Abstract
Introduction:
Several flaps have been described for reconstructing facial or oral defects. Flaps such as forehead and pectoralis major are often too bulky for small-to-moderate-sized defects, for which nasolabial flaps are often ideal. However, nasolabial flaps have limited mobility and reach and may need two stages, particularly for intraoral defects. According to recent literatures, facial artery provides numerous small cutaneous perforators, based on which skin flaps can be islanded, with greater mobility and reach for reconstruction of small-to-moderate-sized intraoral and facial defects in one stage. Our study aims to evaluate the reliability and versatility of facial artery perforator-based flaps in the reconstruction of such defects.
Materials and Methods:
A ethical committee-approved retrospective study was conducted on data of the patients attending our outpatient department between February 2014 and October 2015 with small-to-moderate-sized facial/oral lesions. The total sample size was 23. We studied the relation of flap survival with size of flap, route of inset and neck dissection, functional and aesthetic outcomes and feasibility of adjuvant therapy in cases of malignancies.
Results and Analysis:
A wide range of facial defects, especially intraoral defects, could be reconstructed in one stage using facial artery perforator-based flaps. The flaps were reliable. Complications included only partial skin loss of the flaps in a few cases. Complications were directly related to the length of the flaps and the route of inset. Functional and aesthetic outcomes were satisfactory and none of the flaps showed any significant post-radiotherapy changes.
Conclusions:
We concluded that facial artery perforator flap can be a simple, safe, versatile and one-stage alternative to the traditional flaps in the reconstruction of small-to-moderate-sized facial defects. Neck dissection can be safely done in the same sitting.
KEY WORDS: Facial artery; nasolabial flap; perforator, propeller flap
INTRODUCTION
Reconstruction of facial and intraoral defects due to trauma, neoplasm or infection remains a challenge. Skin grafts and several flaps have been described for reconstruction including local, regional, distant or free flaps. Flaps such as forehead, deltopectoral, pectoralis major myocutaneous and radial artery forearm are often extensive procedures, bulky and too large for small-to-moderate-sized intraoral or facial defects and are associated with donor-site morbidity. Local flaps such as nasolabial flaps are often ideal for such small-to-moderate-sized defects as they provide good colour and texture match with minimum donor-site morbidity, but still they have some limitations such as limited mobility and reach, particularly in intraoral defects and may need two stages.
According to recent literatures, facial artery provides numerous small perforators that supply the facial skin by piercing the superficial musculo-aponeurotic system. The cadaveric study by Ng et al. showed multiple perforators along the facial artery, a mean of 4 on each half of the face (range: 2–8), with a mean diameter of 0.94 mm (range: 0.53–1.36 mm) and maximum perforators between 20 and 60 mm from the origin along the length of the facial artery.[1] This roughly corresponds to an area near the angle of the mouth around the nasolabial fold. A local skin flap based on such perforators can be islanded, with greater freedom in flap designing, mobility and reach and used for reconstruction of small-to-moderate-sized intraoral and facial defects in one stage,[2] maintaining all the advantages of nasolabial flap. We routinely used audio Doppler to search for the facial artery perforators. However, the literature does not definitely tell us whether Doppler ultrasound can distinguish such perforators from the facial artery itself with confidence.[2,3,4,5,6] Again, the process of meticulous dissection around the perforator and identification of a perforator originating from the source artery may not be necessary always because the cranial portion of the flap if left undissected will always include numerous 'micro-perforators', which make the flap reliable and safe.[7] However in all our cases, we have identified the perforators to further improve reliability of the flaps. Our study aims to evaluate the reliability and versatility of facial artery perforator-based island flaps in the reconstruction of small-to-moderate-sized facial defects.
MATERIALS AND METHODS
Having obtained the institutional ethical committee approval, a retrospective study was conducted on the data of the patients who had attended our outpatient department between February 2014 and October 2015 with small-to-moderate-sized facial/oral lesions. Patients with large lesions, whose post-excisional defects would not be amenable to reconstruction by local flaps, were excluded from the study. The total sample size was 23. The parameters studied were site and size of the defect, size of the flap, relation of flap survival with size of flap, route of inset, neck dissection (which involved ligation of facial artery), functional and aesthetic outcomes and lastly, feasibility of adjuvant therapy in cases of malignancies.
