Abstract
Context:
Carpal tunnel syndrome (CTS) is one of the musculoskeletal disorders that is often described as an occupational hazard, including occupations involving computer use. However, clear consensus is lacking as far as the association between the use of computer and risk of possible CTS is concerned.
Aim:
To assess the association between CTS and computer use.
Settings and Design:
A case-control study.
Materials and Methods:
A sample size of 411 (137 cases and 274 controls) was calculated using Epi Info (version 6). Thus, 137 confirmed cases of CTS and 274 controls (matched for age and sex) were studied using a structured questionnaire.
Statistical Analysis Used:
Odds ratio (OR) with 95% confidence interval was calculated between the two groups to analyze the association. For control of confounding factors, logistic regression analysis was done.
Results:
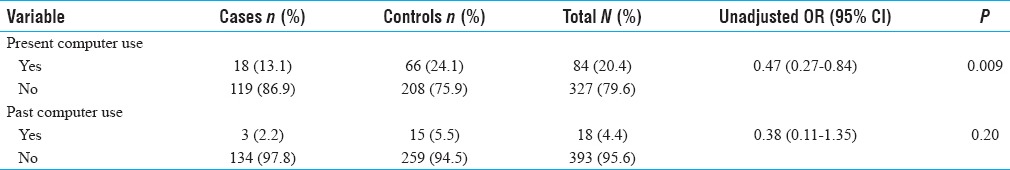
Current use of computer was found to be significantly higher in controls rather than cases (OR = 0.47, CI = 0.27–0.84, P = 0.009). Similarly, past use of computer was also found to be higher in controls. However, the difference was not statistically significant (OR = 0.38, CI = 0.11–1.35, P = 0.20). On applying logistic regression, variables found to be significantly associated with CTS were education (OR = 0.79, CI = 0.66–0.94, P = 0.01), obesity (OR = 3.11, 95%CI = 1.92–5.04, P = 0.00), and short stature (OR = 1.06, 95%CI = 1.02–1.1, P = 0.00). Although current use of computer (OR = 0.33, CI = 0.16–0.67, P = 0.00) was significantly associated with CTS in multivariate model, OR of value less than one does not indicate positive association between this variable and CTS.
Conclusion:
The study did not demonstrate any positive association between computer use and CTS.
Keywords: Carpal tunnel syndrome, computer use, education, obesity, short stature
INTRODUCTION
Carpal tunnel syndrome (CTS) is the most common peripheral nerve compression disorder in adult population accounting for 90% of all entrapment neuropathies.[1,2] Additionally, CTS is one of the musculoskeletal disorders that is often described as an occupational hazard, including occupations involving computer use.[3,4,5,6,7] Census 2011 revealed that more than 23 million households (9.4%) in India have a computer in their house.[8] In the year 2016, country's total number of Internet users was about 462 million, which was 13.5% of world Internet users.[9]
Looking at the huge population working on computers as well as accessing Internet, upper limb nerve injuries such as CTS may emerge out as a common disorder, if it is related to computer use. High rates of repetitive movement of the wrists, working with bent wrists, forceful hand motions, and improper rests of the hands and wrists may result in CTS in computer operators. There are several studies done to find out the relationship between CTS and computer use.[4,5,6,7,10,11,12,13,14,15] However, clear consensus is lacking as far as the association between use of computer and risk of possible CTS is concerned. Hence, this study was conducted with the aim to assess this association.
PATIENTS AND METHODS
This was a case-control study. All confirmed cases of CTS reported at K M Patel School of Physiotherapy, Gujarat were included in the study as cases. Patients attending the same institute, patients attending other OPDs or relatives of patients admitted in attached hospital, not suffering from CTS and matched for age and sex were included as controls.
Putting confidence level at 95%, power at 80%, control to case ratio at 2, expected frequency of exposure in control group at 20%, and closest value of Odds Ratio (OR) to be detected at 2, in sample size calculator of Epi Info (version 6), the sample size turned out to be 411 (137 cases and 274 controls). All the confirmed cases of CTS were enrolled in the study after their consent, as and when they report in KMPIP till the desired sample size was achieved. For every case included in the study, we selected two controls from above-mentioned group after matching for age and sex.
