Abstract
Lateral Ankle sprain (LAS) is a common sports injury associated with recurrent ankle sprain, chronic ankle instability (CAI) and post-traumatic ankle osteoarthritis (PTOA). Platelet Rich Plasma (PRP) has been increasingly used for herapeutic applications in sports-related injuries, and is thought to stimulate tissue healing. We reported a case of LAS with complete tear of anterior talofibular ligament, which showed complete healing of ligament and early ankle stabilization after PRP. The healing is supported by dynamic ultrasound images and magnetic resonance imaging. We therefore proposed that PRP may serve as an alternative non-surgical treatment option in LAS in future research, with the potential to prevent the development of CAI and PTOA.
Level of evidence: IV
Keywords: Anterior talofibular ligament tear, Case reports, Lateral ankle sprain, Platelet rich plasma, Ultrasound
Introduction
Lateral ankle sprain (LAS) is the most common musculoskeletal injury in the physically active population; it is also a common condition in the general population (1). Apart from the pain and temporary period of reduced functioning and disability, it is also associated with increased risk of recurrent ankle sprain, the development of chronic ankle stability (CAI) and post-traumatic ankle osteoarthritis (PTOA). While the direct costs for treatment of an isolated LAS are relatively low, compounding these are indirect costs from follow up care, loss of productivity, time loss of activity and care of its long-term consequences. Therefore, it becomes apparent that the healthcare burden that emerges from so called “simple” LAS is substantial.
Conservative management and early functional rehabilitation remain to be the standard of care for all grades of LAS. Platelet-rich plasma (PRP) is an autologous derivative of whole blood that stimulates a supra-physiological release of growth factors to jump start healing in chronic injuries. Growth factors are released from the alpha granules of platelets which induce chemotaxis, cell migration, angiogenesis, proliferation, differentiation and matrix production (2, 3). PRP is progressively emerging at the forefront of sports and rehabilitation medicine, and its role in different soft injuries has become the focus of research in recent years.
Despite the popularity of PRP research, little was known about its role in the management of LAS. Therefore, we reported a case of high grade LAS with complete tear of the left anterior talofibular ligament (ATFL), its speedy healing and the early achievement of ankle stability after a single injection of PRP. The healing progress was supported by dynamic ultrasound and magnetic resonance imaging (MRI).
Patient information
Consent for this publication has been obtained from the patient.
This is a case of a 39 years old enthusiastic runner who sprained his left ankle on 13th March 2016. He first consulted his family doctor on 14th March with prescription of oral analgesics and a referral of physiotherapy. However, he was eager to recover soon for his running; therefore, he was referred to us on 22nd of March 2016 for the consideration of PRP injection. His pain improved after a week of oral analgesic and rest. Physical examination found significant swelling over the left lateral ankle with moderate tenderness and ecchymosis. The talar tilt test was positive, which signified lateral ankle laxity.
Diagnostic assessment
MRI was done on 15th March 2016 which confirmed the complete tear of ATFL with small to medium joint effusion; other ligaments and tendons were intact [Figure 1a]. Ultrasound was performed on 22nd March which showed significant discontinuation of compact fibrillar pattern of the ATFL compatible with complete tear. On dynamic scanning with left ankle inversion, there was gapping of the discontinuation of ligament and laxity was clearly demonstrated [Figure 1b; Video 1].
Figure 1a.
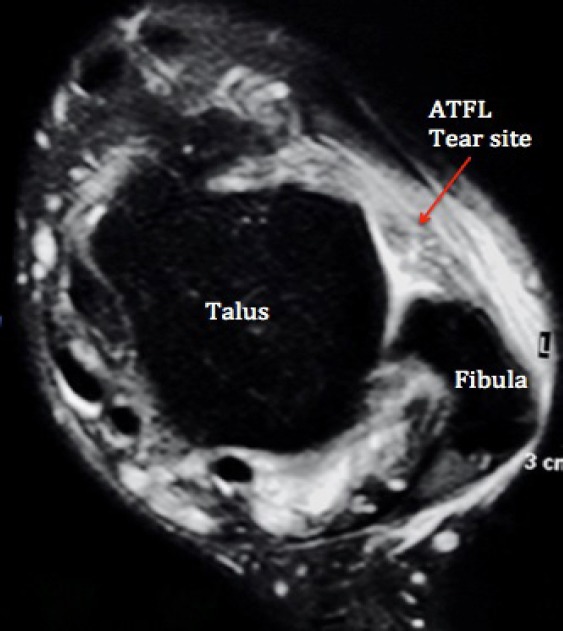
Baseline MRI of ATFL before PRP injection.$$$
MRI: Magnetic Resonance Imaging; ATFL: Anterior Talofibular Ligament; PRP: Platelet Rich Plasma; USG: Ultrasou
Figure 1b.