A handheld audio Doppler was routinely used to locate facial artery perforators in all cases. Pre-operative decision was made regarding the selection of route of inset (direct orocutaneous/subcutaneous tunnel/propeller) depending on the site of the defect in each case. The study population was randomly divided based on the timing of neck dissection (same stage or two stages alternately). Pre-validated questionnaires concerning functional (speech, mastication, deglutition and oral continence) and aesthetic outcomes derived from the article by Hofstra et al.[8] were used to follow up the patients [Table 1].
Table 1.
Questionnaire for oral functional and aesthetic outcome (Courtesy - Hofstra et al.)
A small 2 cm × 1.5 cm dysplastic lesion at the lower lip and right oral commissure is shown along with the course of the facial artery and the line of perforators, which has been marked using audio Doppler [Figure 1a]. The lesion was excised with adequate margin. An islanded flap has been planned at the nasolabial area and elevated in subcutaneous plane, based on a narrow subcutaneous pedicle containing the facial artery perforators [Figure 1b]. A direct orocutaneous route is developed for transferring the flap to intraoral aspect. The route of inset is demonstrated by a finger insinuated from the intra-oral aspect to the extraoral aspect showing that the route is wide enough for transfer of the flap [Figure 1c]. The flap is shown after the final inset with the donor site being closed primarily [Figure 1d]. At 2-month follow-up, an excellent lip contour is achieved with an inconspicuous donor scar [Figure 1e]. Inclusion of hair-bearing part of the nasolabial area in the flap resulted in hair growth inside the oral cavity, which is an occasional drawback of the flap [Figure 1f].
Figure 1.

(a) A small dysplastic lesion at the lower lip and right oral commissure. The course of the facial artery along with the line of perforators has been marked using audio Doppler. (b) Lesion has been excised and an islanded flap has been elevated based on the subcutaneous pedicle containing the facial artery perforators. (c) A finger has been insinuated from the intra-oral aspect to the extra-oral aspect near the flap pedicle to show the route of inset of the flap. (d) The flap after the final inset. The donor site has been closed primarily. (e) The defect created after excision of the lesion was reconstructed with facial artery perforator-based islanded flap. Note the excellent lower lip contour with inconspicuous donor scar at 2-month follow-up. (f) The final appearance of the flap in the inner aspect at 2-month follow-up. Note the inclusion of hair-bearing part inside the oral cavity, which is a drawback of this flap
In another case, a squamous cell carcinoma (SCC) is shown at the left buccal mucosa [Figure 2a]. The lesion was excised with adequate margin. Perforator has been dissected [Figure 2b]. The flap has been islanded over the dissected perforator [Figure 2c]. The flap has been transferred intraorally via a direct orocutaneous route. The final inset is shown in Figure 2d. The final appearance of the flap is shown at 4-month follow-up [Figure 2e].
Figure 2.
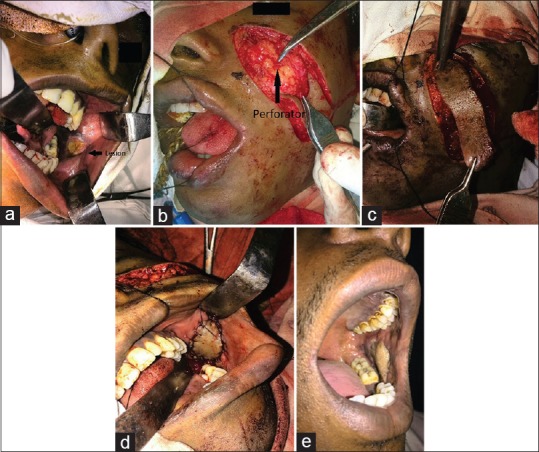
(a) Squamous cell carcinoma at the left buccal mucosa. (b) The flap has been elevated in the nasolabial area. The perforator has been dissected out. (c) The flap has been islanded over the dissected perforator. (d) The flap has been transferred into the oral cavity by a direct orocutaneous route and inset at the defect to line the buccal mucosa. (e) Final appearance of the flap at 4-month follow-up. Note the well-settled flap with an adequate mouth opening
A small SCC at the left ala of nose is shown along with audio Doppler-marked facial artery perforators [Figure 3a]. After excision of the lesion with adequate margin, a full-thickness alar defect is shown in Figure 3b. A flap of 5 cm × 1.5 cm has been designed along with dissection of the facial artery perforators [Figure 3c]. The flap has been rotated in a propeller fashion based on the cranial perforator. The final inset of the flap to create both inner lining and outer skin cover of ala in a single stage is shown along with primary closure of the donor defect [Figure 3d]. A final appearance at 20-month follow-up is shown in Figure 3e.