The case definition of CTS was:
Patient having:
tingling/numbness and/or pain in radial 3½ digits of hand that may worsen at night and may relieved by shaking the affected hand, with or without presence of decreased grip strength of the affected hand and thenar muscle atrophy, and
positive median nerve compression test (sensitivity: 0.87 and specificity: 0.9)[16] and
-
presence of any of the following electro-diagnostic criteria:[17]
- Distal median motor latency more than 4.4 milliseconds (ms);
- Difference between distal motor latency of median and ulnar nerves more than 1.1 ms;
- Difference between distal sensory latency of median and ulnar nerves more than 0.2 ms.
Procedure of nerve conduction study
The participants were comfortably seated on a couch with hands supported on pillow. The skin was cleaned and prepared; the electrodes were secured with gel for optimal conduction. Motor and sensory nerve conduction studies were carried out for both hands. Infrared lamp was used to maintain the temperature when it was cold. Bilateral median and ulnar nerves were studied for motor and sensory components.
Obesity was considered when BMI was ≥25 as per the WHO classification for Asian adults.[18] Short stature was considered when participant's height was less than 150 cm.
Current use of computer was considered when the respondent has used desktop computer for at least one year from the day of inquiry. Similarly, past use of computer was considered when the respondent has used desktop computer for at least one year, but he/she has stopped using it for more than six months from the day of inquiry. Use of laptop was not considered as computer use for the present study.
Data collection
An informed written consent was taken from all the participants found eligible and only those who agree to participate were enrolled in the study. The relevant information was collected using a structured questionnaire. The questionnaire was pretested and pilot-tested before its administration to the study participants.
Statistical analysis
Odds ratio (OR) with 95% confidence interval was calculated between the two groups to analyze the association. For control of confounding factors, logistic regression analysis was done. The study was approved by Institutional Ethics Committee of H. M. Patel Center for Medical Care and Education, Karamsad, Gujarat.
