-36 score | Preop. | 47.86 (18) | 35.31 (14.5) | 0.009* |
| Postop. | 79.12 (15) | 69.36 (18.8) | 0.049* | |
| Pain VAS Score | Preop. | 8.67 (0.9.) | 8.15 (1.3) | 0.120 |
| Postop. | 1.5 (0.7) | 1.6 (0.9) | 0.508 | |
| Range of motion | Preop. | 15.24 | 15.45 | 0.421 |
| Postop. | 21.48 | 21.74 | 0.271 | |
| Radiographic findings | α | 96.71 (1.5) | 96.8 (1.5) | 0.743 |
| β | 87.69 (2) | 87.54 (2.3) | 0.882 | |
| γ | 2.37 (1.3) | 2.36 (1.4) | 0.98 | |
| Δ | 87.81 (1.6) | 87.92 (1.9) | 0.827 | |
The values are meaning (±SD). KSKS, the Knee Society Knee score; KSKS-F, Knee Society Function score; AKPS, Kujala AnteriorKnee Pain Scale; WOMAC, Western Ontario and McMaster Universities Arthritis Index; SF-36, Short Form 36.
Figure 1.
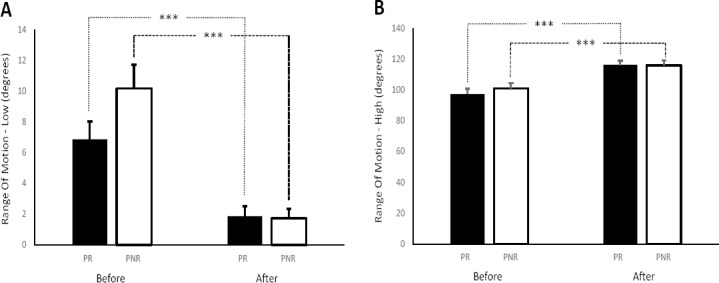
Mean ROM-Low (A) and ROM-high (B) before and after surgery.
Discussion
TKA is one option to relieve pain and to restore function to an arthritic knee (1, 5, 6). The most common reason for knee replacement is that other treatments such as: weight loss, exercise/physical therapy, medicines, and injections have failed to relieve arthritis-associated knee pain. The decision to resurface the patella during TKA remains controversial (7-9). We have performed this clinical trial study to examine the efficacy and short term outcomes of TKA with and without patellar resurfacing. But, we have not any difference between the resurfacing group and the non-resurfacing group in terms of short term efficacy including ROM, KSS, KSKS-F, AKPS, and WOMAC.
Our study had two limitations should be pointed out. First, the number of patients was low and this brings the concern of type II error, which indicates that the non-significant differences between the two groups may be a consequence of small sample size. Second, considering the fact that sometimes the complications occur years after the surgery, our follow up period was relatively short. Hence, we are going to continue to follow the patients for another four years. However, we do not believe that these limitations undermine the main findings of this study.
In this study we have found that TKA in both PR and NPR groups improved KSKS and KSKS-F, however, there is no difference between these two methods in the level of improvement, which is in agreement with the studies of Pavlou et al., Burnett et al. and others (5, 15, 16, 20-24). Nevertheless, in the studies of Schoroed et al. and Waters et al., KSKS was better in PR than PNR group, while the KSKS-F was equal (11, 22). Nizard et al. and Parvizi et al. reported significantly higher scores in both KSKS and KSKS-F in the PR group compared to PNR (25, 26). We could not reject the null hypothesis to show any difference between PR and PNR. The reasons for inability to reject the null hypothesis are small sample size, and bias in sample selection. Moreover, we have found that the minimum range of motion improved to about 5-8 degrees in both groups, though the difference was not significant between the two groups. In addition, the maximum range of motion after surgery was improved to 15-18 degrees in both groups, again with no significant difference in intergroup analysis. Meftah et al. and Burnett et al also reported similar results (15, 27).
In this study, we found a non-significant lower mean functional score in resurfaced group than non-resurfaced. In a meta-analysis of 7 studies, Arirachakaran et al. also showed non-significant lower functional score in patellar resurfacing (609 patients) compared with non-resurfacing (660 patients). However, there was a high and significant heterogeneity between the 7 studies reporting the KSS function score (28). Van Hemert et al. (2009) reported that patients undergoing resurfacing in TKR had a functional advantage over the non-resurfaced cases (27). According to our finding, the non-resurfaced group showed a borderline improvement in Knee Society Function Score compared to the patellar resurfacing groups.