Figure 3.

(a) Squamous cell carcinoma at the left ala. Facial artery perforators have been localised using audio Doppler and marked. (b) Lesion has been excised resulting in full-thickness alar defect. Note the nasal septum visible through the alar defect in the lateral view. (c) Islanded flap has been designed. Note the two dissected perforators. The locations of these perforators are corroborative with the audio Doppler findings in a. (d) The caudal perforator has been ligated and the flap is rotated axially on the cranial perforator in a propeller fashion. After the final inset, both the inner lining and outer skin cover of ala have been recreated in single stage. The donor defect has been closed primarily. (e) The final appearance of the flap and the donor scar at 20-month follow-up. Note the well-settled flap and an almost inconspicuous donor scar that blended nicely with the nasolabial fold
RESULTS AND ANALYSIS
Six patients had lesions over buccal mucosa, six over oral commissure, five had lesions over lip only and three over commissure with adjacent lip whereas there were other less frequented areas such as retromolar trigone (1), floor of mouth (1) and ala of nose (1). Defect sizes ranged from a minimum length and breadth of 2 cm and 1 cm, respectively, to a maximum length and breadth of 6 cm and 5 cm, respectively. In three patients, marginal or segmental mandibulectomy was done for complete excision of the growth [Table 2].
Table 2.
Demography of patients, reconstructive details and outcomes
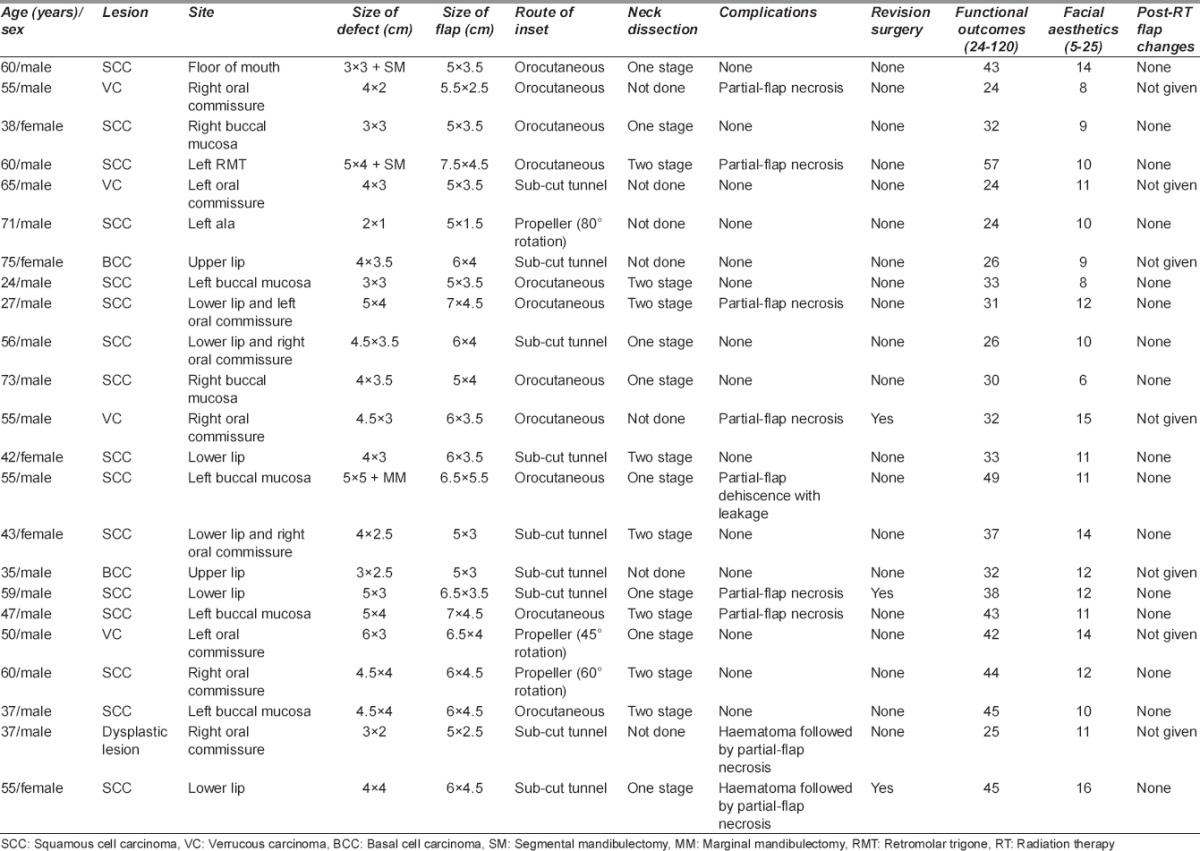
During planning, an extra length of flap was taken into account for the elastic recoil of the skin. We dissected the pedicle to a sufficient length to reach the defect through the intervening tissues. The flap dimensions ranged from a minimum length and breadth of 5 cm and 1.5 cm, respectively, to a maximum length and breadth of 7.5 cm and 5.5 cm, respectively. All the defects were reconstructed by islanded facial artery perforator-based flaps. In nine cases, the flaps were inset by passing through a subcutaneous tunnel into the defect at lip/commissure; in eleven cases, inset was done by passing the flap with the pedicle directly into the oral cavity via a direct orocutaneous route to the intraoral and commissure defects and in three cases, the flaps were raised from the area adjacent to the defect, directly inset into the defect at commissure and at ala as propeller flap by rotating the flap through variable degrees of 45°, 60° and 80°, respectively. Totally 16 neck dissections were performed out of the 23 cases, of which 8 were done in the same stage and the other 8 were done in the second stage after 3 weeks.