RESULTS
The present study included 137 cases and 274 controls with a case-control ratio of 1:2. The mean age of cases was 47.6 ± 10.96 years (range, 18–80), while that of controls was 47.5 ± 10.887 (range, 20–80). A total of 324 (78.8%) females and 87 (21.2%) males participated in the study. Being matched for age and sex, cases and controls did not show any statistically significant difference regarding distribution of these two variables [Table 1]. Majority of cases and controls were educated above secondary level as depicted in Table 1.
Table 1.
Distribution of cases and controls according to socio.demographic characteristics
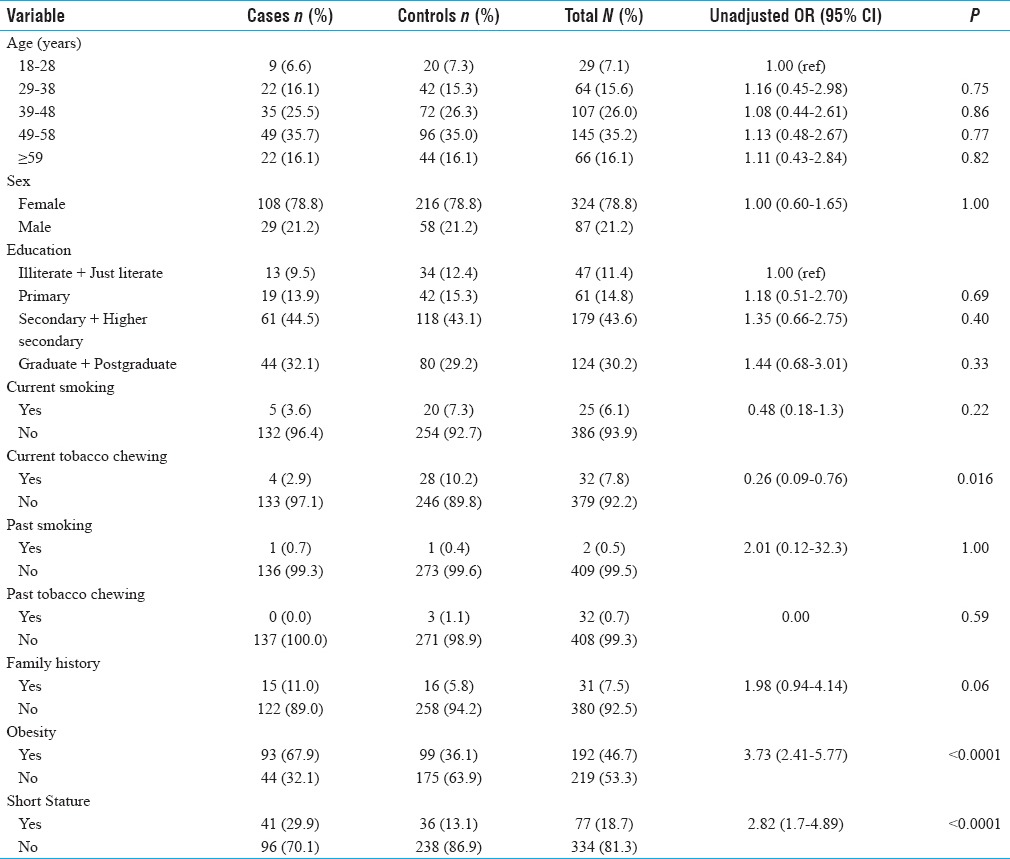
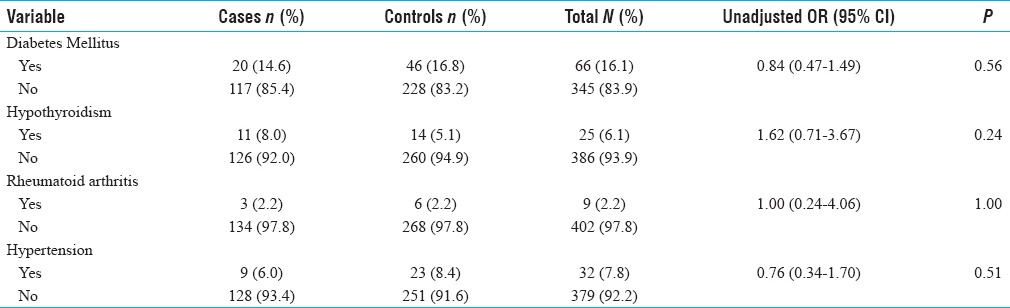
In univariate analysis, significantly higher proportion of cases were found to be obese (OR = 3.73, 95% CI = 2.41–5.77) and having short stature (OR = 2.82, 95% CI = 1.7–4.89). While no difference between cases and controls was detected in education [OR = 1.18, 95% CI = 0.51-2.7 (for primary level education), OR = 1.35, 95% CI = 0.66-2.75 (for secondary and higher secondary level education), and OR = 1.44, 95% CI = 0.68-3.01 (for graduate level education and above)], current (OR = 0.48, 95% CI = 0.18-1.3) or past (OR = 2.01, 95% CI = 0.12-32.3), tobacco smoking and family history (OR = 1.98, 95% CI = 0.94-4.14) as shown in Table 1. Moreover, presence of diseases such as diabetes mellitus (OR = 0.84, 95% CI = 0.47–1.49), hypothyroidism (OR = 1.62, 95% CI = 0.71–3.67), rheumatoid arthritis (OR = 1.0, 95% CI = 0.24–4.06), and hypertension (OR = 0.76, 95% CI = 0.34–1.7) was found to be similar between the two comparison groups [Table 2].
Table 2.
Distribution of cases and controls according to history of present illness
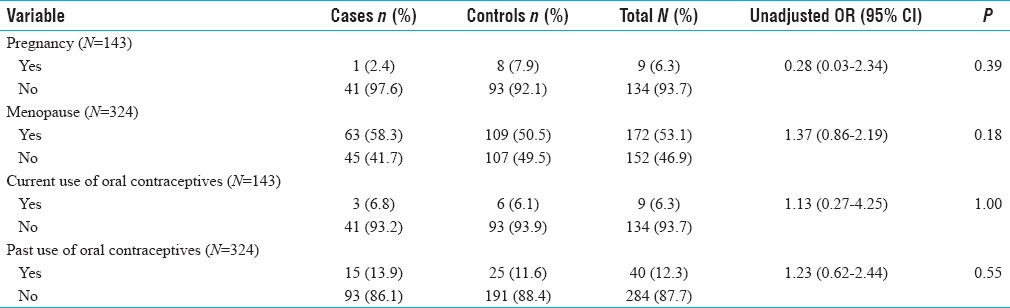
While analysing variables related to female participants only, our study did not find any association between pregnancy (OR = 0.28, 95% CI = 0.03–2.34), menopause (OR = 1.37, 95% CI = 0.86–2.19), and current (OR = 1.13, 95% CI = 0.27–4.25) as well as past (OR = 1.23, 95% CI = 0.62–2.44) use of oral contraceptives and risk of CTS [Table 3].
Table 3.