In the present study the Kujala score was improved equally in both groups postoperatively. One of the limitations of this scoring is that the patient may feel no pain in higher scores, as for example 74.6, in the study by Metsna; thus, its inference should be done deliberately (29). The WOMAC score is inversely related to the patient’s conditions. Knee arthroplasty in both groups reduced WOMAC, with no difference between the PR and PNR groups. This finding is comparable to the studies of Campell et al. and Beaupre et al. (16, 30). Additionally, we have found an increased SF-36 score and a reduced pain score after surgery in both groups similar to the report by Beaupre et al., both the changes were not different between the two groups (31).
Although not statistically significant, the patients in PR group reported more pain when climbing the stairs. It has been previously explained that cauterization around the patella results in reduction of anterior knee pain and better patient satisfaction after surgery (23). We also applied cauterization around the patella in non-resurfacing cases, which might have contributed to pain relief. In studies of Campell et al. and Parry et al., similar to our study, the outcomes of pain reduction were not different between the groups (16, 22). In most studies, anterior knee pain has been assessed after knee arthroplasty; but, in this study it was evaluated as a whole. The results of anterior knee pain score in the literature are confusing. Some studies did not report any difference between the PR and PNR groups, while others show lower pain in either PR or PNR approach (1, 13, 14, 18, 24, 32-34). In addition, in radiographic evaluations, the α, β, γ and δ angles in PR and PNR groups were in accordance with other studies including the reports by Bae et al. and Bach et al., where the angles were not statistically different between groups (35, 36).
In this study, no patella-related complications was observed, neither in PR, nor in PNR group which is in accordance with the study by Meftah et al. (27). Revision was needed in none of the groups in our study; in contrast, Beaupre et al. and Campell et al. performed two revisions in PNR and one in PR groups during the 10-year follow-up (16, 31). It appears that some patients with PNR approach suffered from anterior knee pain; and the revision was implemented not because of the patellofemoral complications, but to control the anterior knee pain. The meta-analysis by Stephan et al showed that occurrence of revision surgery is equal in PR and PNR groups but some other reports suggest less need for revision surgery in PR groups (15, 20). In our study, an accurate judgment could not be made due to the short follow-up period.
In conclusion, this prospective randomized study showed that TKA is an effective procedure with considerable improvements in patients’ pain and function. However, there is no difference between the resurfacing and the non-resurfacing in terms of short term efficacy including pain and function.
References
- 1.Wood DJ, Smith AJ, Collopy D, White B, Brankov B, Bulsara MK. Patellar resurfacing in total knee arthroplasty: a prospective, randomized trial. J Bone Joint Surg Am. 2002;84-A(2):187–93. doi: 10.2106/00004623-200202000-00004. [DOI] [PubMed] [Google Scholar]
- 2.Forster MC. Patellar resurfacing in total knee arthroplasty for osteoarthritis: a systematic review. Knee. 2004;11(6):427–30. doi: 10.1016/j.knee.2004.03.006. [DOI] [PubMed] [Google Scholar]
- 3.Sobhan MR, Mehdinejad M, Jamaladini MH, Mazaheri M, Zare-Shehneh M, Neamatzadeh H. Association between aspartic acid repeat polymorphism of the asporin gene and risk of knee osteoarthritis: a systematic review and meta-analysis. Acta Orthop Traumatol Turc. 2017;51(5):409–15. doi: 10.1016/j.aott.2017.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yazdi MM, Jamalaldini MH, Sobhan MR, Jafari M, Mazaheri M, Zare-Shehneh M, et al. Association of ESRαgene Pvu II T>C, XbaI A>G and BtgI G>A polymorphisms with knee osteoarthritis susceptibility: a systematic review and meta-analysis based on 22 case-control studies. Arch Bone Jt Surg. 2017;5(6):351–62. [PMC free article] [PubMed] [Google Scholar]