None of the flaps in this study suffered complete loss. Among the cases of flap complications, there was only partial-thickness loss of a portion of the flaps whereas a major portion of these flaps survived. There were eight cases of partial-thickness flap necrosis and one case of leakage/fistula [Table 3]. The complication rate increased with increasing length of the flaps. Beyond 6.5-cm length, most of the flaps had some complications [Chart 1]. There were incidences of flap complications with subcutaneous and direct orocutaneous routes probably due to some pedicle compression [Chart 2]. Most of the flap complications were clinically due to venous drainage. However, the flap survival rate did not bear any correlation with the stage in which neck dissection was done [Chart 3]. Nine cases required nasogastric tube feed, after intraoral reconstruction, with a mean duration of 6.78 days. Of the nine cases that developed flap complications, three had to undergo revisions either on lower lips (two cases) or oral commissure and lower lip (one case). Patients were discharged after ensuring the adequacy of oral intake and ruling out any leak or fistula. The mean duration of post-operative hospital stay was 7.96 days.
Table 3.
Types of flap complications
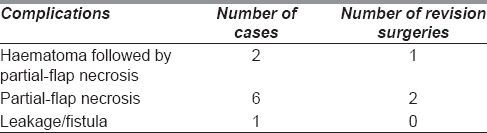
Chart 1.
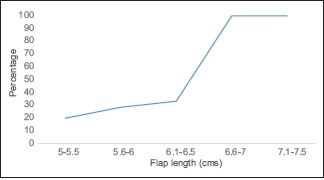
Flap complication rate with increasing flap length
Chart 2.
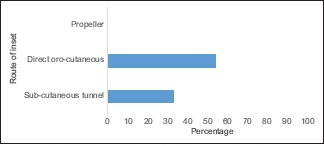
Flap complication rate in different routes of inset
Chart 3.
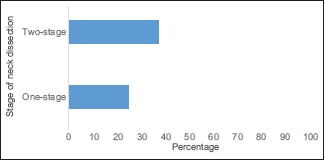
Flap complication rate with same one- or two-stage neck dissection
Functional outcome and facial aesthetics were assessed after 6 weeks of operation, with an average score of 35.43 and 11.13, respectively. These scores were on a scale where best functional and aesthetics scores were 24 and 5, respectively, while poorest scores were 120 and 25, respectively.[8]
The patient with lesion at the left buccal mucosa whose intraoral defect was reconstructed with facial artery perforator-based islanded flap inset via direct orocutaneous route in one stage showed excellent functional outcome with well-settled flap and adequate mouth opening at 4-month follow-up [Figure 2e]. Similar functional outcome is noticed in Figure 1f.