Distribution of female cases and controls according to other background characteristics
Although current use of computer was found to be significantly associated with CTS (P < 0.01), OR of 0.47 suggests that there is no positive association between computer use and CTS [Table 4].
Table 4.
Distribution of cases and controls according to use of computer
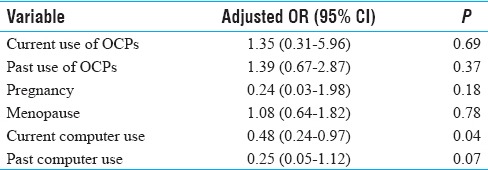
In multivariate model, independent risk factors identified for CTS were education (OR = 0.79, 95% CI = 0.66–0.94), presence of obesity (OR = 3.11, 95% CI = 1.92–5.04), and short stature (OR = 1.06, 95% CI = 1.02–1.1) as shown in Table 5. In this model also, our study found CTS to be significantly associated with current use of computer (P < 0.01). However, OR of value less than one does not indicate positive association between current computer use and CTS [Table 5]. Similarly, multivariate analysis of variables related to only female participants revealed current computer use being associated with CTS (OR = 0.48, 95% CI = 0.24–0.97), nonetheless with OR less than one [Table 6].
Table 5.
Factors associated with CTS - multivariate logistic regression analysis
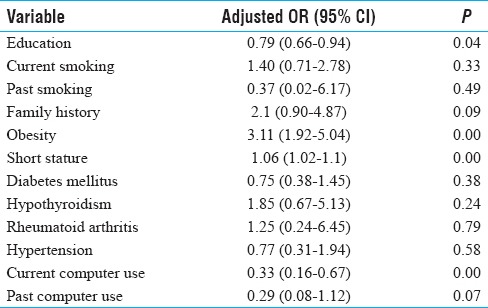
Table 6.
Female factors associated with CTS – multivariate logistic regression analysis
DISCUSSION
The present case-control study was conducted in a school of physiotherapy attached to a teaching hospital. It took about one and a half years to meet the desired sample size of neurophysiologically confirmed cases of CTS. Along with computer use, we studied the conventional risk factors associated with CTS that are described in literature. In our study, level of education, obesity, and short stature were identified as risk factors for CTS. Considering OR less than one in case of education, it can be inferred that it is inversely associated with the risk of CTS. Many studies have demonstrated an association of CTS with obesity [10,19,20,21,22,23] and short stature.[20,21,24] Pressure on the median nerve due to fat near the carpal tunnel may be the reason for this association.[20] Cigarette smoking was reported as a strong age independent risk factor for CTS in a study by Vessey et al.[20] However, a meta-analysis done by Pourmemari et al. found this association only in cross-sectional studies and not in case-control or cohort studies.[25] Our study did not demonstrate smoking, either current or past, as a risk factor for CTS. Similarly, a positive family history was not found to be predictive of CTS in our study, which was in contrast to the finding of a study done by Radecki.[26]
In the present study, chronic diseases such as diabetes mellitus, hypothyroidism, rheumatoid arthritis, and hypertension were not found to be associated with occurrence of CTS. This finding was in congruence to that reported in two European studies done by de Krom et al.[19] and Atroshi et al.[27] However, another case control study conducted by Solomon DH et al. reported a higher risk of CTS in presence of inflammatory arthritis, diabetes and hypothyroidism.[28] Diabetes and hypothyroidism were also found to be in significantly higher proportion in CTS cases than in controls in another case control study done by Karpitskaya et al.[24]
Though pregnancy, use of oral contraceptives, and menopause are linked with CTS, epidemiological evidence seems to be contradictory.[29] Our study did not report significantly higher OR for these variables in respondents with CTS, either in univariate or multivariate model.
The relation between CTS and computer use has been investigated repeatedly by various researchers, however, with unequivocal results. A cross-sectional study conducted in a sample of 648 computer professionals found a higher risk for CTS with higher exposure to computer work.[4] In another study, predictive model of CTS among computer users found a higher probability of CTS with increase in use of computers.[7]
In a meta-analysis conducted by Shiri and Falah-Hassani, six studies conducted among office workers showed a positive association between computer use and CTS. While another six studies in the same meta-analysis demonstrated an inverse association between these two variables.[5] Our study also found negative association between computer use and CTS, which was consistent with the finding of study done by Atroshi et al. that showed a lower risk of CTS in persons with intensive keyboard use at work.[10]
Another review and meta-analysis conducted by Medioni et al. did not show a higher meta-OR for CTS in computer users.[30] In a study done at a medical facility, occurrence of CTS was not found to be different between users and non-users of computer.[12] Similar results were reported in a study done by Hou et al. among male computer users.[13] Thomsen et al., while systematically reviewing eight epidemiological studies, did not find sufficient evidence to support association of computer use and CTS.[15]
In spite of adequate sample size and good case: control ratio, an important limitation of our study is possibility of recall bias because the information regarding past computer use, history of major illnesses, previous use of contraceptives and past smoking was self-reported. Moreover, being a hospital based study, there may be limited generalizability of its results to other populations.