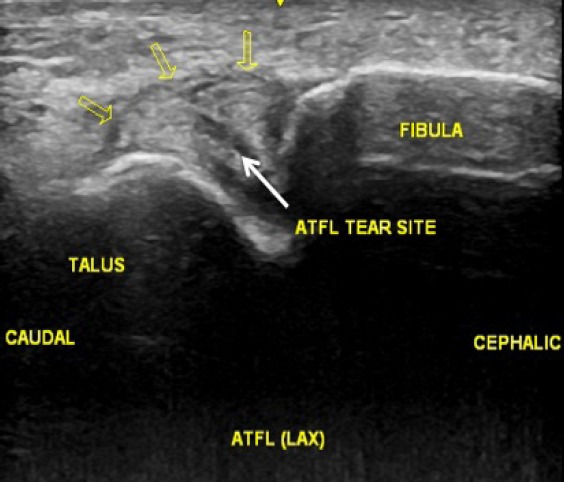
Baseline USG of the ATFL before PRP injection
Intervention
PRP injection was conducted on 24th March with Harvest SmartPrep System. 30 ml venous blood was drawn and the blood product was then put into the centrifuge machine for centrifugation. Three ml of PRP was harvested and used for injection. Before the PRP injection, 0.5 ml of 10% Calcium Chloride was injected prior to the injection to activate the PRP; after that, three ml of the PRP was injected under ultrasound guidance to the tear site of the ATFL. A cast was used to immobilize the ankle for four weeks and patient was advised to have non-weight bearing walking.
Follow up and outcomes
The patient was followed up four weeks after the PRP injection. No adverse side effect was reported. Dynamic ultrasound scan showed no more gapping at the tear site [Video 2]. The cast was removed and he was advised to start active ankle mobilization exercise. At eight-week post PRP injection, dynamic ultrasound scan confirmed the absence of ATFL laxity and gapping, and the patient started on simple jogging activity [Video 3]. The patient was last seen on 19th August, around six months after the initial injury. There was no more ankle pain and he was running one hour every day without any sense of instability. Repeated USG showed healed ATFL [Figure 1c]. MRI was repeated on 25th August which showed that the ATFL was thickened to about twice the normal thickness because of healing, and the overall continuity was well maintained [Figure 1d].
Figure 1c.
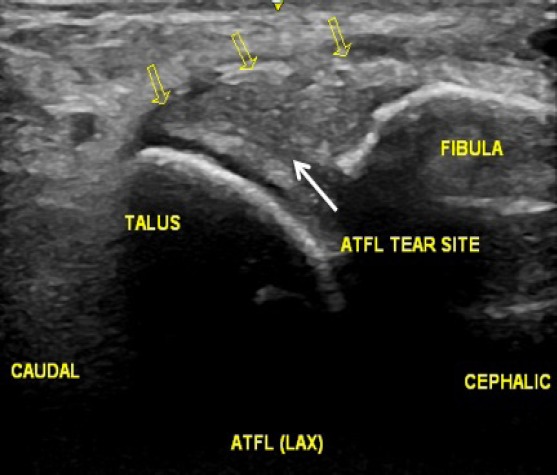
USG of ATFL 6-month post PRP injection.
Figure 1d.
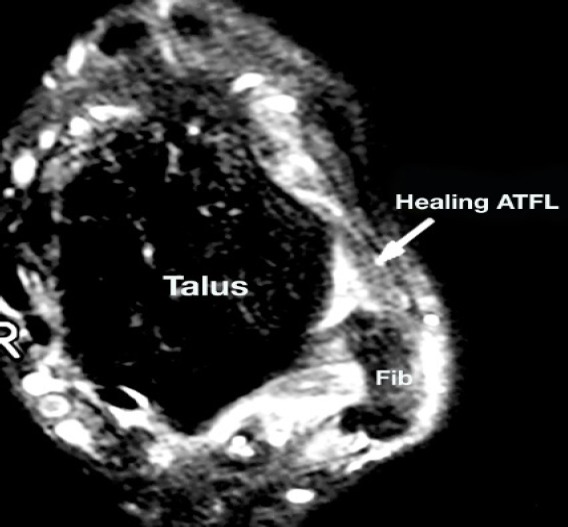
MRI of ATFL 6-month post PRP injection.