The patient with lesion at the left ala of the nose whose defect was reconstructed by a propeller pattern flap based on facial artery perforator showed excellent aesthetic outcome with almost inconspicuous facial scar and a well-settled flap at 20-month follow-up [Figure 3e].
There were no significant differences in 2-point discrimination (mean: 5.6 mm and 5.3 mm for flaps and control sites, respectively), hot-cold and blunt-sharp sensation between flap and control sites.
Sixteen out of 23 cases received adjuvant radiation therapy (RT). The effects of radiation on the flaps were assessed after 6 weeks' post-RT. The signs of radiation damage that were looked for were oedema, erythema, desquamation, volume loss/shrinkage, ulceration, necrosis, fistula/leakage, infection and lastly mouth opening. The flaps did not show any significant change at follow-up. Patients complained of generalised dryness of mouth following RT. RT in the head-and-neck region causes xerostomia.[8,9]
In some of the cases, hair-bearing area of the face had to be included in the flap leading to hair growth inside the oral cavity, for which the patients complained of discomfort, especially those who did not receive RT [Figure 1f]. This issue was addressed to by trimming of hair.
DISCUSSION
The facial artery perforator-based flap is supported by the study of angiosomes of the facial region, which showed that the facial arterial system supplies the cutaneous areas from the submental region to the medial two-thirds of the face.[10] Although Nakajima et al.[11] reported variations in the facial artery and its branches, the superior labial, lateral nasal and angular arteries are consistent in 98% of cases, with 2% of facial arteries terminating at the alar base level. Cadaveric studies have shown a rich perforator density in the perioral and perinasal areas.[1] It has been shown that an average of five perforators exist per facial artery with a mean diameter of 0.96 mm. The perforators were selectively injected with diluted ink solution, and the mean size of all the injected skin areas was 8.05 cm2. Seven main reliable types of perforator territories were identified: the posterior area of the horizontal ramus of the mandible, the anterior area of the horizontal ramus of the mandible, the inferior labial area, the commissural area, the jugal area, the nasolabial area and the subpalpebral area.[12]
It is debatable whether to call this flap a perforator flap. According to the Gent Consensus Conference,[13] a perforator should pierce the deep fascia before reaching the skin. Since there is no deep fascia layer in the face and the vessels pierce the superficial muscular aponeurotic system layer before reaching the skin, this flap can be also called a perforator flap.[2]
In this study, facial artery perforator-based flap was used in the reconstruction of a wide range of defect sites, especially intraoral defects, with distinct advantage over traditional nasolabial flap by virtue of having greater arc of rotation, mobility and thus reach of the flap and being a one-stage procedure. These flaps were used to reconstruct small-to-moderate-sized defects (5–6 cm) and even defects created after certain extent of mandibular resection. Intraoperative perforator identification was corroborative with pre-operative localisation of perforators by audio Doppler.
The flap complication rate showed a strong correlation with flap length. Maximum safe length that can be taken is approximately 6.5 cm. However, other factors such as route of inset and resulting pedicle compression have also to be considered. None of the flaps suffered any complete necrosis. The complication rate was 39.13% which included haematoma, partial-thickness flap necrosis, leakage or fistula. The rate of flap revision was 13.04%. Flap survival did not depend on the stage in which neck dissection was performed, showing that the flaps received their vascular supply adequately from the angular arteries in cases where the facial arteries were ligated.
The functional outcomes (speech, mouth opening, mastication, deglutition, oral continence and flap sensation) and facial aesthetics were acceptable. There were no significant post-RT changes except for generalised dryness of mouth.
However, the inclusion of hair-bearing area in some of the cases raised discomfort in patients, particularly those who did not receive RT. This issue was managed by trimming of the hair.