- 5.Barrack RL, Wolfe MW. Patellar resurfacing in total knee arthroplasty. J Am Acad Orthopaed Surg. 2000;8(2):75–82. doi: 10.5435/00124635-200003000-00001. [DOI] [PubMed] [Google Scholar]
- 6.Fu Y, Wang G, Fu Q. Patellar resurfacing in total knee arthroplasty for osteoarthritis: a meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2011;19(9):1460–6. doi: 10.1007/s00167-010-1365-0. [DOI] [PubMed] [Google Scholar]
- 7.He JY, Jiang LS, Dai LY. Is patellar resurfacing superior than nonresurfacing in total knee arthroplasty?A meta-analysis of randomized trials. Knee. 2011;18(3):137–44. doi: 10.1016/j.knee.2010.04.004. [DOI] [PubMed] [Google Scholar]
- 8.Epinette JA, Manley MT. Outcomes of patellar resurfacing versus nonresurfacing in total knee arthroplasty: a 9-year experience based on a case series of scorpio PS knees. J Knee Surg. 2008;21(4):293–8. doi: 10.1055/s-0030-1247835. [DOI] [PubMed] [Google Scholar]
- 9.Ong K, Lau E, Manley M, Kurtz SM. Patient, hospital, and procedure characteristics influencing total hip and knee arthroplasty procedure duration. J Arthroplasty. 2009;24(6):925–31. doi: 10.1016/j.arth.2008.07.002. [DOI] [PubMed] [Google Scholar]
- 10.Huang CH, Liau JJ, Ho FY, Lin CY, Young TH, Cheng CK. Polyethylene failure of the patellar component in New Jersey low-contact stress total knee arthroplasties. J Arthroplasty. 2005;20(2):202–8. doi: 10.1016/j.arth.2004.08.001. [DOI] [PubMed] [Google Scholar]
- 11.Ortiguera CJ, Berry DJ. Patellar fracture after total knee arthroplasty. J Bone Joint Surg Am. 2002;84-A(4):532–40. doi: 10.2106/00004623-200204000-00004. [DOI] [PubMed] [Google Scholar]
- 12.Newman JH, Ackroyd CE, Shah NA, Karachalios T. Should the patella be resurfaced during total knee replacement? Knee. 2000;7(1):17–23. [Google Scholar]
- 13.Waters TS, Bentley G. Patellar resurfacing in total knee arthroplasty. A prospective, randomized study. J Bone Joint Surg Am. 2003;85-A(2):212–7. doi: 10.2106/00004623-200302000-00005. [DOI] [PubMed] [Google Scholar]
- 14.Kim BS, Reitman RD, Schai PA, Scott RD. Selective patellar nonresurfacing in total knee arthroplasty. 10 year results. Clin Orthop Relat Res. 1999;367(1):81–8. [PubMed] [Google Scholar]
- 15.Burnett RS, Boone JL, Rosenzweig SD, Steger-May K, Barrack RL. Patellar resurfacing compared with nonresurfacing in total knee arthroplasty. A concise follow-up of a randomized trial. J Bone Joint Surg Am. 2009;91(11):2562–7. doi: 10.2106/JBJS.H.00109. [DOI] [PubMed] [Google Scholar]
- 16.Campbell DG, Duncan WW, Ashworth M, Mintz A, Stirling J, Wakefield L, et al. Patellar resurfacing in total knee replacement: a ten-year randomised prospective trial. J Bone Joint Surg Am. 2006;88(6):734–9. doi: 10.1302/0301-620X.88B6.16822. [DOI] [PubMed] [Google Scholar]
- 17.Bourne RB, Burnett RS. The consequences of not resurfacing the patella. Clin Orthop Relat Res. 2004;428(1):166–9. doi: 10.1097/01.blo.0000147137.05927.bf. [DOI] [PubMed] [Google Scholar]
- 18.Calvisi V, Camillieri G, Lupparelli S. Resurfacing versus nonresurfacing the patella in total knee arthroplasty: a critical appraisal of the available evidence. Arch Orthop Trauma Surg. 2009;129(9):1261–70. doi: 10.1007/s00402-008-0801-9. [DOI] [PubMed] [Google Scholar]
- 19.Li S, Chen Y, Su W, Zhao J, He S, Luo X. Systematic review of patellar resurfacing in total knee arthroplasty. Int Orthopaed. 2011;35(3):305–16. doi: 10.1007/s00264-010-1109-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pavlou G, Meyer C, Leonidou A, As-Sultany M, West R, Tsiridis E. Patellar resurfacing in total knee arthroplasty: does design matter?A meta-analysis of 7075 cases. J Bone Joint Surg Am. 2011;93(14):1301–9. doi: 10.2106/JBJS.J.00594. [DOI] [PubMed] [Google Scholar]