Discussion
Lateral ligament insufficiency secondary to LAS is one of the most frequently encountered musculoskeletal injuries. Despite the high prevalence and severity of lifestyle-limiting symptoms that follow the acute episode, LAS is often considered as an innocuous injury that will heal expediently and many patients received neither supervised nor professional administered care (4, 5). It has been reported that up to 70% of individuals with history of ankle sprain have some type of residual and chronic symptoms, recurrent ankle sprains and perceived instability (6, 7). A recent large longitudinal prospective study has examined the onset of sensorimotor deficits following a LAS, and has demonstrated that CAI may begin shortly after the acute sprain injury, with postural control deficits and multiple aberrant movement patterns during a variety of functional tasks (8). The chronic joint instability together with the osteochondral lesions eventually may lead to the development of PTOA, along with decreases in physical activity levels and health-related quality of life (9-11).
Conservative management and early functional rehabilitation remain to be the standard of care for all grades of LAS (12). However, the negative consequences of LAS are concerning, and improved efforts to address these conditions is essential. In view of this, the International Ankle Consortium had presented the Consensus Statement in 2016 which established the burden of LAS and its mid-term and long-term consequences, and called for prevention and early management of LAS. It also encouraged research to determine the optimal treatment of LAS with ultimate goal to improve global musculoskeletal health. It is believed that timely intervention and early restoration of biomechanical deficits will be the optimal treatment of LAS and prevention of CAI and PTOA (13).
The clinical evidence of PRP on soft tissue healing and repair is so far convincing. Case series have shown the beneficial effect on the partial thickness rotator cuff tear (14). Randomized controlled trial has demonstrated positive effect of PRP on patella tendinopathy and the strongest level one evidence of PRP is found in the management of refractory tennis elbow with long term pain reduction and functional improvement (15, 16). A systematic review (SR) conducted in 2014 evaluated the role of PRP in different foot and ankle pathologies; however, all the seventeen included studies did not include LAS as the pathology for treatment (17).
The strength of the current case report is that the healing of ATFL was supported with ultrasound and MRI images, and early ankle stabilization was supported with dynamic ultrasound images. Our results add to the growing evidence of PRP on soft tissue healing; we also suggest the possible beneficial effect of PRP in regaining ligamentous strength, reducing ligament laxity and achieving early ankle stability, which are essential elements in the management of LAS. Future randomized controlled trials may consider evaluating the long-term ankle stability in LAS after PRP, its use in different severity of ankle sprain, and the role of it versus surgical reconstruction in complete ATFL tear refractory to conservative management.
Our report suggested that PRP not only allows healing of the torn ligament, but also hastens its strength recovery. We believed that together with appropriate rehabilitation training, PRP may enhance early ankle stabilization in LAS, prevent the development of CAI and PTOA; it may also serve as an alternative non-surgical treatment option in the management of high grade LAS not responding to conservative therapy.
An inform written consent was obtained from the study participant.