CONCLUSIONS
From the study, it could be concluded that facial artery perforator-based island flap takes all the advantage of nasolabial flap, such as skin colour and texture match and primary closure of the donor site along with the added advantages of a perforator flap, including versatility to cover the defect in terms of mobility and reach, with a reliable and constant blood supply. Thus, facial artery perforator-based flap can be good, simple, safe, versatile and an one-stage alternative to the traditional nasolabial flaps and even some of the major workhorse flaps to reconstruct small-to-moderate-sized facial defects of 10–15 cm2 size, with minimum donor-site morbidity and acceptable functional outcome. Neck dissection can be safely done in the same sitting.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Ng ZY, Fogg QA, Shoaib T. Where to find facial artery perforators: A reference point. J Plast Reconstr Aesthet Surg. 2010;63:2046–51. doi: 10.1016/j.bjps.2010.01.002. [DOI] [PubMed] [Google Scholar]
- 2.D'Arpa S, Cordova A, Pirrello R, Moschella F. Free style facial artery perforator flap for one stage reconstruction of the nasal ala. J Plast Reconstr Aesthet Surg. 2009;62:36–42. doi: 10.1016/j.bjps.2008.06.057. [DOI] [PubMed] [Google Scholar]
- 3.Lyons AJ. Perforator flaps in head and neck surgery. Int J Oral Maxillofac Surg. 2006;35:199–207. doi: 10.1016/j.ijom.2005.07.015. [DOI] [PubMed] [Google Scholar]
- 4.Taylor GI, Palmer JH. The vascular territories (angiosomes) of the body: Experimental study and clinical applications. Br J Plast Surg. 1987;40:113–41. doi: 10.1016/0007-1226(87)90185-8. [DOI] [PubMed] [Google Scholar]
- 5.Demirseren ME, Afandiyev K, Ceran C. Reconstruction of the perioral and perinasal defects with facial artery perforator flaps. J Plast Reconstr Aesthet Surg. 2009;62:1616–20. doi: 10.1016/j.bjps.2008.07.037. [DOI] [PubMed] [Google Scholar]
- 6.Taylor GI, Doyle M, McCarten G. The Doppler probe for planning flaps: Anatomical study and clinical applications. Br J Plast Surg. 1990;43:1–6. doi: 10.1016/0007-1226(90)90039-3. [DOI] [PubMed] [Google Scholar]
- 7.Kim JT. New nomenclature concept of perforator flap. Br J Plast Surg. 2005;58:431–40. doi: 10.1016/j.bjps.2004.12.009. [DOI] [PubMed] [Google Scholar]
- 8.Hofstra EI, Hofer SO, Nauta JM, Roodenburg JL, Lichtendahl DH. Oral functional outcome after intraoral reconstruction with nasolabial flaps. Br J Plast Surg. 2004;57:150–5. doi: 10.1016/j.bjps.2003.11.012. [DOI] [PubMed] [Google Scholar]
- 9.Franzén L, Funegård U, Ericson T, Henriksson R. Parotid gland function during and following radiotherapy of malignancies in the head and neck. A consecutive study of salivary flow and patient discomfort. Eur J Cancer. 1992;28:457–62. doi: 10.1016/s0959-8049(05)80076-0. [DOI] [PubMed] [Google Scholar]
- 10.Houseman ND, Taylor GI, Pan WR. The angiosomes of the head and neck: Anatomic study and clinical applications. Plast Reconstr Surg. 2000;105:2287–313. doi: 10.1097/00006534-200006000-00001. [DOI] [PubMed] [Google Scholar]
- 11.Nakajima H, Imanishi N, Aiso S. Facial artery in the upper lip and nose: Anatomy and a clinical application. Plast Reconstr Surg. 2002;109:855–61. doi: 10.1097/00006534-200203000-00003. [DOI] [PubMed] [Google Scholar]
- 12.Qassemyar Q, Havet E, Sinna R. Vascular basis of the facial artery perforator flap: Analysis of 101 perforator territories. Plast Reconstr Surg. 2012;129:421–9. doi: 10.1097/PRS.0b013e31822b6771. [DOI] [PubMed] [Google Scholar]
- 13.Blondeel PN, Van Landuyt KH, Monstrey SJ, Hamdi M, Matton GE, Allen RJ, et al. The “Gent” consensus on perforator flap terminology: Preliminary definitions. Plast Reconstr Surg. 2003;112:1378–83. doi: 10.1097/01.PRS.0000081071.83805.B6. [DOI] [PubMed] [Google Scholar]