- 21.Feller JA, Bartlett RJ, Lang DM. Patellar resurfacing versus retention in total knee arthroplasty. J Bone Joint Surg Br. 1996;78(2):226–8. [PubMed] [Google Scholar]
- 22.Parry MC, Smith AJ, Blom AW. Early death following primary total knee arthroplasty. J Bone Joint Surg Am. 2011;93(10):948–53. doi: 10.2106/JBJS.J.00425. [DOI] [PubMed] [Google Scholar]
- 23.van Jonbergen H, Scholtes V, van Kampen A, Poolman RW. A randomised, controlled trial of circumpatellar electrocautery in total knee replacement without patellar resurfacing. J Bone Joint Surg. 2011;98(3):1054–9. doi: 10.1302/0301-620X.93B8.26560. [DOI] [PubMed] [Google Scholar]
- 24.Schroeder-Boersch H, Scheller G, Fischer J, Jani L. Advantages of patellar resurfacing in total knee arthroplasty. Two-year results of a prospective randomized study. Arch Orthop Trauma Surg. 1998;117(1-2):73–8. doi: 10.1007/BF00703446. [DOI] [PubMed] [Google Scholar]
- 25.Nizard RS, Biau D, Porcher R, Ravaud P, Bizot P, Hannouche D, et al. A meta-analysis of patellar replacement in total knee arthroplasty. Clin Orthop Relat Res. 2005;432(1):196–203. doi: 10.1097/01.blo.0000150348.17123.7f. [DOI] [PubMed] [Google Scholar]
- 26.Parvizi J, Rapuri VR, Saleh KJ, Kuskowski MA, Sharkey PF, Mont MA. Failure to resurface the patella during total knee arthroplasty may result in more knee pain and secondary surgery. Clin Orthop Relat Res. 2005;438(1):191–6. doi: 10.1097/01.blo.0000166903.69075.8d. [DOI] [PubMed] [Google Scholar]
- 27.Meftah M, Ranawat AS, Ranawat CS. Ten-year follow-up of a rotating-platform, posterior-stabilized total knee arthroplasty. J Bone Joint Surg Am. 2012;94(5):426–32. doi: 10.2106/JBJS.K.00152. [DOI] [PubMed] [Google Scholar]
- 28.Arirachakaran A, Sangkaew C, Kongtharvonskul J. Patellofemoral resurfacing and patellar denervation in primary total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2015;23(6):1770–81. doi: 10.1007/s00167-014-3311-z. [DOI] [PubMed] [Google Scholar]
- 29.Metsna V, Vorobjov S, Martson A. Prevalence of anterior knee pain among patients following total knee arthroplasty with nonreplaced patella: a retrospective study of 1778 knees. Medicina. 2014;50(2):82–6. doi: 10.1016/j.medici.2014.06.001. [DOI] [PubMed] [Google Scholar]
- 30.van Hemert WL, Senden R, Grimm B, Kester AD, van der Linde MJ, Heyligers IC. Patella retention versus replacement in total knee arthroplasty;functional and clinometric aspects. Arch Orthop Trauma Surg. 2009;129(2):259–65. doi: 10.1007/s00402-008-0640-8. [DOI] [PubMed] [Google Scholar]
- 31.Beaupre L, Secretan C, Johnston DW, Lavoie G. A randomized controlled trial comparing patellar retention versus patellar resurfacing in primary total knee arthroplasty 5-10 year follow-up. BMC Res Notes. 2012;5(1):273. doi: 10.1186/1756-0500-5-273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pilling RW, Moulder E, Allgar V, Messner J, Sun Z, Mohsen A. Patellar resurfacing in primary total knee replacement: a meta-analysis. J Bone Joint Surg Am. 2012;94(24):2270–8. doi: 10.2106/JBJS.K.01257. [DOI] [PubMed] [Google Scholar]
- 33.Meneghini RM. Should the patella be resurfaced in primary total knee arthroplasty?An evidence-based analysis. J Arthroplasty. 2008;23(7 Suppl):11–4. doi: 10.1016/j.arth.2008.06.009. [DOI] [PubMed] [Google Scholar]
- 34.Bourne RB, Rorabeck CH, Vaz M, Kramer J, Hardie R, Robertson D. Resurfacing versus not resurfacing the patella during total knee replacement. Clin Orthop Relat Res. 1995;321(1):156–61. [PubMed] [Google Scholar]
- 35.Bae DK, Cho SD, Im SK, Song SJ. Comparison of midterm clinical and radiographic results between total knee arthroplasties using medial pivot and posterior-stabilized prosthesis-a matched pair analysis. J Arthroplasty. 2016;31(2):419–24. doi: 10.1016/j.arth.2015.09.038. [DOI] [PubMed] [Google Scholar]
- 36.Bach CM, Mayr E, Liebensteiner M, Gstottner M, Nogler M, Thaler M. Correlation between radiographic assessment and quality of life after total knee arthroplasty. Knee. 2009;16(3):207–10. doi: 10.1016/j.knee.2008.11.003. [DOI] [PubMed] [Google Scholar]