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
References
- 1.Doherty C, Delahunt E, Caulfield B, Hertel J, Ryan J, Bleakley C. The incidence and prevalence of ankle sprain injury: a systematic review and meta-analysis of prospective epidemiological studies. Sports Med. 2014;44(1):123–40. doi: 10.1007/s40279-013-0102-5. [DOI] [PubMed] [Google Scholar]
- 2.Boswell SG, Cole BJ, Sundman EA, Karas V, Fortier LA. Platelet-rich plasma: a Milieu of bioactive factors. Arthroscopy. 2012;28(3):429–39. doi: 10.1016/j.arthro.2011.10.018. [DOI] [PubMed] [Google Scholar]
- 3.Lyras DN, Kazakos K, Tilkeridis K, Kokka A, Ververidis A, Botaitis S, et al. Temporal and spatial expression of tgf-b1 in the early phase of patellar tendon healing after application of platelet rich plasma. Arch Bone Jt Surg. 2016;4(2):156–60. [PMC free article] [PubMed] [Google Scholar]
- 4.Kaminski TW, Hertel J, Amendola N, Docherty CL, Dolan MG, Hopkins JT, et al. National athletic trainers'association position statement: conservative management and prevention of ankle sprains in athletes. J Athl Train. 2013;48(4):528–45. doi: 10.4085/1062-6050-48.4.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McKay GD, Goldie PA, Payne WR, Oakes BW. Ankle injuries in basketball: injury rate and risk factors. Br J Sports Med. 2001;35(2):103–8. doi: 10.1136/bjsm.35.2.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Anandacoomarasamy A, Barnsley L. Long term outcomes of inversion ankle injuries. Br J Sports Med. 2005;39(3):e14. doi: 10.1136/bjsm.2004.011676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Konradsen L, Bech L, Ehrenbjerg M, Nickelsen T. Seven years follow-up after ankle inversion trauma. Scand J Med Sci Sports. 2002;12(3):129–35. doi: 10.1034/j.1600-0838.2002.02104.x. [DOI] [PubMed] [Google Scholar]
- 8.Doherty C, Bleakley C, Hertel J, Caulfield B, Ryan J, Delahunt E. Recovery from a first-time lateral ankle sprain and the predictors of chronic ankle instability: a prospective cohort analysis. Am J Sports Med. 2016;44(4):995–1003. doi: 10.1177/0363546516628870. [DOI] [PubMed] [Google Scholar]
- 9.Golditz T, Steib S, Pfeifer K, Uder M, Gelse K, Janka R, et al. Functional ankle instability as a risk factor for osteoarthritis: using T2-mapping to analyze early cartilage degeneration in the ankle joint of young athletes. Osteoarthritis Cartilage. 2014;22(10):1377–85. doi: 10.1016/j.joca.2014.04.029. [DOI] [PubMed] [Google Scholar]
- 10.Hubbard-Turner T, Wikstrom EA, Guderian S, Turner MJ. An acute lateral ankle sprain significantly decreases physical activity across the lifespan. J Sports Sci Med. 2015;14(3):556–61. [PMC free article] [PubMed] [Google Scholar]
- 11.Arnold BL, Wright CJ, Ross SE. Functional ankle instability and health-related quality of life. J Athl Train. 2011;46(6):634–41. doi: 10.4085/1062-6050-46.6.634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Doherty C, Bleakley C, Delahunt E, Holden S. Treatment and prevention of acute and recurrent ankle sprain: an overview of systematic reviews with meta-analysis. Br J Sports Med. 2016;51(2):113–25. doi: 10.1136/bjsports-2016-096178. [DOI] [PubMed] [Google Scholar]
- 13.Gribble PA, Bleakley CM, Caulfield BM, Docherty CL, Fourchet F, Fong DT, et al. Evidence review for the 2016 International Ankle Consortium consensus statement on the prevalence, impact and long-term consequences of lateral ankle sprains. >Br J Sports Med. 2016;50(24):1496–1505. doi: 10.1136/bjsports-2016-096189. [DOI] [PubMed] [Google Scholar]
- 14.Zafarani Z, Mirzaee F, Guity M, Aslani H. Clinical results of platelet-rich plasma for partial thickness rotator cuff tears: a case series. Arch Bone Jt Surg. 2017;5(5):328–31. [PMC free article] [PubMed] [Google Scholar]
- 15.Dragoo JL, Wasterlain AS, Braun HJ, Nead KT. Platelet-rich plasma as a treatment for patellar tendinopathy a double-blind, randomized controlled trial. Am J Sports Med. 2014;42(3):610–8. doi: 10.1177/0363546513518416. [DOI] [PubMed] [Google Scholar]
- 16.Mishra AK, Skrepnik NV, Edwards SG, Jones GL, Sampson S, Vermillion DA, et al. Efficacy of platelet-rich plasma for chronic tennis elbow: a double-blind, prospective, multicenter, randomized controlled trial of 230 patients. Am J Sports Med. 2014;42(2):463–71. doi: 10.1177/0363546513494359. [DOI] [PubMed] [Google Scholar]
- 17.Vannini F, Di Matteo B, Filardo G, Kon E, Marcacci M, Giannini S. Platelet-rich plasma for foot and ankle pathologies: a systematic review. Foot Ankle Surg. 2014;20(1):2–9. doi: 10.1016/j.fas.2013.08.001. [DOI] [PubMed] [Google Scholar]