CONCLUSION
Our study, which is perhaps first of its kind that has been conducted in Indian population, provides additional support for negative association between CTS and computer use. However, such an inverse association warrants further risk-benefit analysis by conducting appropriate prospective as well as interventional studies.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Newington L, Harris EC, Walker-Bone K. Carpal Tunnel Syndrome and work. Best Pract Res Clin Rheumatol. 2015;29:440–53. doi: 10.1016/j.berh.2015.04.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aroori S, Spence RA. Carpal tunnel syndrome. Ulster Med J. 2008;77:6–17. [PMC free article] [PubMed] [Google Scholar]
- 3.Kao SY. Carpal Tunnel Syndrome as an occupational disease. J Am Board Fam Med. 2003;16:533–42. doi: 10.3122/jabfm.16.6.533. [DOI] [PubMed] [Google Scholar]
- 4.Ali KM, Sathiyasekaran BW. Computer professionals and Carpal Tunnel Syndrome (CTS) Int J Occup Saf Ergon. 2006;12:319–25. doi: 10.1080/10803548.2006.11076691. [DOI] [PubMed] [Google Scholar]
- 5.Shiri R, Falah-Hassani K. Computer use and carpal tunnel syndrome: A meta-analysis. J Neurol Sci. 2015;349:15–9. doi: 10.1016/j.jns.2014.12.037. [DOI] [PubMed] [Google Scholar]
- 6.Liu CW, Chen TW, Wang MC, Chen CH, Lee CL, Huang MH. Relationship between carpal tunnel syndrome and wrist angle in computer workers. Kaohsiung J Med Sci. 2003;19:617–23. doi: 10.1016/S1607-551X(09)70515-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Matias AC, Salvendy G, Kuczek T. Predictive model of carpal tunnel syndrome causation among VDT operators. Ergonomics. 1998;41:213–26. doi: 10.1080/001401398187260. [DOI] [PubMed] [Google Scholar]
- 8.Office of Registrar General & Census Commissioner, Ministry of Home Affairs, Government of India, New Delhi. Census of India 2011: Houses, household Amenities and assets. [Last accessed on 2017 Apr 25]. Available from: http://censusindia.gov.in/2011census/hlo .
- 9.India internet users. [Last accessed on 2017 Apr 25]. Available from: http://www.internetlivestats.com/internet-users/india/
- 10.Atroshi I, Gummesson C, Ornstein E, Johnsson R, Ranstam J. Carpal tunnel syndrome and keyboard use at work: A population-based study. Arthritis Rheum. 2007;56:3620–5. doi: 10.1002/art.22956. [DOI] [PubMed] [Google Scholar]
- 11.Andersen JH, Thomsen JF, Overgaaard E, Lassen CF, Brandt LPA, Vilstrup I, et al. Computer use and carpal tunnel syndrome: A 1-year follow-up study. JAMA. 2003;289:2963–9. doi: 10.1001/jama.289.22.2963. [DOI] [PubMed] [Google Scholar]
- 12.Stevens JC, Witt JC, Smith BE, Weaver AL. The frequency of carpal tunnel syndrome in computer users at a medical facility. Neurology. 2001;56:1568–70. doi: 10.1212/wnl.56.11.1568. [DOI] [PubMed] [Google Scholar]
- 13.Hou WH, Hsu JH, Lin CH, Liang HW. Carpal tunnel syndrome in male visual display terminal (VDT) workers. Am J Ind Med. 2007;50:1–7. doi: 10.1002/ajim.20396. [DOI] [PubMed] [Google Scholar]
- 14.Mattioli S, Violante FS, Bonfiglioli R. Upper-extremity and neck disorders associated with keyboard and mouse use. Handb Clin Neurol. 2015;131:427–33. doi: 10.1016/B978-0-444-62627-1.00022-6. [DOI] [PubMed] [Google Scholar]
- 15.Thomsen JF, Gerr F, Atroshi I. Carpal tunnel syndrome and the use of computer mouse and keyboard: A systematic review. BMC Musculoskelet Disord. 2008;9:134. doi: 10.1186/1471-2474-9-134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Halikis MN, Taleisnik J, Szabo RM. Compression neuropathies of the upper extremity. In: Chapman MW, editor. Chapman's Orthopedic Surgery. 3rd ed. Philadelphia: Lippincott, Williams and Wilkins; 2001. p. pp. 1554. [Google Scholar]
- 17.Misra UK, Kalita J. Clinical Neurophysiology. 1st ed. New Delhi: BI Churchill Livingstone; 2001. pp. 25–34. [Google Scholar]
- 18.WHO expert consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–63. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- 19.de Krom MC, Kester AD, Knipschild PG, Spaans F. Risk factors for carpal tunnel syndrome. Am J Epidemiol. 1990;132:1102–10. doi: 10.1093/oxfordjournals.aje.a115753. [DOI] [PubMed] [Google Scholar]
- 20.Vessey MP, Villard-Mackintosh L, Yeates D. Epidemiology of carpal tunnel syndrome in women of childbearing age. Findings in a large cohort study. Int J Epidemiol. 1990;19:655–9. doi: 10.1093/ije/19.3.655. [DOI] [PubMed] [Google Scholar]
- 21.de Krom MC, Knipschild PG, Kester AD, Thijs CT, Boekkooi PF, Spaans F. Carpal tunnel syndrome: Prevalence in the general population. J Clin Epidemiol. 1992;45:373–6. doi: 10.1016/0895-4356(92)90038-o. [DOI] [PubMed] [Google Scholar]
- 22.Coggon D, Ntani G, Harris EC, Linaker C, Van der Star R, Cooper C, et al. Differences in risk factors for neurophysiologically confirmed carpal tunnel syndrome and illness with similar symptoms but normal median nerve function: A case-control study. BMC Musculoskelet Disord. 2013;14:240. doi: 10.1186/1471-2474-14-240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Karpitskaya Y, Novak CB, Mackinnon SE. Prevalence of smoking, obesity, diabetes mellitus, and thyroid disease in patients with carpal tunnel syndrome. Ann Plast Surg. 2002;48:269–73. doi: 10.1097/00000637-200203000-00007. [DOI] [PubMed] [Google Scholar]
- 24.Mattioli S, Baldasseroni A, Bovenzi M, Curti S, Cooke RM, Campo G, et al. Risk factors for operated carpal tunnel syndrome: A multicenter population-based case-control study. BMC Public Health. 2009;9:343. doi: 10.1186/1471-2458-9-343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pourmemari MH, Viikari-Juntura E, Shiri R. Smoking and carpal tunnel syndrome: A meta-analysis. Muscle Nerve. 2014;49:345–50. doi: 10.1002/mus.23922. [DOI] [PubMed] [Google Scholar]
- 26.Radecki P. The familial occurrence of carpal tunnel syndrome. Muscle Nerve. 1994;17:325–30. doi: 10.1002/mus.880170311. [DOI] [PubMed] [Google Scholar]
- 27.Atroshi I, Gummesson C, Johnsson R, Ornstein E, Ranstam J, Rosen I. Prevalence of Carpal Tunnel Syndrome in a general population. JAMA. 1999;282:153–8. doi: 10.1001/jama.282.2.153. [DOI] [PubMed] [Google Scholar]
- 28.Solomon DH, Katz JN, Bohn R, Mogun H, Avorn J. Nonoccupational risk factors for carpal tunnel syndrome. J Gen Intern Med. 1999;14:310–4. doi: 10.1046/j.1525-1497.1999.00340.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cooper C, Palmer K. Repeated movements and repeated trauma affecting the musculoskeletal system. In: Baxter PJ, Tar-Ching Aw, Cockcroft A, Durrington P, Harrington JM, editors. Hunter's diseases of occupations. 10th ed. London: Hodder Arnold; 2010. pp. 694–6. [Google Scholar]
- 30.Mediouni Z, de Roquemaurel A, Dumontier C, Becour B, Garrabe H, Roquelaure Y, et al. Is carpal tunnel syndrome related to computer exposure at work. A review and meta-analysis? Occup Environ Med. 2014;56:204–8. doi: 10.1097/JOM.0000000000000080. [DOI] [PubMed] [Google Scholar]


